Evaluation of a Computer-Tailored Healthy Ageing Intervention to Promote Physical Activity among Single Older Adults with a Chronic Disease
Abstract
1. Introduction
2. Materials and Methods
2.1. Intervention
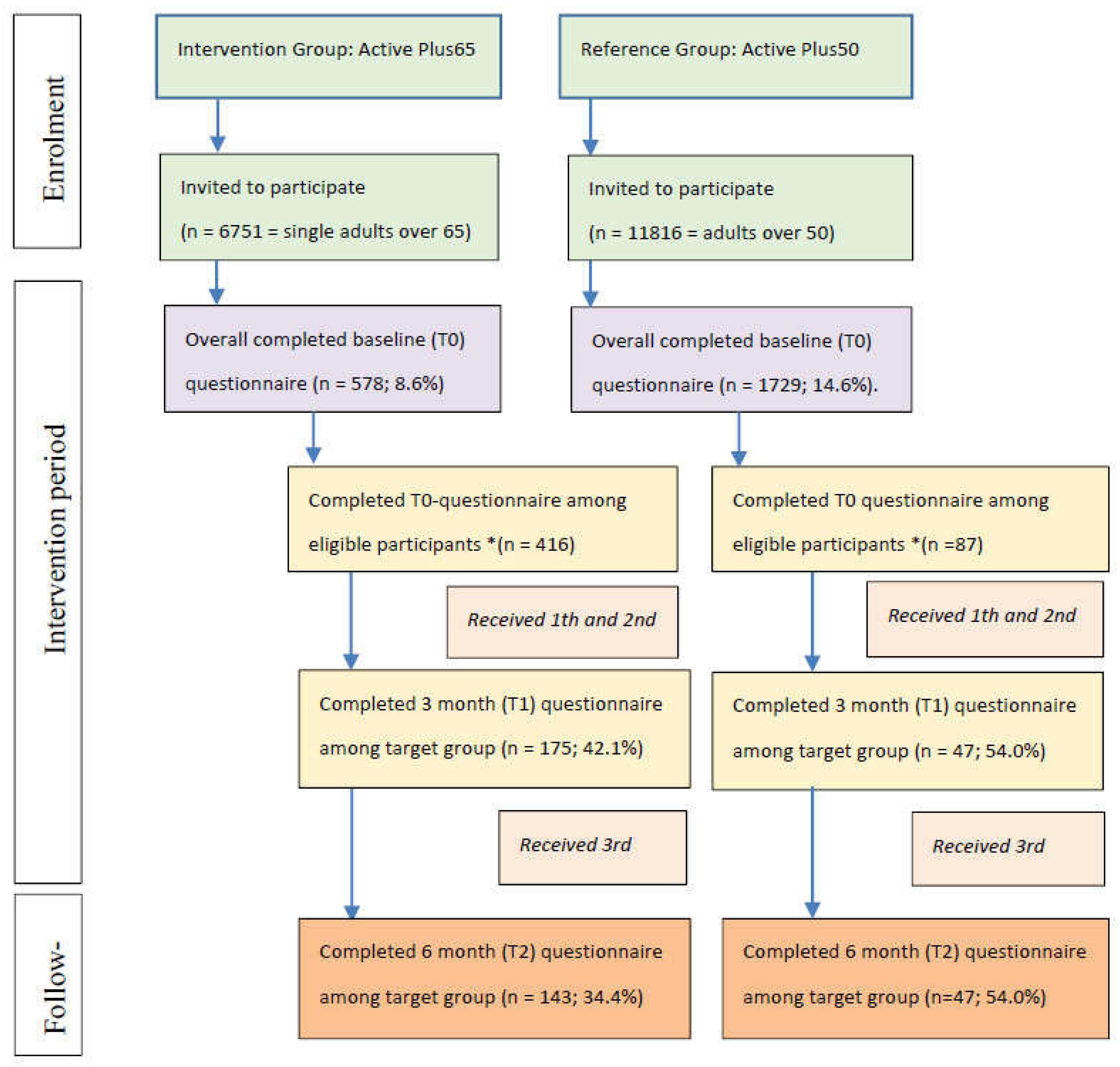
2.2. Study Design and Procedures
2.3. Measures
2.3.1. Outcome Measures
2.3.2. Demographics
2.4. Statistical Analyses
3. Results
3.1. Characteristics of the Study Population
3.2. Intervention Effects on PA
4. Discussion
4.1. Intervention Effects on PA
4.2. Methodological Issues
5. Conclusions
Acknowledgments
Author Contributions
Conflicts of Interest
Abbreviations
| BMI | Body Mass Index |
| ES | Effect Size |
| MVPA | Minutes of moderate to vigorous physical activity |
| NCCD | Non-communicable chronic disease |
| PA | Physical activity |
| RCT | Randomized clinical trial |
References
- World Health Organisation. World Report on Ageing and Health; WHO: Geneva, Switzerland, 2015. [Google Scholar]
- Organisation for Economic Cooperation and Development Expenditure by Disease, Age and Gender. Available online: http://www.oecd.org/els/health-systems/Expenditure-by-disease-age-and-gender-FOCUS-April2016.pdf (accessed on 31 May 2017).
- European Union. Quality of Life: Facts and Views; European Union: Geneva, Switzerland, 2015. [Google Scholar]
- Ding, D.; Lawson, K.D.; Kolbe-Alexander, T.L.; Finkelstein, E.A.; Katzmarzyk, P.T.; van Mechelen, W.; Pratt, M. The economic burden of physical inactivity: A global analysis of major non-communicable diseases. Lancet 2016, 388, 1311–1324. [Google Scholar] [CrossRef]
- McKenna, M.; Collins, J. Current issues and challenges in chronic disease control. In Chronic Disease Epidemiology and Control; Remington, P.L., Wegner, M.V., Brownson, R.C., Eds.; American Public Health Association: Washington, DC, USA, 2010; pp. 1–24. [Google Scholar]
- Goodman, R.A.; Posner, S.F.; Huang, E.S.; Parekh, A.K.; Koh, H.K. Defining and measuring chronic conditions: Imperatives for research, policy, program, and practice. Prev. Chronic Dis. 2013, 10. [Google Scholar] [CrossRef] [PubMed]
- Matheson, G.; Klügl, M.; Engebretsen, L.; Bendiksen, F.; Blair, S.; Börjesson, M.; Budgett, R.; Derman, W.; Erdener, U.; Ioannidis, J.; et al. Prevention and management of non-communicable disease: The ioc consensus statement, lausanne 2013. Sports Med. 2013, 43, 1075–1088. [Google Scholar] [CrossRef] [PubMed]
- World Health Organisation Global Recommendations on Physical Activity for Health. Available online: http://www.who.int/dietphysicalactivity/publications/9789241599979/en/ (accessed on 18 September 2017).
- Hamer, M.; Lavoie, K.L.; Bacon, S.L. Taking up physical activity in later life and healthy ageing: The English longitudinal study of ageing. Br. J. Sports Med. 2014, 48, 239–243. [Google Scholar] [CrossRef] [PubMed]
- Ekelund, U.; Steene-Johannessen, J.; Brown, W.J.; Fagerland, M.W.; Owen, N.; Powell, K.E.; Bauman, A.; Lee, I.M. Does physical activity attenuate, or even eliminate, the detrimental association of sitting time with mortality? A harmonised meta-analysis of data from more than 1 million men and women. Lancet 2016, 388, 1302–1310. [Google Scholar] [CrossRef]
- Gajewski, P.; Falkenstein, M. Physical activity and neurocognitive functioning in aging—A condensed updated review. Eur. Rev. Aging Phys. Act. 2016, 13, 1–7. [Google Scholar] [CrossRef] [PubMed]
- World Health Organisation Global Report on Falls Prevention in Older Adults. Available online: https://books.google.nl/books?hl=nl&lr=&id=ms9o2dvfaQkC&oi=fnd&pg=PA1&dq=world+health+organisation+balance+older+adults&ots=5JFZHDULVP&sig=t88_W268r7Em4gkAayyDsBjZAMA#v=onepage&q=world%20health%20organisation%20balance%20older%20adults&f=false (accessed on 31 May 2017).
- Dutch Department of Health, Welfare and Sports. Physical Activity Guidelines. Available online: http://www.webcitation.org/6rG9EZmy4 (accessed on 16 June 2017).
- Sun, R.; Norman, J.; While, A. Physical activity in older people: A systematic review. BMC Public Health 2013, 13. [Google Scholar] [CrossRef] [PubMed]
- Newsom, J.T.; Huguet, N.; McCarthy, M.J.; Ramage-Morin, P.; Kaplan, M.S.; Bernier, J.; Bentson, M.; McFarland, M.; Oderkirk, J. Health hehavior change following chronic illness in middle and later life. J. Gerontol. Psycholol. Soc. Sci. 2012, 67, 279–288. [Google Scholar] [CrossRef] [PubMed]
- Öztürk, A.; Şimşek, T.T.; Yümin, E.T.; Sertel, M.; Yümin, M. The relationship between physical, functional capacity and quality of life (qol) among elderly people with a chronic disease. Arch. Gerontol. Geriatr. 2011, 53, 278–283. [Google Scholar] [CrossRef] [PubMed]
- World Health Organisation World Report on Disability. Available online: http://www.who.int/disabilities/world_report/2011/en/ (accessed on 19 August 2017).
- Dutch Department of Health, Welfare and Sports. Physical activity and Sports Behavior of People with a Chronic Condition. Available online: http://www.rivm.nl/Documenten_en_publicaties/Algemeen_Actueel/Nieuwsberichten/2015/Mensen_met_een_beperking_sporten_minder (accessed on 3 May 2017).
- World Health Organisation Prevalence of Insufficient Physical Activity. Available online: http://www.who.int/gho/ncd/risk_factors/physical_activity_text/en/ (accessed on 19 January 2017).
- Cattan, M.; White, M.; Bond, J.; Learmouth, A. Preventing social isolation and loneliness among older people: A systematic review of health promotion interventions. Ageing Soc. 2005, 25, 44–67. [Google Scholar] [CrossRef]
- Hawkley, L.C.; Thisted, R.A.; Cacioppo, J.T. Loneliness predicts reduced physical activity: Cross-sectional & longitudinal analyses. Health Psychol. 2009, 28, 354–363. [Google Scholar] [PubMed]
- Hawton, A.; Green, C.; Dickens, A.P.; Richards, S.H.; Taylor, R.S.; Edwards, R.; Greaves, C.J.; Campbell, J.L. The impact of social isolation on the health status and health-related quality of life of older people. Qual. Life 2014, 20, 57–67. [Google Scholar] [CrossRef] [PubMed]
- Muellmann, S.; Forberger, S.; Mollers, T.; Broring, E.; Zeeb, H.; Pischke, C.R. Effectiveness of ehealth interventions for the promotion of physical activity in older adults: A systematic review. Prev. Med. 2017, 108, 93–110. [Google Scholar] [CrossRef] [PubMed]
- Elbert, N.J.; van Os-Medendorp, H.; van Renselaar, W.; Ekeland, A.G.; Hakkaart-van Roijen, L.; Raat, H.; Nijsten, T.E.C.; Pasmans, S.G.M.A. Effectiveness and cost-effectiveness of ehealth interventions in somatic diseases: A systematic review of systematic reviews and meta-analyses. J. Med. Int. Res. 2014, 16, 1–23. [Google Scholar] [CrossRef] [PubMed]
- World Health Organisation. Global Status Report on Non-Communicable Diseases 2014; WHO: Geneva, Switzerland, 2010. [Google Scholar]
- Boekhout, J.M.; Peels, D.A.; Berendsen, B.A.J.; Bolman, C.A.W.; Lechner, L. An ehealth intervention to promote physical activity and social network of single, chronically impaired older adults: Adaptation of an existing intervention using intervention mapping. JMIR Res. Protoc. 2017, 2017. [Google Scholar] [CrossRef] [PubMed]
- Peels, D.A.; Bolman, C.; Golsteijn, R.H.J.; De Vries, H.; Mudde, A.N.; Van Stralen, M.M.; Lechner, L. Long-term efficacy of a tailored physical activity intervention among older adults. Int. J. Behavior Nutr. Phys. Act. 2013, 10. [Google Scholar] [CrossRef]
- Peels, D.A.; Van Stralen, M.M.; Bolman, C.; Golsteijn, R.H.J.; De Vries, H.; Mudde, A.N.; Lechner, L. The differentiated (short-term) effectiveness of a printed versus a web-based tailored intervention to promote physical activity among the over-fifties: A randomized controlled trial. Health Educ. Res. 2014, 29, 870–882. [Google Scholar] [CrossRef] [PubMed]
- Curran, G.M.; Bauer, M.; Mittman, B.; Pyne, J.M.; Stetler, C. Effectiveness-implementation hybrid designs: Combining elements of clinical effectiveness and implementation research to enhance public health impact. Med. Care 2012, 50, 217–226. [Google Scholar] [CrossRef] [PubMed]
- Glasgow, R.E.; Vogt, T.M.; Boles, S.M. Evaluating the public health impact of health promotion interventions: The re-aim framework. Am. J. Public Health 1999, 89, 1322–1327. [Google Scholar] [CrossRef] [PubMed]
- Bartholomew, L.K.; Markham, C.M.; Ruiter, R.A.C.; Fernandez, M.E.; Kok, G.; Parcel, G.S. Planning Health Promotyion Programs: An Intervention Mapping Approach, 4th ed.; Jossey-Bass: San Francisco, CA, USA, 2016. [Google Scholar]
- De Vries, H.; Mudde, A.; Leijs, I.; Charlton, A.; Vartiainen, E.; Buijs, G.; Clemente, M.; Storm, H.; Navarro, A.; Nebot, M.; et al. The European smoking prevention framework approach (EFSA): An example of integral prevention. Health Educ. Res. 2003, 18, 611–626. [Google Scholar] [CrossRef] [PubMed]
- Prochaska, J.O.; Redding, C.A.; Evers, K.E. The transtheoretical model and stages of change. In Health Behaviour and Health Education: Theory, Research, and Practice; Glanz, K., Rimer, B.K., Viswanath, K., Eds.; Jossey-Bass: San Francisco, CA, USA, 2008. [Google Scholar]
- Ryan, R.; Deci, E.L. Self-determination theory and the facilitation of intrinsic motivation, social development, and well-being. Am. Psychol. 2000, 55, 68–78. [Google Scholar] [CrossRef] [PubMed]
- Baumeister, R.F.; Vohs, K.D. Handbook of Self-Regulation: Research, Theory, and Applications; The Guilford Press: New York, NY, USA, 2004. [Google Scholar]
- Schwarzer, R.; Luszczynska, A. How to overcome health-compromising behaviors: The health action process approach. Eur. Psychol. 2008, 13, 141–151. [Google Scholar] [CrossRef]
- Peels, D.A.; Van Stralen, M.M.; Bolman, C.; Golsteijn, R.H.J.; De Vries, H.; Mudde, A.N.; Lechner, L. The development of a web-based computer tailored advice to promote physical activity among people older than 50 years. J. Med. Int. Res. 2012, 14. [Google Scholar] [CrossRef] [PubMed]
- Van Stralen, M.M.; Kok, G.; De Vries, H.; Mudde, A.N.; Bolman, C.; Lechner, L. The active plus protocol: Systematic development of two theory and evidence-based tailored physical activity interventions for the over-fifties. BMC Public Health 2008, 8. [Google Scholar] [CrossRef] [PubMed]
- Hobbs, N.; Godfrey, A.; Lara, J.; Errington, L.; Meyer, T.D.; Rochester, L.; White, M.; Methers, J.C.; Sniehotta, F.F. Are behavioural interventions effective in increasing physical activity at 12 to 36 months in adults aged 55 to 70 years? A systematic review and meta-analysis. BMC Med. 2013, 11. [Google Scholar] [CrossRef] [PubMed]
- Guertler, D.; Vandelanotte, C.; Kirwan, M.; Duncan, M.J. Engagement and nonusage attrition with a free physical activity promotion program: The case of 10,000 steps Australia. J. Med. Int. Res. 2015, 17. [Google Scholar] [CrossRef] [PubMed]
- Neve, M.J.; Collins, C.E.; Morgan, P.J. Dropout, nonusage attrition, and pretreatment predictors of non usage attrition in a commercial web-based weight loss program. J. Med. Int. Res. 2010, 12, 81–96. [Google Scholar]
- Wanner, M.; Martin-Diener, E.; Braun-Fahrländer, C.; Bauer, G.; Martin, B.W. Effectiveness of active-online, an individually tailored physical activity intervention, in a real-life setting: Randomized controlled trial. J. Med. Int. Res. 2009, 11. [Google Scholar] [CrossRef] [PubMed]
- Faul, F.; Erdfelder, E.; Lang, A.-G.; Buchner, A. G*power 3: A flexible statistical power analysis program for the social, behavioral, and biomedical sciences. Behav. Res. Methods 2007, 39, 175–191. [Google Scholar] [CrossRef] [PubMed]
- De Hollander, E.L.; Zwart, L.; De Vries, S.I.; Wendel-Vos, W. The squash was a more valid tool than the obin for categorizing adults according to the dutich physical activity guideline. J. Clin. Epidemiol. 2012, 65, 73–81. [Google Scholar] [CrossRef] [PubMed]
- Wagenmakers, R.; Van den Akker-Scheek, I.; Groothoff, J.W.; Zijlstra, W.; Bulstra, S.K.; Kootstra, J.W.J.; Wendel-Vos, W.; van Raaij, J.J.A.M.; Stevens, M. Reliability and validity of the short questionnaire to assess health-enhancing physical activty (SQUASH) in patients after total hip arthroplasty. BMC Muskuloskeletal Disord. 2008, 9. [Google Scholar] [CrossRef]
- Wendel-Vos, G.C.; Schuit, A.J.; Saris, W.H.; Kromhout, D. Reproducibility and relative validity of the short questionnaire to assess health-enhancing physical activity. J. Clin. Epidemiol. 2003, 56, 1163–1169. [Google Scholar] [CrossRef]
- Fishbein, M.; Ajzen, I. Predicting and Changing Behavior: The Reasoned Action Approach; Psychology Press: New York, NY, USA, 2010. [Google Scholar]
- Sheeran, P.; Orbell, S. Implementation intentions and repeated behaviour: Augmenting the predictive validity of the theory of planned behaviour. Eur. J. Soc. Psychol. 1999, 29, 349–369. [Google Scholar] [CrossRef]
- Van Stralen, M.M.; De Vries, H.; Bolman, C.; Mudde, A.N.; Lechner, L. Determinants of initiation and maintenance of physical activity in older adults: A literature review. Health Psychol. Rev. 2009, 3, 147–207. [Google Scholar] [CrossRef]
- Van Stralen, M.M.; de Vries, H.; Mudde, A.N.; Bolman, C.; Lechner, L. The long-term efficacy of two computer-tailored physical activity interventions for older adults: Main effects and mediators. Health Psychol. 2011, 30, 442–452. [Google Scholar] [CrossRef] [PubMed]
- Twisk, J.; de Boer, M.; de Vente, W.; Heymans, M. Multiple imputation of missing values was not necessary before performing a longitudinal mixed-model analysis. J. Clin. Epidemiol. 2013, 66, 1022–1028. [Google Scholar] [CrossRef] [PubMed]
- Morris, S.B.; DeShon, R.P. Combining effect size estimates in meta-analysis with repeated measures and independent-groups designs. Psychol. Methods 2002, 7, 105–125. [Google Scholar] [CrossRef] [PubMed]
- York University, D.O.P. Effect Size Calculator. Available online: http://www.yorku.ca/ncepeda/effectsize.html (accessed on 21 November 2017).
- University of Colorado Effect Size Calculator. Available online: https://www.uccs.edu/~lbecker/ (accessed on 21 October 2017).
- Cohen, J. A power primer. Psychol. Bull. 1992, 112, 155–159. [Google Scholar] [CrossRef] [PubMed]
- Gardner, B.; Smith, L.; Lorencatto, F.; Hamer, M.; Biddle, S.J.H. How to reduce sitting time? A review of behaviour change strategies used in sedentary behaviour reduction interventions among adults. Health Psychol. Rev. 2016, 10, 89–112. [Google Scholar] [CrossRef] [PubMed]
- Bankoski, A.; Harris, T.B.; McClain, J.J.; Brychta, R.J.; Caserotti, P.; Chen, K.Y.; Berrigan, D.; Troiano, R.P.; Koster, A. Sedentary activity associated with metabolic syndrome independent of physical activity. Diabetes Care 2011, 34, 497–503. [Google Scholar] [CrossRef] [PubMed]
- Van der Ploeg, H.P.; Chey, T.; Korda, R.J.; Banks, E.; Bauman, A. Sitting time and all-cause mortality risk in 222,497 Australian adults. Arch. Int. Med. 2012, 172, 494–500. [Google Scholar] [CrossRef] [PubMed]
- Duvivier, B.; Schaper, N.; Hesselink, M.; Kan, L.; Stienen, N.; Winkens, B.; Koster, A.; Savelberg, H. Breaking sitting with light activities vs. structured exercise: A randomised crossover study demonstrating benefits for glycaemic control and insulin sensitivity in type 2 diabetes. Diabetologia 2017, 60, 490–498. [Google Scholar] [CrossRef] [PubMed]
- Milton, K.; Clemes, S.; Bull, F. Can a single question provide an accurate measure of physical activity? Br. J. Med. 2013, 47, 44–48. [Google Scholar] [CrossRef] [PubMed]
- Wanner, M.; Probst-Hensch, N.; Kriemler, S.; Meier, F.; Bauman, A.; Martin, B.W. What physical activity surveillance needs: Validity of a single-item questionnaire. Br. J. Sports Med. 2014, 48, 1570–1576. [Google Scholar] [CrossRef] [PubMed]
- Greaves, C.J.; Sheppard, K.E.; Abraham, C.; Hardeman, W.; Roden, M.; Evans, P.H.; Schwarz, P. Systematic review of reviews of intervention components associated with increased effectiveness in dietary and physical activity interventions. BMC Public Health 2011, 11, 119–130. [Google Scholar] [CrossRef] [PubMed]
- Kwasnicka, D.; Dombrowski, S.U.; White, M.; Sniehotta, F. Theoretical explanations for maintenance of behaviour change: A systematic review of behaviour theories. Health Psychol. Rev. 2016, 10, 277–296. [Google Scholar] [CrossRef] [PubMed]
- Ory, M.G.; Smith, M.L.; Mier, N.; Wernicke, M.M. The science of sustaining health behavior change: The health maintenance consortium. Am. J. Health Behav. 2010, 34, 647–659. [Google Scholar] [CrossRef] [PubMed]
- Brouwer, W.B.F.; Kroeze, W.; Crutzen, R.; De Nooijer, J.; De Vries, N.; Brug, J.; Oenema, A. Which intervention characteristics are related to more exposure to internet-delivered healthy lifestyle promotion interventions? A systematic review. J. Med. Int. Res. 2011, 13. [Google Scholar] [CrossRef] [PubMed]
- Greaney, M.L.; Sprunck-Harrild, K.; Bennett, G.G.; Puleo, E.; Haines, J.; Viswanath, K.V.; Emmons, K.M. Use of email and telephone prompts to increase self-monitoring in a web-based intervention: Randomized controlled trial. J. Med. Int. Res. 2012, 14. [Google Scholar] [CrossRef] [PubMed]
- Schneider, F.; de Vries, H.; Candel, M.; van de Kar, A.; van Osch, L. Periodic email prompts to re-use an internet-delivered computer-tailored lifestyle program: Influence of prompt content and timing. J. Med. Int. Res. 2013, 15, 91–102. [Google Scholar] [CrossRef] [PubMed]
- Schneider, F.; van Osch, L.; Schulz, D.N.; Kremers, S.P.J.; de Vries, H. The influence of user characteristics and a periodic email prompt on exposure to an internet-delivered computer-tailored lifestyle program. J. Med. Int. Res. 2012, 14. [Google Scholar] [CrossRef] [PubMed]
- Chase, J.D. Interventions to increase physical activity among older adults: A meta-analysis. Gerontologist 2015, 55, 706–718. [Google Scholar] [CrossRef] [PubMed]
- Conn, V.S.; Hafdahl, A.R.; Brown, S.A.; Brown, L.M. Meta-analysis of patient education interventions to increase physical activity among chronically ill adults. Patient Educ. Couns. 2008, 70, 157–172. [Google Scholar] [CrossRef] [PubMed]
- Dishman, R.K.; Buckworth, J. Increasing physical activity: A quantitative synthesis. Med. Sci. Sports Exerc. 1996, 28, 706–719. [Google Scholar] [CrossRef] [PubMed]
- Eysenbach, G. The law of attrition. J. Med. Int. Res. 2005, 7. [Google Scholar] [CrossRef] [PubMed]
- Adams, K.B.; Leibbrandt, S.; Moon, H. A critical review of the literature on social and leisure activity and wellbeing in later life. Ageing Soc. 2011, 31, 683–712. [Google Scholar] [CrossRef]
- Brown, W.J.; Burton, N.W.; Marshall, A.L.; Miller, Y.D. Reliability and validity of a modified self-administered version of the active Australia physical activity survey in a sample of mid-age women. Aust. N. Z. J. Public Health 2008, 32, 535–541. [Google Scholar] [CrossRef] [PubMed]
- Webster, S.; Khan, A.; Nitz, J.C. A brief questionnaire is able to measure population physical activity levels accurately: A comparative validation study. J. Clin. Gerontol. Geriatr. 2011, 2, 83–87. [Google Scholar] [CrossRef]
- Harris, T.J.; Owen, C.G.; Victor, C.R.; Adams, R.; Ekelund, U.; Cook, D.G. A comparison of questionnaire, accelerometer, and pedometer: Measures in older people. Med. Sci. Sports Exerc. 2009, 41, 1392–1402. [Google Scholar] [CrossRef] [PubMed]
- European Union Digital Economy and Society Statistics: Households and Individuals. Available online: http://ec.europa.eu/eurostat/statistics-explained/index.php/Digital_economy_and_society_statistics_-_households_and_individuals (accessed on 3 May 2017).
| Variables | Active Plus65 | Reference Group | p-Value |
|---|---|---|---|
| (n = 416) | (n = 86) | ||
| Days per week with sufficient MVPA (mean ± SD) | 2.36 (2.31) | 3.46 (2.24) | <0.001 * |
| Weekly minutes of MVPA (mean ± SD) | 491.49 (±635.63) | 539.28 (±616.18) | 0.526 |
| Age (years) (mean ± SD) | 76.75 (±7.75) | 74.36 (±6.26) | 0.002 * |
| Gender (% male) | 35.6% | 22.4% | 0.018 * |
| Education (% low) | 67.4% | 62.8% | 0.413 |
| BMI (mean ± SD) | 27.3 (±5.05) | 26.8 (±5.0) | 0.390 |
| Way of entry (% online) | 41.1% | 30.2% | 0.060 |
| Degree of impairment (% very to extremely impaired) | 51.8% | 32.6% | 0.002 * |
| Intention to be physically active | 6.712 (±1.67) | 6.48 (±2.13) | 0.355 |
| Effects on Days per Week with Sufficient MVPA | B | SE | p | 95% CI | ES |
| T1 | −0.18 | 0.36 | 0.626 | −0.89/0.53 | 0.07 |
| T2 | 0.29 | 0.40 | 0.473 | −0.50/1.08 | 0.03 |
| Effects on Weekly Minutes of MVPA | B | SE | p | 95% CI | ES |
| T1 | 205.03 | 118.48 | 0.084 | −27.88/437.93 | 0.11 |
| T2 | 370.94 | 127.18 | 0.004 | 120.96/620.91 | 0.25 |
© 2018 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Boekhout, J.M.; Berendsen, B.A.J.; Peels, D.A.; Bolman, C.A.W.; Lechner, L. Evaluation of a Computer-Tailored Healthy Ageing Intervention to Promote Physical Activity among Single Older Adults with a Chronic Disease. Int. J. Environ. Res. Public Health 2018, 15, 346. https://doi.org/10.3390/ijerph15020346
Boekhout JM, Berendsen BAJ, Peels DA, Bolman CAW, Lechner L. Evaluation of a Computer-Tailored Healthy Ageing Intervention to Promote Physical Activity among Single Older Adults with a Chronic Disease. International Journal of Environmental Research and Public Health. 2018; 15(2):346. https://doi.org/10.3390/ijerph15020346
Chicago/Turabian StyleBoekhout, Janet M., Brenda A. J. Berendsen, Denise A. Peels, Catherine A. W. Bolman, and Lilian Lechner. 2018. "Evaluation of a Computer-Tailored Healthy Ageing Intervention to Promote Physical Activity among Single Older Adults with a Chronic Disease" International Journal of Environmental Research and Public Health 15, no. 2: 346. https://doi.org/10.3390/ijerph15020346
APA StyleBoekhout, J. M., Berendsen, B. A. J., Peels, D. A., Bolman, C. A. W., & Lechner, L. (2018). Evaluation of a Computer-Tailored Healthy Ageing Intervention to Promote Physical Activity among Single Older Adults with a Chronic Disease. International Journal of Environmental Research and Public Health, 15(2), 346. https://doi.org/10.3390/ijerph15020346







