Computer-Aided Surgical Simulation for Yaw Control of the Mandibular Condyle and Its Actual Application to Orthognathic Surgery: A One-Year Follow-Up Study
Abstract
1. Introduction
2. Materials and Methods
2.1. Patients
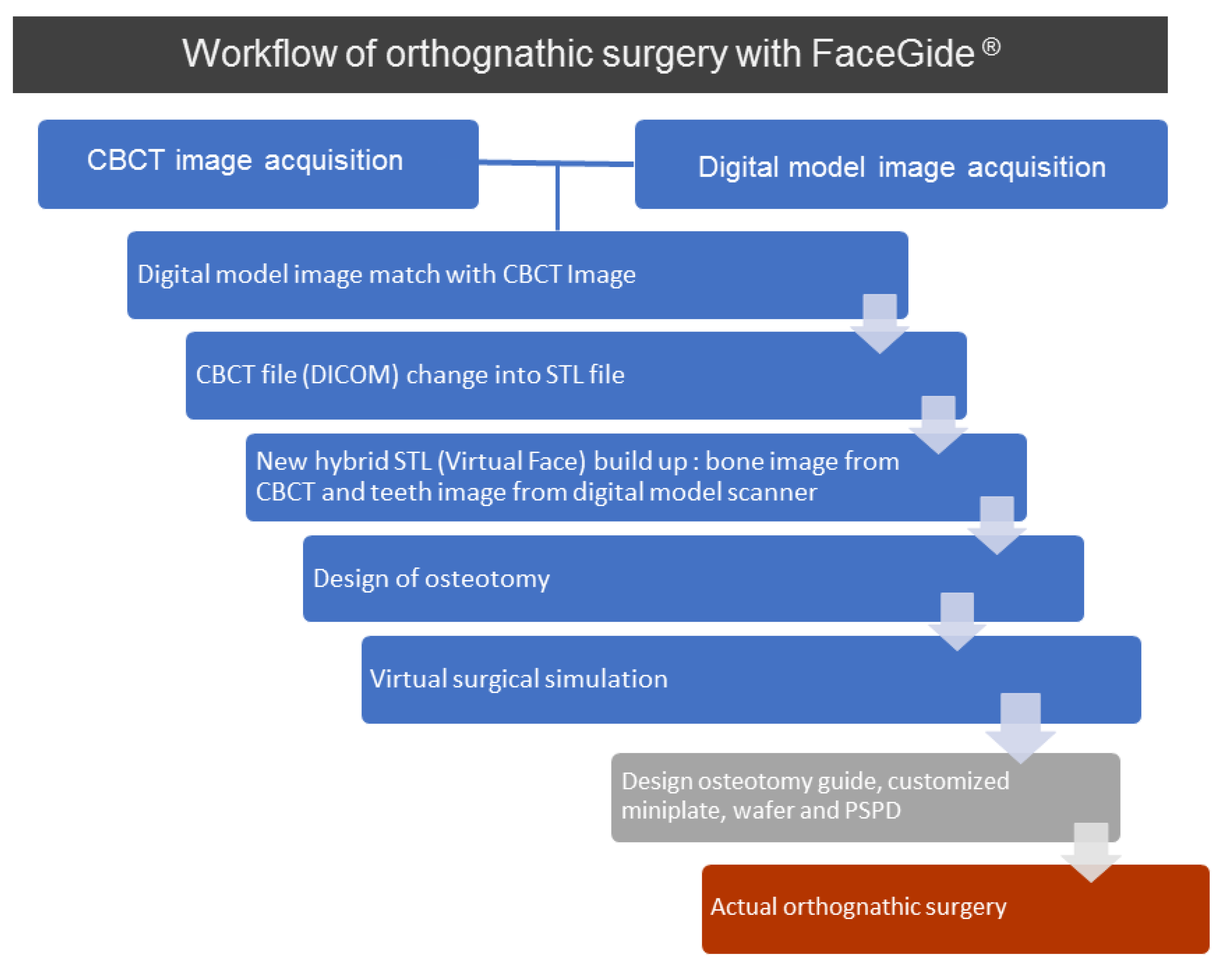
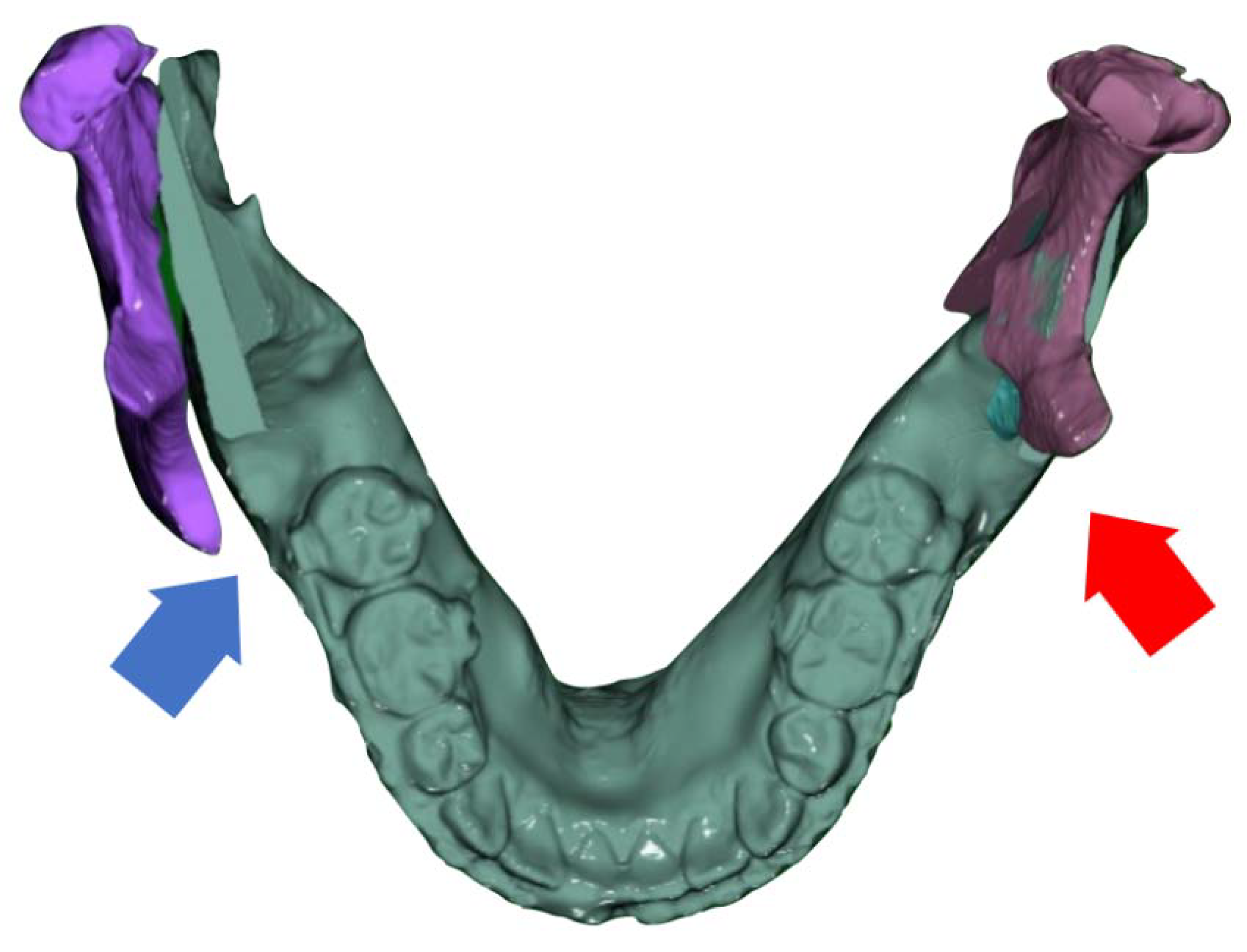
2.2. Virtual Surgery and Actual Surgery
2.3. Radiological Evaluation
2.4. Functional Evaluation
2.5. Statistics
3. Results
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Raffaini, M.; Pisani, C. Orthognathic surgery with or without autologous fat micrograft injection: Preliminary report on aesthetic outcomes and patient satisfaction. Int. J. Oral Maxillofac. Surg. 2015, 44, 362–370. [Google Scholar] [CrossRef] [PubMed]
- Arnett, G.W.; Gunson, M.J. Esthetic treatment planning for orthognathic surgery. J. Clin. Orthod. 2010, 44, 196–200. [Google Scholar] [PubMed]
- Yang, W.S. The study on the orthodontic patients who visited department of orthodontics, Seoul National University Hospital. J. Korean Dent. Assoc. 1990, 28, 811–821. [Google Scholar]
- Cheong, Y.W.; Lo, L.J. Facial asymmetry: Etiology, evaluation, and management. Chang Gung Med. J. 2011, 34, 341–351. [Google Scholar] [PubMed]
- Trauner, R.; Obwegeser, H. The surgical correction of mandibular prognathism and retrognathia with consideration of genioplasty. I. Surgical procedures to correct mandibular prognathism and reshaping of the chin. Oral Surg. Oral Med. Oral Pathol. 1957, 10, 677–689. [Google Scholar] [CrossRef]
- Lee, W.; Park, J.U. Three-dimensional evaluation of positional change of the condyle after mandibular setback by means of bilateral sagittal split ramus osteotomy. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. Endod. 2002, 94, 305–309. [Google Scholar] [CrossRef] [PubMed]
- Reyneke, J.P.; Bryant, R.S.; Suuronen, R.; Becker, P.J. Postoperative skeletal stability following clockwise and counter-clockwise rotation of the maxillomandibular complex compared to conventional orthognathic treatment. Br. J. Oral Maxillofac. Surg. 2007, 45, 56–64. [Google Scholar] [CrossRef] [PubMed]
- Shetty, V.; Freymiller, E.; McBrearty, D.; Caputo, A.A. Experimental analysis of functional stability of sagittal split ramus osteotomies secured by miniplates and position screws. J. Oral Maxillofac. Surg. Off. J. Am. Assoc. Oral Maxillofac. Surg. 1996, 54, 1317–1324, discussion 1324-1316. [Google Scholar] [CrossRef]
- Joss, C.U.; Vassalli, I.M. Stability after bilateral sagittal split osteotomy advancement surgery with rigid internal fixation: A systematic review. J. Oral Maxillofac. Surg. Off. J. Am. Assoc. Oral Maxillofac. Surg. 2009, 67, 301–313. [Google Scholar] [CrossRef] [PubMed]
- Freihofer, H.P., Jr.; Petresevic, D. Late results after advancing the mandible by sagittal splitting of the rami. J. Maxillofac. Surg. 1975, 3, 250–257. [Google Scholar] [CrossRef]
- Magalhaes, A.E.; Stella, J.P.; Tahasuri, T.H. Changes in condylar position following bilateral sagittal split ramus osteotomy with setback. Int. J. Adult Orthod. Orthognath. Surg. 1995, 10, 137–145. [Google Scholar]
- Hu, J.; Wang, D.; Zou, S. Effects of mandibular setback on the temporomandibular joint: A comparison of oblique and sagittal split ramus osteotomy. J. Oral Maxillofac. Surg. Off. J. Am. Assoc. Oral Maxillofac. Surg. 2000, 58, 375–380, discussion 380-371. [Google Scholar] [CrossRef]
- Epker, B.N.; Wylie, G.A. Control of the condylar-proximal mandibular segments after sagittal split osteotomies to advance the mandible. Oral Surg. Oral Med. Oral Pathol. 1986, 62, 613–617. [Google Scholar] [CrossRef]
- Ellis, E., 3rd. A method to passively align the sagittal ramus osteotomy segments. J. Oral Maxillofac. Surg. Off. J. Am. Assoc. Oral Maxillofac. Surg. 2007, 65, 2125–2130. [Google Scholar] [CrossRef] [PubMed]
- Angle, A.D.; Rebellato, J.; Sheats, R.D. Transverse displacement of the proximal segment after bilateral sagittal split osteotomy advancement and its effect on relapse. J. Oral Maxillofac. Surg. Off. J. Am. Assoc. Oral Maxillofac. Surg. 2007, 65, 50–59. [Google Scholar] [CrossRef] [PubMed]
- Bettega, G.; Dessenne, V.; Raphael, B.; Cinquin, P. Computer-assisted mandibular condyle positioning in orthognathic surgery. J. Oral Maxillofac. Surg. Off. J. Am. Assoc. Oral Maxillofac. Surg. 1996, 54, 553–558. [Google Scholar] [CrossRef]
- Ueki, K.; Degerliyurt, K.; Hashiba, Y.; Marukawa, K.; Nakagawa, K.; Yamamoto, E. Horizontal changes in the condylar head after sagittal split ramus osteotomy with bent plate fixation. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. Endod. 2008, 106, 656–661. [Google Scholar] [CrossRef] [PubMed]
- Kang, M.G.; Yun, K.I.; Kim, C.H.; Park, J.U. Postoperative condylar position by sagittal split ramus osteotomy with and without bone graft. J. Oral Maxillofac. Surg. Off. J. Am. Assoc. Oral Maxillofac. Surg. 2010, 68, 2058–2064. [Google Scholar] [CrossRef] [PubMed]
- Kim, M.J.; Kim, S.G.; Park, Y.W. Positional stability following intentional posterior ostectomy of the distal segment in bilateral sagittal split ramus osteotomy for correction of mandibular prognathism. J. Cranio-Maxillo-Facial Surg. Off. Publ. Eur. Assoc. Cranio-Maxillo-Facial Surg. 2002, 30, 35–40. [Google Scholar] [CrossRef] [PubMed]
- Hunsuck, E.E. A modified intraoral sagittal splitting technic for correction of mandibular prognathism. J. Oral Surg. (Am. Dent. Assoc. 1965) 1968, 26, 250–253. [Google Scholar]
- Wolford, L.M.; Bennett, M.A.; Rafferty, C.G. Modification of the mandibular ramus sagittal split osteotomy. Oral Surg. Oral Med. Oral Pathol. 1987, 64, 146–155. [Google Scholar] [CrossRef]
- Hackney, F.L.; Van Sickels, J.E.; Nummikoski, P.V. Condylar displacement and temporomandibular joint dysfunction following bilateral sagittal split osteotomy and rigid fixation. J. Oral Maxillofac. Surg. Off. J. Am. Assoc. Oral Maxillofac. Surg. 1989, 47, 223–227. [Google Scholar] [CrossRef]
- Politi, M.; Toro, C.; Costa, F.; Polini, F.; Robiony, M. Intraoperative awakening of the patient during orthognathic surgery: A method to prevent the condylar sag. J. Oral Maxillofac. Surg. Off. J. Am. Assoc. Oral Maxillofac. Surg. 2007, 65, 109–114. [Google Scholar] [CrossRef] [PubMed]
- Jacobs, R.; Salmon, B.; Codari, M.; Hassan, B.; Bornstein, M.M. Cone beam computed tomography in implant dentistry: Recommendations for clinical use. BMC Oral Health 2018, 18, 88. [Google Scholar] [CrossRef] [PubMed]
- Mangano, F.; Gandolfi, A.; Luongo, G.; Logozzo, S. Intraoral scanners in dentistry: A review of the current literature. BMC Oral Health 2017, 17, 149. [Google Scholar] [CrossRef] [PubMed]
- Mangano, C.; Luongo, F.; Migliario, M.; Mortellaro, C.; Mangano, F.G. Combining Intraoral Scans, Cone Beam Computed Tomography and Face Scans: The Virtual Patient. J. Craniofacial Surg. 2018. [Google Scholar] [CrossRef] [PubMed]
- Colombo, M.; Mangano, C.; Mijiritsky, E.; Krebs, M.; Hauschild, U.; Fortin, T. Clinical applications and effectiveness of guided implant surgery: A critical review based on randomized controlled trials. BMC Oral Health 2017, 17, 150. [Google Scholar] [CrossRef] [PubMed]
- Joda, T.; Zarone, F.; Ferrari, M. The complete digital workflow in fixed prosthodontics: A systematic review. BMC Oral Health 2017, 17, 124. [Google Scholar] [CrossRef] [PubMed]
- Mangano, F.; Veronesi, G. Digital versus Analog Procedures for the Prosthetic Restoration of Single Implants: A Randomized Controlled Trial with 1 Year of Follow-Up. BioMed Res. Int. 2018, 2018, 5325032. [Google Scholar] [CrossRef] [PubMed]
- Ackerman, J.L.; Proffit, W.R.; Sarver, D.M.; Ackerman, M.B.; Kean, M.R. Pitch, roll, and yaw: Describing the spatial orientation of dentofacial traits. Am. J. Orthod. Dentofac. Orthop. 2007, 131, 305–310. [Google Scholar] [CrossRef] [PubMed]
- Lonic, D.; Lo, L.-J. Three-dimensional simulation of orthognathic surgery-surgeon’s perspective. J. Formos. Med. Assoc. 2016, 115, 387–388. [Google Scholar] [CrossRef] [PubMed]
- Baek, S.H.; Kim, T.K.; Kim, M.J. Is there any difference in the condylar position and angulation after asymmetric mandibular setback? Oral Surg. Oral Med. Oral Pathol. Oral Radiol. Endod. 2006, 101, 155–163. [Google Scholar] [CrossRef] [PubMed]
- Obwegeser, H. The Indications for Surgical Correction of Mandibular Deformity by the Sagittal Splitting Technique. Br. J. Oral Surg. 1964, 1, 157–171. [Google Scholar] [CrossRef]
- Epker, B.N. Modifications in the sagittal osteotomy of the mandible. J. Oral Surg. (Am. Dent. Assoc. 1965) 1977, 35, 157–159. [Google Scholar]
- Ghang, M.H.; Kim, H.M.; You, J.Y.; Kim, B.H.; Choi, J.P.; Kim, S.H.; Choung, P.H. Three-dimensional mandibular change after sagittal split ramus osteotomy with a semirigid sliding plate system for fixation of a mandibular setback surgery. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. 2013, 115, 157–166. [Google Scholar] [CrossRef] [PubMed]
- Kim, Y.I.; Jung, Y.H.; Cho, B.H.; Kim, J.R.; Kim, S.S.; Son, W.S.; Park, S.B. The assessment of the short- and long-term changes in the condylar position following sagittal split ramus osteotomy (SSRO) with rigid fixation. J. Oral Rehabilit. 2010, 37, 262–270. [Google Scholar] [CrossRef] [PubMed]
- Bamber, M.A.; Abang, Z.; Ng, W.F.; Harris, M.; Linney, A. The effect of posture and anesthesia on the occlusal relationship in orthognathic surgery. J. Oral Maxillofac. Surg. Off. J. Am. Assoc. Oral Maxillofac. Surg. 1999, 57, 1164–1172, discussion 1172-1164. [Google Scholar] [CrossRef]
- Jakobsone, G.; Stenvik, A.; Sandvik, L.; Espeland, L. Three-year follow-up of bimaxillary surgery to correct skeletal Class III malocclusion: Stability and risk factors for relapse. Am. J. Orthod. Dentofac. Orthop. Off. Publ. Am. Assoc. Orthod. Const. Soc. Am. Board Orthod. 2011, 139, 80–89. [Google Scholar] [CrossRef] [PubMed]
- Mucedero, M.; Coviello, A.; Baccetti, T.; Franchi, L.; Cozza, P. Stability factors after double-jaw surgery in Class III malocclusion. A systematic review. Angle Orthod. 2008, 78, 1141–1152. [Google Scholar] [CrossRef] [PubMed]
- Costa, F.; Robiony, M.; Zorzan, E.; Zerman, N.; Politi, M. Stability of skeletal Class III malocclusion after combined maxillary and mandibular procedures: Titanium versus resorbable plates and screws for maxillary fixation. J. Oral Maxillofac. Surg. Off. J. Am. Assoc. Oral Maxillofac. Surg. 2006, 64, 642–651. [Google Scholar] [CrossRef] [PubMed]
- Cho, H.J. Long-term stability of surgical mandibular setback. Angle Orthod. 2007, 77, 851–856. [Google Scholar] [CrossRef] [PubMed]
- Yang, H.J.; Hwang, S.J. Change in condylar position in posterior bending osteotomy minimizing condylar torque in BSSRO for facial asymmetry. J. Cranio-Maxillo-Facial Surg. Off. Publ. Eur. Assoc. Cranio-Maxillo-Facial Surg. 2014, 42, 325–332. [Google Scholar] [CrossRef] [PubMed]
- Yang, H.J.; Lee, W.J.; Yi, W.J.; Hwang, S.J. Interferences between mandibular proximal and distal segments in orthognathic surgery for patients with asymmetric mandibular prognathism depending on different osteotomy techniques. Oral Surg. Oral Med. Oral Pathol. Oral radiol. Endod. 2010, 110, 18–24. [Google Scholar] [CrossRef] [PubMed]
- Ellis, E. Condylar positioning devices for orthognathic surgery: Are they necessary? J. Oral Maxillofac. Surg. 1994, 52, 536–552. [Google Scholar] [CrossRef]
- Dawson, P. Functional Occlusion: From TMJ to Smile Design; CV Mosby: St. Louis, MO, USA, 2007; p. 35. [Google Scholar]
- Rotskoff, K.S.; Herbosa, E.G.; Villa, P. Maintenance of condyle-proximal segment position in orthognathic surgery. J. Oral Maxillofac. Surg. 1991, 49, 2–7. [Google Scholar] [CrossRef]
- Xi, T.; de Koning, M.; Berge, S.; Hoppenreijs, T.; Maal, T. The role of mandibular proximal segment rotations on skeletal relapse and condylar remodelling following bilateral sagittal split advancement osteotomies. J. Cranio-Maxillo-Facial Surg. Off. Publ. Eur. Assoc. Cranio-Maxillo-Facial Surg. 2015, 43, 1716–1722. [Google Scholar] [CrossRef] [PubMed]
- Lindauer, S.J.; Sabol, G.; Isaacson, R.J.; Davidovitch, M. Condylar movement and mandibular rotation during jaw opening. Am. J. Orthod. Dentofac. Orthop. 1995, 107, 573–577. [Google Scholar] [CrossRef]
- Hadjidakis, D.J.; Androulakis, I.I. Bone remodeling. Ann. N. Y. Acad. Sci. 2006, 1092, 385–396. [Google Scholar] [CrossRef] [PubMed]
- Nishimura, A.; Sakurada, S.; Iwase, M.; Nagumo, M. Positional changes in the mandibular condyle and amount of mouth opening after sagittal split ramus osteotomy with rigid or nonrigidosteosynthesis. J. Oral Maxillofac. Surg. Off. J. Am. Assoc. Oral Maxillofac. Surg. 1997, 55, 672–676, discussion 677-678. [Google Scholar] [CrossRef]
- Trapozzano, V.R.; Lazzari, J.B. The physiology of the terminal rotational position of the condyles in the temporomandibular joint. J. Prosthet. Dent. 1967, 17, 122–133. [Google Scholar] [CrossRef]
- Serrano, P.; Nicholls, J.; Yuodelis, R. Centric relation change during therapy with corrective occlusion prostheses. J. Prosthet. Dent. 1984, 51, 97–105. [Google Scholar] [CrossRef]






| T0 | Tv | T1 | T2 | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| n = 40 | n = 40 | n = 40 | n = 40 | ||||||||||
| Average | SD | Average | SD | Average | SD | Average | SD | df | F | p(1) | B (2) | ||
| AJS | mm | 1.92 | 0.7 | 1.89 | 0.7 | 2.6 | 0.79 | 2.07 | 0.63 | 1.72 | 25.44 | 0.00 * | T1 > T0, Tv, T2 |
| SJS | mm | 2.48 | 1.06 | 2.25 | 0.86 | 3.48 | 1.12 | 2.51 | 0.9 | 1.79 | 33.75 | 0.00 * | T1 > T0, Tv, T2 |
| T2 >Tv | |||||||||||||
| PJS | mm | 2.07 | 0.93 | 2.04 | 0.91 | 2.67 | 1.01 | 2.09 | 0.68 | 1.48 | 11.78 | 0.00 * | T1 > T0, Tv, T2 |
| MJS | mm | 2.28 | 1.09 | 2.46 | 0.91 | 3.37 | 1.07 | 2.25 | 0.7 | 2.27 | 39.35 | 0.00 * | T1 > T0, Tv, T2 |
| Tv > T2 | |||||||||||||
| LJS | mm | 1.95 | 0.82 | 1.82 | 0.56 | 2.6 | 1.25 | 2.08 | 0.58 | 1.61 | 14.21 | 0.00 * | T1 > T0, Tv, T2 |
| T2 > Tv | |||||||||||||
| angle | degree | 71.64 | 6.66 | 69.03 | 7.65 | 67.93 | 7.44 | 71.98 | 6.22 | 1.49 | 15.82 | 0.00 * | T2 > Tv, T1 |
| T0 > Tv, T1 | |||||||||||||
| Tv > T1 | |||||||||||||
© 2018 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kim, J.-W.; Kim, J.-C.; Cheon, K.-J.; Cho, S.-W.; Kim, Y.-H.; Yang, B.-E. Computer-Aided Surgical Simulation for Yaw Control of the Mandibular Condyle and Its Actual Application to Orthognathic Surgery: A One-Year Follow-Up Study. Int. J. Environ. Res. Public Health 2018, 15, 2380. https://doi.org/10.3390/ijerph15112380
Kim J-W, Kim J-C, Cheon K-J, Cho S-W, Kim Y-H, Yang B-E. Computer-Aided Surgical Simulation for Yaw Control of the Mandibular Condyle and Its Actual Application to Orthognathic Surgery: A One-Year Follow-Up Study. International Journal of Environmental Research and Public Health. 2018; 15(11):2380. https://doi.org/10.3390/ijerph15112380
Chicago/Turabian StyleKim, Ju-Won, Jong-Cheol Kim, Kyeong-Jun Cheon, Seoung-Won Cho, Young-Hee Kim, and Byoung-Eun Yang. 2018. "Computer-Aided Surgical Simulation for Yaw Control of the Mandibular Condyle and Its Actual Application to Orthognathic Surgery: A One-Year Follow-Up Study" International Journal of Environmental Research and Public Health 15, no. 11: 2380. https://doi.org/10.3390/ijerph15112380
APA StyleKim, J.-W., Kim, J.-C., Cheon, K.-J., Cho, S.-W., Kim, Y.-H., & Yang, B.-E. (2018). Computer-Aided Surgical Simulation for Yaw Control of the Mandibular Condyle and Its Actual Application to Orthognathic Surgery: A One-Year Follow-Up Study. International Journal of Environmental Research and Public Health, 15(11), 2380. https://doi.org/10.3390/ijerph15112380





