Assessment of Dietary Mercury Intake and Blood Mercury Levels in the Korean Population: Results from the Korean National Environmental Health Survey 2012–2014
Abstract
:1. Introduction
2. Materials and Methods
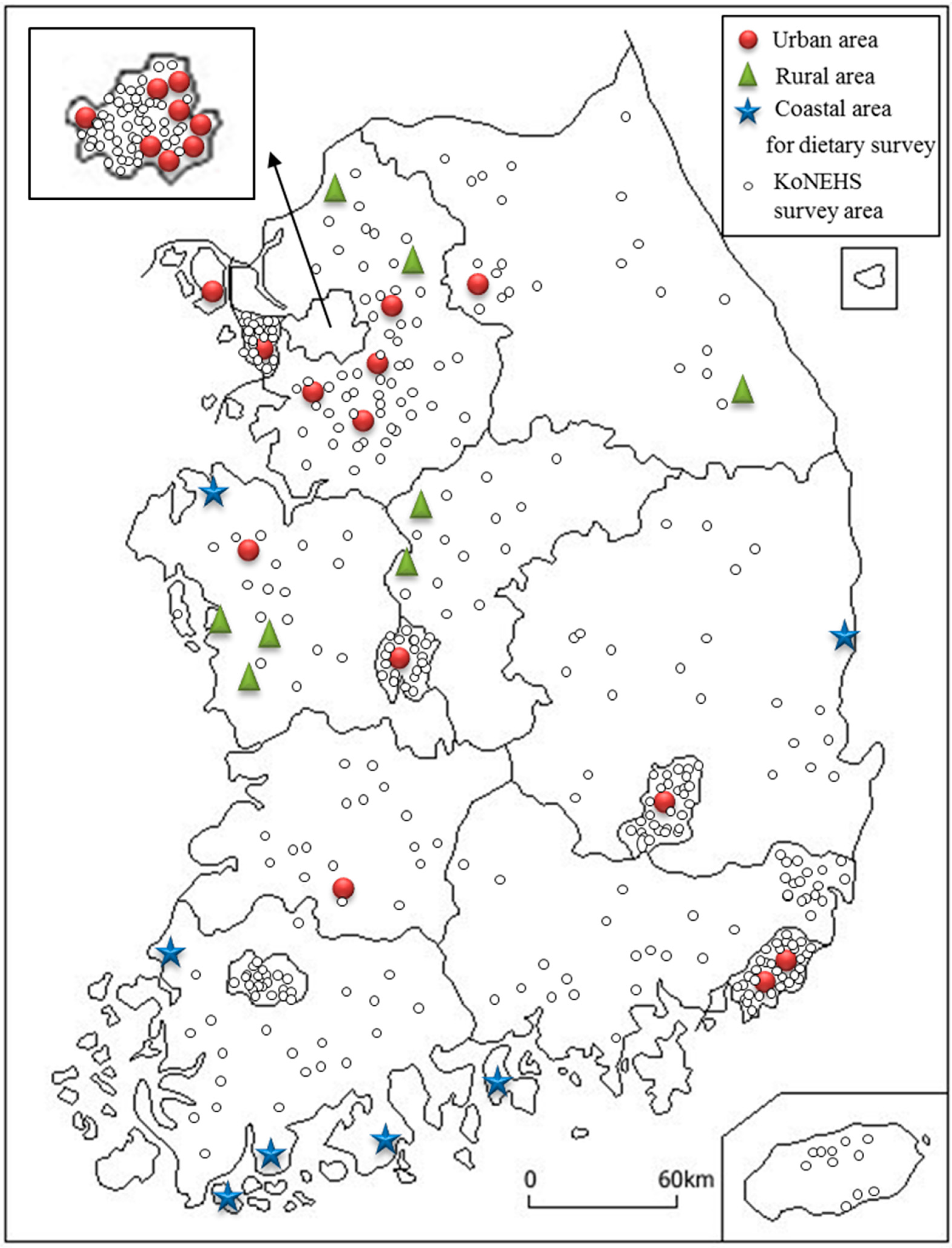
2.1. Study Design and Subjects
2.2. Dietary Mercury Exposure
2.3. Risk Assessment of Dietary Mercury Exposure of Koreans
2.4. Measurement of the Blood Mercury Concentration
2.5. Statistical Analysis
3. Results
3.1. General Characteristics of the Study Subjects
3.2. Daily Total and Methylmercury Intakes
3.3. The Blood Mercury Concentration
3.4. The Association between the Dietary Mercury Intake and the Blood Mercury Level
3.5. Contribution of Different Food Groups to Mercury Intake
3.6. The Dose–Response Relationship between Seafood Intake and Blood Mercury Concentration
4. Discussion
5. Conclusions
Acknowledgments
Author Contributions
Conflicts of Interest
References
- WHO (World Health Organization). Exposure to Mercury: A Major Public Health Concern; Public Health and Environment: Geneva, Switzerland, 2007; Available online: http://www.who.int/phe/news/Mercury-flyer.pdf (accessed on 4 June 2013).
- EPA (Environmental Protection Agency). Office of Air Quality Planning & Standards and Office of Research and Development; Mercury Study Report to Congress: Washington, DC, USA, 1997; Volume 1. Available online: http://www.epa.gov/ttn/caaa/t3/reports/volume1.pdf (accessed on 4 June 2013).
- Mergler, D.; Anderson, H.A.; Chan, L.H.M.; Mahaffey, K.R.; Murray, M.; Sakamoto, M.; Stern, A.H. Methylmercury exposure and health effects in humans: A worldwide concern. AMBIO 2007, 36, 3–11. [Google Scholar] [CrossRef]
- Brown, I.A.; Austin, D.W. Maternal transfer of mercury to the developing embryo/fetus: Is there a safe level? Toxicol. Environ. Chem. 2012, 94, 1610–1627. [Google Scholar] [CrossRef]
- Clarkson, T.W. Mercury: Major issues in environmental health. Environ. Health Perspect. 1993, 100, 31–38. [Google Scholar] [CrossRef] [PubMed]
- Agency for Toxic Substances and Disease Registry. Toxicological Profile for Mercury; 1999. Available online: http://stacks.cdc.gov/view/cdc/6476/Print (accessed on 4 June 2013).
- WHO (World Health Organization). Methyl Mercury; World Health Organization, International Programme on Chemical Safety: Geneva, Switzerland, 1990; Volume 101. [Google Scholar]
- CDC (Centers for Disease Control and Prevention). National Biomonitoring Program Homepage. Available online: http://www.cdc.gov/biomonitoring/index.html (accessed on 20 December 2014).
- Statistics Canada. Canadian Health Measures Survey. Available online: http://www23.statcan.gc.ca/imdb/p2SV.pl?Function=getSurvey&SDDS=5071 (accessed on 20 December 2014).
- Umweltbundesamt. German Environmental Survey Homepage. Available online: http://www.umweltbundesamt.de/en/topics/health/assessing-environmentally-related-health-risks/german-environmental-surveys/german-environmental-survey-2014-2017-geres-v (accessed on 20 December 2014).
- Korea Rural Economic Institute. 2013 Food Balance Sheet. Available online: https://www.krei.re.kr/web/www/23?p_p_id=EXT_BBS&p_p_lifecycle=0&p_p_state=normal&p_p_mode=view&_EXT_BBS_struts_action=%2Fext%2Fbbs%2Fview_message&_EXT_BBS_messageId=404443 (accessed on 20 April 2016).
- Thompson, F.E.; Subar, A.F. Dietary assessment methodology. In Nutrition in the Prevention and Treatment of Diseases; Coulston, A.M., Rock, C.L., Monsen, E.R., Eds.; Academic Press: San Diego, CA, USA, 2001; pp. 3–30. [Google Scholar]
- Hoffmann, K.; Boeing, H.; Dufour, A.; Volatier, J.; Telman, J.; Virtanen, M.; Becker, W.; De Henauw, S.; EFCOSUM Group. Estimating the distribution of usual dietary intake by short-term measurements. Eur. J. Clin. Nutr. 2002, 56, S53–S62. [Google Scholar] [CrossRef] [PubMed]
- Tian, W.; Egeland, G.M.; Sobol, I.; Chan, H.M. Mercury hair concentrations and dietary exposure among Inuit preschool children in Nunavut, Canada. Environ. Int. 2011, 37, 42–48. [Google Scholar] [CrossRef] [PubMed]
- Bjermo, H.; Sand, S.; Nälsén, C.; Lundh, T.; Barbieri, E.H.; Pearson, M.; Lindroos, A.K.; Jönsson, B.A.; Barregård, L.; Darnerud, P.O. Lead, mercury, and cadmium in blood and their relation to diet among Swedish adults. Food Chem. Toxicol. 2013, 57, 161–169. [Google Scholar] [CrossRef] [PubMed]
- Gonzalez-Munoz, M.; Pena, A.; Meseguer, I. Monitoring heavy metal contents in food and hair in a sample of young Spanish subjects. Food Chem. Toxicol. 2008, 46, 3048–3052. [Google Scholar] [CrossRef] [PubMed]
- Den Hond, E.; Govarts, E.; Willems, H.; Smolders, R.; Casteleyn, L.; Kolossa-Gehring, M.; Schwedler, G.; Seiwert, M.; Fiddicke, U.; Castaño, A. First steps toward harmonized human biomonitoring in Europe: Demonstration project to perform human biomonitoring on a European scale. Environ. Health Perspect. 2015, 123, 255–263. [Google Scholar] [CrossRef] [PubMed]
- Son, J.Y.; Lee, J.; Paek, D.; Lee, J.T. Blood levels of lead, cadmium, and mercury in the Korean population: Results from the Second Korean National Human Exposure and Bio-monitoring Examination. Environ. Res. 2009, 109, 738–744. [Google Scholar] [CrossRef] [PubMed]
- Park, S.; Lee, B.K. Strong positive associations between seafood, vegetables, and alcohol with blood mercury and urinary arsenic levels in the Korean adult population. Arch. Environ. Contam. Toxicol. 2013, 64, 160–170. [Google Scholar] [CrossRef] [PubMed]
- Thompson, F.E.; Byers, T. Dietary assessment resource manual. J. Nutr. 1994, 124, 2245s–2317s. [Google Scholar] [PubMed]
- Kim, S.A.; Shin, S.; Lee, J.W.; Joung, H. Development of a mercury database for commonly consumed by Koreans. J. Nutr. Health 2014, 47, 364–373. [Google Scholar] [CrossRef]
- WHO (World Health Organization). Summary Report of the Seventy-Second Meeting of JECFA; Joint FAO/WHO Expert Committee on Food Additives (JECFA): Rome, Italy, 2010. Available online: http://www.who.int/foodsafety/chem/summary72 rev.pdf (accessed on 4 June 2013).
- Noisel, N.; Bouchard, M.; Carrier, G.; Plante, M. Comparison of a toxicokinetic and a questionnaire-based approach to assess methylmercury intake in exposed individuals. J. Expo. Sci. Environ. Epidemiol. 2010, 21, 328–335. [Google Scholar] [CrossRef] [PubMed]
- Schulz, C.; Wilhelm, M.; Heudorf, U.; Kolossa-Gehring, M. Update of the reference and HBM values derived by the German Human Biomonitoring Commission. Int. J. Hyg. Environ. Health 2011, 215, 26–35. [Google Scholar] [CrossRef] [PubMed]
- Ministry of Health and Welfare. Dietary Reference Intakes for Koreans 2015; Korea Ministry of Health and Welfare: Sejong, Korea, 2015.
- Becker, K.; Kaus, S.; Krause, C.; Lepom, P.; Schulz, C.; Seiwert, M.; Seifert, B. German Environmental Survey 1998 (GerES III): Environmental pollutants in blood of the German population. Int. J. Hyg. Environ. Health 2002, 205, 297–308. [Google Scholar] [CrossRef] [PubMed]
- Caldwell, K.L.; Mortensen, M.E.; Jones, R.L.; Caudill, S.P.; Osterloh, J.D. Total blood mercury concentrations in the US population: 1999–2006. Int. J. Hyg. Environ. Health 2009, 212, 588–598. [Google Scholar] [CrossRef] [PubMed]
- CDC (Centers for Disease Control and Prevention). Biomonitoring Summary: Mercury. Available online: http://www.cdc.gov/biomonitoring/Mercury_BiomonitoringSummary.html (accessed on 20 January 2015).
- Sherlock, J.; Hislop, J.; Newton, D.; Topping, G.; Whittle, K. Elevation of mercury in human blood from controlled chronic ingestion of methylmercury in fish. Hum. Toxicol. 1984, 3, 117–131. [Google Scholar] [CrossRef] [PubMed]
- Swanson, D.; Block, R.; Mousa, S.A. Omega-3 fatty acids EPA and DHA: Health benefits throughout life. Adv. Nutr. 2012, 3, 1–7. [Google Scholar] [CrossRef] [PubMed]
- Neff, L.M.; Culiner, J.; Cunningham-Rundles, S.; Seidman, C.; Meehan, D.; Maturi, J.; Wittkowski, K.M.; Levine, B.; Breslow, J.L. Algal docosahexaenoic acid affects plasma lipoprotein particle size distribution in overweight and obese adults. J. Nutr. 2011, 141, 207–213. [Google Scholar] [CrossRef] [PubMed]
- Ganther, H.E. Modification of methylmercury toxicity and metabolism by selenium and vitamin E: Possible mechanisms. Environ. Health Perspect. 1978, 25, 71–76. [Google Scholar] [CrossRef] [PubMed]
- Barrett, J.R. Rice is a significant source of methylmercury: Research in China assesses exposures. Environ. Health Perspect. 2010, 118, a398. [Google Scholar] [CrossRef] [PubMed]
- Korea Ministry of Food and Drug Safety. Dietary Intake and Risk Assessment of Contaminants in Korean Foods; Korea Ministry of Food and Drug Safety: Seoul, Korea, 2009.
- Martin, M.; Naleway, C. The inhibition of mercury absorption by dietary ethanol in humans: Cross-sectional and case-control studies. Occup. Environ. Med. 2004, 61, e8. [Google Scholar] [CrossRef] [PubMed]
- Krishnan, E.; Sokka, T.; Hannonen, P. Smoking-gender interaction and risk for rheumatoid arthritis. Arthritis Res. Ther. 2003, 5, R158–R162. [Google Scholar] [CrossRef] [PubMed]
- Al-Shahristani, H.; Shihab, K.M. Variation of biological half-life of methylmercury in man. Arch. Environ. Health 1974, 28, 342–344. [Google Scholar] [CrossRef] [PubMed]
- Oskarsson, A.; Schütz, A.; Skerfving, S.; Hallén, I.P.; Ohlin, B.; Lagerkvist, B.J. Total and inorganic mercury in breast milk and blood in relation to fish consumption and amalgam fillings in lactating women. Arch. Environ. Health 1996, 51, 234–241. [Google Scholar] [CrossRef] [PubMed]
| Variables | Total | Male | Female | p Value 1 | |||
|---|---|---|---|---|---|---|---|
| n | % | n | % | n | % | ||
| Age (years) | |||||||
| 20–29 | 37 | 6.69 | 16 | 6.64 | 21 | 6.73 | NS |
| 30–39 | 87 | 15.73 | 41 | 17.01 | 46 | 14.74 | |
| 40–49 | 115 | 20.80 | 41 | 17.01 | 74 | 23.72 | |
| 50–59 | 117 | 21.16 | 58 | 24.07 | 59 | 18.91 | |
| 60–69 | 122 | 22.06 | 52 | 21.58 | 70 | 22.44 | |
| ≥70 | 75 | 13.56 | 33 | 13.69 | 42 | 13.46 | |
| Residence 2 | |||||||
| Urban area | 317 | 57.32 | 135 | 56.02 | 182 | 58.33 | NS |
| Rural area | 125 | 22.60 | 57 | 23.65 | 68 | 21.79 | |
| Coastal area | 111 | 20.07 | 49 | 20.33 | 62 | 19.87 | |
| Obesity 3 | |||||||
| Underweight | 10 | 1.81 | 3 | 1.24 | 7 | 2.24 | NS |
| Normal | 328 | 59.31 | 135 | 56.02 | 193 | 61.86 | |
| Obese | 215 | 38.88 | 103 | 42.74 | 112 | 35.90 | |
| Smoking status 4 | |||||||
| Current smoker | 106 | 19.17 | 92 | 38.17 | 14 | 4.49 | <0.001 |
| Ex-smoker | 89 | 16.09 | 85 | 35.27 | 4 | 1.28 | |
| Non-smoker | 358 | 64.74 | 64 | 26.56 | 294 | 94.23 | |
| Alcohol drinking status 5 | |||||||
| Current drinker | 325 | 58.77 | 181 | 75.10 | 144 | 46.15 | <0.001 |
| Ex-drinker | 31 | 5.61 | 25 | 10.37 | 6 | 1.92 | |
| Non-drinker | 197 | 35.62 | 35 | 14.52 | 162 | 51.92 | |
| Total | 553 | 241 | 43.58 | 312 | 56.42 | ||
| Total Mercury Intake (μg/day) | % PTDI for Inorganic Mercury 1 | Methylmercury Intake from Fish and Shellfish (μg/day) 2 | % PTDI for Methylmercury 3 | % PTDI ≥ 100% for Inorganic Mercury | % PTDI ≥ 100% for Methylmercury | ||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| n | Mean ± SD | Mean ± SD | Mean ± SD | Mean ± SD | n | % | p Value 4 | n | % | p Value 4 | |
| Sex | |||||||||||
| Male | 241 | 4.74 ± 6.83 a | 12.03 ± 17.44 a | 3.72 ± 6.60 a | 23.67 ± 41.99 a | 1 | 0.41 | NS | 10 | 4.15 | NS |
| Female | 312 | 3.07 ± 3.43 b | 9.16 ± 9.67 b | 2.19 ± 3.29 b | 16.27 ± 23.11 b | 0 | 0.00 | 6 | 1.92 | ||
| Age (years) | |||||||||||
| 20–29 | 37 | 2.33 ± 2.08 a | 6.74 ± 7.18 a | 1.62 ± 2.02 a | 12.04 ± 17.14 a | 0 | 0.00 | NS | 0 | 0.00 | NS |
| 30–39 | 87 | 3.26 ± 2.69 a | 8.51 ± 6.92 a | 2.35 ± 2.51 a | 15.19 ± 16.23 a | 0 | 0.00 | 0 | 0.00 | ||
| 40–49 | 115 | 3.70 ± 4.45 a,b | 10.09 ± 12.30 a,b | 2.75 ± 4.29 a,b | 18.74 ± 29.56 a,b | 0 | 0.00 | 5 | 4.35 | ||
| 50–59 | 117 | 4.13 ± 4.12 a,b | 11.31 ± 11.34 a,b | 3.12 ± 3.95 a,b | 21.33 ± 27.19 a,b | 0 | 0.00 | 4 | 3.42 | ||
| 60–69 | 122 | 3.59 ± 4.68 a,b | 10.22 ± 12.73 a,b | 2.63 ± 4.50 a,b | 18.68 ± 30.57 a,b | 0 | 0.00 | 3 | 2.46 | ||
| ≥70 | 75 | 5.11 ± 9.97 b | 13.86 ± 24.28 b | 4.16 ± 9.63 b | 27.80 ± 58.78 b | 1 | 1.33 | 4 | 5.33 | ||
| Residence 5 | |||||||||||
| Urban area | 317 | 3.12 ± 3.20 a | 8.57 ± 8.74 a | 2.20 ± 3.05 a | 15.08 ± 20.81 a | 0 | 0.00 | NS | 4 | 1.26 | 0.012 |
| Rural area | 125 | 3.53 ± 4.09 a | 9.75 ± 11.37 a | 2.55 ± 3.93 a | 17.49 ± 27.32 a | 0 | 0.00 | 5 | 4.00 | ||
| Coastal area | 111 | 6.04 ± 9.17 b | 16.43 ± 22.94 b | 5.08 ± 8.83 b | 34.37 ± 55.28 b | 1 | 0.90 | 7 | 6.31 | ||
| Obesity 6 | |||||||||||
| Underweight | 10 | 2.67 ± 2.17 | 10.49 ± 8.47 | 2.02 ± 2.12 | 19.79 ± 20.72 | 0 | 0.00 | NS | 0 | 0.00 | NS |
| Normal | 328 | 3.64 ± 4.06 | 10.79 ± 12.03 | 2.71 ± 3.89 | 20.03 ± 28.84 | 0 | 0.00 | 12 | 3.66 | ||
| Obese | 215 | 4.09 ± 6.77 | 9.84 ± 16.05 | 3.12 ± 6.53 | 18.66 ± 38.70 | 1 | 0.47 | 4 | 1.86 | ||
| Smoking status 7 | |||||||||||
| Current smoker | 106 | 4.50 ± 4.73 a | 11.84 ± 13.80 a,b | 3.55 ± 4.56 a | 23.49 ± 33.11 a,b | 0 | 0.00 | NS | 6 | 5.66 | 0.002 |
| Ex-smoker | 89 | 5.82 ± 9.94 b | 14.78 ± 24.68 a | 4.76 ± 9.61 a | 30.21 ± 59.59 a | 1 | 1.12 | 6 | 6.74 | ||
| Non-smoker | 358 | 3.09 ± 3.19 c | 8.91 ± 8.67 b | 2.18 ± 3.03 b | 15.65 ± 20.63 b | 0 | 0.00 | 4 | 1.12 | ||
| Alcohol drinking status 8 | |||||||||||
| Current drinker | 325 | 4.18 ± 6.19 | 10.97 ± 15.50 | 3.23 ± 5.97 | 21.07 ± 37.36 | 0 | 0.00 | NS | 10 | 3.08 | NS |
| Ex-drinker | 31 | 3.95 ± 3.85 | 9.92 ± 9.59 | 2.95 ± 3.63 | 18.55 ± 22.52 | 0 | 0.00 | 1 | 3.23 | ||
| Non-drinker | 197 | 3.15 ± 3.40 | 9.57 ± 10.68 | 2.23 ± 3.26 | 17.05 ± 25.49 | 1 | 0.31 | 5 | 2.54 | ||
| Total | 553 | 3.80 ± 5.26 | 10.41 ± 13.67 | 2.86 ± 5.06 | 19.50 ± 32.88 | 1 | 0.18 | 16 | 2.89 | ||
| Blood Mercury (μg/L) 1 | Blood Mercury ≥ 5 μg/L 2 | ||||
|---|---|---|---|---|---|
| GM (95% CI) | p Value 3 | n | % | p Value 4 | |
| Sex | |||||
| Male | 3.92 (3.64–4.23) | <0.001 | 79 | 32.92 | <0.001 |
| Female | 2.61 (2.46–2.77) | 29 | 9.32 | ||
| Age (years) | |||||
| 20–29 | 2.56 (2.18–3.00) | NS | 4 | 10.81 | NS |
| 30–39 | 2.87 (2.54–3.25) | 15 | 17.24 | ||
| 40–49 | 3.14 (2.86–3.44) | 20 | 17.39 | ||
| 50–59 | 3.32 (2.99–3.68) | 28 | 24.14 | ||
| 60–69 | 3.05 (2.73–3.41) | 21 | 17.36 | ||
| ≥70 | 3.51 (2.94–4.20) | 20 | 26.67 | ||
| Residence 5 | |||||
| Urban area | 2.98 (2.80–3.18) | <0.001 | 56 | 17.72 | <0.001 |
| Rural area | 2.59 (2.34–2.87) | 14 | 11.20 | ||
| Coastal area | 4.36 (3.91–4.87) | 38 | 34.55 | ||
| Obesity 6 | |||||
| Underweight | 2.35 (1.56–3.53) | NS | 1 | 10.00 | NS |
| Normal | 3.02 (2.83–3.22) | 62 | 18.96 | ||
| Obese | 3.31 (3.05–3.59) | 45 | 21.03 | ||
| Smoking status 7 | |||||
| Current smoker | 3.54 (3.17–3.96) | <0.001 | 30 | 28.30 | <0.001 |
| Ex-smoker | 4.29 (3.80–4.85) | 32 | 36.36 | ||
| Non-smoker | 2.77 (2.61–2.94) | 46 | 12.89 | ||
| Alcohol drinking status 8 | |||||
| Current drinker | 3.52 (3.30–3.76) | <0.001 | 88 | 27.08 | <0.001 |
| Ex-drinker | 3.19 (2.54–4.00) | 4 | 13.33 | ||
| Non-drinker | 2.54 (2.35–2.74) | 16 | 8.16 | ||
| Total | 3.12 (2.96–3.28) | 108 | 19.60 | ||
| Dietary Intake | Blood Mercury (μg/L) 1 | p Value 2 | OR for Blood Mercury ≥ HBM I 3 | ||||||
|---|---|---|---|---|---|---|---|---|---|
| n | Mean | Range | GM | 95% CI | OR | 95% CI | |||
| Total mercury intake (μg/day) | T1 | 184 | 0.99 | (0.32–1.48) | 2.56 | (2.35–2.78) | <0.001 | 1.00 | - |
| T2 | 185 | 2.42 | (1.49–3.56) | 2.84 | (2.62–3.08) | 1.29 | (0.67–2.50) | ||
| T3 | 184 | 7.99 | (3.57–81.72) | 4.16 | (3.84–4.51) | 3.27 | (1.79–5.95) | ||
| % PTDI for inorganic mercury 4 | T1 | 184 | 2.73 | (0.79–4.18) | 2.60 | (2.40–2.83) | <0.001 | 1.00 | - |
| T2 | 185 | 6.77 | (4.19–9.99) | 3.02 | (2.77–3.30) | 1.53 | (0.81–2.88) | ||
| T3 | 184 | 21.77 | (10.00–195.91) | 3.85 | (3.55–4.16) | 3.29 | (1.81–6.01) | ||
| Methylmercury intake from fish and shellfish (μg/day) 5 | T1 | 184 | 0.20 | (0–0.63) | 2.56 | (2.35–2.79) | <0.001 | 1.00 | - |
| T2 | 185 | 1.52 | (0.64–2.57) | 2.88 | (2.65–3.14) | 1.30 | (0.67–2.51) | ||
| T3 | 184 | 6.86 | (2.58–78.27) | 4.09 | (3.79–4.42) | 3.20 | (1.77–5.79) | ||
| % PTDI for methylmercury 6 | T1 | 184 | 1.41 | (0–4.71) | 2.56 | (2.35–2.78) | <0.001 | 1.00 | - |
| T2 | 185 | 10.62 | (4.71–17.99) | 3.01 | (2.76–3.28) | 1.54 | (0.81–2.94) | ||
| T3 | 184 | 46.51 | (18.00–469.06) | 3.94 | (3.64–4.26) | 3.13 | (1.72–5.67) | ||
| Rank | Food Group | Average Food Group Intake (g/day) | Average Mercury Intake (μg/day) | Contribution Rate (%) | Blood Mercury (μg/L) GM (95% CI) 1 | OR for Blood Mercury ≥ HBM I 3 | ||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| T1 | T2 | T3 | p Value 2 | T1 | T2 | T3 | p Value | |||||
| 1 | Fish | 47.3 | 2.50 | 65.8 | 2.55 (2.35–2.77) | 2.99 (2.75–3.24) | 3.97 (3.64–4.32) | <0.001 | 1.00 | 1.73 (0.90–3.32) | 3.11 (1.69–5.75) | <0.001 |
| 2 | Shellfish and other Seafood | 65.3 | 0.45 | 12.0 | 2.53 (2.32–2.76) | 3.00 (2.78–3.25) | 3.98 (3.65–4.33) | <0.001 | 1.00 | 1.87 (0.97–3.58) | 3.28 (1.77–6.05) | <0.001 |
| 3 | Grains | 263.1 | 0.38 | 10.0 | 3.06 (2.81–3.34) | 3.28 (3.00–3.59) | 3.01 (2.76–3.28) | NS | 1.00 | 0.50 (2.80–0.91) | 0.62 (0.35–1.11) | NS |
| 4 | Vegetables | 281.5 | 0.16 | 4.3 | 2.81 (2.59–3.06) | 3.10 (2.83–3.39) | 3.47 (3.19–3.78) | NS | 1.00 | 0.77 (0.43–1.40) | 1.07 (0.59–1.92) | NS |
| 5 | Fruits | 166.9 | 0.07 | 1.8 | 3.26 (2.97–3.58) | 3.10 (2.86–3.37) | 2.66 (2.75–3.26) | NS | 1.00 | 0.84 (0.48–1.47) | 0.86 (0.48–1.53) | NS |
| 6 | Meats | 74.0 | 0.05 | 1.2 | 3.01 (2.75–3.29) | 3.17 (2.89–3.47) | 3.18 (2.94–3.44) | NS | 1.00 | 1.49 (0.81–2.74) | 1.60 (0.85–2.99) | NS |
| 7 | Mushrooms | 4.0 | 0.04 | 1.1 | 3.22 (3.02–3.43) | 2.59 (2.12–3.18) | 3.02 (2.76–3.29) | NS | 1.00 | 0.70 (0.19–2.56) | 1.11 (0.68–1.81) | NS |
| 8 | Beverages and Alcohols | 179.5 | 0.03 | 0.8 | 2.85 (2.62–3.10) | 2.99 (2.77–3.23) | 3.56 (3.23–3.91) | 0.002 | 1.00 | 1.27 (0.66–2.44) | 2.95 (1.57–5.56) | <0.001 |
| 9 | Legumes | 41.5 | 0.03 | 0.8 | 3.05 (2.81–3.32) | 3.19 (2.91–3.50) | 3.11 (2.85–3.38) | NS | 1.00 | 1.30 (0.74–2.28) | 0.84 (0.47–1.51) | NS |
| 10 | Seaweeds | 3.7 | 0.02 | 0.6 | 3.07 (2.80–3.37) | 2.87 (2.66–3.11) | 3.43 (3.14–3.74) | 0.029 | 1.00 | 0.69 (0.38–1.24( | 1.11 (0.64–1.92) | NS |
| 11 | Potatoes and Starch | 32.6 | 0.02 | 0.5 | 3.26 (2.97–3.59) | 3.03 (2.79–3.30) | 3.06 (2.82–3.32) | NS | 1.00 | 0.88 (0.50–1.54) | 1.10 (0.62–1.94) | NS |
| 12 | Eggs | 20.5 | 0.01 | 0.4 | 3.25 (2.96–3.56) | 3.08 (2.82–3.37) | 3.03 (2.79–3.28) | NS | 1.00 | 1.07 (0.61–1.89) | 0.92 (0.51–1.67) | NS |
| 13 | Seasonings | 35.9 | 0.01 | 0.3 | 2.72 (2.49–2.98) | 3.12 (2.86–3.40) | 3.56 (3.28–3.87) | NS | 1.00 | 1.24 (0.68–2.26) | 1.64 (0.91–2.93) | NS |
| 14 | Milk and Dairy Products | 58.4 | 0.01 | 0.3 | 3.29 (3.06–3.53) | 2.89 (2.58–3.22) | 2.97 (2.72–3.25) | NS | 1.00 | 0.44 (0.20–0.98) | 0.92 (0.54–1.55) | NS |
| 15 | Others | 2.3 | 0.00 | 0.1 | 3.09 (2.93–3.26) | 3.31 (2.90–3.79) | - | NS | - | 1.00 | 0.90 (0.44–1.86) | NS |
| 16 | Fat and Oils | 7.3 | 0.00 | 0.0 | 3.08 (2.81–3.37) | 3.21 (2.94–3.52) | 3.06 (2.83–3.32) | NS | 1.00 | 1.65 (0.94–2.90) | 1.23 (0.67–2.24) | NS |
| 17 | Sugars | 6.5 | 0.00 | 0.0 | 3.14 (2.86–3.43) | 3.24 (2.96–3.54) | 2.98 (2.75–3.23) | NS | 1.00 | 0.91 (0.52–1.61) | 1.21 (0.68–2.13) | NS |
| 18 | Seeds and Nuts | 4.4 | 0.00 | 0.0 | 3.23 (2.95–3.54) | 3.07 (2.82–3.35) | 3.05 (2.80–3.31) | NS | 1.00 | 1.04 (0.59–1.83) | 0.98 (0.56–1.72) | NS |
| Fish (Portion Size/Day) 1 | Shellfish and Other Seafood (Portion Size/Day) 1 | |||||||
|---|---|---|---|---|---|---|---|---|
| <1 | 1–2 | ≥2 | p Value 3 | <1 | 1–2 | ≥2 | p Value 4 | |
| n (%) | 317 (57.3) | 140 (25.3) | 96 (17.4) | <0.001 | 514 (93.0) | 29 (5.2) | 10 (1.8) | <0.001 |
| Food group intake (g/day) [Mean ± SD] | 14.3 ± 13.0 | 53.4 ± 21.0 | 147.4 ± 125.3 | <0.001 | 56.2 ± 74.8 | 167.4 ± 88.7 | 237.3 ± 46.6 | <0.001 |
| Methylmercury intake (μg/day) [Mean ± SD] | 0.6 ± 0.9 | 2.5 ± 1.7 | 8.1 ± 9.5 | <0.001 | 0.3 ± 0.5 | 2.3 ± 1.0 | 3.9 ± 1.4 | <0.001 |
| Blood mercury (μg/L) 2 [GM (95% CI)] | 2.77 (2.60–2.96) | 3.44 (3.11–3.80) | 3.96 (3.51–4.46) | 0.001 | 3.07 (2.91–3.24) | 3.66 (3.02–4.42) | 4.19 (3.49–5.04) | 0.030 |
| OR for Blood mercury ≥ HBM I 4 [OR (95% CI)] | 1.00 | 1.24 (0.72–2.15) | 2.07 (1.15–3.72) | 0.050 | 1.00 | 2.30 (0.95–5.58) | 0.65 (0.08–5.56) | NS |
© 2016 by the authors; licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC-BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kim, S.-A.; Kwon, Y.; Kim, S.; Joung, H. Assessment of Dietary Mercury Intake and Blood Mercury Levels in the Korean Population: Results from the Korean National Environmental Health Survey 2012–2014. Int. J. Environ. Res. Public Health 2016, 13, 877. https://doi.org/10.3390/ijerph13090877
Kim S-A, Kwon Y, Kim S, Joung H. Assessment of Dietary Mercury Intake and Blood Mercury Levels in the Korean Population: Results from the Korean National Environmental Health Survey 2012–2014. International Journal of Environmental Research and Public Health. 2016; 13(9):877. https://doi.org/10.3390/ijerph13090877
Chicago/Turabian StyleKim, Seong-Ah, YoungMin Kwon, Suejin Kim, and Hyojee Joung. 2016. "Assessment of Dietary Mercury Intake and Blood Mercury Levels in the Korean Population: Results from the Korean National Environmental Health Survey 2012–2014" International Journal of Environmental Research and Public Health 13, no. 9: 877. https://doi.org/10.3390/ijerph13090877
APA StyleKim, S.-A., Kwon, Y., Kim, S., & Joung, H. (2016). Assessment of Dietary Mercury Intake and Blood Mercury Levels in the Korean Population: Results from the Korean National Environmental Health Survey 2012–2014. International Journal of Environmental Research and Public Health, 13(9), 877. https://doi.org/10.3390/ijerph13090877






