The Role of Influenza in the Delay between Low Temperature and Ischemic Heart Disease: Evidence from Simulation and Mortality Data from Japan
Abstract
:1. Introduction
2. Materials and Methods
2.1. Simulation Using Multi-State Models with Competing Risks
2.1.1. Competing Risks and Multi-State Models
2.1.2. Simulation for IHD Morbidity
2.2. Mortality Data from Japan
2.2.1. Data
2.2.2. Statistical Analysis
Cross-Correlations
Time Series Analysis
3. Results
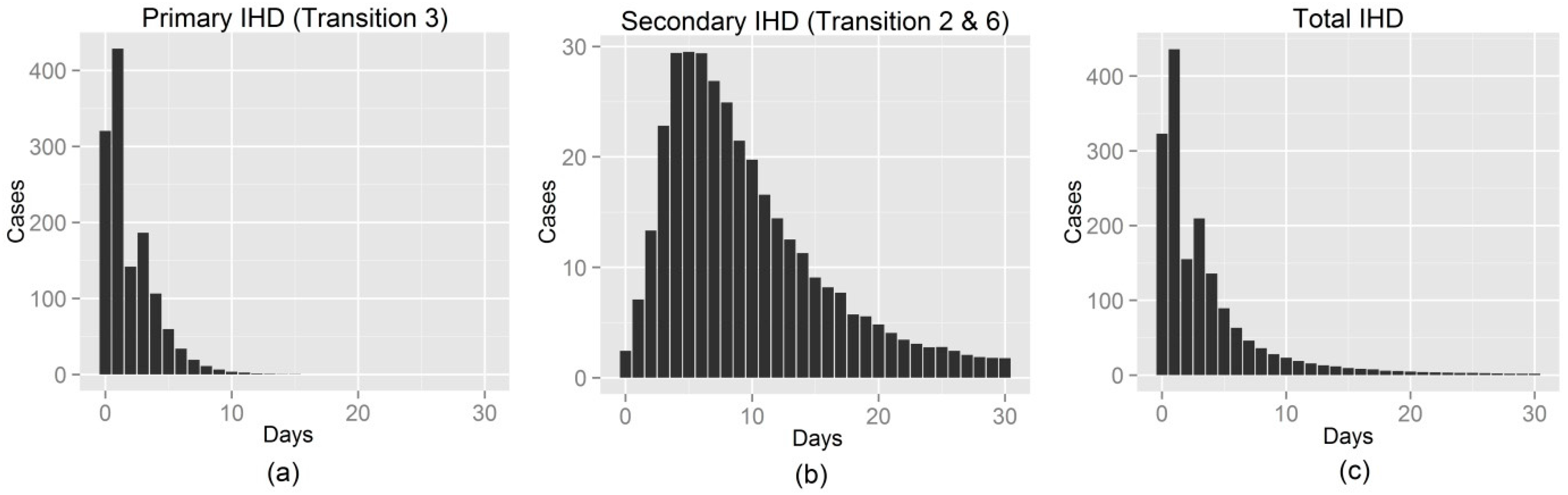
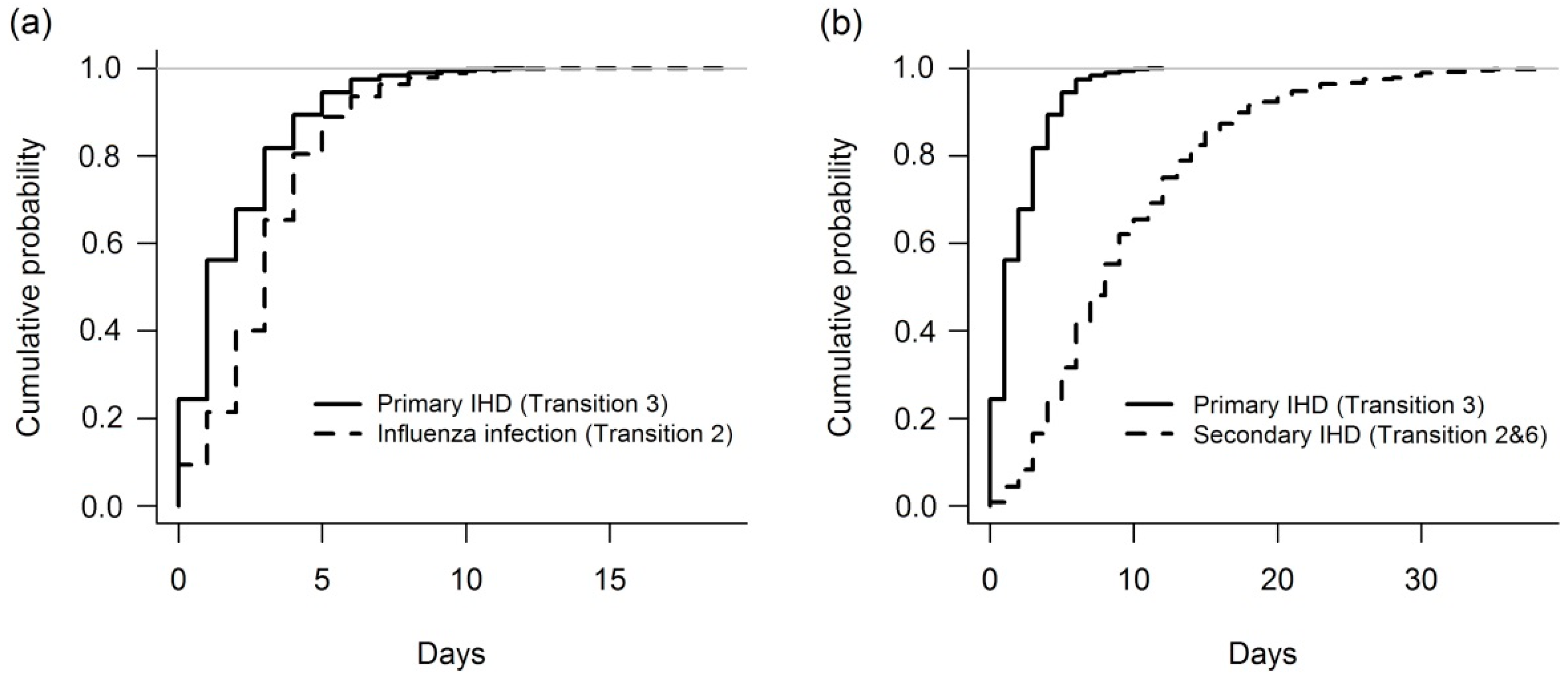
3.1. Simulation
3.2. Japan’s Mortality Data
3.2.1. Cross-Correlations
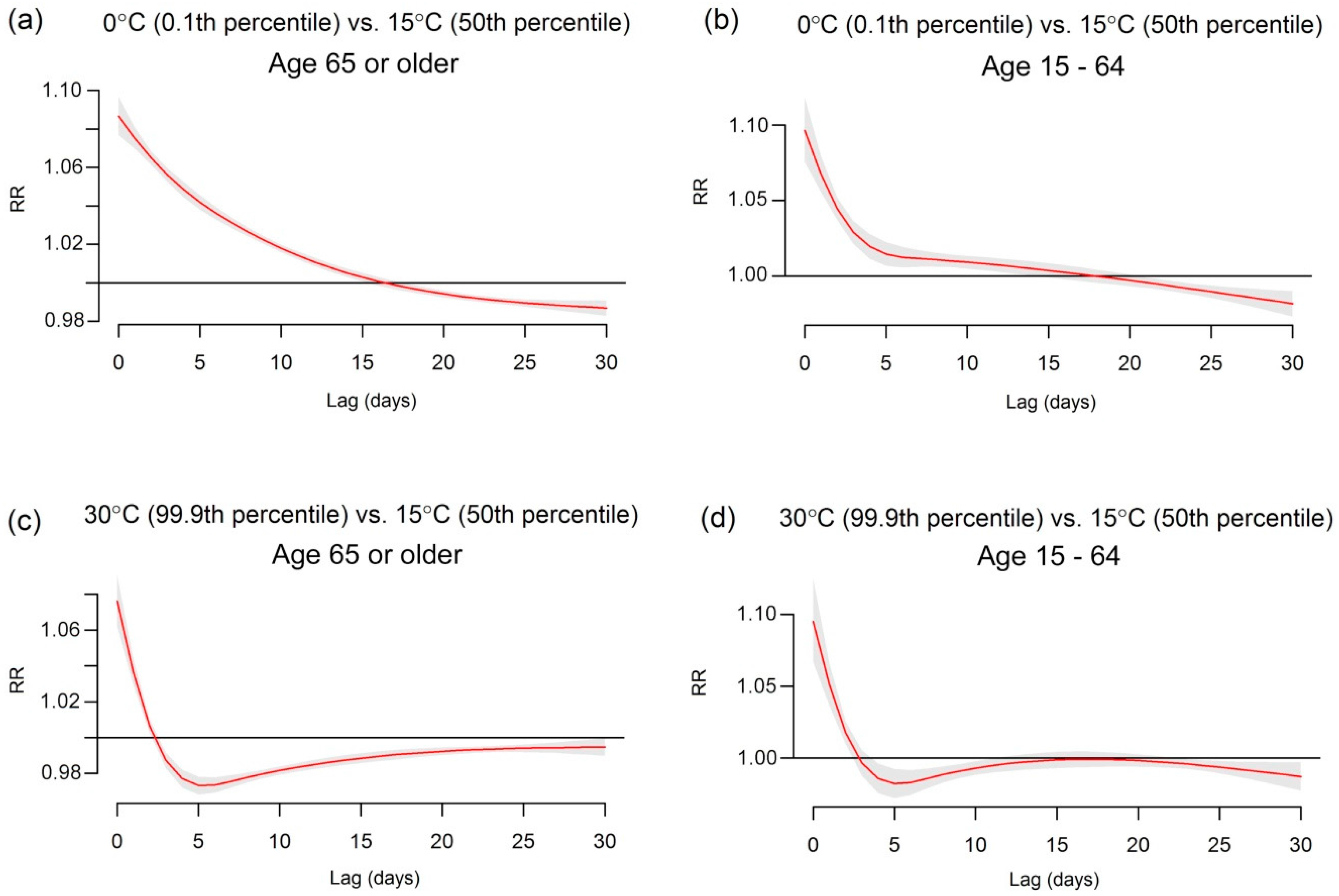
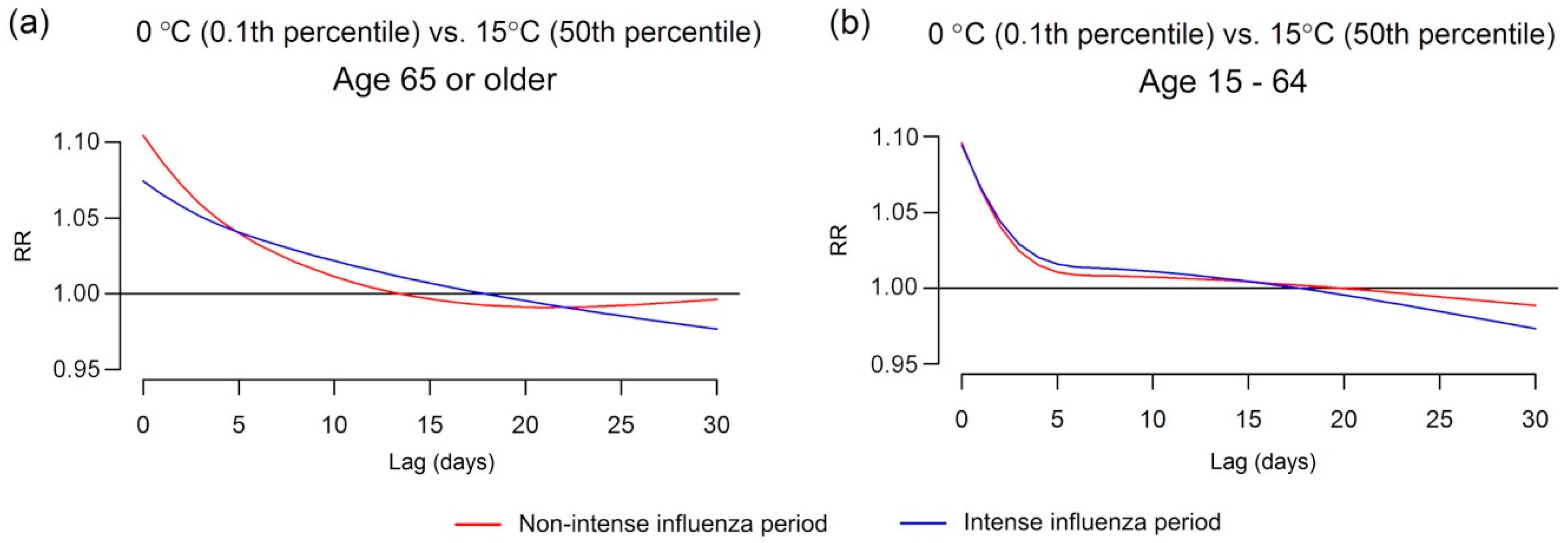
3.2.2. Time Series Analysis
4. Discussion
5. Conclusions
Supplementary Materials
Acknowledgments
Author Contributions
Conflicts of Interest
Abbreviations
| ICD | International Classification of Diseases |
| IHD | Ischemic heart diseases |
| MHLW | Ministry of Health, Labour and Welfare |
| P&I | Pneumonia and influenza |
| RR | Relative risks |
References
- Analitis, A.; Katsouyanni, K.; Biggeri, A.; Baccini, M.; Forsberg, B.; Bisanti, L.; Kirchmayer, U.; Ballester, F.; Cadum, E.; Goodman, P.G.; et al. Effects of cold weather on mortality: Results from 15 European cities within the PHEWE project. Am. J. Epidemiol. 2008, 168, 1397–1408. [Google Scholar] [CrossRef] [PubMed]
- Tian, Z.; Li, S.; Zhang, J.; Jaakkola, J.; Guo, Y. Ambient temperature and coronary heart disease mortality in Beijing, China: A time series study. Environ. Health 2012, 11, 56. [Google Scholar] [CrossRef] [PubMed]
- Warren-Gash, C.; Hayward, A.C.; Hemingway, H.; Denaxas, S.; Thomas, S.L.; Timmis, A.D.; Whitaker, H.; Smeeth, L. Influenza infection and risk of acute myocardial infarction in England and Wales: A caliber self-controlled case series study. J. Infect. Dis. 2012, 206, 1652–1659. [Google Scholar] [CrossRef] [PubMed]
- Lichenstein, R.; Magder, L.S.; King, R.E.; King, J.C. The relationship between influenza outbreaks and acute ischemic heart disease in Maryland residents over a 7-year period. J. Infect. Dis. 2012, 206, 821–827. [Google Scholar] [CrossRef] [PubMed]
- Siriwardena, A.N. Increasing evidence that influenza is a trigger for cardiovascular disease. J. Infect. Dis. 2012, 206, 1636–1638. [Google Scholar] [CrossRef] [PubMed]
- Marsden, P.A. Inflammation and coagulation in the cardiovascular system: The contribution of influenza. Circ. Res. 2006, 99, 1152–1153. [Google Scholar] [CrossRef] [PubMed]
- Udell, J.A.; Zawi, R.; Bhatt, D.L.; Keshtkar-Jahromi, M.; Gaughran, F.; Phrommintikul, A.; Ciszewski, A.; Vakili, H.; Hoffman, E.B.; Farkouh, M.E.; et al. Association between influenza vaccination and cardiovascular outcomes in high-risk patients: A meta-analysis. JAMA 2013, 310, 1711–1720. [Google Scholar] [CrossRef] [PubMed]
- Kunst, A.E.; Looman, C.W.N.; Mackenbach, J.P. Outdoor air temperature and mortality in the Netherlands: A time-series analysis. Am. J. Epidemiol. 1993, 137, 331–341. [Google Scholar] [PubMed]
- Beyersmann, J.; Allignol, A.; Schumacher, M. Competing Risks and Multistate Models with R; Springer: Freiburg, Germany, 2011. [Google Scholar]
- De Wreede, L.C.; Fiocco, M.; Putter, H. The mstate package for estimation and prediction in non- and semi-parametric multi-state and competing risks models. Comput. Methods Programs Biomed. 2010, 99, 261–274. [Google Scholar] [CrossRef] [PubMed]
- Pintilie, M. An introduction to competing risks analysis. Rev. Esp. Cardiol. 2011, 64, 599–605. [Google Scholar] [CrossRef] [PubMed]
- Putter, H.; Fiocco, M.; Geskus, R.B. Tutorial in biostatistics: Competing risks and multi-state models. Stat. Med. 2007, 26, 2389–2430. [Google Scholar] [CrossRef] [PubMed]
- Fujikawa, A.; Suzue, T.; Jitsunari, F.; Hirao, T. Evaluation of health-related quality of life using EQ-5D in Takamatsu, Japan. Environ. Health Prev. Med. 2011, 16, 25–35. [Google Scholar] [CrossRef] [PubMed]
- National Federation of Health Insurance Societies. Report for the Trend of Common Cold, Influenza, and Seasonal Disease 2012. Available online: http://www.kenporen.com/study/toukei_data/pdf/chosa_h24_12.pdf (accessed on 12 December 2014).
- Japanese Ministiry of Health Labour and Welfare. Summary of Patient Survey, 2011. Available online: http://www.mhlw.go.jp/toukei/saikin/hw/kanja/11/ (accessed on 12 December 2014).
- Smeeth, L.; Thomas, S.L.; Hall, A.J.; Hubbard, R.; Farrington, P.; Vallance, P. Risk of myocardial infarction and stroke after acute infection or vaccination. N. Engl. J. Med. 2004, 351, 2611–2618. [Google Scholar] [CrossRef] [PubMed]
- Hong, K.W.; Cheong, H.J.; Choi, W.S.; Lee, J.; Wie, S.H.; Baek, J.H.; Kim, H.Y.; Jeong, H.W.; Kim, W.J. Clinical courses and outcomes of hospitalized adult patients with seasonal influenza in Korea, 2011–2012: Hospital-based influenza morbidity and mortality (HIMM) surveillance. J. Infect. Chemother. 2014, 20, 9–14. [Google Scholar] [CrossRef] [PubMed]
- Alonso, W.J.; Viboud, C.; Simonsen, L.; Hirano, E.W.; Daufenbach, L.Z.; Miller, M.A. Seasonality of influenza in Brazil: A traveling wave from the amazon to the subtropics. Am. J. Epidemiol. 2007, 165, 1434–1442. [Google Scholar] [CrossRef] [PubMed]
- Reichert, T.A.; Simonsen, L.; Sharma, A.; Pardo, S.A.; Fedson, D.S.; Miller, M.A. Influenza and the winter increase in mortality in the United States, 1959–1999. Am. J. Epidemiol. 2004, 160, 492–502. [Google Scholar] [CrossRef] [PubMed]
- Simonsen, L. The global impact of influenza on morbidity and mortality. Vaccine 1999, 17 (Suppl. 1), S3–S10. [Google Scholar] [CrossRef]
- Viboud, C.; Bjornstad, O.N.; Smith, D.L.; Simonsen, L.; Miller, M.A.; Grenfell, B.T. Synchrony, waves, and spatial hierarchies in the spread of influenza. Science 2006, 312, 447–451. [Google Scholar] [CrossRef] [PubMed]
- Viboud, C.; Boelle, P.Y.; Pakdaman, K.; Carrat, F.; Valleron, A.J.; Flahault, A. Influenza epidemics in the United States, France, and Australia, 1972–1997. Emerg. Infect. Dis. 2004, 10, 32–39. [Google Scholar] [CrossRef] [PubMed]
- Gasparrini, A.; Armstrong, B.; Kenward, M.G. Distributed lag non-linear models. Stat. Med. 2010, 29, 2224–2234. [Google Scholar] [CrossRef] [PubMed]
- Gasparrini, A. Distributed lag linear and non-linear models in R: The package DLNM. J. Stat. Softw. 2011, 43, 1–20. [Google Scholar] [CrossRef] [PubMed]
- Huang, C.; Barnett, A.G.; Wang, X.; Tong, S. Effects of extreme temperatures on years of life lost for cardiovascular deaths: A time series study in Brisbane, Australia. Circ. Cardiovasc. Qual. Outcomes 2012, 5, 609–614. [Google Scholar] [CrossRef] [PubMed]
- Guo, Y.; Barnett, A.G.; Pan, X.; Yu, W.; Tong, S. The impact of temperature on mortality in Tianjin, China: A case-crossover design with a distributed lag nonlinear model. Environ. Health Perspect. 2011, 119, 1719–1725. [Google Scholar] [CrossRef] [PubMed]
- Bhaskaran, K.; Gasparrini, A.; Hajat, S.; Smeeth, L.; Armstrong, B. Time series regression studies in environmental epidemiology. Int. J. Epidemiol. 2013, 42, 1187–1195. [Google Scholar] [CrossRef] [PubMed]
- R Core Team. R: A Language and Environment for Statistical Computing. Available online: http://www.R-project.org (accessed on 22 January 2016).
- Huang, J.; Wang, J.; Yu, W. The lag effects and vulnerabilities of temperature effects on cardiovascular disease mortality in a subtropical climate zone in China. Int. J. Environ. Res. Public Health 2014, 11, 3982–3994. [Google Scholar] [CrossRef] [PubMed]
- Yu, W.; Hu, W.; Mengersen, K.; Guo, Y.; Pan, X.; Connell, D.; Tong, S. Time course of temperature effects on cardiovascular mortality in Brisbane, Australia. Heart 2011, 97, 1089–1093. [Google Scholar] [CrossRef] [PubMed]
- Braga, A.L.; Zanobetti, A.; Schwartz, J. The effect of weather on respiratory and cardiovascular deaths in 12 U.S. Cities. Environ. Health Perspect. 2002, 110, 859–863. [Google Scholar] [CrossRef] [PubMed]
- Jousilahti, P.; Vartiainen, E.; Tuomilehto, J.; Puska, P. Sex, age, cardiovascular risk factors, and coronary heart disease: A prospective follow-up study of 14,786 middle-aged men and women in Finland. Circulation 1999, 99, 1165–1172. [Google Scholar] [CrossRef] [PubMed]
- Keatinge, W.R. Winter mortality and its causes. Int. J. Circumpolar Health 2002, 61, 292–299. [Google Scholar] [CrossRef] [PubMed]
- Bhaskaran, K.; Hajat, S.; Haines, A.; Herrett, E.; Wilkinson, P.; Smeeth, L. Effects of ambient temperature on the incidence of myocardial infarction. Heart 2009, 95, 1760–1769. [Google Scholar] [CrossRef] [PubMed]
- Von Klot, S.; Zanobetti, A.; Schwartz, J. Influenza epidemics, seasonality, and the effects of cold weather on cardiac mortality. Environ. Health 2012, 11, 74. [Google Scholar] [CrossRef] [PubMed]
- Halonen, J.I.; Zanobetti, A.; Sparrow, D.; Vokonas, P.S.; Schwartz, J. Associations between outdoor temperature and markers of inflammation: A cohort study. Environ. Health 2010, 11. [Google Scholar] [CrossRef] [PubMed]
- Vallance, P.; Collier, J.; Bhagat, K. Infection, inflammation, and infarction: Does acute endothelial dysfunction provide a link? Lancet 1997, 349, 1391–1392. [Google Scholar] [CrossRef]
- Fraser, C.; Riley, S.; Anderson, R.M.; Ferguson, N.M. Factors that make an infectious disease outbreak controllable. Proc. Natl. Acad. Sci. USA 2004, 101, 6146–6151. [Google Scholar] [CrossRef] [PubMed]
- Elveback, L.R.; Fox, J.P.; Ackerman, E.; Langworthy, A.; Boyd, M.; Gatewood, L. An influenza simulation model for immunization studies. Am. J. Epidemiol. 1976, 103, 152–165. [Google Scholar] [PubMed]
- Wu, J.T.; Riley, S.; Fraser, C.; Leung, G.M. Reducing the impact of the next influenza pandemic using household-based public health interventions. PLoS Med. 2006, 3, e361. [Google Scholar] [CrossRef] [PubMed]
- Mourtzoukou, E.G.; Falagas, M.E. Exposure to cold and respiratory tract infections. Int. J. Tuberc. Lung Dis. 2007, 11, 938–943. [Google Scholar] [PubMed]
- Gasparrini, A.; Guo, Y.; Hashizume, M.; Lavigne, E.; Zanobetti, A.; Schwartz, J.; Tobias, A.; Tong, S.; Rocklov, J.; Forsberg, B.; et al. Mortality risk attributable to high and low ambient temperature: A multi-country study. Lancet 2015, 386, 369–375. [Google Scholar] [CrossRef]
- Mann, J.K.; Tager, I.B.; Lurmann, F.; Segal, M.; Quesenberry, C.P., Jr.; Lugg, M.M.; Shan, J.; Van Den Eeden, S.K. Air pollution and hospital admissions for ischemic heart disease in persons with congestive heart failure or arrhythmia. Environ. Health Perspect. 2002, 110, 1247–1252. [Google Scholar] [CrossRef] [PubMed]
- Brook, R.D.; Franklin, B.; Cascio, W.; Hong, Y.; Howard, G.; Lipsett, M.; Luepker, R.; Mittleman, M.; Samet, J.; Smith, S.C., Jr.; et al. Air pollution and cardiovascular disease: A statement for healthcare professionals from the Expert Panel on Population and Prevention Science of the American Heart Association. Circulation 2004, 109, 2655–2671. [Google Scholar] [CrossRef] [PubMed]
- Buckley, J.P.; Samet, J.M.; Richardson, D.B. Commentary: Does air pollution confound studies of temperature? Epidemiology 2014, 25, 242–245. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. The Top 10 Cause of Death. Available online: http://www.who.int/mediacentre/factsheets/fs310/en (accessed on 21 November 2014).
- United Nations. World Population Aging 2013. Available online: http://www.un.org/en/development/desa/population/publications/pdf/ageing/WorldPopulationAgeing2013.pdf (accessed on 21 November 2014).
- Mori, M.; Watanabe, M.; Shiogama, H.; Inoue, J.; Kimoto, M. Robust arctic sea-ice influence on the frequent Eurasian cold winters in past decades. Nature Geosci. 2014, 7, 869–873. [Google Scholar] [CrossRef]


© 2016 by the authors; licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC-BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Imai, C.; Barnett, A.G.; Hashizume, M.; Honda, Y. The Role of Influenza in the Delay between Low Temperature and Ischemic Heart Disease: Evidence from Simulation and Mortality Data from Japan. Int. J. Environ. Res. Public Health 2016, 13, 454. https://doi.org/10.3390/ijerph13050454
Imai C, Barnett AG, Hashizume M, Honda Y. The Role of Influenza in the Delay between Low Temperature and Ischemic Heart Disease: Evidence from Simulation and Mortality Data from Japan. International Journal of Environmental Research and Public Health. 2016; 13(5):454. https://doi.org/10.3390/ijerph13050454
Chicago/Turabian StyleImai, Chisato, Adrian G. Barnett, Masahiro Hashizume, and Yasushi Honda. 2016. "The Role of Influenza in the Delay between Low Temperature and Ischemic Heart Disease: Evidence from Simulation and Mortality Data from Japan" International Journal of Environmental Research and Public Health 13, no. 5: 454. https://doi.org/10.3390/ijerph13050454
APA StyleImai, C., Barnett, A. G., Hashizume, M., & Honda, Y. (2016). The Role of Influenza in the Delay between Low Temperature and Ischemic Heart Disease: Evidence from Simulation and Mortality Data from Japan. International Journal of Environmental Research and Public Health, 13(5), 454. https://doi.org/10.3390/ijerph13050454





