Examining the Cervical Screening Behaviour of Women Aged 50 or above and Its Predicting Factors: A Population-Based Survey
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Design, Setting and Participants
2.2. Questionnaire
2.3. Ethical Considerations
2.4. Statistical Analysis
3. Results
3.1. Socio-Demographic Characteristics and Health Status
3.2. Health Related Perceptions and Utilisation of Complementary Therapies
3.3. Cervical Cancer Screening Behaviour
3.4. Factors Associated with Ever Having Had a Cervical Smear Test
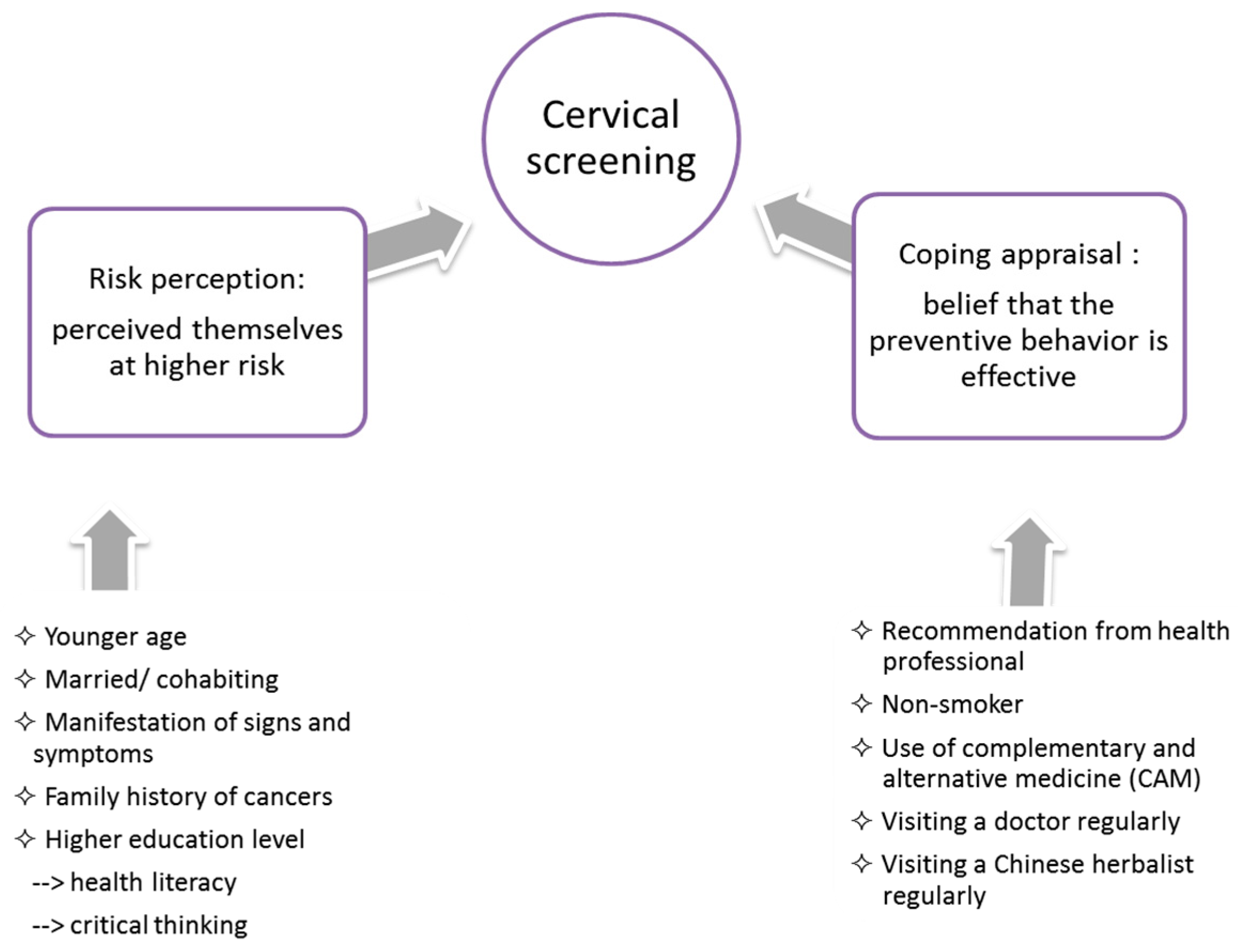
4. Discussion
Limitations
5. Conclusions
Acknowledgments
Author Contributions
Conflicts of Interest
References
- Vaccarella, S.; Franceschi, S.; Engholm, G.; Lönnberg, S.; Khan, S.; Bray, F. 50 years of screening in the Nordic countries: Quantifying the effects on cervical cancer incidence. Br. J. Cancer 2014, 111, 965–969. [Google Scholar] [CrossRef] [PubMed]
- Vaccarella, S.; Lortet-Tieulent, J.; Plummer, M.; Franceschi, S.; Bray, F. Worldwide trends in cervical cancer incidence: Impact of screening against changes in disease risk factors. Eur. J. Cancer 2013, 49, 3262–3273. [Google Scholar] [CrossRef] [PubMed]
- Dickinson, J.A.; Stankiewicz, A.; Popadiuk, C.; Pogany, L.; Onysko, J.; Miller, A.B. Reduced cervical cancer incidence and mortality in Canada: National data from 1932 to 2006. BMC Public Health 2012, 12, 992. [Google Scholar] [CrossRef] [PubMed]
- Centers for Disease Control & Prevention (CDC). Cervical cancer screening among women by hysterectomy status and among women aged ≥ 65 years—United States, 2000–2010. MMWR Morb. Mortal. Wkly. Rep. 2013, 61, 1043–1047. [Google Scholar]
- Rogers, R.; Cacioppo, J.; Petty, R. Cognitive and physiological processes in fear appeals and attitude change: A revised theory of protection motivation. In Social Psychophysiology: A Sourcebook; Cacioppo, J., Petty, R., Eds.; The Guilford Press: New York, NY, USA, 1983; pp. 153–177. [Google Scholar]
- Rogers, R.W. A protection motivation theory of fear appeals and attitude change 1. J. Psychol. 1975, 91, 93–114. [Google Scholar] [CrossRef]
- Chan, C.W.H.; Yang, S.B.; Gu, C.; Wang, X.; Tao, L. Perception of cervical cancer risk and screening behavior: A literature review. Int. J. Nurs. Knowl. 2015, 26, 2–18. [Google Scholar] [CrossRef] [PubMed]
- Shin, D.W.; Kim, Y.W.; Oh, J.H.; Kim, S.W.; Chung, K.W.; Lee, W.Y.; Lee, J.E.; Lee, W.C.; Guallar, E.; Cho, J. Knowledge, attitudes, risk perception, and cancer screening behaviors among cancer survivors. Cancer 2011, 117, 3850–3859. [Google Scholar] [CrossRef] [PubMed]
- So, W.K.W.; Choi, K.C.; Chan, D.N.S.; Shiu, A.T.Y.; Ho, S.S.M.; Chan, H.Y.L.; Lam, W.W.T.; Cheng, K.K.F.; Goggins, W.; Chan, C.W.H. Colorectal cancer screening behaviour and associated factors among Chinese aged 50 and above in Hong Kong—A population-based survey. Euro. J. Oncol. Nurs. 2012, 16, 413–418. [Google Scholar] [CrossRef] [PubMed]
- Gu, C.; Chan, C.W.H.; Twinn, S. How sexual history and knowledge of cervical cancer and screening influence Chinese women’s screening behavior in mainland China. Cancer Nurs. 2010, 33, 445–453. [Google Scholar] [CrossRef] [PubMed]
- Gu, C.; Chan, C.W.H.; Twinn, S.; Choi, K.C. The influence of knowledge and perception of the risk of cervical cancer on screening behavior in mainland Chinese women. Psychooncology 2012, 21, 1299–1308. [Google Scholar] [CrossRef] [PubMed]
- Shea, J.; Klainin-Yobas, P.; Mackey, S. Young Singaporean women’s knowledge of cervical cancer and pap smear screening: A descriptive study. J. Clin. Nurs. 2013, 22, 3310–3319. [Google Scholar] [CrossRef] [PubMed]
- Gu, C.; Chan, C.W.H.; He, G.P.; Choi, K.C.; Yang, S.B. Chinese women’s motivation to receive future screening: The role of social-demographic factors, knowledge and risk perception of cervical cancer. Euro. J. Oncol. Nurs. 2013, 17, 154–161. [Google Scholar] [CrossRef] [PubMed]
- Lee, P.W.H.; Kwan, T.T.C.; Tam, K.F.; Chan, K.K.L.; Young, P.M.C.; Lo, S.S.T.; Cheung, A.N.Y.; Ngan, H.Y.S. Beliefs about cervical cancer and human papillomavirus (HPV) and acceptability of HPV vaccination among Chinese women in Hong Kong. Prev. Med. 2007, 45, 130–134. [Google Scholar] [CrossRef] [PubMed]
- Twinn, S.; Shiu, A.T.Y.; Holroyd, E. Women’s knowledge about cervical cancer and cervical screening practice: A pilot study of Hong Kong Chinese women. Cancer Nurs. 2002, 25, 377–384. [Google Scholar] [CrossRef] [PubMed]
- Cuzick, J.; Myers, O.; Hunt, W.C.; Robertson, M.; Joste, N.E.; Castle, P.E.; Benard, V.B.; Wheeler, C.M.; New Mexico HPV Pap Registry Steering Committee. A population-based evaluation of cervical screening in the United States: 2008–2011. Cancer Epidemiol. Biomarkers Prev. 2014, 23, 765–773. [Google Scholar] [CrossRef] [PubMed]
- Wharam, J.F.; Zhang, F.; Xu, X.; Landon, B.E.; Ross-Degnan, D. National trends and disparities in cervical cancer screening among commercially insured Women, 2001–2010. Cancer Epidemiol. Biomarkers Prev. 2014, 23, 2366–2373. [Google Scholar] [CrossRef] [PubMed]
- Olesen, S.; Butterworth, P.; Jacomb, P.; Tait, R. Personal factors influence use of cervical cancer screening services: Epidemiological survey and linked administrative data address the limitations of previous research. BMC Health Serv. Res. 2012, 12, 34. [Google Scholar] [CrossRef] [PubMed]
- Geyer, S.; Jaunzeme, J.; Hillemanns, P. Cervical cancer screening in Germany: Group-specific participation rates in the state of Niedersachsen (Lower Saxony). A study with health insurance data. Arch. Gynecol. Obstet. 2015, 291, 623–629. [Google Scholar] [CrossRef] [PubMed]
- Lee, M.; Park, E.C.; Chang, H.S.; Kwon, J.A.; Yoo, K.B.; Kim, T.H. Socioeconomic disparity in cervical cancer screening among Korean women: 1998–2010. BMC Public Health 2013, 13, 553. [Google Scholar] [CrossRef] [PubMed]
- Smith, A.M.A.; Heywood, W.; Ryall, R.; Shelley, J.M.; Pitts, M.K.; Richters, J.; Simpson, J.M.; Patrick, K. Association between sexual behavior and cervical cancer screening. J. Womens Health 2011, 20, 1091–1096. [Google Scholar] [CrossRef] [PubMed]
- Seow, A.; Wong, M.L.; Smith, W.C.S.; Lee, H.P. Beliefs and attitudes as determinants of cervical cancer screening: A community-based study in Singapore. Prev. Med. 1995, 24, 134–141. [Google Scholar] [CrossRef] [PubMed]
- Hewitt, M.; Devesa, S.S.; Breen, N. Cervical cancer screening among U.S. women: Analyses of the 2000 National Health Interview Survey. Prev. Med. 2004, 39, 270–278. [Google Scholar] [CrossRef] [PubMed]
- Miles, A.; Cockburn, J.; Smith, R.A.; Wardle, J. A perspective from countries using organized screening programs. Cancer 2004, 101 (Suppl. S5), 1201–1213. [Google Scholar] [CrossRef] [PubMed]
- Tacken, M.A.; Braspenning, J.C.; Hermens, R.P.; Spreeuwenberg, P.M.; van den Hoogen, H.J.; de Bakker, D.H.; Groenewegen, P.P.; Grol, R.P.T. Uptake of cervical cancer screening in The Netherlands is mainly influenced by women’s beliefs about the screening and by the inviting organization. Eur. J. Public Health 2007, 17, 178–185. [Google Scholar] [CrossRef] [PubMed]
- Ma, G.X.; Wang, M.Q.; Ma, X.S.; Shive, S.E.; Tan, Y.; Toubbeh, J.I. Pathways of cervical cancer screening among Chinese women. Int. J. Womens Health 2013, 5, 351–359. [Google Scholar] [CrossRef] [PubMed]
- Mo, B. Modesty, sexuality, and breast health in Chinese-American women. West. J. Med. 1992, 157, 260–264. [Google Scholar] [PubMed]
- Zhou, Y.R. Changing behaviours and continuing silence: Sex in the post-immigration lives of mainland Chinese immigrants in Canada. Cult. Health Sex. 2012, 14, 87–100. [Google Scholar] [CrossRef] [PubMed]
- Abdullah, A.S.; Leung, K.F.; Leung, C.K.; Leung, N.S.; Leung, W.W.; Leung, Y.Y.; Leung, R.Y.; Li, K.Y.; Li, P.H.; Liang, Y.S.; et al. Factors associated with the use of breast and cervical cancer screening services among Chinese women in Hong Kong. Public Health 2001, 115, 212–217. [Google Scholar] [CrossRef]
- Jia, Y.; Li, S.; Yang, R.; Zhou, H.; Xiang, Q.; Hu, T.; Zhang, Q.; Chen, Z.; Ma, D.; Feng, L. Knowledge about cervical cancer and barriers of screening program among women in Wufeng County, a high-incidence region of cervical cancer in China. PLoS ONE 2013, 8, e67005. [Google Scholar] [CrossRef] [PubMed]
- Lindau, S.T.; Tomori, C.; Lyons, T.; Langseth, L.; Bennett, C.L.; Garcia, P. The association of health literacy with cervical cancer prevention knowledge and health behaviors in a multiethnic cohort of women. Am. J. Obstet. Gynecol. 2002, 186, 938–943. [Google Scholar] [CrossRef] [PubMed]
- Sentell, T.L.; Tsoh, J.Y.; Davis, T.; Davis, J.; Braun, K.L. Low health literacy and cancer screening among Chinese Americans in California: A cross-sectional analysis. BMJ Open 2015, 5, e006104. [Google Scholar] [CrossRef] [PubMed]
- Wong, Y.L.; Chinna, K.; Mariapun, J.; Shuib, R. Correlates between risk perceptions of cervical cancer and screening practice. Prev. Med. 2013, 57, S24–S26. [Google Scholar] [CrossRef] [PubMed]
| Socio-Demographic Characteristics | n (%) | |
| Age (Years) | 50–59 | 418 (43.6%) |
| 60–69 | 232 (24.2%) | |
| 70–79 | 202 (21.1%) | |
| 80 or Above | 107 (11.2%) | |
| Education Level | Primary or Below | 510 (53.3%) |
| Secondary | 352 (36.8%) | |
| Matriculation or Above | 95 (9.9%) | |
| Marital Status | Single/Divorced/Widowed | 284 (29.9%) |
| Married/Cohabiting | 665 (70.1%) | |
| Employment Status | Unemployed | 815 (85.1%) |
| Employed | 143 (14.9%) | |
| Monthly Household Income (HK$) | <10,000 | 278 (29.4%) |
| 10,000–29,999 | 200 (21.1%) | |
| ≥30,000 | 102 (10.8%) | |
| Don’t Know/Declined to Disclose | 366 (38.7%) | |
| Health Status | n (%) | |
| Chronic Illness | Any Confirmed Chronic Illness | 433 (45.2%) |
| Serious Disease | Ever Had a Serious Disease or Cancer | 81 (8.4%) |
| Family History of Cancer | No/Don’t Know | 746 (77.8%) |
| Yes | 213 (22.2%) | |
| Smoking Status | Never Smoked | 925 (96.5%) |
| Ex-Smoker | 14 (1.5%) | |
| Current Smoker | 20 (2.1%) | |
| Health-Related Perceptions | n (%) | |
| Perceived Health Status | Excellent/very Good/Good | 365 (38.1%) |
| Fair/Poor | 594 (61.9%) | |
| Believing that the Following Practices are Good for Health | Exercise | 734 (76.5%) |
| A Healthy Diet | 715 (74.6%) | |
| Visiting a Doctor Regularly | 462 (48.2%) | |
| Visiting a Chinese Herbalist Regularly | 242 (25.2%) | |
| Taking Dietary Supplements | 241 (25.1%) | |
| Perceived Susceptibility to Cancer (Range: 1 = Not at All Likely to 10 = Extremely Likely) | ≤5 | 621 (64.8%) |
| >5 | 55 (5.7%) | |
| Unsure | 283 (29.5%) | |
| Utilisation of Complementary Therapy | n (%) | |
| Ever Used the Following Complementary Therapies | Acupuncture | 174 (18.1%) |
| Cupping | 115 (12.0%) | |
| herbal Remedies | 337 (35.1%) | |
| Bone Setting | 225 (23.5%) | |
| Chinese Massage | 153 (16.0%) | |
| Use of Complementary Therapy Index | 0 (≤50th Percentile) | 446 (46.5%) |
| 1–2 (>50th–75th Percentile) | 251 (26.2%) | |
| ≥3 (>75th Percentile) | 262 (27.3%) | |
| Screening Behaviour | n (%) | |
| Any Health Professional Recommended a Cervical Smear Test | No/Unsure | 876 (91.3%) |
| Yes | 83 (8.7%) | |
| Ever Had a Cervical Smear Test | No | 500 (52.1%) |
| Yes | 457 (47.7%) | |
| Unsure | 2 (0.2%) | |
| Among Those Who Had Ever Had a Cervical Smear Test (n = 457) | n (%) | |
| Time since the Most Recent Test | <1 Year | 75 (16.4%) |
| 1–2 Years | 163 (35.7%) | |
| 3–4 Years | 99 (21.7%) | |
| 5–6 Years | 44 (9.6%) | |
| >6 Years | 45 (9.8%) | |
| Can’t Remember | 31 (6.8%) | |
| Ever Had an Abnormal Test Result | No | 426 (93.2%) |
| Yes | 29 (6.3%) | |
| Unsure | 2 (0.4%) | |
| The Three Main Reasons for the Most Recent Cervical Smear Test | 1. Regular Medical Check-Up | 351 (76.8%) |
| 2. Prompted by Local Signs and Symptoms * | 28 (6.1%) | |
| 3. Physician’s Recommendation | 21 (4.6%) | |
| Among Those Who Had Not Had a Cervical Smear Test (n = 500) | n (%) | |
| The Three Most Important Reasons For Not Having A Cervical Screening | 1. Not Necessary | 331 (66.2%) |
| 2. Healthy All Along | 43 (8.6%) | |
| 3. Other Unspecified Reason | 24 (4.8%) | |
| Factors | Ever Had a Cervical Smear Test | ORU | p-Value | ORA (95% CI) | p-Value | ||
|---|---|---|---|---|---|---|---|
| No (n = 500) | Yes (n = 457) | ||||||
| Demographic Characteristics | - | - | - | - | - | - | |
| Age (Years) | 50–59 (Reference) | 141 (33.8%) | 276 (66.2%) | 1 | - | 1 | - |
| 60–69 | 120 (51.7%) | 112 (48.3%) | 0.48 | <0.001 | 0.53 (0.36–0.77) | 0.001 | |
| 70–79 | 145 (71.8%) | 57 (28.2%) | 0.20 | <0.001 | 0.29 (0.18–0.44) | <0.001 | |
| 80 or Above | 94 (88.7%) | 12 (11.3%) | 0.07 | <0.001 | 0.12 (0.06–0.23) | <0.001 | |
| Education Level | Primary or Below (Reference) | 330 (64.8%) | 179 (35.2%) | 1 | - | 1 | - |
| Secondary | 140 (39.9%) | 211 (60.1%) | 2.78 | <0.001 | 1.55 (1.10–2.19) | 0.012 | |
| Matriculation or Above | 29 (30.5%) | 66 (69.5%) | 4.20 | <0.001 | 2.59 (1.49–4.48) | 0.001 | |
| Employment Status | Unemployed (Reference) | 450 (55.3%) | 364 (44.7%) | 1 | - | NS | - |
| Employed | 50 (35.2%) | 92 (64.8%) | 2.27 | <0.001 | - | - | |
| Monthly Household Income (HK$) | <10,000 (Reference) | 180 (64.7%) | 98 (35.3%) | 1 | - | NS | - |
| 10,000–29,999 | 81 (40.5%) | 119 (59.5%) | 2.70 | <0.001 | - | - | |
| ≥30,000 | 26 (25.5%) | 76 (74.5%) | 5.37 | <0.001 | - | - | |
| Don’t Know/Decline to Disclose | 206 (56.6%) | 158 (43.4%) | 1.41 | 0.037 | - | - | |
| Marital Status | Single/Divorced/Widowed (Reference) | 194 (68.3%) | 90 (31.7%) | 1 | - | 1 | - |
| Married/Cohabiting | 302 (45.6%) | 361 (54.4%) | 2.58 | <0.001 | 1.80 (1.25–2.58) | 0.001 | |
| Health Status | - | - | - | - | - | - | |
| Any Confirmed Chronic Illness | No (Reference) | 252 (48.1%) | 272 (51.9%) | 1 | - | NS | - |
| Yes | 248 (57.3%) | 185 (42.7%) | 0.69 | 0.005 | - | - | |
| Ever Had A Serious Disease or Cancer | No (Reference) | 462 (52.7%) | 414 (47.3%) | 1 | - | NE | - |
| Yes | 38 (46.9%) | 43 (53.1%) | 1.26 | 0.316 | - | ||
| Family History of Cancer | No/Don’t Know (Reference) | 428 (57.5%) | 316 (42.5%) | 1 | - | 1 | - |
| Yes | 72 (33.8%) | 141 (66.2%) | 2.65 | <0.001 | 1.89 (1.30–2.73) | 0.001 | |
| Smoking Status | Never Smoked (Reference) | 473 (51.2%) | 450 (48.8%) | 1 | - | 1 | - |
| Ex-Smoker/Current Smoker | 27 (79.4%) | 7 (20.6%) | 0.27 | 0.002 | 0.28 (0.11–0.72) | 0.008 | |
| Use of Complementary Therapy | - | - | - | - | - | - | |
| Use of Complementary Therapy Index | 0 (≤50th Percentile) | 285 (64.2%) | 159 (35.8%) | 1 | - | 1 | - |
| 1–2 (>50th–75th Percentile) | 139 (55.4%) | 112 (44.6%) | 1.44 | 0.022 | 1.35 (0.93–1.98) | 0.118 | |
| ≥3 (>75th Percentile) | 76 (29.0%) | 186 (71.0%) | 4.39 | <0.001 | 2.07 (1.38–3.12) | <0.001 | |
| Recommendation from Health Professional | - | - | - | - | - | - | |
| Health Professional Recommended the Test | No/Unsure (Reference) | 481 (55.0%) | 393 (45.0%) | 1 | - | 1 | - |
| Yes | 19 (22.9%) | 64 (77.1%) | 4.12 | <0.001 | 4.04 (2.21–7.39) | <0.001 | |
| Health-Related Perceptions | - | - | - | - | - | - | |
| Perceived Health Status | Excellent/very good/good (Reference) | 180 (49.6%) | 183 (50.4%) | 1 | - | NS | - |
| Fair/Poor | 320 (53.9%) | 274 (46.1%) | 0.84 | 0.198 | - | - | |
| Thought Exercise was Good for Health | No (Reference) | 118 (52.7%) | 106 (47.3%) | 1 | - | NE | - |
| Yes | 382 (52.1%) | 351 (47.9%) | 1.02 | 0.882 | - | - | |
| Believed a Healthy Diet was Good for the Health | No (Reference) | 150 (61.5%) | 94 (38.5%) | 1 | - | NS | - |
| Yes | 350 (49.1%) | 363 (50.9%) | 1.66 | 0.001 | - | - | |
| Thought Visiting A Doctor Regularly Was Good For The Health | No (Reference) | 299 (60.3%) | 197 (39.7%) | 1 | - | 1 | - |
| Yes | 201 (43.6%) | 260 (56.4%) | 1.96 | <0.001 | 2.09 (1.51–2.88) | <0.001 | |
| Thought Visiting a Chinese Herbalist Regularly was Good for the Health | No (Reference) | 422 (59.0%) | 293 (41.0%) | 1 | - | 1 | - |
| Yes | 78 (32.2%) | 164 (67.8%) | 3.03 | <0.001 | 1.96 (1.31–2.93) | 0.001 | |
| Thought Taking Dietary Supplements was Good for the Health | No (Reference) | 399 (55.6%) | 318 (44.4%) | 1 | - | NS | - |
| Yes | 101 (42.1%) | 139 (57.9%) | 1.73 | <0.001 | - | - | |
| Perceived Susceptibility to Cancer (Range: 1 = Not at All Likely to 10 = Extremely Likely) | ≤5 (Reference) | 311 (50.2%) | 309 (49.8%) | 1 | - | NS | - |
| >5 | 24 (43.6%) | 31 (56.4%) | 1.30 | 0.355 | - | - | |
| Unsure | 165 (58.5%) | 117 (41.5%) | 0.71 | 0.020 | - | - | |
| Variables | Employment Status a | Monthly Household Income b | Any Confirmed Chronic Illness a | Perceive a Healthy Diet Is Good for Health a | Perceive Taking Dietary Supplements Is Good for Health a | Perceived Susceptibility to Cancer b |
|---|---|---|---|---|---|---|
| Age | −0.364 (p < 0.001) | 0.270 (p < 0.001) | 0.249 (p < 0.001) | −0.038 (p = 0.235) | −0.056 (p = 0.086) | 0.093 (p = 0.011) |
| Education Level | 0.216 (p < 0.001) | 0.294 (p < 0.001) | −0.117 (p < 0.001) | 0.092 (p = 0.005) | 0.094 (p = 0.004) | 0.081 (p = 0.014) |
| Marital Status | −0.005 (p = 0.887) | 0.222 (p < 0.001) | −0.175 (p < 0.001) | −0.016 (p = 0.628) | 0.011 (p = 0.734) | 0.067 (p = 0.120) |
| Family History of Cancer | 0.102 (p = 0.002) | 0.106 (p = 0.104) | −0.047 (p = 0.144) | 0.042 (p = 0.193) | 0.085 (p = 0.009) | 0.177 (p < 0.001) |
| Smoking Status | 0.031 (p = 0.339) | 0.067 (p = 0.233) | 0.018 (p = 0.571) | −0.095 (p = 0.003) | −0.007 (p = 0.832) | 0.052 (p = 0.280) |
| Use of complementary Therapy Index | 0.121 (p < 0.001) | 0.148 (p < 0.001) | −0.018 (p = 0.583) | 0.132 (p < 0.001) | 0.149 (p < 0.001) | 0.108 (p < 0.001) |
| Health Professional’s Recommendationt | 0.080 (p = 0.013) | 0.116 (p = 0.005) | 0.026 (p = 0.427) | 0.044 (p = 0.174) | 0.062 (p = 0.057) | 0.074 (p = 0.072) |
| Perceives Visiting a Doctor Regularly as Good for Health | 0.003 (p = 0.924) | 0.018 (p = 0.962) | 0.216 (p < 0.001) | 0.204 (p < 0.001) | 0.142 (p < 0.001) | 0.033 (p = 0.595) |
| Perceived Visiting a Chinese Herbalist Regularly as Good for Health | 0.109 (p = 0.001) | 0.102 (p = 0.019) | 0.017 (p = 0.601) | 0.114 (p < 0.001) | 0.129 (p < 0.001) | 0.083 (p = 0.037) |
| Factors | Ever Had a Cervical Smear Test | ORU | p-Value | ORA (95% CI) | p-Value | ||
|---|---|---|---|---|---|---|---|
| No (n = 261) | Yes (n = 388) | ||||||
| Demographic Characteristics | - | - | - | - | - | - | |
| Age (Years) | 50–59 (Reference) | 141 (33.8%) | 276 (66.2%) | 1 | - | 1 | - |
| 60–69 | 120 (51.7%) | 112 (48.3%) | 0.48 | <0.001 | 0.53 (0.36–0.78) | 0.001 | |
| Education Level | Primary or Below (Reference) | 129 (49.4%) | 132 (50.6%) | 1 | - | 1 | - |
| Secondary | 113 (36.5%) | 197 (63.5%) | 1.70 | 0.002 | 1.45 (0.98–2.13) | 0.062 | |
| Matriculation or above | 18 (23.7%) | 58 (76.3%) | 3.15 | <0.001 | 2.67 (1.38–5.16) | 0.004 | |
| Employment Status | Unemployed (Reference) | 212 (41.8%) | 295 (58.2%) | 1 | - | NS | - |
| Employed | 49 (34.8%) | 92 (65.2%) | 1.35 | 0.131 | - | - | |
| Monthly Household Income (HK$) | <10,000 (Reference) | 84 (54.5%) | 70 (45.5%) | 1 | - | NS | - |
| 10,000–29,999 | 63 (36.0%) | 112 (64.0%) | 2.13 | 0.001 | - | - | |
| ≥30,000 | 23 (23.2%) | 76 (76.8%) | 3.97 | <0.001 | - | - | |
| Don’t Know/Decline to Disclose | 85 (40.7%) | 124 (59.3%) | 1.75 | 0.009 | - | - | |
| Marital Status | Single/Divorced/Widowed (Reference) | 71 (53.4%) | 62 (46.6%) | 1 | - | 1 | - |
| Married/Cohabiting | 188 (37.0%) | 320 (63.0%) | 1.95 | 0.001 | 2.31 (1.46–3.64) | <0.001 | |
| Health Status | - | - | - | - | - | - | |
| Any Confirmed Chronic Illness | No (Reference) | 152 (37.8%) | 250 (62.2%) | 1 | - | NS | - |
| Yes | 109 (44.1%) | 138 (55.9%) | 0.77 | 0.111 | - | - | |
| Ever Had a Serious Disease or Cancer | No (Reference) | 236 (40.1%) | 353 (59.9%) | 1 | - | NE | - |
| Yes | 25 (41.7%) | 35 (58.3%) | 0.94 | 0.810 | - | - | |
| Family History of Cancer | No/Don’t Know (Reference) | 214 (45.0%) | 262 (55.0%) | 1 | - | 1 | - |
| Yes | 47 (27.2%) | 126 (72.8%) | 2.19 | <0.001 | 1.81 (1.18–2.79) | 0.006 | |
| Smoking Status | Never Smoked (Reference) | 247 (39.3%) | 382 (60.7%) | 1 | - | 1 | - |
| Ex-Smoker/Current Smoker | 14 (70.0%) | 6 (30.0%) | 0.28 | 0.009 | 0.28 (0.10–0.83) | 0.021 | |
| Use of Complementary Therapy | - | - | - | - | - | - | |
| Use of Complementary Therapy Index | 0 (≤50th Percentile) | 147 (54.4%) | 123 (45.6%) | 1 | - | 1 | - |
| 1–2 (>50th–75th Percentile) | 61 (38.9%) | 96 (61.1%) | 1.88 | 0.002 | 1.68 (1.06–2.66) | 0.027 | |
| ≥3 (>75th Percentile) | 53 (23.9%) | 169 (76.1%) | 3.81 | <0.0001 | 2.51 (1.56–4.04) | <0.001 | |
| Recommendation from Health Professional | - | - | - | - | - | - | |
| Health Professional Recommended the Test | No/Unsure (Reference) | 249 (42.7%) | 334 (57.3%) | 1 | - | 1 | - |
| Yes | 12 (18.2%) | 54 (81.8%) | 3.36 | <0.001 | 3.38 (1.68–6.79) | 0.001 | |
| Health-Related Perceptions | - | - | - | - | - | - | |
| Perceived Health Status | Excellent/very Good/Good (Reference) | 95 (38.3%) | 153 (61.7%) | 1 | - | NE | - |
| Fair/Poor | 166 (41.4%) | 235 (58.6%) | 0.88 | 0.435 | - | - | |
| Perceived Exercise as Good for the Health | No (Reference) | 74 (42.5%) | 100 (57.5%) | 1 | - | NE | - |
| Yes | 187 (39.4%) | 288 (60.6%) | 1.14 | 0.467 | - | - | |
| Perceived a Healthy Diet as Good for the Health | No (Reference) | 76 (49.4%) | 78 (50.6%) | 1 | - | NS | - |
| Yes | 185 (37.4%) | 310 (62.6%) | 1.63 | 0.008 | - | - | |
| Perceive Visiting a Doctor Regularly as Good for the Health | No (Reference) | 183 (51.4%) | 173 (48.6%) | 1 | - | 1 | - |
| Yes | 78 (26.6%) | 215 (73.4%) | 2.92 | <0.001 | 2.65 (1.81–3.87) | <0.001 | |
| Perceived Visiting a Chinese Herbalist Regularly as Good for the Health | No (Reference) | 220 (47.8%) | 240 (52.2%) | 1 | - | 1 | - |
| Yes | 41 (21.7%) | 148 (78.3%) | 3.31 | <0.001 | 1.90 (1.18–3.06) | 0.009 | |
| Perceived Taking Dietary Supplements as Good for the Health | No (Reference) | 211 (44.1%) | 267 (55.9%) | 1 | - | NS | - |
| Yes | 50 (29.2%) | 121 (70.8%) | 1.91 | 0.001 | - | - | |
| Perceived Susceptibility to Cancer (Range: 1 = not at All Likely to 10 = Extremely Likely) | ≤5 (Reference) | 160 (37.6%) | 265 (62.4%) | 1 | - | NS | - |
| >5 | 19 (41.3%) | 27 (58.7%) | 0.86 | 0.628 | - | - | |
| Unsure | 82 (46.1%) | 96 (53.9%) | 0.71 | 0.055 | - | - | |
© 2016 by the authors; licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC-BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Chan, C.W.H.; Choi, K.C.; Wong, R.S.; Chow, K.M.; So, W.K.W.; Leung, D.Y.P.; Lam, W.W.T.; Goggins, W. Examining the Cervical Screening Behaviour of Women Aged 50 or above and Its Predicting Factors: A Population-Based Survey. Int. J. Environ. Res. Public Health 2016, 13, 1195. https://doi.org/10.3390/ijerph13121195
Chan CWH, Choi KC, Wong RS, Chow KM, So WKW, Leung DYP, Lam WWT, Goggins W. Examining the Cervical Screening Behaviour of Women Aged 50 or above and Its Predicting Factors: A Population-Based Survey. International Journal of Environmental Research and Public Health. 2016; 13(12):1195. https://doi.org/10.3390/ijerph13121195
Chicago/Turabian StyleChan, Carmen W. H., Kai Chow Choi, Rosa S. Wong, Ka Ming Chow, Winnie K. W. So, Doris Y. P. Leung, Wendy W. T. Lam, and William Goggins. 2016. "Examining the Cervical Screening Behaviour of Women Aged 50 or above and Its Predicting Factors: A Population-Based Survey" International Journal of Environmental Research and Public Health 13, no. 12: 1195. https://doi.org/10.3390/ijerph13121195
APA StyleChan, C. W. H., Choi, K. C., Wong, R. S., Chow, K. M., So, W. K. W., Leung, D. Y. P., Lam, W. W. T., & Goggins, W. (2016). Examining the Cervical Screening Behaviour of Women Aged 50 or above and Its Predicting Factors: A Population-Based Survey. International Journal of Environmental Research and Public Health, 13(12), 1195. https://doi.org/10.3390/ijerph13121195






