Cardiovascular Mortality Associated with Low and High Temperatures: Determinants of Inter-Region Vulnerability in China
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Area
| Province | Region |
|---|---|
| Anhui Province | Chaohu City, Yushan District of Ma’anshan City, Daguan District of Anqing City, Tianchang City, Mengcheng County, and Jing County |
| Hunan Province | Tianxin District of Changsha City, Liuyang City, Pingjiang County, Wuling District of Changde City, Suxian District of Chenzhou City, Hongjiang City, and Fenghuang County |
| Guangxi Zhuang Autonomous Region | Binyang County, Liubei District of Liuzhou City, Xiufeng District of Guilin City, Hepu County, Lingyun County, and Luocheng Mulam Autonomous County |
| Hainan Province | Meilan District of Haikou City, and An’ding County |
| Tibet Autonomous Region | Chengguan District of Lasa City, Mozhugongka County, Naidong County, Jiangzi County, and Milin County |

2.2. Source of the Data
2.3. Statistical Analysis
2.3.1. First Stage: Using a Poisson Generalized Additive Model (GAM) to Calculate the Percent Changes in Cardiovascular Mortality at Low and High Temperatures
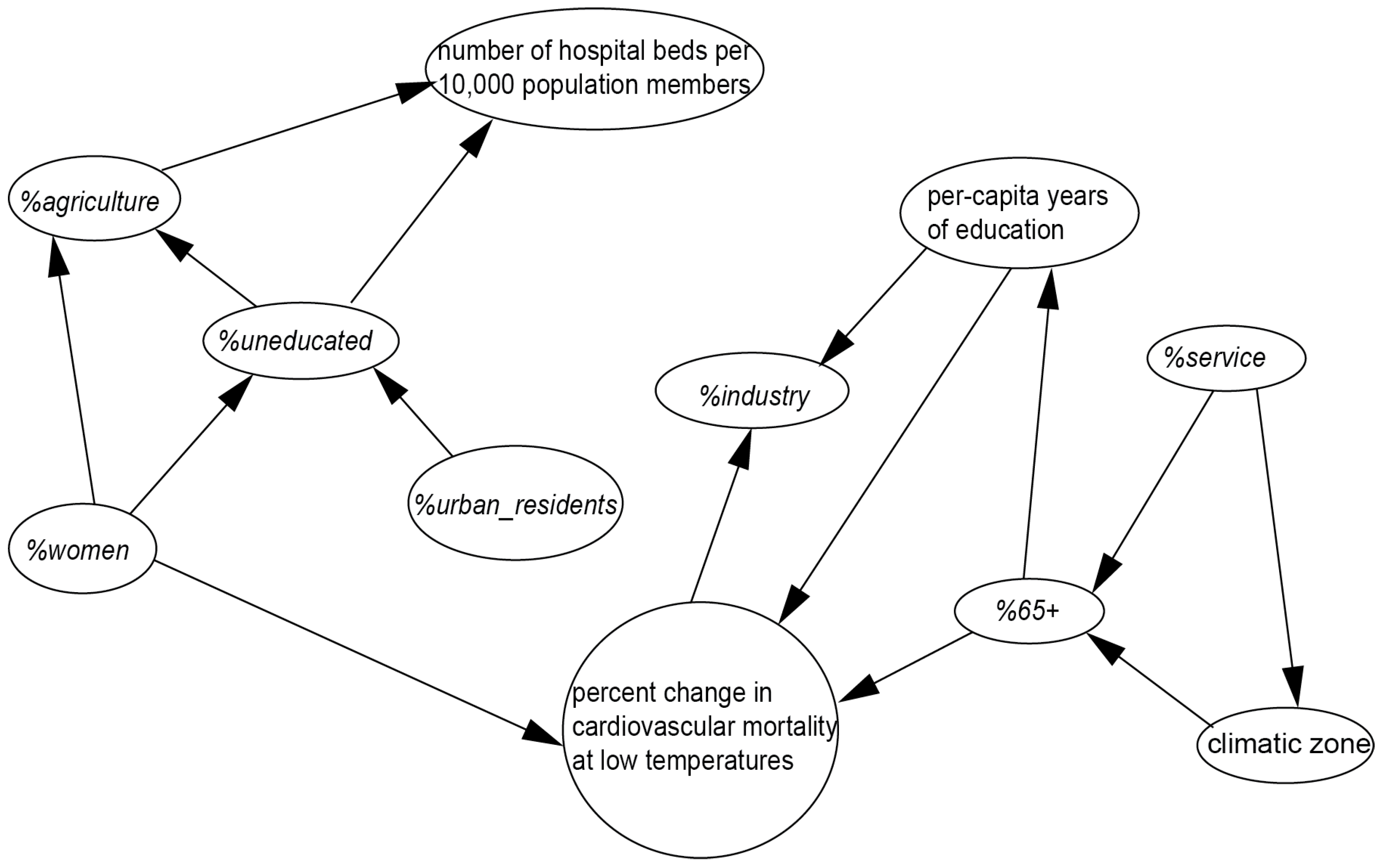
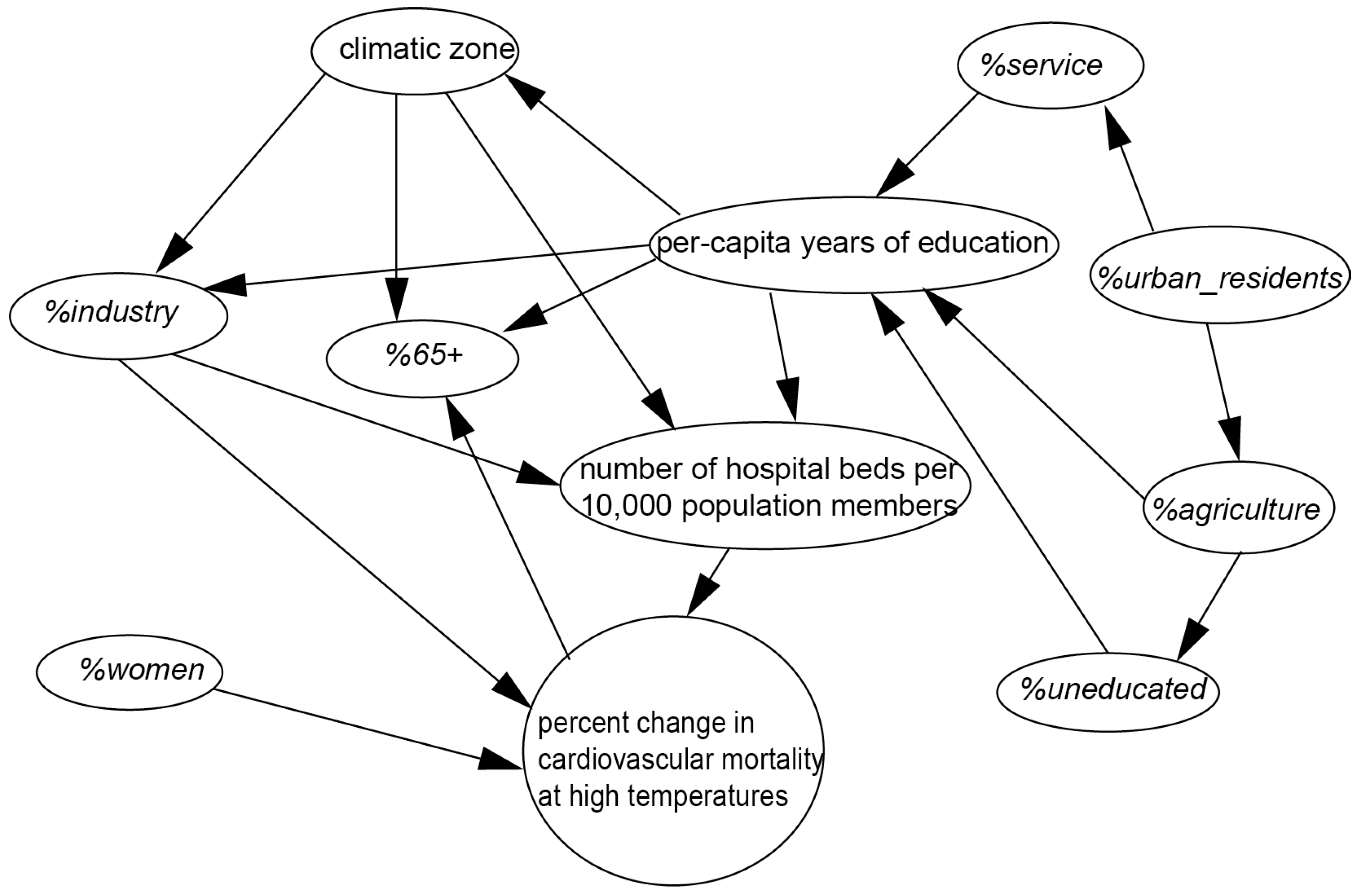
2.3.2. Second Stage: Using a Bayesian Network (BN) to Identify Socioeconomic and Demographic Factors responsible for Variation of the Temperature Effect on Cardiovascular Mortality
3. Results
| Quantitative Factors | State and Intervals | Percent Change in Cardiovascular Mortality at Low Temperatures | |
|---|---|---|---|
| Low Risk | High Risk | ||
| Per capita years of education | low level [5.18, 5.25] | 0.500 | 0.500 |
| high level (5.25, 12.31] | 0.658 | 0.342 | |
| %65+ | low level [3.49, 5.65] | 0.310 | 0.690 |
| high level (5.65, 12.68] | 0.727 | 0.273 | |
| %women | low level [46.66, 50.08] | 0.619 | 0.381 |
| high level (50.08, 50.94] | 0.791 | 0.209 | |
| Quantitative Factors | State and Intervals | Percent Change in Cardiovascular Mortality at High Temperatures | |
|---|---|---|---|
| Low Risk | High Risk | ||
| Number of hospital beds per 10,000 people | low level [4.95, 30.71] | 0.401 | 0.599 |
| high level (30.71, 109.38] | 0.819 | 0.181 | |
| %industry | low level [1.02, 6.36] | 0.195 | 0.805 |
| middle level (6.36, 23.14] | 0.870 | 0.130 | |
| high level (23.14, 51.24) | 0.703 | 0.297 | |
| %women | low level [46.66, 50.83] | 0.521 | 0.479 |
| high level (50.83, 50.94] | 0.454 | 0.546 | |
| Target Variables | State | pd | pf | Accuracy |
|---|---|---|---|---|
| Percent change in cold-related cardiovascular mortality | low risk | 0.882 | 0.333 | 0.808 |
| high risk | 0.667 | 0.118 | 0.808 | |
| Percent change in heat-related cardiovascular mortality | low risk | 0.947 | 0.143 | 0.923 |
| high risk | 0.857 | 0.063 | 0.923 |
4. Discussion
5. Conclusions
Supplementary Files
Supplementary File 1Acknowledgments
Author Contributions
Conflicts of Interest
References
- Intergovernmental Panel on Climate Change (IPCC). Climate Change 2013: The Physical Science Basis; Cambridge University Press: Cambridge, UK, 2013. [Google Scholar]
- Patz, J.A.; Campbell-Lendrum, D.; Holloway, T.; Foley, J.A. Impact of regional climate change on human health. Nature 2005, 438, 310–317. [Google Scholar] [CrossRef] [PubMed]
- Basu, R.; Samet, J.M. Relation between elevated ambient temperature and mortality: A review of the epidemiologic evidence. Epidemiol. Rev. 2002, 24, 190–202. [Google Scholar] [CrossRef] [PubMed]
- Tian, Z.; Li, S.; Zhang, J.; Jaakkola, J.J.; Guo, Y. Ambient temperature and coronary heart disease mortality in Beijing, China: A time series study. Environ. Health 2012, 11, 56. [Google Scholar] [CrossRef] [PubMed]
- Kan, H.D.; Jia, J.; Chen, B.H. Temperature and daily mortality in Shanghai: A time-series study. Biomed. Environ. Sci. 2003, 16, 133–139. [Google Scholar] [PubMed]
- Guo, Y.M.; Barnett, A.G.; Pan, X.C.; Yu, W.W.; Tong, S.L. The impact of temperature on mortality in Tianjin, China: A case-crossover design with a distributed lag nonlinear model. Environ. Health Perspect. 2011, 119, 1719–1725. [Google Scholar] [CrossRef] [PubMed]
- Yang, J.; Ou, C.Q.; Ding, Y.; Zhou, Y.X.; Chen, P.Y. Daily temperature and mortality: A study of distributed lag non-linear effect and effect modification in Guangzhou. Environ. Health 2012, 11. [Google Scholar] [CrossRef]
- Goggins, W.B.; Chan, E.Y.; Ng, E.; Ren, C.; Chen, L. Effect modification of the association between short-term meteorological factors and mortality by urban heat islands in Hong Kong. PLoS ONE 2012, 7. [Google Scholar] [CrossRef] [PubMed]
- China Meteorological Administration. Climate and Environment in China; Meteorology Press: Beijing, China, 2006. (in Chinese)
- Jiang, Z.; Song, J.; Li, L.; Chen, W.; Wang, Z.; Wang, J. Extreme climate events in China: IPCC-AR4 model evaluation and projection. Clim. Chang. 2012, 110, 385–401. [Google Scholar] [CrossRef]
- Zhai, P.; Pan, X. Trends in temperature extremes during 1951–1999 in China. Geophys. Res. Lett. 2003, 37. [Google Scholar] [CrossRef]
- Martens, W.J.M. Climate change, thermal stress and mortality changes. Soc. Sci. Med. 1998, 46, 331–334. [Google Scholar] [CrossRef] [PubMed]
- Curriero, F.C.; Heiner, K.S.; Samet, J.M.; Zeger, S.L.; Strug, L.; Patz, J.A. Temperature and mortality in 11 cities of the Eastern United States. Am. J. Epidemiol. 2002, 155, 80–87. [Google Scholar] [CrossRef] [PubMed]
- Yu, W.; Hu, W.; Mengersen, K.; Guo, Y.; Pan, X.; Connell, D.; Tong, S. Time course of temperature effects on cardiovascular mortality in Brisbane, Australia. Heart 2011, 97, 1089–1093. [Google Scholar] [CrossRef] [PubMed]
- Huang, J.; Wang, J.; Yu, W. The lag effects and vulnerabilities of temperature effects on cardiovascular disease mortality in a subtropical climate zone in China. Int. J. Environ. Res. Public Health 2014, 11, 3982–3994. [Google Scholar] [CrossRef] [PubMed]
- Doyon, B.; Belanger, D.; Gosselin, P. The potential impact of climate change on annual and seasonal mortality for three cities in Quebec, Canada. Int. J. Health Geogr. 2008, 7, 23. [Google Scholar] [CrossRef] [PubMed]
- Dominici, F.; McDermott, A.; Zeger, S.L.; Samet, J.M. On the use of generalized additive models in time-series studies of air pollution and health. Am. J. Epidemiol. 2002, 156, 193–203. [Google Scholar] [CrossRef] [PubMed]
- Wu, P.C.; Lin, C.Y.; Lung, S.C.; Guo, H.R.; Chou, C.H.; Su, H.J. Cardiovascular mortality during heat and cold events: Determinants of regional vulnerability in Taiwan. Occup. Environ. Med. 2010, 68, 525–530. [Google Scholar] [CrossRef] [PubMed]
- Li, L.; Wang, J.; Leung, H.; Jiang, C. Assessment of catastrophic risk using Bayesian network constructed from domain knowledge and spatial data. Risk Anal. 2010, 30, 1157–1175. [Google Scholar] [CrossRef] [PubMed]
- Liao, Y.L.; Wang, J.F.; Guo, Y.Q.; Zheng, X.Y. Risk assessment of human neural tube defects using a Bayesian belief network. Stoch. Environ. Res. Risk Assess. 2010, 24, 93–100. [Google Scholar] [CrossRef]
- Population Census Office under the State Council and the Department of Population and Employment Statistics National Bureau of Statistics. Tabulation on the 2010 Population Census of the People’s Republic of China by County; China Statistics Press: Beijing, China, 2010.
- National Bureau of Statistics of China. China City Statistical Yearbooks; China Statistics: Beijing, China, 2010.
- National Bureau of Statistics of China. China County Statistical Yearbooks; China Statistics: Beijing, China, 2010.
- National Bureau of Statistics of China. China Statistical Yearbooks for Regional Economy; China Statistics: Beijing, China, 2010.
- Cheng, X.S.; Su, H. Effects of climatic temperature stress on cardiovascular diseases. Eur. J. Intern. Med. 2010, 21, 164–167. [Google Scholar] [CrossRef] [PubMed]
- Li, Y.; Lan, L.; Wang, Y.; Yang, C.; Tang, W.; Gui, G.; Luo, S.; Cheng, Y.; Liu, Y.; Liu, J.; et al. Extremely cold and hot temperatures increase the risk of diabetes mortality in metropolitan areas of two Chinese cities. Environ. Res. 2014, 134, 91–97. [Google Scholar] [CrossRef] [PubMed]
- Ou, C.Q.; Song, Y.F.; Yang, J.; Chau, P.Y.K.; Yang, L.; Chen, P.Y.; Wong, C.M. Excess winter mortality and cold temperatures in a subtropical city, Guangzhou, China. PLoS ONE 2013, 8. [Google Scholar] [CrossRef] [PubMed]
- Yu, W.; Pan, X.; Tong, S.; Wang, X.; Ye, X. Assessing the threshold temperatures among different age and cause-of-deaths. In Proceedings of the International Conference on Environmental, Biomedical and Biotechnology, Shanghai, China, 19–21 August 2011; IACSIT Press: Singapore, 2011; pp. 35–40. [Google Scholar]
- Braga, A.L.F.; Zanobetti, A.; Schwartz, J. The time course of weather-related deaths. Epidemiology 2001, 12, 662–667. [Google Scholar] [CrossRef] [PubMed]
- Peng, R.D.; Dominici, F.; Louis, T.A. Model choice in time series studies of air pollution and mortality. J. R. Stat. Soc.: Ser. A (Stat. Soc.) 2006, 169, 179–203. [Google Scholar] [CrossRef]
- Chung, J.Y.; Honda, Y.; Hong, Y.C.; Pan, X.C.; Guo, Y.L.; Kim, H. Ambient temperature and mortality: An international study in four capital cites of East Asia. Sci. Total Environ. 2009, 408, 390–396. [Google Scholar] [CrossRef] [PubMed]
- Dominici, F.; McDermott, A.; Hastie, T.J. Improved semiparametric time series models of air pollution and mortality. J. Am. Stat. Assoc. 2004, 99, 938–948. [Google Scholar] [CrossRef]
- Akaike, H. Information theory and an extension of the maximum likelihood principle. In Proceedings of the Second International Symposium on Information Theory, Tsahkadsor, Armenia, 2–8 September 1971; Petrov, B., Caski, F., Eds.; Akademinai Kiado: Budapest, Hungary, 1973; pp. 267–281. [Google Scholar]
- Ma, W.; Chen, R.; Kan, H. Temperature-related mortality in 17 large Chinese cities: How heat and cold affect mortality in China. Environ. Res. 2014, 134, 127–133. [Google Scholar] [CrossRef] [PubMed]
- Samet, J.; Zeger, S.; Dominici, F.; Curriero, F.; Coursac, I.; Dockery, D.; Schwartz, J.; Zanobetti, A. The national morbidity, mortality, and air pollution study. In Part II: Morbidity and Mortality from Air Pollution in the United States; Research Report; Health Effects Institute: Boston, MA, USA, 2000. [Google Scholar]
- Huynen, M.M.; Martens, P.; Schram, D.; Weijenberg, M.P.; Kunst, A.E. The impact of heat waves and cold spells on mortality rates in the Dutch population. Environ. Health Perspect. 2001, 109, 463–470. [Google Scholar] [CrossRef] [PubMed]
- Iñiguez, C.; Ballester, F.; Ferrandiz, J.; Pérez-Hoyos, S.; Sáez Zafra, M.; López, A. Relation between temperature and mortality in thirteen Spanish cities. Int. J. Environ. Res. Public Health 2010, 7, 3196–3210. [Google Scholar] [CrossRef] [PubMed]
- Gouveia, N.; Hajat, S.; Armstrong, B. Socioeconomic differentials in the temperature-mortality relationship in Sao Paulo, Brazil. Int. J. Epidemiol. 2003, 32, 390–397. [Google Scholar] [CrossRef] [PubMed]
- Green, R.S.; Basu, R.; Malig, B.; Broadwin, R.; Kim, J.J.; Ostro, B. The effect of temperature on hospital admissions in nine California counties. Int. J. Public Health 2010, 55, 113–121. [Google Scholar] [CrossRef] [PubMed]
- Wood, S. Mixed GAM Computation Vehicle with GCV/AIC/REML Smoothness Estimation (R Package Version 1.8–0). Available online: http://cran.r-project.org/web/packages/mgcv/mgcv.pdf (accessed on 14 May 2015).
- Jensen, F.V. An Introduction to Bayesian Networks; University College London Press: London, UK, 1996. [Google Scholar]
- Neapolitan, R.E. Learning Bayesian Networks; Prentice Hall: New York, NY, USA, 2004. [Google Scholar]
- Bouckaert, R.R. Bayesian Belief Network: From Construction to Inference. Ph.D. Thesis, Utrecht University, Utrecht, The Netherlands, 1995. [Google Scholar]
- O’Neill, M.S.; Zanobetti, A.; Schwartz, J. Modifiers of the temperature and mortality association in seven US cities. Am. J. Epidemiol. 2003, 157, 1074–1082. [Google Scholar] [CrossRef] [PubMed]
- Atsumi, A.; Ueda, K.; Irie, F.; Sairenchi, T.; Iimura, K.; Watanabe, H.; Iso, H.; Ota, H.; Aonuma, K. Relationship between cold temperature and cardiovascular mortality, with assessment of effect modification by individual characteristics—Ibaraki prefectural health study. Circ. J. 2013, 77, 1854–1861. [Google Scholar] [CrossRef] [PubMed]
- Kysely, J.; Pokorna, L.; Kyncl, J.; Kriz, B. Excess cardiovascular mortality associated with cold spells in the Czech Republic. BMC Public Health 2009, 9, 19. [Google Scholar] [CrossRef] [PubMed]
- O’Neill, M.S.; Hajat, S.; Zanobetti, A.; Ramirez-Aguilar, M.; Schwartz, J. Impact of control for air pollution and respiratory epidemics on the estimated associations of temperature and daily mortality. Int. J. Biometeorol. 2005, 50, 121–129. [Google Scholar] [CrossRef] [PubMed]
- Johnson, D.P.; Wilson, J.S.; Luber, G.C. Socioeconomic indicators of heat-related health risk supplemented with remotely sensed data. Int. J. Health Geogr. 2009, 8, 57. [Google Scholar] [CrossRef] [PubMed]
- Son, J.Y.; Lee, J.T.; Anderson, G.B.; Bell, M.L. The impact of heat waves on mortality in seven major cities in Korea. Environ. Health Perspect. 2012, 120, 566–571. [Google Scholar] [CrossRef] [PubMed]
- Bell, M.L.; O’Neill, M.S.; Ranjit, N.; Borja-Aburto, V.H.; Cifuentes, L.A.; Gouveia, N.C. Vulnerability to heat-related mortality in Latin America: A case-crossover study in Sao Paulo, Brazil, Santiago, Chile and Mexico City, Mexico. Int. J. Epidemiol. 2008, 37, 796–804. [Google Scholar] [CrossRef] [PubMed]
- Donaldson, G.C.; Robinson, D.; Allaway, S.L. An analysis of arterial disease mortality and BUPA health screening data in men, in relation to outdoor temperature. Clin. Sci. 1997, 92, 261–268. [Google Scholar] [PubMed]
- Liu, L.; Breitner, S.; Pan, X.; Franck, U.; Leitte, A.M.; Wiedensohler, A.; von Klot, S.; Wichmann, H.E.; Peters, A.; Schneider, A. Associations between air temperature and cardio-respiratory mortality in the urban area of Beijing, China: A time-series analysis. Environ. Health 2011, 10, 51. [Google Scholar] [CrossRef] [PubMed]
- Basu, R. High ambient temperature and mortality: A review of epidemiologic studies from 2001 to 2008. Environ. Health 2009, 8, 40. [Google Scholar] [CrossRef] [PubMed]
- Zanobetti, A.; Schwartz, J. Temperature and mortality in nine US cities. Epidemiology 2008, 19, 563–570. [Google Scholar] [CrossRef] [PubMed]
- Basu, R.; Dominici, F.; Samet, J.M. Temperature and mortality among the elderly in the United States: A comparison of epidemiologic methods. Epidemiology 2005, 16, 58–66. [Google Scholar] [CrossRef] [PubMed]
- Stafoggia, M.; Forastiere, F.; Agostini, D.; Biggeri, A.; Bisanti, L.; Cadum, E.; Caranci, N.; de’ Donato, F.; de Lisio, S.; de Maria, M.; et al. Vulnerability to heat-related mortality: A multicity, population-based, case-crossover analysis. Epidemiology 2006, 17, 315–323. [Google Scholar] [CrossRef] [PubMed]
- Vaneckova, P.; Beggs, P.J.; de Dear, R.J.; McCracken, K.W. Effect of tem perature on mortality during the six warmer months in Sydney, Australia, between 1993 and 2004. Environ. Res. 2008, 108, 361–369. [Google Scholar] [CrossRef] [PubMed]
- Ren, C.; Tong, S. Temperature modifies the health effects of particulate matter in Brisbane, Australia. Int. J. Biometeorol. 2006, 51, 87–96. [Google Scholar] [CrossRef] [PubMed]
- Kalkstein, L.S.; Greene, J.S. An evaluation of climate/mortality relationships in large U.S. cities and the possibleimpacts of a climate change. Environ. Health Perspect. 1997, 105, 84–93. [Google Scholar] [CrossRef] [PubMed]
- Kunst, A.E.; Looman, C.W.; Mackenbach, J.P. Outdoor air temperature and mortality in the Netherlands: A time-series analysis. Am. J. Epidemiol. 1993, 137, 331–341. [Google Scholar] [PubMed]
- Gosling, S.N.; Lowe, J.A.; McGregor, G.R.; Pelling, M.; Malamud, B.D. Associations between elevated atmospheric temperature and human mortality: A critical review of the literature. Clim. Chang. 2009, 92, 299–341. [Google Scholar] [CrossRef]
© 2015 by the authors; licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Yang, X.; Li, L.; Wang, J.; Huang, J.; Lu, S. Cardiovascular Mortality Associated with Low and High Temperatures: Determinants of Inter-Region Vulnerability in China. Int. J. Environ. Res. Public Health 2015, 12, 5918-5933. https://doi.org/10.3390/ijerph120605918
Yang X, Li L, Wang J, Huang J, Lu S. Cardiovascular Mortality Associated with Low and High Temperatures: Determinants of Inter-Region Vulnerability in China. International Journal of Environmental Research and Public Health. 2015; 12(6):5918-5933. https://doi.org/10.3390/ijerph120605918
Chicago/Turabian StyleYang, Xunfeng, Lianfa Li, Jinfeng Wang, Jixia Huang, and Shijun Lu. 2015. "Cardiovascular Mortality Associated with Low and High Temperatures: Determinants of Inter-Region Vulnerability in China" International Journal of Environmental Research and Public Health 12, no. 6: 5918-5933. https://doi.org/10.3390/ijerph120605918
APA StyleYang, X., Li, L., Wang, J., Huang, J., & Lu, S. (2015). Cardiovascular Mortality Associated with Low and High Temperatures: Determinants of Inter-Region Vulnerability in China. International Journal of Environmental Research and Public Health, 12(6), 5918-5933. https://doi.org/10.3390/ijerph120605918







