The Role of Seawater and Saline Solutions in Treatment of Upper Respiratory Conditions
Abstract
1. Introduction
- Composition of solution in context of differences between saline and solutions based on seawater.
- Mechanism of action in nasal cavity and elsewhere.
- Safety and efficacy of use in different indications.
2. Composition of Saline/Seawater Preparations
3. Mechanism of Action
4. Aspects of Saline/Seawater in Human Use
4.1. Safety
4.2. Efficacy
4.2.1. Chronic Sinusitis
4.2.2. Allergic Rhinitis
4.2.3. Other Indications
4.2.4. The Place of Saline/Seawater Preparations in the COVID-19 Pandemic
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Meera, S.; Vandana Rani, M.; Sreedhar, C.; Robin, D.T. A Review on the Therapeutic Effects of NetiKriya with Special Reference to JalaNeti. J. Ayurveda Integr. Med. 2020, 11, 185–189. [Google Scholar] [CrossRef]
- Khianey, R.; Oppenheimer, J. Is Nasal Saline Irrigation All It Is Cracked up to Be? Ann. Allergy Asthma Immunol. 2012, 109, 20–28. [Google Scholar] [CrossRef]
- Principi, N.; Esposito, S. Nasal Irrigation: An Imprecisely Defined Medical Procedure. Int. J. Environ. Res. Public Health 2017, 14, 516. [Google Scholar] [CrossRef]
- Ho, E.Y.; Cady, K.A.; Robles, J.S. A Case Study of the Neti Pot’s Rise, Americanization, and Rupture as Integrative Medicine in U.S. Media Discourse. Health Commun. 2016, 31, 1181–1192. [Google Scholar] [CrossRef]
- Baraniuk, J.N.; Ali, M.; Yuta, A.; Fang, S.Y.; Naranch, K. Hypertonic Saline Nasal Provocation Stimulates Nociceptive Nerves, Substance P Release, and Glandular Mucous Exocytosis in Normal Humans. Am. J. Respir. Crit. Care Med. 1999, 160, 655–662. [Google Scholar] [CrossRef]
- National Ocean Service website What Is the Forchhammer’s Principle? Available online: https://oceanservice.noaa.gov/facts/forchhammers-principle.html (accessed on 1 December 2021).
- Cheng, L.; Trenberth, K.E.; Gruber, N.; Abraham, J.P.; Fasullo, J.T.; Li, G.; Mann, M.E.; Zhao, X.; Zhu, J. Improved Estimates of Changes in Upper Ocean Salinity and the Hydrological Cycle. J. Clim. 2020, 33, 10357–10381. [Google Scholar] [CrossRef]
- Bindoff, N.L.; Cheung, W.W.L.; Kairo, J.G.; Arístegui, J.; Guinder, V.A.; Hallberg, R.; Hilmi, N.; Jiao, N.; Karim, M.S.; Levin, L.; et al. Changing Ocean, Marine Ecosystems, and Dependent Communities; IPCC: Geneva, Switzerland, 2019. [Google Scholar]
- Lyman, J.; Fleming, R.H. Composition of Sea Water. J. Mar. Res. 1940, 3, 134–146. [Google Scholar]
- Cox, R.A.; Culkin, F.; Riley, J.P.; Cox, R.A.; Culkin, F.; Riley, J.P. The Electrical Conductivity/Chlorinity Relationship in Natural Sea Water. DSRA 1967, 14, 203–220. [Google Scholar] [CrossRef]
- Morris, A.W.; Riley, J.P. The Bromide/Chlorinity and Sulphate/Chlorinity Ratio in Sea Water. Deep. Sea Res. Oceanogr. Abstr. 1966, 13, 699–705. [Google Scholar] [CrossRef]
- Millero, F.J. Chemical Oceanography, 4th ed.; CRC Press: Boca Raton, FL, USA, 2013. [Google Scholar]
- Štanfel, D. Comparasion of Ion Chromatography with Other Methods in Sea Water Analysis of the Adriatic Coast; University of Zagreb: Zagreb, Croatia, 2006. [Google Scholar]
- Bhalla, A.; Sankaralingam, S.; Dundas, R.; Swaminathan, R.; Wolfe, C.D.A.; Rudd, A.G. Influence of Raised Plasma Osmolality on Clinical Outcome after Acute Stroke. Stroke 2000, 31, 2043–2048. [Google Scholar] [CrossRef]
- Trimble, A.T.; Whitney Brown, A.; Laube, B.L.; Lechtzin, N.; Zeman, K.L.; Wu, J.; Ceppe, A.; Waltz, D.; Bennett, W.D.; Donaldson, S.H. Hypertonic Saline Has a Prolonged Effect on Mucociliary Clearance in Adults with Cystic Fibrosis. J. Cyst. Fibros. 2018, 17, 650–656. [Google Scholar] [CrossRef]
- Cingi, C.; Halis Unlu, H.; Songu, M.; Yalcin, S.; Topcu, I.; Cakli, H.; Bal, C. Seawater Gel in Allergic Rhinitis: Entrapment Effect and Mucociliary Clearance Compared with Saline. Ther. Adv. Respir. Dis. 2010, 4, 13–18. [Google Scholar] [CrossRef]
- Bonnomet, A.; Luczka, E.; Coraux, C.; de Gabory, L. Non-Diluted Seawater Enhances Nasal Ciliary Beat Frequency and Wound Repair Speed Compared to Diluted Seawater and Normal Saline. Int. Forum Allergy Rhinol. 2016, 6, 1062–1068. [Google Scholar] [CrossRef]
- Bennett, W.D.; Wu, J.; Fuller, F.; Balcazar, J.R.; Zeman, K.L.; Duckworth, H.; Donn, K.H.; O’Riordan, T.G.; Boucher, R.C.; Donaldson, S.H. Duration of Action of Hypertonic Saline on Mucociliary Clearance in the Normal Lung. J. Appl. Physiol. 2015, 118, 1483–1490. [Google Scholar] [CrossRef]
- Pavia, D.; Thomson, M.L.; Clarke, S.W. Enhanced Clearance of Secretions from the Human Lung after the Administration of Hypertonic Saline Aerosol. Am. Rev. Respir. Dis. 1978, 117, 199–203. [Google Scholar] [CrossRef]
- Bastier, P.L.; Lechot, A.; Bordenave, L.; Durand, M.; de Gabory, L. Nasal Irrigation: From Empiricism to Evidence-Based Medicine. A Review. Eur. Ann. Otorhinolaryngol. Head Neck Dis. 2015, 132, 281–285. [Google Scholar] [CrossRef]
- Quraishi, M.S.; Jones, N.S.; Mason, J. The Rheology of Nasal Mucus: A Review. Clin. Otolaryngol. 1998, 23, 403–413. [Google Scholar] [CrossRef]
- Sleigh, M.A. Ciliary Adaptations for the Propulsion of Mucus. Biorheology 1990, 27, 527–532. [Google Scholar] [CrossRef]
- Mahakit, P.; Pumhlrun, P. A Preliminary Study of Nasal Mucociliary Clearance in Smokers, Sinusitis and Allergic Rhinitis Patients. Asian Pac. J. Allergy Immunol. 1995, 13, 119–121. [Google Scholar]
- Passàli, D.; Ferri, R.; Becchini, G.; Passàli, G.C.; Bellussi, L. Alterations of Nasal Mucociliary Transport in Patients with Hypertrophy of the Inferior Turbinates, Deviations of the Nasal Septum and Chronic Sinusitis. Eur. Arch. Otorhinolaryngol. 1999, 256, 335–337. [Google Scholar] [CrossRef]
- Ohashi, Y.; Nakai, Y. Reduced Ciliary Action in Chronic Sinusitis. Acta Oto-Laryngol. 2009, 95, 3–9. [Google Scholar] [CrossRef]
- Hafner, B.; Davris, S.; Riechelmann, H.; Mann, W.J.; Amedee, R.G. Endonasal Sinus Surgery Improves Mucociliary Transport in Severe Chronic Sinusitis. Am. J. Rhinol. 1997, 11, 271–274. [Google Scholar] [CrossRef]
- Papsin, B.; McTavish, A. Saline Nasal Irrigation: Its Role as an Adjunct Treatment. Can. Fam. Physician 2003, 49, 168. [Google Scholar]
- Süslü, N.; Bajin, M.D.; Süslü, A.E.; Öǧretmenoǧlu, O. Effects of Buffered 2.3%, Buffered 0.9%, and Non-Buffered 0.9% Irrigation Solutions on Nasal Mucosa after Septoplasty. Eur Arch Otorhinolaryngol 2009, 266, 685–689. [Google Scholar] [CrossRef]
- Wabnitz, D.A.M.; Wormald, P.J. A Blinded, Randomized, Controlled Study on the Effect of Buffered 0.9% and 3% Sodium Chloride Intranasal Sprays on Ciliary Beat Frequency. Laryngoscope 2005, 115, 803–805. [Google Scholar] [CrossRef]
- Homer, J.J.; England, R.J.; Wilde, A.D.; Harwood, G.R.J.; Stafford, N.D. The Effect of PH of Douching Solutions on Mucociliary Clearance. Clin. Otolaryngol. 1999, 24, 312–315. [Google Scholar] [CrossRef]
- Talbot, A.R.; Herr, T.M.; Parsons, D.S. Mucociliary Clearance and Buffered Hypertonic Saline Solution. Laryngoscope 1997, 107, 500–503. [Google Scholar] [CrossRef]
- Wen, Z.; Wu, C.; Cui, F.; Zhang, H.; Mei, B.; Shen, M. The Role of Osmolality in Saline Fluid Nebulization after Tracheostomy: Time for Changing? BMC Pulm. Med. 2016, 16, 1–10. [Google Scholar] [CrossRef]
- Lee, S.H.; Song, J.S.; Lee, S.H.; Hwang, S.J.; Lee, H.M. Effect of Hypertonic Seawater (Sinomarin(R)) on Mucociliary Clearance in Normal Subjects. J. Rhinol. 2003, 10, 19–22. [Google Scholar]
- Keojampa, B.K.; Hoang Nguyen, M.; Ryan, M.W. Effects of Buffered Saline Solution on Nasal Mucociliary Clearance and Nasal Airway Patency. Otolaryngol. Head Neck Surg. 2004, 131, 679–682. [Google Scholar] [CrossRef]
- Daviskas, E.; Anderson, S.D.; Gonda, I.; Eberl, S.; Meikle, S.; Seale, J.P.; Bautovich, G. Inhalation of Hypertonic Saline Aerosol Enhances Mucociliary Clearance in Asthmatic and Healthy Subjects. Eur. Respir. J. 1996, 9, 725–732. [Google Scholar] [CrossRef] [PubMed]
- Eng, P.; Morton, J.; Douglass, J.; Riedler, J.; Wilson, J.; Robertson, C. Short-term Efficacy of Ultrasonically Nebulized Hypertonic Saline in Cystic Fibrosis. Pediatr. Pulmonol. 1996, 21, 77–83. [Google Scholar] [CrossRef]
- Stahl, M.; Wielpütz, M.O.; Ricklefs, I.; Dopfer, C.; Barth, S.; Schlegtendal, A.; Graeber, S.Y.; Sommerburg, O.; Diekmann, G.; Hüsing, J.; et al. Preventive Inhalation of Hypertonic Saline in Infants with Cystic Fibrosis (PRESIS). A Randomized, Double-Blind, Controlled Study. Am. J. Respir. Crit. Care Med. 2019, 199, 1238–1248. [Google Scholar] [CrossRef] [PubMed]
- Robinson, M.; Hemming, A.L.; Regnis, J.A.; Wong, A.G.; Bailey, D.L.; Bautovich, G.J.; King, M.; Bye, P.T.P. Effect of Increasing Doses of Hypertonic Saline on Mucociliary Clearance in Patients with Cystic Fibrosis. Thorax 1997, 52, 900–903. [Google Scholar] [CrossRef] [PubMed]
- Baron, J.; El-Chaar, G. Hypertonic Saline for the Treatment of Bronchiolitis in Infants and Young Children: A Critical Review of the Literature. J. Pediatr. Pharmacol. Ther. 2016, 21, 7–26. [Google Scholar] [CrossRef]
- Li, H.-B.; Shi, J.-B.; Cao, F.; Cheng, L.; Wen, W.-P.; Xu, G. Hypertonic Saline Solution Stimulated CLC-3 Production in Primary Cultured Human Nasal Epithelial Cells. Auris Nasus Larynx 2008, 35, 47–51. [Google Scholar] [CrossRef] [PubMed]
- Holmström, M.; Rosén, G.; Wåhlander, L. Effect of Nasal Lavage on Nasal Symptoms and Physiology in Wood Industry Workers. Rhinology 1997, 35, 108–112. [Google Scholar]
- Shoseyov, D.; Bibi, H.; Shai, P.; Shoseyov, N.; Shazberg, G.; Hurvitz, H. Treatment with Hypertonic Saline versus Normal Saline Nasal Wash of Pediatric Chronic Sinusitis. J. Allergy Clin. Immunol. 1998, 101, 602–605. [Google Scholar] [CrossRef]
- Rabone, S.J.; Saraswati, S.B. Acceptance and Effects of Nasal Lavage in Volunteer Woodworkers. Occup. Med. 1999, 49, 365–369. [Google Scholar] [CrossRef][Green Version]
- Taccariello, M.; Parikh, A.; Darby, Y.; Scadding, G. Nasal Douching as a Valuable Adjunct in the Management of Chronic Rhinosinusitis. Rhinology 1999, 37, 29–32. [Google Scholar]
- Bachmann, G.; Hommel, G.; Michel, O. Effect of Irrigation of the Nose with Isotonic Salt Solution on Adult Patients with Chronic Paranasal Sinus Disease. Eur. Arch. Otorhinolaryngol. 2000, 257, 537–541. [Google Scholar] [CrossRef] [PubMed]
- Heatley, D.G.; McConnell, K.E.; Kille, T.L.; Leverson, G.E. Nasal Irrigation for the Alleviation of Sinonasal Symptoms. Otolaryngol. Head Neck Surg. 2001, 125, 44–48. [Google Scholar] [CrossRef] [PubMed]
- Rabago, D.; Zgierska, A.; Mundt, M.; Barrett, B.; Bobula, J.; Maberry, R. Efficacy of Daily Hypertonic Saline Nasal Irrigation among Patients with Sinusitis: A Randomized Controlled Trial. J. Fam. Pract. 2002, 51, 1049–1055. [Google Scholar]
- Garavello, W.; Romagnoli, M.; Sordo, L.; Gaini, R.M.; di Berardino, C.; Angrisano, A. Hypersaline Nasal Irrigation in Children with Symptomatic Seasonal Allergic Rhinitis: A Randomized Study. Pediatr. Allergy Immunol. 2003, 14, 140–143. [Google Scholar] [CrossRef] [PubMed]
- Chkhartishvili, E.; Zhorzholiani, L.; Karseladze, R. Nasal Disease Management by Using Aqua Maris Solution. Ann. Biomed. Res. Educ. 2004, 4, 186–187. [Google Scholar]
- Tano, L.; Tano, K. A Daily Nasal Spray with Saline Prevents Symptoms of Rhinitis. Acta Otolaryngol. 2004, 124, 1059–1062. [Google Scholar] [CrossRef] [PubMed]
- Wormald, P.J.; Cain, T.; Oates, L.; Hawke, L.; Wong, I. A Comparative Study of Three Methods of Nasal Irrigation. Laryngoscope 2004, 114, 2224–2227. [Google Scholar] [CrossRef]
- Cordray, S.; Harjo, J.B.; Miner, L. Comparison of Intranasal Hypertonic Dead Sea Saline Spray and Intranasal Aqueous Triamcinolone Spray in Seasonal Allergic Rhinitis. Ear Nose Throat J. 2005, 84, 426–430. [Google Scholar] [CrossRef]
- Garavello, W.; di Berardino, F.; Romagnoli, M.; Sambataro, G.; Gaini, R.M. Nasal Rinsing with Hypertonic Solution: An Adjunctive Treatment for Pediatric Seasonal Allergic Rhinoconjunctivitis. Int. Arch. Allergy Immunol. 2005, 137, 310–314. [Google Scholar] [CrossRef]
- Kim, C.H.; Hyun Song, M.; Eun Ahn, Y.; Lee, J.G.; Yoon, J.H. Effect of Hypo-, Iso- and Hypertonic Saline Irrigation on Secretory Mucins and Morphology of Cultured Human Nasal Epithelial Cells. Acta Otolaryngol. 2005, 125, 1296–1300. [Google Scholar] [CrossRef]
- Passàli, D.; Damiani, V.; Passàli, F.M.; Passàli, G.C.; Bellussi, L. Atomized Nasal Douche vs Nasal Lavage in Acute Viral Rhinitis. Arch. Otolaryngol. Head Neck Surg. 2005, 131, 788–790. [Google Scholar] [CrossRef] [PubMed]
- Friedman, M.; Vidyasagar, R.; Joseph, N. A Randomized, Prospective, Double-Blind Study on the Efficacy of Dead Sea Salt Nasal Irrigations. Laryngoscope 2006, 116, 878–882. [Google Scholar] [CrossRef] [PubMed]
- Rabago, D.; Barrett, B.; Marchand, L.; Maberry, R.; Mundt, M. Qualitative Aspects of Nasal Irrigation Use by Patients with Chronic Sinus Disease in a Multimethod Study. Ann. Fam. Med. 2006, 4, 295–301. [Google Scholar] [CrossRef] [PubMed]
- Hauptman, G.; Ryan, M.W. The Effect of Saline Solutions on Nasal Patency and Mucociliary Clearance in Rhinosinusitis Patients. Otolaryngol. Head Neck Surg. 2007, 137, 815–821. [Google Scholar] [CrossRef]
- Kuzik, B.A.; al Qadhi, S.A.; Kent, S.; Flavin, M.P.; Hopman, W.; Hotte, S.; Gander, S. Nebulized Hypertonic Saline in the Treatment of Viral Bronchiolitis in Infants. J. Pediatr. 2007, 151, 266–270.e1. [Google Scholar] [CrossRef]
- Pynnonen, M.A.; Mukerji, S.S.; Kim, H.M.; Adams, M.E.; Terrell, J.E. Nasal Saline for Chronic Sinonasal Symptoms: A Randomized Controlled Trial. Arch. Otolaryngol. Head Neck Surg. 2007, 133, 1115–1120. [Google Scholar] [CrossRef]
- Karpova, E.P.; Feĭzullaev, E.F. Experience in Using Laryngeal Aqua Maris Spray for the Local Treatment of Chronic Tonsillitis in Children. Vestn. Otorinolaringol. 2008, 4, 85–86. [Google Scholar]
- Šlapak, I.; Skoupá, J.; Strnad, P.; Horník, P. Efficacy of Isotonic Nasal Wash (Seawater) in the Treatment and Prevention of Rhinitis in Children. Arch. Otolaryngol. Head Neck Surg. 2008, 134, 67–74. [Google Scholar] [CrossRef]
- Ural, A.; Oktemer, T.K.; Kizil, Y.; Ileri, F.; Uslu, S. Impact of Isotonic and Hypertonic Saline Solutions on Mucociliary Activity in Various Nasal Pathologies: Clinical Study. J. Laryngol. Otol. 2009, 123, 517–521. [Google Scholar] [CrossRef]
- Gelardi, M.; Fiorella, M.L.; Di Gioacchino, M.; Ciprandi, G. Immune Effects of Nickel. Int. J. Immunopathol. Pharmacol. 2009, 17, 63–69. [Google Scholar]
- Li, H.; Sha, Q.; Zuo, K.; Jiang, H.; Cheng, L.; Shi, J.; Xu, G. Nasal Saline Irrigation Facilitates Control of Allergic Rhinitis by Topical Steroid in Children. ORL J. Otorhinolaryngol. Relat. Spec. 2009, 71, 50–55. [Google Scholar] [CrossRef]
- Rabago, D.; Zgierska, A.; Peppard, P.; Bamber, A. The Prescribing Patterns of Wisconsin Family Physicians Surrounding Saline Nasal Irrigation for Upper Respiratory Conditions. WMJ 2009, 108, 145. [Google Scholar] [PubMed]
- Culig, J.; Leppée, M.; Vceva, A.; Djanic, D. Efficiency of Hypertonic and Isotonic Seawater Solutions in Chronic Rhinosinusitis. Med. Glas. 2010, 7, 116–123. [Google Scholar]
- Miraglia Del Giudice, M.; Decimo, F.; Maiello, N.; Leonardi, S.; Parisi, G.; Golluccio, M.; Capasso, M.; Balestrieri, U.; Rocco, A.; Perrone, L.; et al. Effectiveness of Ischia Thermal Water Nasal Aerosol in Children with Seasonal Allergic Rhinitis: A Randomized and Controlled Study. Int. J. Immunopathol. Pharmacol. 2011, 24, 1103–1109. [Google Scholar] [CrossRef] [PubMed]
- Miraglia Del Giudice, M.; Saitta, F.; Leonardi, S.; Capasso, M.; Niglio, B.; Chinellato, I.; Decimo, F.; Maiello, N.; Capristo, C.; Perrone, L.; et al. Effectiveness of Nebulized Hypertonic Saline and Epinephrine in Hospitalized Infants with Bronchiolitis. Int. J. Immunopathol. Pharmacol. 2012, 25, 485–491. [Google Scholar] [CrossRef]
- Hermelingmeier, K.E.; Weber, R.K.; Hellmich, M.; Heubach, C.P.; Mösges, R. Nasal Irrigation as an Adjunctive Treatment in Allergic Rhinitis: A Systematic Review and Meta-Analysis. Am. J. Rhinol. Allergy 2012, 26. [Google Scholar] [CrossRef]
- Satdhabudha, A.; Poachanukoon, O. Efficacy of Buffered Hypertonic Saline Nasal Irrigation in Children with Symptomatic Allergic Rhinitis: A Randomized Double-Blind Study. Int. J. Pediatr. Otorhinolaryngol. 2012, 76, 583–588. [Google Scholar] [CrossRef]
- Tantilipikorn, P.; Tunsuriyawong, P.; Jareoncharsri, P.; Bedavanija, A.; Assanasen, P.; Bunnag, C.; Metheetrairut, C. A Randomized, Prospective, Double-Blind Study of the Efficacy of Dexpanthenol Nasal Spray on the Postoperative Treatment of Patients with Chronic Rhinosinusitis after Endoscopic Sinus Surgery. J. Med. Assoc. Thai 2012, 95, 58–63. [Google Scholar]
- Kumar, R.A.; Viswanatha, B.; Krishna, N.; Jayanna, N.; Shetty, D.R. Efficacy of Hypertonic Saline and Normal Saline in the Treatment of Chronic Sinusitis. Int. J. Otolaryn. Head Neck Surg. 2013, 2, 90–96. [Google Scholar] [CrossRef][Green Version]
- Chen, J.R.; Jin, L.; Li, X.Y. The Effectiveness of Nasal Saline Irrigation (Seawater) in Treatment of Allergic Rhinitis in Children. Int. J. Pediatr. Otorhinolaryngol. 2014, 78, 1115–1118. [Google Scholar] [CrossRef]
- Low, T.H.; Woods, C.M.; Ullah, S.; Carney, A.S. A Double-Blind Randomized Controlled Trial of Normal Saline, Lactated Ringer’s, and Hypertonic Saline Nasal Irrigation Solution after Endoscopic Sinus Surgery. Am. J. Rhinol. Allergy 2014, 28, 225–231. [Google Scholar] [CrossRef] [PubMed]
- Marchisio, P.; Picca, M.; Torretta, S.; Baggi, E.; Pasinato, A.; Bianchini, S.; Nazzari, E.; Esposito, S.; Principi, N. Nasal Saline Irrigation in Preschool Children: A Survey of Attitudes and Prescribing Habits of Primary Care Pediatricians Working in Northern Italy. Ital. J. Pediatr. 2014, 40, 47. [Google Scholar] [CrossRef]
- Nguyen, S.A.; Psaltis, A.J.; Schlosser, R.J. Isotonic Saline Nasal Irrigation Is an Effective Adjunctive Therapy to Intranasal Corticosteroid Spray in Allergic Rhinitis. Am. J. Rhinol. Allergy 2014, 28, 308–311. [Google Scholar] [CrossRef]
- Pham, V.; Sykes, K.; Wei, J. Long-Term Outcome of Once Daily Nasal Irrigation for the Treatment of Pediatric Chronic Rhinosinusitis. Laryngoscope 2014, 124, 1000–1007. [Google Scholar] [CrossRef] [PubMed]
- Stoelzel, K.; Bothe, G.; Chong, P.W.; Lenarz, M. Safety and Efficacy of Nasya/Prevalin in Reducing Symptoms of Allergic Rhinitis. Clin. Respir. J. 2014, 8, 382–390. [Google Scholar] [CrossRef] [PubMed]
- Wang, Y.H.; Ku, M.S.; Sun, H.L.; Lue, K.H. Efficacy of Nasal Irrigation in the Treatment of Acute Sinusitis in Atopic Children. J. Microbiol. Immunol. Infect. 2014, 47, 63–69. [Google Scholar] [CrossRef]
- Alvarez-Puebla, M.J.; Olaguibel, J.M.; Almudevar, E.; Echegoyen, A.A.; Vela, C.; de Esteban, B. Mannitol versus Hypertonic Saline: Safety and Efficacy of Mannitol and Hypertonic Saline in Sputum Induction and Bronchial Hyperreactivity Assessment. Chron. Respir. Dis. 2015, 12, 197–203. [Google Scholar] [CrossRef]
- Köksal, T.; Çizmeci, M.N.; Bozkaya, D.; Kanburoğlu, M.K.; Şahin, Ş.; Taş, T.; Yüksel, Ç.N.; Tatli, M.M. Comparison between the Use of Saline and Seawater for Nasal Obstruction in Children under 2 Years of Age with Acute Upper Respiratory Infection. Turk. J. Med. Sci. 2016, 46, 1004–1013. [Google Scholar] [CrossRef]
- Grasso, M.; de Vincentiis, M.; Agolli, G.; Cilurzo, F.; Grasso, R. The Effectiveness of Long-Term Course of Sterimar Mn Nasal Spray for Treatment of the Recurrence Rates of Acute Allergic Rhinitis in Patients with Chronic Allergic Rhinitis. Drug Des. Devel. Ther. 2018, 12, 705–709. [Google Scholar] [CrossRef]
- Bergmann, C.; Müller, K.; Thieme, U.; Zeman, F.; Huppertz, G.; Koller, M.; Meiser, P. Real-World Data on the Use of Hypertonic Saline Nasal Spray in ENT Practice. SN Compr. Clin. Med. 2019, 1, 354–361. [Google Scholar] [CrossRef]
- Bogomilskiy, M.R.; Radcig, E.; Radcig, A.N. Complex Treatment of Acute Infectious Rhinitis in Children. Pediatrija. Žurnal IM. G.N. Speranskogo 2019, 98, 120–123. [Google Scholar] [CrossRef]
- Stobbelaar, K.; Kool, M.; de Kruijf, D.; van Hoorenbeeck, K.; Jorens, P.; de Dooy, J.; Verhulst, S. Nebulised Hypertonic Saline in Children with Bronchiolitis Admitted to the Paediatric Intensive Care Unit: A Retrospective Study. J. Paediatr. Child Health 2019, 55, 1125–1132. [Google Scholar] [CrossRef] [PubMed]
- Craig, S.S.; Seith, R.W.; Cheek, J.A.; Wilson, K.; Egerton-Warburton, D.; Paul, E.; West, A. Lidocaine and Phenylephrine versus Saline Placebo Nasal Spray for the Pain and Distress of Nasogastric Tube Insertion in Young Children and Infants: A Randomised, Double-Blind, Controlled Trial. Lancet Child Adolesc. Health 2019, 3, 391–397. [Google Scholar] [CrossRef]
- Perić, A.; Kovačević, S.V.; Barać, A.; Gaćeša, D.; Perić, A.V.; Jožin, S.M. Efficacy of Hypertonic (2.3%) Sea Water in Patients with Aspirin-Induced Chronic Rhinosinusitis Following Endoscopic Sinus Surgery. Acta Otolaryngol. 2019, 139, 529–535. [Google Scholar] [CrossRef]
- Ramalingam, S.; Graham, C.; Dove, J.; Morrice, L.; Sheikh, A. Hypertonic Saline Nasal Irrigation and Gargling Should Be Considered as a Treatment Option for COVID-19. J. Glob. Health 2020, 10, 010332. [Google Scholar] [CrossRef]
- Huang, S.; Constant, S.; de Servi, B.; Meloni, M.; Saaid, A.; Culig, J.; Bertini, M. Is a Diluted Seawater-Based Solution Safe and Effective on Human Nasal Epithelium? Eur. Arch. Otorhinolaryngol. 2021, 278, 2837–2842. [Google Scholar] [CrossRef]
- Jiang, M.; Chen, J.; Ding, Y.; Gan, C.; Hou, Y.; Lei, J.; Wan, M.; Li, X.; Xiao, Z. Efficacy and Safety of Sea Salt-Derived Physiological Saline Nasal Spray as Add-On Therapy in Patients with Acute Upper Respiratory Infection: A Multicenter Retrospective Cohort Study. Med. Sci. Monit. 2021, 27, e929714. [Google Scholar] [CrossRef]
- Chusakul, S.; Warathanasin, S.; Suksangpanya, N.; Phannaso, C.; Ruxrungtham, S.; Snidvongs, K.; Aeumjaturapat, S. Comparison of Buffered and Nonbuffered Nasal Saline Irrigations in Treating Allergic Rhinitis. Laryngoscope 2013, 123, 53–56. [Google Scholar] [CrossRef]
- Brown, C.L.; Graham, S.M. Nasal Irrigations: Good or Bad? Curr. Opin. Otolaryngol. Head Neck Surg. 2004, 12, 9–13. [Google Scholar] [CrossRef] [PubMed]
- Harvey, R.; Hannan, S.A.; Badia, L.; Scadding, G. Nasal Saline Irrigations for the Symptoms of Chronic Rhinosinusitis. Cochrane Database Syst. Rev. 2007. [Google Scholar] [CrossRef]
- Kassel, J.C.; King, D.; Spurling, G.K. Saline Nasal Irrigation for Acute Upper Respiratory Tract Infections. Cochrane Database Syst. Rev. 2010. [Google Scholar] [CrossRef]
- Zhang, L.; Mendoza-Sassi, R.A.; Wainwright, C.; Klassen, T.P. Nebulized Hypertonic Saline Solution for Acute Bronchiolitis in Infants. Cochrane Database Syst. Rev. 2008. [Google Scholar] [CrossRef]
- Adappa, N.D.; Wei, C.C.; Palmer, J.N. Nasal Irrigation with or without Drugs: The Evidence. Curr. Opin. Otolaryngol. Head Neck Surg. 2012, 20, 53–57. [Google Scholar] [CrossRef] [PubMed]
- Chirico, G.; Quartarone, G.; Mallefet, P. Nasal Congestion in Infants and Children: A Literature Review on Efficacy and Safety of Non-Pharmacological Treatments. Minerva Pediatrica 2014, 66, 549–557. [Google Scholar] [PubMed]
- Chong, L.Y.; Head, K.; Hopkins, C.; Philpott, C.; Glew, S.; Scadding, G.; Burton, M.J.; Schilder, A.G.M. Saline Irrigation for Chronic Rhinosinusitis. Cochrane Database Syst. Rev. 2016, 4. [Google Scholar] [CrossRef] [PubMed]
- Madison, S.; Brown, E.A.; Franklin, R.; Wickersham, E.A.; McCarthy, L.H. Nasal Saline or Intranasal Corticosteroids to Treat Allergic rhinitis in Children. J. Okla. State Med. Assoc. 2016, 109, 152. [Google Scholar] [PubMed]
- Kanjanawasee, D.; Seresirikachorn, K.; Chitsuthipakorn, W.; Snidvongs, K. Hypertonic Saline Versus Isotonic Saline Nasal Irrigation: Systematic Review and Meta-Analysis. Am. J. Rhinol. Allergy 2018, 32, 269–279. [Google Scholar] [CrossRef]
- Li, C.L.; Lin, H.C.; Lin, C.Y.; Hsu, T.F. Effectiveness of Hypertonic Saline Nasal Irrigation for Alleviating Allergic Rhinitis in Children: A Systematic Review and Meta-Analysis. J. Clin. Med. 2019, 8, 64. [Google Scholar] [CrossRef]
- King, D. What Role for Saline Nasal Irrigation? Drug Ther. Bull. 2019, 57, 56–59. [Google Scholar] [CrossRef]
- Halawi, A.M.; Smith, S.S.; Chandra, R.K. Chronic Rhinosinusitis: Epidemiology and Cost. Allergy Asthma Proc. 2013, 34, 328–334. [Google Scholar] [CrossRef]
- Sedaghat, A.R. Chronic Rhinosinusitis. Am. Fam. Physician 2017, 96, 500–506. [Google Scholar] [PubMed]
- Radtsig, E.; Ermilova, N.V.; Bogomilskiy, M.R. Nose Obstruction in Children: Causes and Methods of Treatment. Pediatrija. Žurnal IM. G.N. Speranskogo 2012, 91, 85–90. [Google Scholar]
- Greiner, A.N.; Hellings, P.W.; Rotiroti, G.; Scadding, G.K. Allergic Rhinitis. Lancet 2011, 378, 2112–2122. [Google Scholar] [CrossRef]
- Garavello, W.; Somigliana, E.; Acaia, B.; Gaini, L.; Pignataro, L.; Gaini, R.M. Nasal Lavage in Pregnant Women with Seasonal Allergic Rhinitis: A Randomized Study. Int. Arch. Allergy Immunol. 2010, 151, 137–141. [Google Scholar] [CrossRef]
- Rapiejko, P.; Jurkiewicz, D. The Use of Hypertonic Sea-Water Solution in Patients after Surgery of the Nose and Paranasal Sinuses. Otolaryngol. Pol. 2010, 64, 20–30. [Google Scholar] [CrossRef]
- Baxter, A.L.; Schwartz, K.R.; Johnson, R.W.; Kuchinski, A.-M.; Swartout, K.M.; Rao, A.S.R.S.; Gibson, R.W.; Cherian, E.; Giller, T.; Boomer, H.; et al. Rapid Initiation of Nasal Saline Irrigation to Reduce Severity in High-Risk COVID+ Outpatients: A Randomized Clinical Trial Compared to a National Dataset Observational Arm. medRxiv 2021. [Google Scholar] [CrossRef]
- Casale, M.; Rinaldi, V.; Sabatino, L.; Moffa, A.; Ciccozzi, M. Could Nasal Irrigation and Oral Rinse Reduce the Risk for COVID-19 Infection? Int. J. Immunopathol. Pharmacol. 2020, 34. [Google Scholar] [CrossRef]
- Panta, P.; Chatti, K.; Andhavarapu, A. Do Saline Water Gargling and Nasal Irrigation Confer Protection against COVID-19? Explore 2021, 17, 127–129. [Google Scholar] [CrossRef]
- Farrell, N.F.; Klatt-Cromwell, C.; Schneider, J.S. Benefits and Safety of Nasal Saline Irrigations in a Pandemic-Washing COVID-19 Away. JAMA Otolaryngol. Head Neck Surg. 2020, 146, 787–788. [Google Scholar] [CrossRef]
- Huijghebaert, S.; Hoste, L.; Vanham, G. Essentials in Saline Pharmacology for Nasal or Respiratory Hygiene in Times of COVID-19. Eur. J. Clin. Pharmacol. 2021, 77, 1275–1293. [Google Scholar] [CrossRef]
- Chatterjee, U.; Chakraborty, A.; Naskar, S.; Bandyapadhyay, B.; Shee, S. Efficacy of Normal Saline Nasal Spray and Gargle on SARS-CoV-2 for Prevention of COVID-19 Pneumonia; Research Square: Durham, NC, USA, 2021. [Google Scholar] [CrossRef]
- Singh, S.; Sharma, N.; Singh, U.; Singh, T.; Mangal, D.; Singh, V. Nasopharyngeal Wash in Preventing and Treating Upper Respiratory Tract Infections: Could It Prevent COVID-19? Lung India 2020, 37, 246–251. [Google Scholar] [CrossRef] [PubMed]
- Hildenbrand, T.; Weber, R.K.; Brehmer, D. Rhinitis Sicca, Dry Nose and Atrophic Rhinitis: A Review of the Literature. Eur. Arch Otorhinolaryngol. 2011, 268, 17–26. [Google Scholar] [CrossRef] [PubMed]

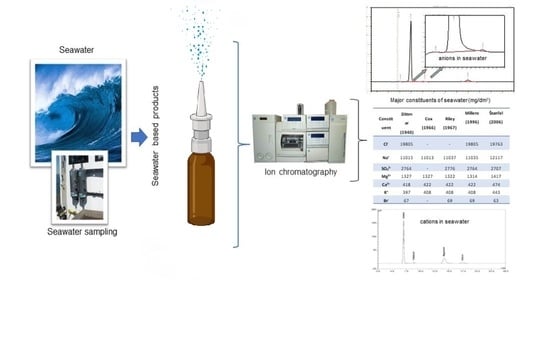
| Constituent | Dittmar (1940) * [9] | Cox (1966) * [10] | Riley (1967) * [11] | Millero (1996) * [12] | Štanfel (2006) * [13] |
|---|---|---|---|---|---|
| Cl− | 19,805 | - | - | 19,805 | 19,763 |
| Na+ | 11,015 | 11,013 | 11,037 | 11,035 | 12,117 |
| SO42− | 2764 | - | 2776 | 2764 | 2707 |
| Mg2+ | 1327 | 1327 | 1322 | 1314 | 1417 |
| Ca2+ | 418 | 422 | 422 | 422 | 474 |
| K+ | 397 | 408 | 408 | 408 | 443 |
| Br− | 67 | - | 69 | 69 | 63 |
| Constituent | Action |
|---|---|
| Mg2+ | Promotes cell repair and limits inflammation by reducing the eicosanoid metabolism both at the level of the liberation of arachidonic acid and by direct inhibition of the 5-lipoxygenase enzyme. Inhibits exocytosis from permeabilized eosinophils. Reduces apoptosis of respiratory cells. |
| Ca2+ | Acetylcholine and serotonin act as messengers, increasing calcium intake in ciliated cells and thus regulating ciliary beat frequency and synchronization. Airflow promotes cell calcium intake and ciliary beat via shear-stress-induced mechanotransduction. |
| K+ | Anti-inflammatory action. Promotes respiratory epithelium repair via the EGF/EGFR pathway. |
| HCO3− | Reduces mucous viscosity by acting as a buffer. Facilitates elimination by ciliary cells movement. |
| Study | Design | Subjects | Intervention | Safety Conclusions | Other Remarks |
|---|---|---|---|---|---|
| Holmstrom, 1997 [41] | Cross-sectional | 45 healthy adults exposed to wood dust | Nasal lavage with Rhinomer force 2, four times a day, every workday. | One increase in allergic symptoms (with concomitant local steroid). One anterior epistaxis and one throat irritation. | At week 3, 88% subjects wanted to continue treatment, and 3 weeks after stopping treatment, 83% wished to start the treatment again. |
| Shoseyov, 1998 [42] | RCT | 34 children with chronic sinusitis | Hypertonic (3.5%) vs. isotonic saline, 10 drops, three times daily for 4 weeks. | Three subjects in hypertonic group and one in isotonic group left study because of the burning feeling in the nose and throat. | Burning and itching was more common in hypertonic group, but only during the first 3 to 4 days. After that period, there was no difference between the groups. |
| Rabone, 1999 [43] | Crossover trial with 1-year follow-up | 46 woodworkers exposed to wood dust | Gravity fed, home-made unbuffered isotonic saline for 2 months. | Generally safe, no notable adverse events. | The group reported significantly decreased nasal symptoms and over half of subjects continued to use nasal lavage voluntarily after 1 year. |
| Taccariello, 1999 [44] | RCT | 40 patients with chronic rhinosinusitis | Traditional alkaline nasal douche vs. a sterile seawater spray, in addition to their regular treatment. | No adverse effects mentioned. | Alkaline nasal douche had a significant effect upon endoscopic appearances, whereas the spray did not; conversely, spray improved quality of life, whereas alkaline douche did not. |
| Bachmann, 2000 [45] | RCT | 40 adults with paranasal sinus disease | Isotonic Ems salt solution or isotonic sodium chloride solution nasal irrigation twice daily for 7 days. | No adverse events mentioned in either group. | A slight difference between treatment with Ems salt solution and sodium chloride solution; questionable clinical relevance. |
| Heatley, 2001 [46] | Prospective RCT | 150 adults with chronic rhinosinusitis | Nasal saline irrigation with bulb syringe or irrigation pot vs. placebo, daily for 2 weeks. | No significant adverse events; comparable efficacy in all three groups. | More than one-third of subjects reported using less concomitant medication. |
| Rabago, 2002 [47] | RCT | 76 adults with acute or chronic rhinosinusitis | Nasal saline irrigation with 150 mL daily per nostril for 6 months vs. no treatment. | Ten side effects, of which 8 were considered as “not significant” and 2 as significant, but affected subjects were still “highly satisfied” with the treatment. | Subjects treated with nasal saline used statistically significantly less antibiotic treatment compared to control group. |
| Garavello, 2003 [48] | Prospective RCT | 20 children with allergic rhinitis | Hypertonic saline in 10 subjects, no treatment in 10 subjects; 2.5 mL in each nostril three times daily for 6 weeks. | No patients lost to follow up and no adverse events reported. | Statistically significant decrease in use of oral antihistamines in hypertonic saline group. |
| Lee, 2003 [33] | RCT, crossover | 28 healthy adult subjects | Hypertonic (Sinomarin, 3%) or isotonic saline. 10 sprays of both preparations (on different days) in the same nostril. | Complaints of mild prickling sensation after nasal douching with hypertonic seawater. | The effect of the hypertonic solution is probably due to changes in mucus viscoelastic properties. |
| Chkhartishvili, 2004 [49] | Case-control open clinical trial | 30 children with allergic rhinitis, acute and chronic bacterial rhinosinusitis and 30 children in control group | “Aqua Maris” seawater solution, either irrigation or 2 drops in nasal cavity 3 times a day from 2 to 4 weeks. | Nasal drops in children up to 2 years of age were well-tolerated, with no complication. No adverse effects mentioned for the irrigation group. | In subjects with bacterial rhinosinusitis, time to relief of symptoms in Aqua Maris group was 7 ± 3.2 days vs. 10 ± 2.4 days in control group. In allergic rhinitis group, Aqua Maris reduced the use of systemic drugs in 7 of 15 patients. |
| Tano, 2004 [50] | Prospective trial | 108 healthy army conscripts | 10-week nasal spraying with physiological saline twice daily, followed by a 10-week period of follow up. | Two cases of nose dryness. | There was a mean of 0.7 episodes of upper respiratory tract infection during the spray period, compared with 1.0 episodes during the observation. |
| Wormald, 2004 [51] | Prospective, cross-over study | 12 adult subjects | Nasal irrigation with normal saline containing Technetium 99m sulfur colloid | No adverse effects mentioned. | The nasal cavity was well irrigated using three techniques (spray, nebulization, douching). Douching was significantly more effective in penetrating the maxillary sinus and frontal recess. The sphenoid and frontal sinuses were poorly irrigated by all three techniques. |
| Cordray, 2005 [52] | Prospective, randomized, single-blind, placebo-controlled | 15 patients with seasonal allergic rhinitis | Intranasal hypertonic dead sea saline spray, intranasal aqueous triamcinolone spray, placebo nasal saline spray for 7 days. | Two subjects withdrew for adverse events (unknown group). | Significant improvements were seen in both active-treatment groups; the corticosteroid spray was the more effective. Dead Sea saline solution can be an effective alternative in mild-to-moderate allergic rhinitis, particularly with respect to nasal and eye symptoms. It improves mucociliary clearance, while Mg cation probably exerts anti-inflammatory effects on the nasal mucosa and on the systemic immune response. |
| Garavello, 2005 [53] | Prospective RCT | 44 children with allergic rhinitis | Hypertonic saline vs. no treatment; 3 sprays (50 μL) in each nostril three times daily for 7 weeks. | No adverse events in the treatment group. | Statistically significant decrease in use of oral antihistamines in hypertonic saline group. |
| Kim, 2005 [54] | In vitro study | Cell cultures of fully differentiated passage-2 normal human nasal epithelial cells | Cells in the cultures were treated with pure water and with 0.3% (hypotonic), 0.9% (isotonic) and 3% (hypertonic) saline solutions. | In vitro study. | mRNA for major airway mucins analysis and morphologic analysis suggest that pure water damaged epithelial cells, and that only isotonic saline did not affect their morphology. |
| Passali, 2005 [55] | RCT | 200 patients with acute viral rhinosinusitis | Atomized nasal douche vs. nasal lavages with isotonic sodium chloride solution. | No adverse effects mentioned. | Atomized nasal douches significantly improved inspiratory and expiratory rhinomanometric resistance and nasal volumes and normalized mucociliary transport time to a physiological level. |
| Wabnitz, 2005 [29] | In-vitro study | 8 healthy adult subjects | One application of four sprays of hypertonic (3.0%) saline (one nostril) and isotonic saline (another nostril) in all subjects. | No adverse effects mentioned. | Cell samples from subjects receiving saline solutions. The administration of hypertonic saline results in a significantly faster CBF 5 min (but not 60 min) after administration. |
| Friedman, 2006 [56] | Randomized, prospective, double-blind study | 42 adults seeking treatment for chronic rhinosinusitis | Nasal irrigation using hypertonic dead sea salt solution with hypertonic saline. | No adverse effects mentioned. | Both groups had significant improvement after treatment. However, the dead sea salt patients had significantly better symptom relief and showed improved RQLQ(S) scores. |
| Rabago, 2006 [57] | Semi-structured, in-depth interviews in a 3-part, multimethod study | 28 subjects with frequent rhinosinusitis and chronic sinonasal symptoms. | Hypertonic saline nasal irrigation. | Side effects including saline drainage, nasal burning and irritation were noted, but not identified as important enough to stop the treatment. | This is a well-tolerated, inexpensive, effective long-term therapy that patients can use at home with minimal training and follow-up. |
| Hauptman, 2007 [58] | RCT | 80 adult patients with rhinosinusitis | 1 mL of physiological or hypertonic saline to one nostril. | Increased nasal burning/irritation with hypertonic saline compared to physiological saline. | Buffered physiological saline significantly affected nasal airway patency, whereas buffered hypertonic saline had no effect on nasal patency. |
| Kuzik, 2007 [59] | Prospective, randomized, double-blinded, controlled, multicenter trial | 96 infants with viral bronchiolitis | Repeated doses of nebulized 3% hypertonic saline or 0.9% normal saline, in addition to routine therapy. | All participants tolerated therapy without apparent adverse effects, and were eventually discharged after achieving full recovery. | Clinically relevant reduction in length of stay to 2.6 ± 1.9 days in hypertonic saline group, compared with 3.5 ± 2.9 days in the normal saline group. |
| Pynnonen, 2007 [60] | Prospective RCT | 127 adults with chronic nasal and sinus symptoms | Irrigation with large volume and low positive pressure or spray for 8 weeks. | Forty-one subjects reported a total of 67 adverse effects. Posttreatment nasal drainage was the most common adverse effect (n = 14) in each group. | Nasal irrigations performed in large volumes and delivered with low positive pressure are more effective than saline sprays for treatment of chronic nasal and sinus symptoms in a community-based population. |
| Karpova, 2008 [61] | Open-label parallel-group trial | 84 children with chronic tonsilitis | Experimental group with 64 subjects using Aqua Maris seawater solution, and control group using furacilin solution for 6–8 courses of crypt lavage. | No adverse effects mentioned. | Aqua Maris group showed superior results in terms of odynophagia and dysphagia severity and duration, and hyperaemia and infiltration of the palatine arches. |
| Slapak, 2008 [62] | Prospective RCT in parallel groups | 401 children with cold or influenza | Nasal saline irrigation delivered via jet flow or fine spray, or added to standard medication vs. standard medication alone. Applied 6 times daily in acute phase and 3 times daily for 12 weeks thereafter. | At the second visit, only 8.7% patients recorded nasal wash complaints, and at the final visit, this dropped to 2.4%. The other reported complaints were burning, bitter taste and nose bleeding. | The saline treatment was well tolerated. Most complaints appeared in the medium jet group and were associated with the stronger flow of the wash. |
| Süslü, 2009 [28] | Prospective RCT | 45 adult subjects after septoplasty | 2.3% buffered hypertonic seawater, buffered isotonic saline, unbuffered isotonic saline; irrigation six times daily for 20 days. | No dropouts; no adverse events mentioned. | Buffered isotonic saline group had worse nasal burning VAS score when compared with both buffered hypertonic and nonbuffered isotonic saline solutions. |
| Ural, 2009 [63] | Observational | 132 adult subjects | Control, allergic rhinitis, acute sinusitis and chronic sinusitis groups received two daily doses of hypertonic (3%) or isotonic nasal irrigation for 10 days. | No patients lost to follow up, and no serious side effects or intolerance necessitating cessation of irrigation reported. | Nasal irrigation with isotonic or hypertonic saline can improve mucociliary clearance time in various nasal pathologies. |
| Gelardi, 2009 [64] | Randomized pilot study | 20 adult subjects with acute rhinosinusitis | A nasal syringe (10 mL saline solution, 3 times daily for 14 days) or the Lavonase system (250 mL saline solution sac, twice daily for 14 days). | No adverse effects mentioned. | Nasal irrigation with the Lavonase system was found to be more effective in reducing symptoms and decreasing nasal resistances. |
| Li, 2009 [65] | RCT | 26 children with allergic rhinitis | Saline irrigation, steroid therapy, saline + steroid therapy groups; twice a day for 8 weeks. | No subjects lost to follow up; no adverse events in saline group. | As adjunctive treatment, nasal saline irrigation alleviates the symptoms and signs of allergic rhinitis in children, and decreases use of topical steroids. |
| Rabago, 2009 [66] | Electronic questionnaire | 330 practicing family physicians in Wisconsin, US | Saline nasal irrigation for upper respiratory conditions. | Respondents were not queried directly about perceived safety profile of the treatment. | Analysis showed that 86.7% of respondents have used the treatment as adjunctive care for conditions including chronic rhinosinusitis (91%), acute bacterial rhinosinusitis (67%), seasonal allergic rhinitis (66%), viral upper respiratory infection (59%), other allergic rhinitis (48%), irritant based congestion (48%) and rhinitis of pregnancy (17%). |
| Cingi, 2010 [16] | Prospective | 100 adult subjects with allergic rhinitis | Seawater gel nasal spray in 4-h intervals, two sprays per nostril, from morning till evening for 10 days. | Gel was well-tolerated with no side-effects occurring. | Clinical findings evaluation revealed a statistically significantly decreased rate of nasal congestion and discharge after a 10-day regimen of seawater nasal spray. |
| Culig, 2010 [67] | RCT | 60 patients with chronic rhinosinusitis | Isotonic vs. hypertonic seawater spray solution, applied 3–6 times daily. | No adverse events were observed. | Hypertonic solution was statistically significantly superior to the isotonic for all symptoms. |
| Miraglia Del Giudice, 2011 [68] | RCT | 40 children with seasonal allergic rhinitis | Nasal lavage with Ischia thermal water vs. isotonic saline. | No significant side effects in either group. | Nasal lavage hyper-mineral chloride-sodium water was effective in children with seasonal allergic rhinitis. |
| Miraglia Del Giudice, 2012 [69] | RCT | 34 infants with bronchiolitis | Nebulized normal saline or 3% hypertonic solution in addition to epinephrine and to conventional treatment | Both treatments have an excellent safety profile. | Administration of 3% hypertonic saline is more effective than normal saline in combination with epinephrine in hospitalized children with bronchiolitis. |
| Hermelingmeier, 2012 [70] | Systematic review and meta-analysis | 400 subjects of which 86 were children/adolescent and 45 were pregnant | Different treatments. | No adverse events mentioned, however not all studies included safety outcomes. | Saline nasal irrigation using isotonic solution can be recommended as complementary therapy in allergic rhinitis. |
| Satdhabudha, 2012 [71] | Prospective RCT | 81 children with allergic rhinitis | Buffered hypertonic (1.25%) saline or isotonic saline; nasal irrigation 2 times daily for 4 weeks. | One subject in each study group experienced nasal burning during the first use. | Satisfaction with nasal irrigation was comparable between groups. |
| Tantilipikorn, 2012 [72] | Prospective RCT | 50 adult subjects with chronic rhinosinusitis after endoscopic surgery | Dexpanthenol (Mar Plus) vs. isotonic saline nasal sprays; 4 applications weekly on 1st, 2nd, 4th and 6th postoperative weeks. | Dropout rate was comparable between groups. Three subjects in nasal saline group reported burning sensation. | Product containing seawater (Mar Plus) had better efficacy and comparable safety to nasal saline. |
| Kumar, 2013 [73] | RCT | 50 subjects with chronic sinusitis | Hypertonic (3.5%) or isotonic nasal saline; 10 drops, three times a day in both nostrils for 4 weeks. | None of the patients’ groups reported severe burning sensation. Mild burning sensation was reported by 14.3% in isotonic group and by 57.1% in hypertonic group. Moderate burning sensation was reported by 19% of patients in hypertonic group. | Hypertonic saline nasal solution was more efficacious and well tolerated, and it improved quality of life in patients. |
| Chen, 2014 [74] | Parallel design with 3 groups | 61 children with allergic rhinitis | Nasal irrigation, intranasal corticosteroid, and combined treatment. | No adverse events reported by subjects. | Nasal irrigation and decreased nasal corticosteroids in combination effected a significant improvement in symptoms and signs, and a significant decrease in the mean eosinophile count in nasal secretions were observed at week 12. |
| Low, 2014 [75] | RCT | 74 adult subjects after endoscopic sinus surgery | Normal saline, Ringer’s solution and hypertonic saline group. | No adverse events mentioned. | All groups showed an improvement with treatment in SNOT-20 scores and VAS scores, as well as endoscopic evaluation of mucosa appearance over time, but no improvement of MCC. |
| Marchisio, 2014 [76] | Questionnaire sent by e-mail | 860 primary care paediatricians | Nasal saline irrigation in preschool children. | 98.3% of the participating physicians evaluated the treatment as effective and safe. | About 40% of physicians expressed doubts about parental compliance, mainly because of a certain difficulty in administration or the supposed invasiveness of the procedure. |
| Nguyen, 2014 [77] | Prospective, unblinded, single-arm pilot study | 40 subjects with allergic rhinitis | Large-volume low-pressure saline irrigation twice daily for 8 weeks to the ongoing regiment of nasal corticosteroids. | No adverse events reported. | Saline treatment significantly improved QOL, with no significant changes in nasal flows, pattern use of nasal steroids or adverse events. |
| Pham, 2014 [78] | Retrospective cohort study and cross-sectional survey | 144 children with paediatric chronic rhinosinusitis | 6 weeks of once-daily nasal irrigation. | The results of a long-term (median of 48 months) follow-up in 54 participants show treatment as safe and well-tolerated. | Nasal irrigation is effective as a first-line treatment for paediatric chronic rhinosinusitis and subsequent nasal symptoms, and reduces need for FESS and CT imaging. |
| Stoelzel, 2014 [79] | RCT | 20 adult subjects with allergic rhinitis | Nasya/Prevalin (a thixotropic nasal gel) vs. isotonic seawater nasal spray; 2 sprays (2 × 0.14 mL) into each nostril. | Three mild AEs were documented in two subjects in the Nasya/Prevalin group (swallowing difficulties, nasal airways obstruction and headache); none related to the application of the investigational product. | There was no difference between the two treatment groups regarding the global assessment of tolerability provided by the investigators or by the subjects. |
| Wang, 2014 [80] | Prospective, placebo-controlled RCT | 60 atopic children with acute sinusitis | Standard treatment (including systemic antibiotics, mucolytics and nasal decongestants) with nasal irrigation with normal saline vs. standard treatment alone. | No significant side effects were recorded in the isotonic saline irrigation group. | There were significant improvements in mean PRQLQ and nPEFR values for the irrigation compared to the non-irrigation group. There was no significant difference in radiographic findings between the groups. The irrigation group recorded significant improvements in eye congestion, rhinorrhea, nasal itching, sneezing and cough symptoms. |
| Alvarez-Puebla, 2015 [81] | CT | 35 adults with asthma | Hypertonic saline (5%, administered by nebulizer) or mannitol. | Treatments were well tolerated. | Mannitol and hypertonic saline behaved similarly at sputum induction. |
| Koksal, 2016 [82] | Prospective, randomized double-blind trial | 109 children under 2 years of age with acute upper respiratory infection | Saline nasal drops (0.9%), seawater nasal drops (2.3%) and control group (no treatment). | No adverse events mentioned. | No significant difference between saline and seawater groups in terms of nasal congestion, but a significant difference between the control group and these two groups. |
| Bennett, 2015 [18] | RCT, open label, cross-over | 12 healthy adults | Hypertonic saline; 2.8% NaCl, 4 mL. | No adverse events mentioned. | Inhaled 2.8% hypertonic saline in normal subjects was associated with a short-lived acceleration of MC, predominately in the central airways. |
| Bonnomet, 2016 [17] | Randomized, controlled, blinded, in vitro study | Airway epithelial cells obtained from 13 nasal polyp explants | Response (ciliary beat frequency and epithelial wound repair speed) of cells to 3 isotonic nasal irrigation solutions: normal saline 0.9%; non-diluted seawater; and 30% diluted seawater | In vitro study. | Non-diluted seawater obtains the best results on ciliary beat frequency and wound-repair speed vs. normal saline showing a deleterious effect on epithelial cell function. |
| Grasso, 2018 [83] | Prospective, controlled clinical trial | 60 patients with allergic rhinitis | Daily, 5-month treatment with isotonic seawater nasal spray enriched with manganese (4 puffs/day). | No adverse events mentioned. | The treatment significantly decreased the number of episodes of acute allergic rhinitis and increased QOL without the adverse effects of the standard care therapy. |
| Bergmann, 2019 [84] | Uncontrolled, prospective, longitudinal CT | 136 patients with disorders of nose and paranasal sinuses including 11 pregnant women and one nursing mother | Seawater nasal spray (2.7%). | One adverse event reported (epistaxis). | Over the study period (mean 44 days) statistically significant reductions in 10 out of 12 symptoms was found. Only for parameters “impairment of taste” and “impairment of food intake” was no significant change in symptoms observed. |
| Bogomil’skij, 2019 [85] | Uncontrolled, prospective, longitudinal CT | Children aged 2–5 years with acute infectious rhinitis (some with viral comorbidity) | Aqua Maris spray. | None reported. | Rapid regression of symptoms, such as nasal congestion and snoring, a decrease in the amount of nasal discharge by the 3rd day from the start of drug use and normalization of the rhinoscopic findings by the 5th–7th day of treatment. |
| Stobbelaar, 2019 [86] | Retrospective study | 104 children up to 2 years of age with bronchiolitis in intensive care unit | Nebulised hypertonic saline. | No adverse events mentioned. | In respiratory syncytial virus positive patients, the use of nebulised hypertonic saline was correlated with a decrease in the duration of respiratory support and the length of stay by factors 0.72 and 0.81, respectively. |
| Craig, 2019 [87] | Prospective, randomised, controlled, double-blind, superiority trial | 107 children aged 6 months to 5 years planned to have a nasogastric tube inserted in emergency department | Lidocaine and phenylephrine nasal spray or 0.9% sodium chloride placebo nasal spray, before nasogastric insertion. | Adverse effects occurred in 28% of those who received lidocaine and phenylephrine, and 42% of those who received placebo. | Lidocaine and phenylephrine nasal spray does not reduce procedure-related distress associated with nasogastric tube insertion in young children compared with saline. |
| Perić, 2019 [88] | Prospective, randomized study | 30 patients with aspirin-induced chronic rhinosinusitis undergoing endoscopic sinus surgery | Hypertonic (2.3% NaCl) seawater and isotonic 0.9% NaCl. | Nasal discomforts were detected in two patients in hypertonic seawater group and in two patients in the isotonic group. | Significantly lower total symptom score during the 7th, 14th, 21st and 28th days, lower total endoscopic score on the 21st and 28th days, lower nasal obstruction, facial pain/pressure, headache and trouble sleeping, and lower nasal mucosal oedema, nasal secretion and nasal crusting in patients treated by hypertonic seawater. |
| Ramalingam, 2020 [89] | Post-hoc secondary analysis of data from the Edinburgh and Lothians Viral Intervention Study | 66 adults with upper respiratory tract infection | The intervention group used hypertonic saline at home and performed nasal irrigation and gargling up to 12 times/day. Control arm participants did not use a specific treatment. | None mentioned. | The duration of illness was shorter in the intervention arm in the subset of patients infected with coronavirus (mean 5.6 vs. 8.1 days). The difference in the duration of blocked nose was −3.1 days, cough −3.3 days and hoarseness of voice −2.9 days in favour of hypertonic saline treatment. |
| Huang, 2021 [90] | In vitro | A 3D reconstituted human nasal epithelium model; mixture of human nasal cells isolated from 14 donors. | Seawater preparation (Stérimar Nasal Hygiene), tissue integrity via transepithelial electrical resistance was measured. | In vitro study. | Treatment did not compromise the integrity of the nasal epithelium in vitro but was effective for removal of foreign particles through MCC increase and for enhancing wound repair on nasal mucosa. |
| Jiang, 2021 [91] | Multicentre retrospective cohort trial | 144 adult subjects with upper respiratory tract infections | Non-drug supportive treatment vs. supportive treatment and nasal irrigation with sea-salt-derived physiological saline. | No adverse events reported. | Seawater group was statistically significantly superior in terms of nasal congestion, nasal discharge, sleep quality and appetite, but not for cough and fatigue. |
| Study | Design | Indication(s) | Intervention(s) | Remarks |
|---|---|---|---|---|
| Papsin, 2003 [27] | Literature review | Rhinosinusitis, allergic rhinitis, postoperative irrigation, common cold | Nasal irrigation as an adjunct treatment | The procedure has been used safely by both adults and children and has no documented serious adverse effects. Trials indicate that patients treated with nasal irrigation rely less on other medications, and that some postsurgical patients tend to require fewer visits to physicians. Both effects are likely to have desirable economic consequences for patients and the health care system. |
| Brown, 2004 [93] | Literature review | (Chronic) sinusitis, sinonasal conditions, rhinitis, postoperative patients | Isotonic and hypertonic saline, buffered/unbuffered solutions, additives such as antibacterial or antifungal agents, home recipes vs. manufactured solutions | Nasal irrigations are an important component in the management of most sinonasal conditions. Authors note a disparity of opinion about the effects of irrigations on ciliary beat frequency and mucociliary clearance and controversy concerning irrigation tonicity and the use of additives to the irrigating solution. |
| Harvey, 2007 [94] | Review (Cochrane) | Chronic sinusitis | Randomised controlled trials in which saline was evaluated in comparison with either no treatment, a placebo, as an adjunct to other treatments or against treatments. The comparison of hypertonic versus isotonic solutions. | Saline irrigations are well tolerated. Although minor side effects are common, the beneficial effect of saline appears to outweigh these drawbacks for the majority of patients. The use of topical saline could be included as a treatment adjunct for the symptoms of chronic rhinosinusitis. |
| Kassel, 2010 [95] | Review (Cochrane) | Upper respiratory tract infections | RCTs comparing topical nasal saline treatment to other interventions in adults and children with clinically diagnosed acute URTIs. | Three RCTs (618 participants) were included. Most results showed no difference between nasal saline treatment and control. However, there was limited evidence of benefit with nasal saline irrigation in adults. Minor discomfort was not uncommon and 40% of babies did not tolerate nasal saline drops. |
| Zhang, 2008 [96] | Review (Cochrane) | Acute bronchiolitis in infants | Nebulized hypertonic saline alone or in conjunction with bronchodilators as an active intervention in infants with acute bronchiolitis. | Current evidence suggests nebulized 3% saline may significantly reduce the length of hospital stay among infants hospitalized with non-severe acute viral bronchiolitis and improve the clinical severity score in both outpatient and inpatient populations. |
| Adappa, 2012 [97] | Literature review | Rhinosinusitis | Saline irrigation (hypertonic vs. physiologic), saline spray, antibiotics, topical steroids, topical antifungal treatment, anti IL-5 treatment | Physiologic saline irrigation is beneficial in the treatment of symptoms of CRS. Low-level evidence supports the effectiveness of topical antibiotics in the treatment of CRS. The use of topical antifungals is not supported by the majority of studies. Intranasal steroids are beneficial in the treatment of CRS with nasal polyposis. There is insufficient evidence to demonstrate a clear overall benefit for topical steroids in CRS without nasal polyposis. |
| Chirico, 2014 [98] | Literature review | Nasal congestion in infants and children | Nasal saline | The use of isotonic and hypertonic saline solutions is a valuable non-pharmacological treatment for nasal congestion in children, especially by improving mucociliary clearance and reducing the use of medications (antihistamines, decongestants, antibiotics, corticosteroids) during the treatment of URTIs. They are well tolerated and can be recommended for infants. |
| Bastier, 2015 [20] | Overview of randomized clinical trials | Different sinonasal pathologies and postoperative care | Different treatments compared to nasal irrigation including rhinocorticoids, antihistamines, buffered, unbuffered, alkaline hypertonic and isotonic saline | Large-volume low-pressure nasal irrigation using undiluted seawater seems, according to the present state of knowledge, to be the most effective protocol. |
| Chong, 2016 [99] | Review (Cochrane) | Chronic rhinosinusitis | Studies with follow-up periods of at least three months comparing saline delivered to the nose by any means (douche, irrigation, drops, spray or nebuliser) with placebo, no treatment or other pharmacological interventions | The evidence suggests that there is no benefit from a low-volume nebulised saline spray as opposed to intranasal steroids. There is some benefit from daily, large-volume (150 mL) saline irrigation with a hypertonic solution when compared with placebo. |
| Baron, 2016 [39] | Literature review | Bronchiolitis in infants | Hypertonic saline | Authors agree with the AAP guidelines regarding the use of nebulised hypertonic saline to reduce bronchiolitis scores and length of stay for infants with bronchiolitis who are expected to be hospitalised for more than 72 h. |
| Madison, 2016 [100] | Literature review | Allergic rhinitis in children | Nasal saline irrigation vs. intranasal corticosteroids | Intranasal steroids are more effective than nasal saline alone in reducing symptoms of allergic rhinitis in children. However, combination therapy further improves symptom reduction. |
| Kanjanawasee, 2018 [101] | Systematic search with Ovid MEDLINE, Scopus, PubMed and Google Scholar | Sinonasal diseases, including rhinitis and rhinosinusitis | Hypertonic vs. isotonic saline | Nine studies (740 patients) were included. Hypertonic nasal irrigation brought greater benefits than isotonic treatment in symptom reduction; however, no difference was shown in SNOT-20 improvement. Effects favouring hypertonic solution were greater in patients with rhinitis compared with rhinosinusitis; in patients under the age of 18 years; in saline irrigation using high volume compared with low volume and in saline irrigation with hypertonicity of <3% and hypertonicity of 3–5% compared with hypertonicity of >5%. No major adverse effects were reported. |
| Li, 2019 [102] | Systematic review and meta-analysis literature following the PRISMA guidelines | Allergic rhinitis in children | Hypertonic saline nasal irrigation | Hypertonic saline treatment improved patients’ nasal symptom scores and significantly lowered rescue antihistamine use rate. Analyses comparing hypertonic with isotonic saline nasal irrigation found better nasal symptom scores in hypertonic group, although the antihistamine use and adverse-effect rates were similar between groups. |
| King, 2019 [103] | Literature review with evidence for each of the indications | Chronic sinusitis, allergic rhinitis, acute URTI | Saline solutions, dependent on the indication studied | Saline nasal irrigation is recommended as an adjunct therapy for common colds/rhinosinusitis, chronic sinusitis, allergic rhinitis and after nasal surgery. It appears to be safe and generally well tolerated, even for children. The use of SNI has the potential to reduce the number of antibiotic prescriptions for acute and chronic sinus infections, and improve outcomes for patients. |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Štanfel, D.; Kalogjera, L.; Ryazantsev, S.V.; Hlača, K.; Radtsig, E.Y.; Teimuraz, R.; Hrabač, P. The Role of Seawater and Saline Solutions in Treatment of Upper Respiratory Conditions. Mar. Drugs 2022, 20, 330. https://doi.org/10.3390/md20050330
Štanfel D, Kalogjera L, Ryazantsev SV, Hlača K, Radtsig EY, Teimuraz R, Hrabač P. The Role of Seawater and Saline Solutions in Treatment of Upper Respiratory Conditions. Marine Drugs. 2022; 20(5):330. https://doi.org/10.3390/md20050330
Chicago/Turabian StyleŠtanfel, Danijela, Livije Kalogjera, Sergej V. Ryazantsev, Kristina Hlača, Elena Y. Radtsig, Rashidov Teimuraz, and Pero Hrabač. 2022. "The Role of Seawater and Saline Solutions in Treatment of Upper Respiratory Conditions" Marine Drugs 20, no. 5: 330. https://doi.org/10.3390/md20050330
APA StyleŠtanfel, D., Kalogjera, L., Ryazantsev, S. V., Hlača, K., Radtsig, E. Y., Teimuraz, R., & Hrabač, P. (2022). The Role of Seawater and Saline Solutions in Treatment of Upper Respiratory Conditions. Marine Drugs, 20(5), 330. https://doi.org/10.3390/md20050330