Herring Milt Protein Hydrolysate Improves Insulin Resistance in High-Fat-Diet-Induced Obese Male C57BL/6J Mice
Abstract
1. Introduction
2. Results
2.1. Chemical Composition of HPH
2.2. Body Weight and Food Intake
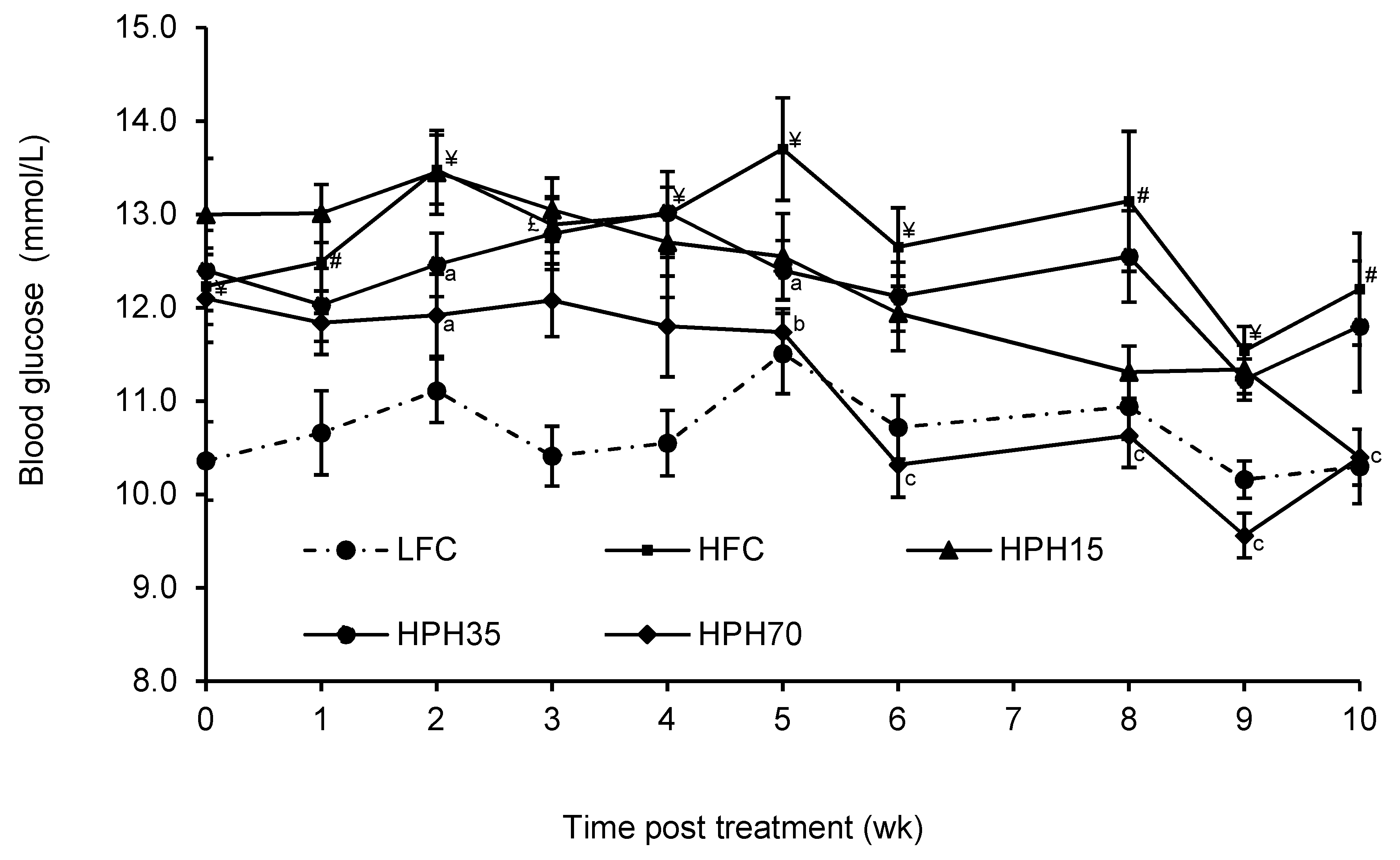
2.3. Blood Glucose
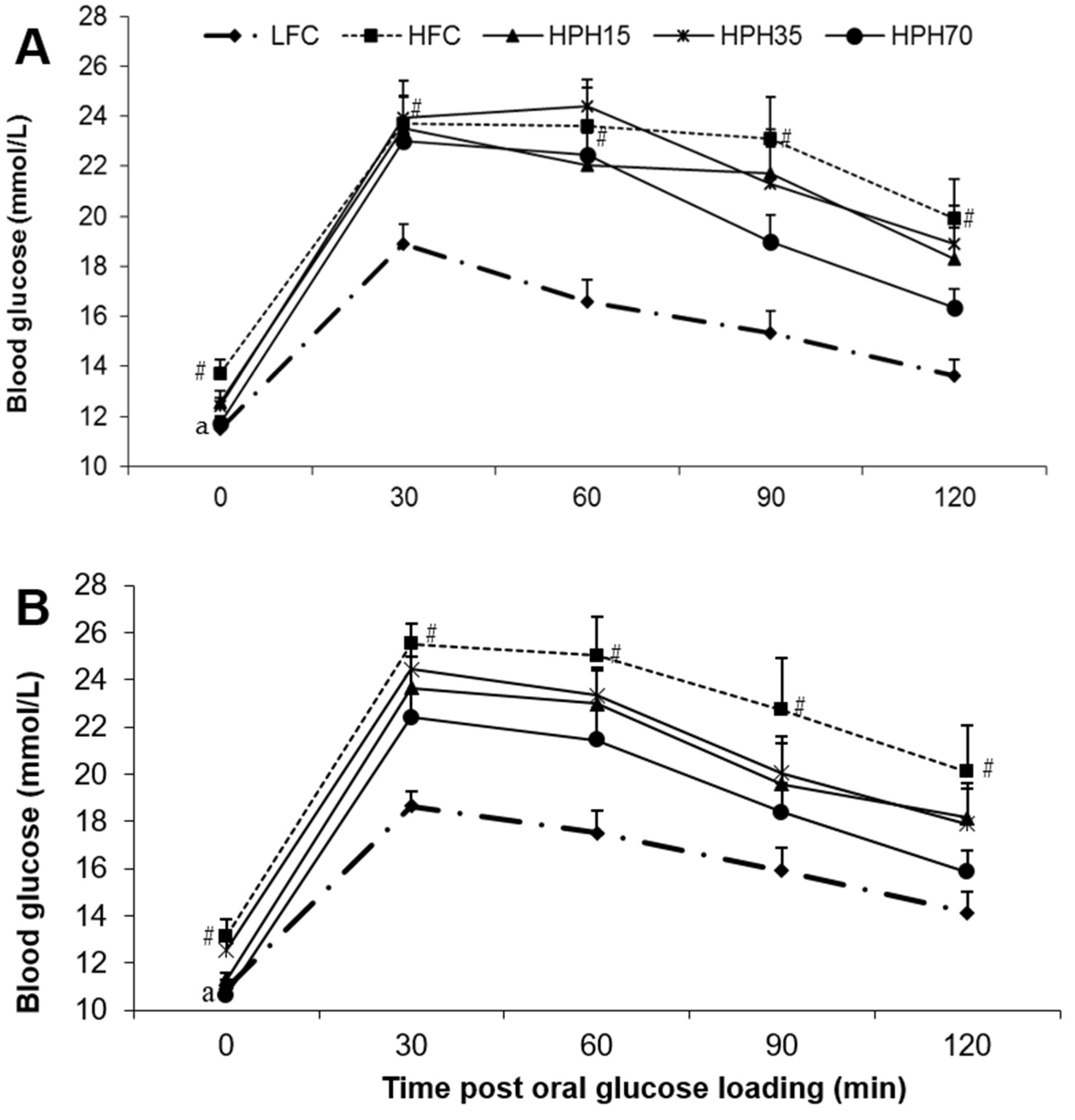
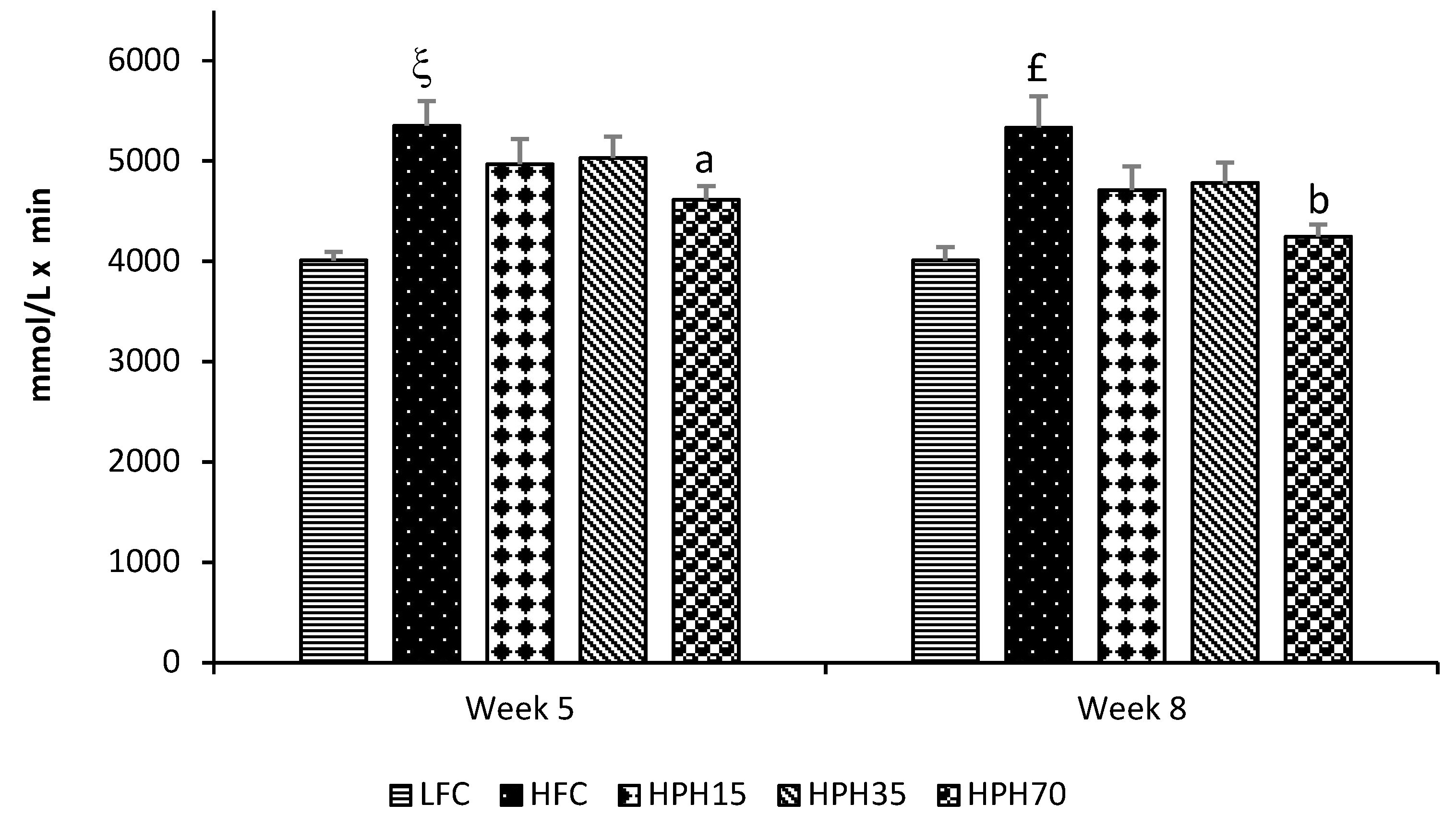
2.4. Oral Glucose Tolerance
2.5. Fasting Serum Insulin, Leptin, Adiponectin, and Free Fatty Acids
2.6. HOMA-IR and HOMA-β
2.7. Fasting Serum Total Cholesterol and Triglycerides
3. Discussion
4. Materials and Methods
4.1. Preparation of HPH
4.2. Analysis of HPH
4.3. Animals and Diets
4.4. Oral Glucose Tolerance Test
4.5. Serum Insulin, Leptin, and Adiponectin Analysis
4.6. Homeostasis Model Assessment of Insulin Resistance and β-Cell Function
4.7. Analysis of Serum Lipids
4.8. Analysis of Serum Glucose
4.9. Statistical Analysis
Supplementary Materials
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Sami, W.; Ansari, T.; Butt, N.S.; Hamid, M.R.A. Effect of diet on type 2 diabetes mellitus: A review. Int. J. Health Sci. 2017, 11, 65–71. [Google Scholar]
- Cho, N.H.; Shaw, J.E.; Karuranga, S.; Huang, Y.; da Rocha Fernandes, J.D.; Ohlrogge, A.W.; Malanda, B. IDF Diabetes Atlas: Global estimates of diabetes prevalence for 2017 and projections for 2045. Diabetes Res. Clin. Pract. 2018, 138, 271–281. [Google Scholar] [CrossRef] [PubMed]
- Harvie, M.N.; Pegington, M.; Mattson, M.P.; Frystyk, J.; Dillon, B.; Evans, G.; Cuzick, J.; Jebb, S.A.; Martin, B.; Cutler, R.G.; et al. The effects of intermittent or continuous energy restriction on weight loss and metabolic disease risk markers: A randomized trial in young overweight women. Int. J. Obes. 2011, 35, 714–727. [Google Scholar] [CrossRef] [PubMed]
- Diabetes Prevention Program Research Group. Long-term effects of lifestyle intervention or metformin on diabetes development and microvascular complications over 15-year follow-up: The Diabetes Prevention Program Outcomes Study. Lancet Diabetes Endocrinol. 2015, 3, 866–875. [Google Scholar] [CrossRef]
- Shah, S.H.; Crosslin, D.R.; Haynes, C.S.; Nelson, S.; Turer, C.B.; Stevens, R.D.; Muehlbauer, M.J.; Wenner, B.R.; Bain, J.R.; Laferrere, B.; et al. Branched-chain amino acid levels are associated with improvement in insulin resistance with weight loss. Diabetologia 2012, 55, 321–330. [Google Scholar] [CrossRef] [PubMed]
- Unnikrishnan, R.; Pradeepa, R.; Joshi, S.R.; Mohan, V. Type 2 Diabetes: Demystifying the Global Epidemic. Diabetes 2017, 66, 1432–1442. [Google Scholar] [CrossRef]
- Storlien, L.H.; Higgins, J.A.; Thomas, T.C.; Brown, M.A.; Wang, H.Q.; Huang, X.F.; Else, P.L. Diet composition and insulin action in animal models. Br. J. Nutr. 2000, 83, S85–S90. [Google Scholar] [CrossRef]
- Tremblay, F.; Lavigne, C.; Jacques, H.; Marette, A. Dietary cod protein restores insulin-induced activation of phosphatidylinositol 3-kinase/Akt and GLUT4 translocation to the T-tubules in skeletal muscle of high-fat-fed obese rats. Diabetes 2003, 52, 29–37. [Google Scholar] [CrossRef][Green Version]
- Sluijs, I.; Beulens, J.W.; van der, A.D.; Spijkerman, A.M.; Grobbee, D.E.; van der Schouw, Y.T. Dietary intake of total, animal, and vegetable protein and risk of type 2 diabetes in the European Prospective Investigation into Cancer and Nutrition (EPIC)-NL study. Diabetes Care 2010, 33, 43–48. [Google Scholar] [CrossRef]
- Beasley, J.M.; Wylie-Rosett, J. The role of dietary proteins among persons with diabetes. Curr. Atheroscler. Rep. 2013, 15, 348. [Google Scholar] [CrossRef]
- Luukkonen, P.K.; Sadevirta, S.; Zhou, Y.; Kayser, B.; Ali, A.; Ahonen, L.; Lallukka, S.; Pelloux, V.; Gaggini, M.; Jian, C.; et al. Saturated Fat Is More Metabolically Harmful for the Human Liver Than Unsaturated Fat or Simple Sugars. Diabetes Care 2018, 41, 1732–1739. [Google Scholar] [CrossRef] [PubMed]
- Madani, Z.; Louchami, K.; Sener, A.; Malaisse, W.J.; Ait Yahia, D. Dietary sardine protein lowers insulin resistance, leptin and TNF-alpha and beneficially affects adipose tissue oxidative stress in rats with fructose-induced metabolic syndrome. Int. J. Mol. Med. 2012, 29, 311–318. [Google Scholar] [PubMed]
- Ouellet, V.; Marois, J.; Weisnagel, S.J.; Jacques, H. Dietary cod protein improves insulin sensitivity in insulin-resistant men and women: A randomized controlled trial. Diabetes Care 2007, 30, 2816–2821. [Google Scholar] [CrossRef] [PubMed]
- Huynh, M.D.; Kitts, D.D.; Hu, C.; Trites, A.W. Comparison of fatty acid profiles of spawning and non-spawning Pacific herring, Clupea harengus pallasi. Comp. Biochem. Physiol. B Biochem. Mol. Biol. 2007, 146, 504–511. [Google Scholar] [CrossRef] [PubMed]
- Bjorndal, B.; Burri, L.; Wergedahl, H.; Svardal, A.; Bohov, P.; Berge, R.K. Dietary supplementation of herring roe and milt enhances hepatic fatty acid catabolism in female mice transgenic for hTNFalpha. Eur. J. Nutr. 2012, 51, 741–753. [Google Scholar] [CrossRef] [PubMed]
- Qatanani, M.; Lazar, M.A. Mechanisms of obesity-associated insulin resistance: Many choices on the menu. Genes Dev. 2007, 21, 1443–1455. [Google Scholar] [CrossRef] [PubMed]
- Plante, S.; Beland, F.; Tchoukanova, N.; Gagnon, J. Novel meals from Eastern Canada’s marine fishery by-products as alternative to fishmeal. J. Aquat. Food Prod. Technol. 2017, 26, 366–374. [Google Scholar] [CrossRef]
- Wang, Y.; Fofana, B.; Roy, M.; Ghose, K.; Yao, X.H.; Nixon, M.S.; Hair, S.; Nyomba, G.B.L. Flaxseed lignan secoisolariciresinol diglucoside improves insulin sensitivity through upregulation of GLUT4 expression in diet-induced obese mice. J. Funct. Foods 2015, 18, 1–9. [Google Scholar] [CrossRef]
- Nair, S.; Gagnon, J.; Pelletier, C.; Tchoukanova, N.; Zhang, J.; Ewart, H.S.; Ewart, K.V.; Jiao, G.; Wang, Y. Shrimp oil extracted from the shrimp processing waste reduces the development of insulin resistance and metabolic phenotypes in diet-induced obese rats. Appl. Physiol. Nutr. Metab. 2017, 42, 841–849. [Google Scholar] [CrossRef]
- Droz, B.A.; Sneed, B.L.; Jackson, C.V.; Zimmerman, K.M.; Michael, M.D.; Emmerson, P.J.; Coskun, T.; Peterson, R.G. Correlation of disease severity with body weight and high fat diet in the FATZO/Pco mouse. PLoS ONE 2017, 12, e0179808. [Google Scholar] [CrossRef]
- Hosomi, R.; Yoshida, M.; Fukunaga, K. Seafood consumption and components for health. Glob. J. Health Sci. 2012, 4, 72–86. [Google Scholar] [CrossRef] [PubMed]
- Bjorndal, B.; Berge, C.; Ramsvik, M.S.; Svardal, A.; Bohov, P.; Skorve, J.; Berge, R.K. A fish protein hydrolysate alters fatty acid composition in liver and adipose tissue and increases plasma carnitine levels in a mouse model of chronic inflammation. Lipids Health Dis. 2013, 12, 143. [Google Scholar] [CrossRef] [PubMed]
- Couet, C.; Delarue, J.; Ritz, P.; Antoine, J.M.; Lamisse, F. Effect of dietary fish oil on body fat mass and basal fat oxidation in healthy adults. Int. J. Obes. Relat. Metab. Disord. 1997, 21, 637–643. [Google Scholar] [CrossRef] [PubMed]
- Logan, S.L.; Spriet, L.L. Omega-3 Fatty Acid Supplementation for 12 Weeks Increases Resting and Exercise Metabolic Rate in Healthy Community-Dwelling Older Females. PLoS ONE 2015, 10, e0144828. [Google Scholar] [CrossRef] [PubMed]
- Jensen, I.J.; Walquist, M.; Liaset, B.; Elvevoll, E.O.; Eilertsen, K.E. Dietary intake of cod and scallop reduces atherosclerotic burden in female apolipoprotein E-deficient mice fed a Western-type high fat diet for 13 weeks. Nutr. Metab. 2016, 13, 8. [Google Scholar] [CrossRef] [PubMed]
- Nagy, C.; Einwallner, E. Study of In Vivo Glucose Metabolism in High-fat Diet-fed Mice Using Oral Glucose Tolerance Test (OGTT) and Insulin Tolerance Test (ITT). J. Vis. Exp. 2018, 131, e56672. [Google Scholar] [CrossRef] [PubMed]
- Williams, L.M.; Campbell, F.M.; Drew, J.E.; Koch, C.; Hoggard, N.; Rees, W.D.; Kamolrat, T.; Thi Ngo, H.; Steffensen, I.L.; Gray, S.R.; et al. The development of diet-induced obesity and glucose intolerance in C57BL/6 mice on a high-fat diet consists of distinct phases. PLoS ONE 2014, 9, e106159. [Google Scholar] [CrossRef]
- Lavigne, C.; Marette, A.; Jacques, H. Cod and soy proteins compared with casein improve glucose tolerance and insulin sensitivity in rats. Am. J. Physiol. Endocrinol. Metab. 2000, 278, E491–E500. [Google Scholar] [CrossRef]
- Lee, C.; Liese, A.; Wagenknecht, L.; Lorenzo, C.; Haffner, S.; Hanley, A. Fish consumption, insulin sensitivity and beta-cell function in the Insulin Resistance Atherosclerosis Study (IRAS). Nutr. Metab. Cardiovasc. Dis. 2013, 23, 829–835. [Google Scholar] [CrossRef]
- Dale, H.F.; Madsen, L.; Lied, G.A. Fish–derived proteins and their potential to improve human health. Nutr. Rev. 2019, 77, 572–583. [Google Scholar] [CrossRef]
- Acosta-Montano, P.; Garcia-Gonzalez, V. Effects of Dietary Fatty Acids in Pancreatic Beta Cell Metabolism, Implications in Homeostasis. Nutrients 2018, 10, 393. [Google Scholar] [CrossRef]
- Kim, K.S.; Oh, D.H.; Kim, J.Y.; Lee, B.G.; You, J.S.; Chang, K.J.; Chung, H.J.; Yoo, M.C.; Yang, H.I.; Kang, J.H.; et al. Taurine ameliorates hyperglycemia and dyslipidemia by reducing insulin resistance and leptin level in Otsuka Long-Evans Tokushima fatty (OLETF) rats with long-term diabetes. Exp. Mol. Med. 2012, 44, 665–673. [Google Scholar] [CrossRef]
- Torris, C.; Smastuen, M.C.; Molin, M. Nutrients in Fish and Possible Associations with Cardiovascular Disease Risk Factors in Metabolic Syndrome. Nutrients 2018, 10, 952. [Google Scholar] [CrossRef]
- Chen, W.; Guo, J.; Zhang, Y.; Zhang, J. The beneficial effects of taurine in preventing metabolic syndrome. Food Funct. 2016, 7, 1849–1863. [Google Scholar] [CrossRef]
- L’Amoreaux, W.J.; Cuttitta, C.; Santora, A.; Blaize, J.F.; Tachjadi, J.; El Idrissi, A. Taurine regulates insulin release from pancreatic beta cell lines. J. Biomed. Sci. 2010, 17, S11. [Google Scholar] [CrossRef]
- Thams, P.; Capito, K. L-arginine stimulation of glucose-induced insulin secretion through membrane depolarization and independent of nitric oxide. Eur. J. Endocrinol. 1999, 140, 87–93. [Google Scholar] [CrossRef]
- Leiss, V.; Flockerzie, K.; Novakovic, A.; Rath, M.; Schonsiegel, A.; Birnbaumer, L.; Schurmann, A.; Harteneck, C.; Nurnberg, B. Insulin secretion stimulated by L-arginine and its metabolite L-ornithine depends on Galpha(i2). Am. J. Physiol. Endocrinol. Metab. 2014, 307, E800–E812. [Google Scholar] [CrossRef]
- Yuan, C.S.; Attele, A.S.; Zhang, L.; Lynch, J.P.; Xie, J.T.; Shi, Z.Q. Leptin reduces body weight gain in neonatal rats. Pediatr. Res. 2000, 48, 380–383. [Google Scholar] [CrossRef][Green Version]
- Calapai, G.; Corica, F.; Corsonello, A.; Sautebin, L.; Di Rosa, M.; Campo, G.M.; Buemi, M.; Mauro, V.N.; Caputi, A.P. Leptin increases serotonin turnover by inhibition of brain nitric oxide synthesis. J. Clin. Investig. 1999, 104, 975–982. [Google Scholar] [CrossRef]
- Zhao, W.; Feng, X.; Liu, B.; Xian, J.; Zhang, N. Er-Miao-Fang Extracts Inhibits Adipose Lipolysis and Reduces Hepatic Gluconeogenesis via Suppression of Inflammation. Front. Physiol. 2018, 9, 1041. [Google Scholar] [CrossRef]
- Zhao, W.; Li, A.; Feng, X.; Hou, T.; Liu, K.; Liu, B.; Zhang, N. Metformin and resveratrol ameliorate muscle insulin resistance through preventing lipolysis and inflammation in hypoxic adipose tissue. Cell Signal. 2016, 28, 1401–1411. [Google Scholar] [CrossRef]
- Kowalski, G.M.; De Souza, D.P.; Burch, M.L.; Hamley, S.; Kloehn, J.; Selathurai, A.; Tull, D.; O’Callaghan, S.; McConville, M.J.; Bruce, C.R. Application of dynamic metabolomics to examine in vivo skeletal muscle glucose metabolism in the chronically high-fat fed mouse. Biochem. Biophys. Res. Commun. 2015, 462, 27–32. [Google Scholar] [CrossRef]
- Lafontan, M.; Girard, J. Impact of visceral adipose tissue on liver metabolism. Part I: Heterogeneity of adipose tissue and functional properties of visceral adipose tissue. Diabetes Metab. 2008, 34, 317–327. [Google Scholar] [CrossRef]
- Perry, R.J.; Samuel, V.T.; Petersen, K.F.; Shulman, G.I. The role of hepatic lipids in hepatic insulin resistance and type 2 diabetes. Nature 2014, 510, 84–91. [Google Scholar] [CrossRef]
- Lavoie, F.; Frisch, F.; Brassard, P.; Normand-Lauziere, F.; Cyr, D.; Gagnon, R.; Drouin, R.; Baillargeon, J.P.; Carpentier, A.C. Relationship between total and high molecular weight adiponectin levels and plasma nonesterified fatty acid tolerance during enhanced intravascular triacylglycerol lipolysis in men. J. Clin. Endocrinol. Metab. 2009, 94, 998–1004. [Google Scholar] [CrossRef]
- Stern, J.H.; Rutkowski, J.M.; Scherer, P.E. Adiponectin, Leptin, and Fatty Acids in the Maintenance of Metabolic Homeostasis through Adipose Tissue Crosstalk. Cell Metab. 2016, 23, 770–784. [Google Scholar] [CrossRef]
- Wergedahl, H.; Liaset, B.; Gudbrandsen, O.A.; Lied, E.; Espe, M.; Muna, Z.; Mork, S.; Berge, R.K. Fish protein hydrolysate reduces plasma total cholesterol, increases the proportion of HDL cholesterol, and lowers acyl-CoA:cholesterol acyltransferase activity in liver of Zucker rats. J. Nutr. 2004, 134, 1320–1327. [Google Scholar] [CrossRef]
- Hosomi, R.; Fukunaga, K.; Arai, H.; Kanda, S.; Nishiyama, T.; Yoshida, M. Fish protein decreases serum cholesterol in rats by inhibition of cholesterol and bile acid absorption. J. Food Sci. 2011, 76, H116–H121. [Google Scholar] [CrossRef]
- Wang, Y.; Yi, X.; Ghanam, K.; Zhang, S.; Zhao, T.; Zhu, X. Berberine decreases cholesterol levels in rats through multiple mechanisms, including inhibition of cholesterol absorption. Metabolism 2014, 63, 1167–1177. [Google Scholar] [CrossRef]
- Folch, J.; Lees, M.; Sloane Stanley, G.H. A simple method for the isolation and purification of total lipides from animal tissues. J. Biol. Chem. 1957, 226, 497–509. [Google Scholar]
| Treatment | Time Post Treatment (Week) | ||||||
|---|---|---|---|---|---|---|---|
| 1 | 2 | 3 | 5 | 6 | 8 | 10 | |
| LFC | 3.1 ± 0.2 | 3.0 ± 0.2 | 3.5 ± 0.1 | 3.3 ± 0.1 | 3.8 ± 0.1 | 3.4 ± 0.2 | 3.2 ± 0.1 |
| HFC | 3.0 ± 0.1 | 3.0 ± 0.1 | 2.8 ± 0.1 # | 2.9 ± 0.1 # | 3.0 ± 0.1 # | 2.9 ± 0.1 # | 3.0 ± 0.1 |
| HPH15 | 2.7 ± 0.1 | 2.9 ± 0.1 | 2.7 ± 0.1 | 2.7 ± 0.1 | 2.9 ± 0.1 | 2.9 ± 0.1 | 3.0 ± 0.1 |
| HPH35 | 2.6 ± 0.1 | 2.9 ± 0.1 | 2.9 ± 0.1 | 2.9 ± 0.1 | 2.8 ± 0.1 | 2.9 ± 0.1 | 3.1 ± 0.1 |
| HPH70 | 2.4 ± 0.1 | 3.1 ± 0.1 | 3.0 ± 0.1 | 3.4 ± 0.2 | 3.3 ± 0.2 | 3.1 ± 0.1 | 3.8 ± 0.3 |
| Treatment | Time Post Treatment (Week) | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| 0 | 1 | 2 | 3 | 4 | 5 | 6 | 8 | 9 | 10 | |
| LFC | 34.2 ± 0.5 | 35.5 ± 0.5 | 35.7 ± 0.5 | 35.4 ± 0.5 | 36 ± 0.6 | 36.7 ± 0.6 | 36.7 ± 0.5 | 37.5 ± 0.7 | 38.2 ± 0.7 | 37 ± 0.5 |
| HFC | 42.3 ± 1.2 # | 43.6 ± 1.3 # | 44.8 ± 1.2 # | 46.5 ± 1.2 # | 47.3 ± 1.2 # | 47.6 ± 1.2 # | 48.1 ± 1.1 # | 49.5 ± 0.9 # | 49.8 ± 0.8 # | 49.4 ± 0.7 # |
| HPH15 | 43.8 ± 1.4 | 45.0 ± 1.3 | 45.7 ± 1.1 | 47.2 ± 1.0 | 47.8 ± 0.9 | 48.6 ± 0.8 | 49.1 ± 0.6 | 50.2 ± 0.5 | 50.5 ± 0.6 | 49.2 ± 1.2 |
| HPH35 | 43.0 ± 1.1 | 42.8 ± 1.0 | 43.3 ± 1.0 | 45.0 ± 0.9 | 45.7 ± 0.9 | 46.4 ± 0.9 | 45.6 ± 1.1 | 47.8 ± 0.9 | 48.1 ± 0.9 | 48.1 ± 0.8 |
| HPH70 | 43.1 ± 1.2 | 41.3 ± 1.2 | 40.1 ± 1.3 | 40.4 ± 1.3 a | 40.3 ± 1.3 b | 41.2 ± 1.4 b | 41.3 ± 1.4 b | 41.9 ± 1.5 b | 40.8 ± 1.5 b | 41.1 ± 1.6 b |
| LFC | HFC | HPH15 | HPH35 | HPH70 | |
|---|---|---|---|---|---|
| Fasting blood glucose (mmol/L) | 7.88 ± 0.42 | 10.57 ± 0.27 ξ | 9.51 ± 0.54 | 10.01 ± 0.35 | 8.37 ± 0.50 c |
| Serum insulin (ng/mL) | 0.45 ± 0.07 | 1.68 ± 0.20 ξ | 1.97 ± 0.38 | 1.21 ± 0.28 | 0.84 ± 0.18 b |
| Serum leptin (ng/mL) | 25.80 ± 2.44 | 60.77 ± 3.08 ξ | 56.97 ± 6.17 | 56.37 ± 2.88 | 36.70 ± 6.14 b |
| Serum adiponectin (ng/mL) | 10.66 ± 0.31 | 9.79 ± 0.26 # | 8.84 ± 0.36 | 9.95 ± 0.22 | 8.99 ± 0.40 |
| Total cholesterol (mg/dL) | 160.20 ± 5.95 | 232.51 ± 8.3 ξ | 263.24 ± 17.2 | 251.70 ± 9.2 | 202.82 ± 16.8 a |
| Triglycerides (mg/dL) | 60.70 ± 2.18 | 50.48 ± 2.85 ¥ | 58.24 ± 3.51 | 61.73 ± 2.18 | 58.04 ± 5.07 |
| FFA (mmol/mL) | 0.13 ± 0.01 | 0.10 ± 0.01 | 0.12 ± 0.01 | 0.11 ± 0.01 | 0.09 ± 0.01 |
| HOMA-IR | 5.53 ± 0.93 | 31.51 ± 3.41 ξ | 34.37 ± 6.08 | 18.75 ± 4.92 | 11.27 ± 2.61 b |
| HOMA-β | 0.30 ± 0.06 | 0.04 ± 0.00 ξ | 0.05 ± 0.00 | 0.09 ± 0.01a | 0.29 ± 0.04 c |
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Wang, Y.; Gagnon, J.; Nair, S.; Sha, S. Herring Milt Protein Hydrolysate Improves Insulin Resistance in High-Fat-Diet-Induced Obese Male C57BL/6J Mice. Mar. Drugs 2019, 17, 456. https://doi.org/10.3390/md17080456
Wang Y, Gagnon J, Nair S, Sha S. Herring Milt Protein Hydrolysate Improves Insulin Resistance in High-Fat-Diet-Induced Obese Male C57BL/6J Mice. Marine Drugs. 2019; 17(8):456. https://doi.org/10.3390/md17080456
Chicago/Turabian StyleWang, Yanwen, Jacques Gagnon, Sandhya Nair, and Shelly Sha. 2019. "Herring Milt Protein Hydrolysate Improves Insulin Resistance in High-Fat-Diet-Induced Obese Male C57BL/6J Mice" Marine Drugs 17, no. 8: 456. https://doi.org/10.3390/md17080456
APA StyleWang, Y., Gagnon, J., Nair, S., & Sha, S. (2019). Herring Milt Protein Hydrolysate Improves Insulin Resistance in High-Fat-Diet-Induced Obese Male C57BL/6J Mice. Marine Drugs, 17(8), 456. https://doi.org/10.3390/md17080456







