Impact of Periprocedural Risk Predictors on Long-Term Outcomes in Patients with Diabetes Undergoing Coronary Artery Bypass Grafting
Abstract
1. Introduction
2. Patients and Methods
2.1. Patients
2.2. Follow-Up
2.3. Group Analysis
2.4. Primary and Secondary Objectives and Definitions
2.5. Statistical Analysis
3. Results
3.1. Pre-Operative Characteristics
3.2. Intra-Operative Characteristics
3.3. Post-Operative Outcomes
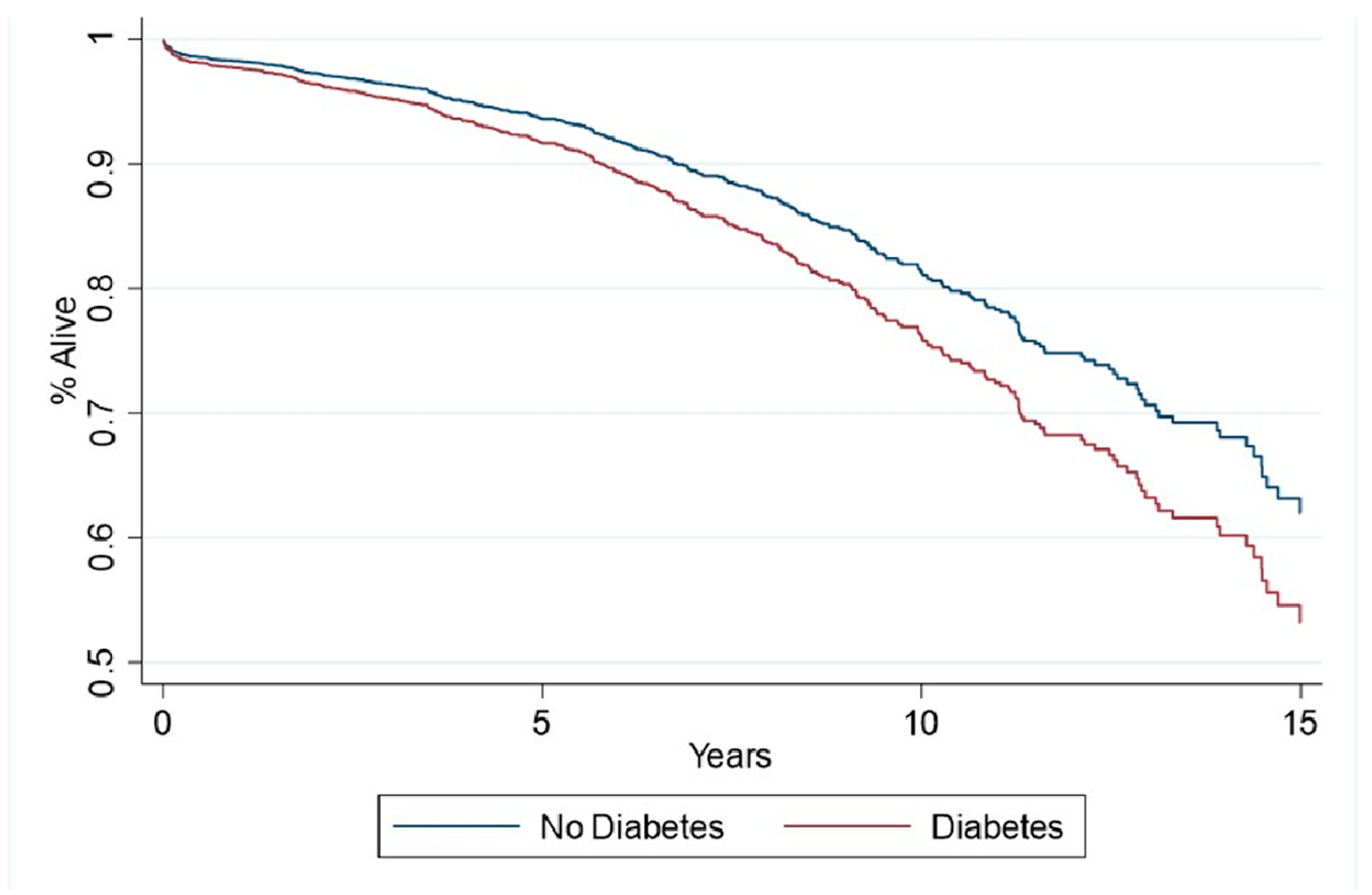
3.4. Follow-Up
3.5. Risk-Predictor Analysis
4. Discussion
- (I)
- Patients with diabetes are at a higher risk of death and occurrence of MACCE compared to those without diabetes following isolated CABG surgery (Table 4);
- (II)
- The presence of diabetes mellitus was an independent risk factor for late mortality and MACCE;
- (III)
- COPD, PVD, and serum creatinine levels > 2 mg/dL predicted all-cause mortality and MACCE in patients with and without diabetes mellitus.
4.1. All-Cause Death
4.2. Incidence of MACCE
4.3. Predictors for Late All-Cause Death and MACCE in Patients with Diabetes
4.4. Incidence of Nonfatal Stroke
4.5. Incidence of Myocardial Infarction
4.6. Incidence of Reoperation
4.7. Clinical Impact of Risk Predictors from Our Study
5. Limitations
6. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| CABG | coronary artery bypass grafting |
| CAD | coronary artery disease |
| CKD | chronic kidney disease |
| COPD | chronic obstructive pulmonary disease |
| PVD | peripheral vascular disease |
| OR | operating room |
| ICU | intensive care unit |
| BMI | body mass index |
| SVG | saphenous venous grafting |
| IMA | internal mammary artery |
| MI | myocardial infarction |
| CBVD | cerebrovascular disease |
| RBC | red blood cells |
| FFP | fresh frozen plasma |
| PCI | percutaneous coronary intervention |
| MACCE | major cardiovascular and cerebrovascular events |
References
- Kapur, A.; Malik, I.; Bagger, J.; Anderson, J.; Kooner, J.; Thomas, M.; Punjabi, P.; Mayet, J.; Millane, T.; Goedicke, J.; et al. The Coronary Artery Revascularisation in Diabetes (CARDia) trial: Background, aims, and design. Am. Heart J. 2005, 149, 13–19. [Google Scholar] [CrossRef]
- Serruys, P.W.; Morice, M.C.; Kappetein, A.P.; Colombo, A.; Holmes, D.R.; Mack, M.J.; Ståhle, E.; Feldman, T.E.; Van Den Brand, M.; Bass, E.J.; et al. Percutaneous coronary intervention versus coronary-artery bypass grafting for severe coronary artery disease. N. Engl. J. Med. 2009, 360, 961–972. [Google Scholar] [CrossRef]
- Farkouh, M.E.; Domanski, M.; Dangas, G.D.; Godoy, L.C.; Mack, M.J.; Siami, F.S.; Hamza, T.H.; Shah, B.; Stefanini, G.G.; Sidhu, M.S.; et al. Long-Term Survival Following Multivessel Revascularization in Patients With Diabetes: The FREEDOM Follow-On Study. J. Am. Coll. Cardiol. 2019, 73, 629–638. [Google Scholar] [CrossRef]
- Bartnes, K.; Hermansen, S.E.; Dahl-Eriksen, Ø.; Iqbal, A.; Mannsverk, J.T.; Steigen, T.K.; Trovik, T.; Busund, R.; Dahl, P.E.; Sørlie, D.G.; et al. Radial artery graft patency relates to gender, diabetes mellitus and angiotensin inhibition. Scand. Cardiovasc. J. 2010, 44, 230–236. [Google Scholar] [CrossRef] [PubMed]
- Cosgrove, D.M.; Loop, F.D.; Lytle, B.W.; Gill, C.C.; Golding, L.A.; Gibson, C.; Stewart, R.W.; Taylor, P.C.; Goormastic, M. Determinants of 10-year survival after primary myocardial revascularization. Ann. Surg. 1985, 202, 480–490. [Google Scholar] [CrossRef]
- Adler, D.S.; Goldman, L.; O’Neil, A.; Cook, E.F.; Mudge, G.H., Jr.; Shemin, R.J.; DiSesa, V.; Cohn, L.H.; Collins, J.J., Jr. Long-term survival of more than 2,000 patients after coronary artery bypass grafting. Am. J. Cardiol. 1986, 58, 195–202. [Google Scholar] [CrossRef] [PubMed]
- Lawrie, G.M.; Morris, G.C., Jr.; Glaeser, D.H. Influence of diabetes mellitus on the results of coronary bypass surgery. Follow-up of 212 diabetic patients ten to 15 years after surgery. JAMA 1986, 256, 2967–2971. [Google Scholar] [CrossRef] [PubMed]
- Morris, J.J.; Smith, L.R.; Jones, R.H.; Glower, D.D.; Morris, P.B.; Muhlbaier, L.H.; Reves, J.G.; Rankin, J.S. Influence of diabetes and mammary artery grafting on survival after coronary bypass. Circulation 1991, 84, III275-84. [Google Scholar]
- Morricone, L.; Ranucci, M.; Denti, S.; Cazzaniga, A.; Isgrò, G.; Enrini, R.; Caviezel, F. Diabetes and complications after cardiac surgery: Comparison with a non-diabetic population. Acta Diabetol. 1999, 36, 77–84. [Google Scholar] [CrossRef]
- Stone, N.J.; Robinson, J.G.; Lichtenstein, A.H.; Bairey Merz, C.N.; Blum, C.B.; Eckel, R.H.; Goldberg, A.C.; Gordon, D.; Levy, D.; Lloyd-Jones, D.M.; et al. American College of Cardiology/American Heart Association Task Force on Practice Guidelines. 2013 ACC/AHA guideline on the treatment of blood cholesterol to reduce atherosclerotic cardiovascular risk in adults: A report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. J. Am. Coll. Cardiol. 2014, 63, 2889–2934. [Google Scholar]
- BARI Investigators. The final 10-year follow-up results from the BARI randomized trial. J. Am. Coll. Cardiol. 2007, 49, 1600–1606. [CrossRef] [PubMed]
- Wang, R.; Serruys, P.W.; Gao, C.; Hara, H.; Takahashi, K.; Ono, M.; Kawashima, H.; O’lEary, N.; Holmes, D.R.; Witkowski, A.; et al. Ten-year all-cause death after percutaneous or surgical revascularization in diabetic patients with complex coronary artery disease. Eur. Heart J. 2021, 43, 56–67. [Google Scholar] [CrossRef] [PubMed]
- Yamaji, K.; Shiomi, H.; Morimoto, T.; Matsumura-Nakano, Y.; Ehara, N.; Sakamoto, H.; Takeji, Y.; Yoshikawa, Y.; Yamamoto, K.; Kato, E.T.; et al. Modifiers of the Risk of Diabetes for Long-Term Outcomes After Coronary Revascularization: CREDO-Kyoto PCI/CABG Registry. JACC Asia 2022, 2, 294–308. [Google Scholar] [CrossRef] [PubMed]
- Tam, D.Y.; Dharma, C.; Rocha, R.; Farkouh, M.E.; Abdel-Qadir, H.; Sun, L.Y.; Wijeysundera, H.C.; Austin, P.C.; Udell, J.A.; Gaudino, M.; et al. Long-Term Survival After Surgical or Percutaneous Revascularization in Patients With Diabetes and Multivessel Coronary Disease. J. Am. Coll. Cardiol. 2020, 76, 1153–1164. [Google Scholar] [CrossRef]
- Farkouh, M.E.; Domanski, M.; Sleeper, L.A.; Siami, F.S.; Dangas, G.; Mack, M.; Yang, M.; Cohen, D.J.; Rosenberg, Y.; Solomon, S.D.; et al. Strategies for multivessel revascularization in patients with diabetes. N. Engl. J. Med. 2012, 367, 2375–2384. [Google Scholar] [CrossRef]
- Júnior, F.P.; Pereira, E.M.C.; Valle, F.H.; Filho, G.F.T.; Nesralla, I.A.; Sant’Anna, J.R.M.; Prates, P.R.; Kalil, R.A.K. Does diabetes mellitus increase immediate surgical risk in octogenarian patients submitted to coronary artery bypass graft surgery? Rev. Bras. Cir. Cardiovasc. 2012, 27, 600–606. [Google Scholar] [CrossRef]
- Van Straten, A.H.; Soliman Hamad, M.A.; van Zundert, A.A.; Martens, E.J.; Schönberger, J.P.; ter Woorst, J.F.; de Wolf, A.M. Diabetes and survival after coronary artery bypass grafting: Comparison with an age- and sex-matched population. Eur. J. Cardiothorac. Surg. 2010, 37, 1068–1074. [Google Scholar] [CrossRef]
- Barsness, G.W.; Peterson, E.D.; Ohman, E.M.; Nelson, C.L.; DeLong, E.R.; Reves, J.G.; Smith, P.K.; Anderson, R.D.; Jones, R.H.; Mark, D.B.; et al. Relationship between diabetes mellitus and long-term survival after coronary bypass and angioplasty. Circulation 1997, 96, 2551–2556. [Google Scholar] [CrossRef]
- Zhao, H.; Li, L.; Yang, G.; Gong, J.; Ye, L.; Zhi, S.; Zhang, X.; Li, J. Postoperative outcomes of patients with chronic obstructive pulmonary disease undergoing coronary artery bypass grafting surgery: A meta-analysis. Medicine 2019, 98, e14388. [Google Scholar] [CrossRef]
- Banning, A.P.; Serruys, P.; De Maria, G.L.; Ryan, N.; Walsh, S.; Gonzalo, N.; Jan van Geuns, R.; Onuma, Y.; Sabate, M.; Davies, J.; et al. Five-year outcomes after state-of-the-art percutaneous coronary revascularization in patients with de novo three-vessel disease: Final results of the SYNTAX II study. Eur. Heart J. 2022, 43, 1307–1316. [Google Scholar] [CrossRef]
- Thourani, V.H.; Weintraub, W.S.; Stein, B.; Gebhart, S.S.; Craver, J.M.; Jones, E.L.; Guyton, R.A. Influence of diabetes mellitus on early and late outcome after coronary artery bypass grafting. Ann. Thorac. Surg. 1999, 67, 1045–1052. [Google Scholar] [CrossRef]
- Dahl-Jorgensen, K.; Larsen, J.R.; Hanssen, K.F. Atherosclerosis in childhood and adolescent type 1 diabetes: Early disease, early treatment? Diabetologia 2005, 48, 1445–1453. [Google Scholar] [CrossRef]
- Dokollari, A.; Sicouri, S.; Hosseinian, L.; Erten, O.; Ramlawi, B.; Bisleri, G.; Bonacchi, M.; Sicouri, N.; Torregrossa, G.; Sutter, F.P. Periprocedural Risk Predictors Affecting Long-Term Prognosis in Patients With Chronic Obstructive Pulmonary Disease Undergoing Coronary Artery Bypass Grafting. Tex. Heart Inst. J. 2024, 51, e238199. [Google Scholar] [CrossRef]
- Leavitt, B.J.; Sheppard, L.; Maloney, C.; Clough, R.A.; Braxton, J.H.; Charlesworth, D.C.; Weintraub, R.M.; Hernandez, F.; Olmstead, E.M.; Nugent, W.C.; et al. Effect of diabetes and associated conditions on long-term survival after coronary artery bypass graft surgery. Circulation 2004, 110, II41-4. [Google Scholar] [CrossRef]
- Bonaca, M.P.; Catarig, A.M.; Houlind, K.; Ludvik, B.; Nordanstig, J.; Ramesh, C.K.; Rasouli, N.; Sourij, H.; Videmark, A.; Verma, S. Semaglutide and walking capacity in people with symptomatic peripheral artery disease and type 2 diabetes (STRIDE): A phase 3b, double-blind, randomised, placebo-controlled trial. Lancet 2025, 405, 1580–1593. [Google Scholar] [CrossRef]
- Dokollari, A.; Sicouri, S.; Yamashita, Y.; Arora, R.; Ghorpade, N.; Kjelstrom, S.; Montone, G.; Cabrucci, F.; Bacchi, B.; Chiarello, B.; et al. Periprocedural Risk Predictors in Patients with Chronic Kidney Disease Undergoing Coronary Artery Bypass Grafting. J. Community Med. Public Health 2023, 4, 2692–9899. [Google Scholar]
- Farkouh, M.E.; Sidhu, M.S.; Brooks, M.M.; Vlachos, H.; Boden, W.E.; Frye, R.L.; Hartigan, P.; Siami, F.; Bittner, V.A.; Chaitman, B.R.; et al. Impact of Chronic Kidney Disease on Outcomes of Myocardial Revascularization in Patients With Diabetes. J. Am. Coll. Cardiol. 2019, 73, 400–411. [Google Scholar] [CrossRef]
| Unmatched Patients | Matched Patients | |||||
|---|---|---|---|---|---|---|
| No Diabetes n = 2852 | Diabetes n = 2019 | p-Value | No Diabetes n =1589 | Diabetes n =1589 | p-Value | |
| Age Years (mean/SD) | 71.4 (11.2) | 70.5 (10.8) | 0.006 | 71.22 (11.1) | 71.43 (10.6) | 0.5 |
| Gender | <0.0001 | 0.7 | ||||
| Female n (%) | 602 (21.1%) | 575 (28.5%) | 404 (25.4%) | 396 (24.9%) | ||
| Male n (%) | 2250 (78.9%) | 1444 (71.5%) | 1185 (75.1%) | 1193 (75.0%) | ||
| Race | <0.0001 | 0.8 | ||||
| White n (%) | 2563 (89.9%) | 1742 (86.3%) | 1390 (87.5%) | 1399 (88.0%) | ||
| Black or African American n (%) | 239 (8.4%) | 222 (11.0%) | 162 (10.2%) | 156 (9.8%) | ||
| Other n (%) | 50 (1.8%) | 55 (2.7%) | 37 (2.3%) | 34 (2.1%) | ||
| STS Risk of Mortality % (median/IQR) | 0.84 (0.47–1.8) | 1.2 (0.64–2.6) | <0.0001 | 0.98 (0.51–2.1) | 1.1 (0.59–2.37) | 0.02 |
| BMI kg/m2 (Mean/SD) | 28.1 (4.9) | 30.9 (11.6) | <0.0001 | 29.4 (5.35) | 29.2 (5.01) | 0.1 |
| Obese n (%) | 850 (29.8%) | 1008 (49.9%) | <0.0001 | 652 (41.0%) | 633 (39.8%) | 0.4 |
| Creatine Level (Median/IQR) | 1 (0.9–1.2) | 1 (0.9–1.3) | <0.0001 | 1 (0.9–1.2) | 1 (0.9–1.3) | 0.08 |
| Creatinine level < 1.2 mg/dL | 2083 (73.0%) | 1282 (63.5%) | 116 (70.2%) | 1056 (66.5%) | ||
| Creatinine level 1.2 to 1.5 mg/dL | 588 (20.6%) | 432 (21.4%) | 343 (21.6%) | 350 (22.0%) | ||
| Creatinine level > 1.5 to 2.0 mg/dL | 97 (3.4%) | 155 (7.7%) | 58 (3.7%) | 110 (6.9%) | ||
| Creatinine level > 2.0 or on dialysis | 84 (3.0%) | 150 (7.4%) | 72 (4.5%) | 73 (4.6%) | ||
| Dialysis n (%) | 39 (1.4%) | 80 (4.0%) | <0.0001 | 36 (2.3%) | 28 (1.8%) | 0.2 |
| Smoking n (%) | 1303 (45.7%) | 964 (47.7%) | 0.1 | 757 (47.6%) | 762 (47.9%) | 0.8 |
| COPD n (%) | 398 (14.0%) | 369 (18.3%) | <0.0001 | 259 (16.3%) | 254 (16.0%) | 0.8 |
| Hypertension n (%) | 2321 (81.4%) | 1884 (93.3%) | <0.0001 | 1461 (91.9%) | 1455 (91.6%) | 0.6 |
| Dyslipidemia n (%) | 2462 (86.3%) | 1769 (87.6%) | 0.1 | 1375 (86.5%) | 1380 (86.8%) | 0.7 |
| CBVD n (%) | 443 (15.5%) | 455 (22.5%) | <0.0001 | 307 (19.3%) | 315 (19.8%) | 0.7 |
| PVD n (%) | 327 (11.5%) | 395 (19.6%) | <0.0001 | 251 (15.8%) | 251 (15.8%) | 1 |
| Liver disease n (%) | 35 (1.2%) | 27 (1.3%) | 0.7 | 25 (1.6%) | 19 (1.2%) | 0.3 |
| Prior Mediastinal Radiation n (%) | 23 (0.8%) | 22 (1.1%) | 0.3 | 17 (1.1%) | 16 (1.0%) | 0.8 |
| Previous PCI n (%) | 997 (35.0%) | 821 (40.7%) | <0.0001 | 612 (38.5%) | 629 (39.6%) | 0.5 |
| Prior CABG n (%) | 65 (2.3%) | 47 (2.3%) | 0.9 | 36 (2.3%) | 41 (2.6%) | 0.5 |
| Prior MI n (%) | 1539 (54.0%) | 1185 (58.7%) | 0.001 | 891 (56.1%) | 894 (56.3%) | 0.9 |
| Prior Valve Surgery n (%) | 16 (0.6%) | 14 (0.7%) | 0.5 | 11 (0.7%) | 13 (0.8%) | 0.6 |
| Atrial Fibrillation n (%) | 344 (12.1%) | 249 (12.3%) | 0.7 | 210 (13.2%) | 202 (12.7%) | 0.6 |
| Pre-operative EF (mean/SD) n (%) | 53.4 (12.7) | 51.1 (14.1) | <0.0001 | 52.4 (13.3) | 52.5 (13.5) | 0.8 |
| EF n (%) | <0.0001 | 0.233 | ||||
| EF < 25% | 99 (3.5%) | 108 (5.4%) | 70 (4.4%) | 61 (3.8%) | ||
| EF 25–50% | 1029 (36.1%) | 786 (38.9%) | 608 (38.3%) | 571 (35.9%) | ||
| EF > 50% | 1724 (60.4%) | 1125 (55.7%) | 911 (57.3%) | 957 (60.2%) | ||
| Diseased Vessels | <0.0001 | 0.7 | ||||
| 1 n (%) | 322 (11.3%) | 137 (6.8%) | 132 (8.3%) | 124 (7.8%) | ||
| 2 n (%) | 770 (27.0%) | 455 (22.5%) | 400 (25.2%) | 399 (25.1%) | ||
| 3 n (%) | 1666 (58.4%) | 1340 (66.4%) | 990 (62.3%) | 1009 (63.5%) | ||
| 4 n (%) | 94 (3.3%) | 87 (4.3%) | 67 (4.2%) | 57 (3.6%) | ||
| Left Main Coronary Artery Stenosis > 50% n (%) | 744 (26.1%) | 487 (24.1%) | 0.1 | 392 (24.7%) | 402 (25.3%) | 0.6 |
| Severe Proximal LAD Lesion > 70% n (%) | 2373 (83.2%) | 1714 (84.9%) | 0.1 | 1336 (84.1%) | 1333 (83.9%) | 0.8 |
| Insulin n (%) | 0 | 1825 (90.4%) | <0.0001 | 0 | 1482 (93.2%) | <0.0001 |
| Metformin n (%) | 0 | 1025 (50.7%) | <0.0001 | 0 | 892 (56.1%) | <0.0001 |
| B-blockers n (%) | 2125 (74.3%) | 1926 (95.3%) | <0.0001 | 1482 (93.2%) | 1476 (92.8%) | 0.5 |
| ACE-ARB inhibitors n (%) | 1254 (43.9%) | 1845 (91.3%) | <0.0001 | 956 (60.1%) | 1543 (97.1%) | <0.0001 |
| Unmatched | Matched | |||||
|---|---|---|---|---|---|---|
| No Diabetes n = 2852 | Diabetes n = 2019 | p-Value | No Diabetes n =1589 | Diabetes n =1589 | p-Value | |
| IMA use | <0.0001 | 0.7 | ||||
| Single IMA n (%) | 2343 (82.2%) | 1890 (93.6%) | 1447 (92.9%) | 1467 (92.3%) | ||
| IMA + RIMA n (%) | 457 (16.0%) | 90 (4.5%) | 81 (5.1%) | 89 (5.6%) | ||
| None n (%) | 52 (1.8%) | 39 (1.9%) | 31 (1.9%) | 33 (2.1%) | ||
| Radial Artery Graft, n (%) | 547 (19.2%) | 346 (17.1%) | 0.07 | 270 (17.0%) | 278 (17.5%) | 0.7 |
| SVG, n (%) | 1340 (50.0%) | 1107 (54.8%) | <0.0001 | 797 (49.8%) | 842 (53%) | 0.1 |
| Number of Grafts (median/IQR) | 2 (1–3) | 2 (1–3) | 0.05 | 2 (1–3) | 2 (1–3) | 0.05 |
| Number of Grafts | 0.2 | 0.2 | ||||
| 1 | 1227 (43.0%) | 811 (40.2%) | 712 (44.8%) | 665 (41.8%) | ||
| 2 | 479 (16.8%) | 349 (17.3%) | 260 (16.4%) | 260 (16.4%) | ||
| 3 | 676 (23.7%) | 512 (25.4%) | 375 (23.6%) | 398 (25.0%) | ||
| 4 | 359 (12.6%) | 256 (12.7%) | 192 (12.1%) | 195 (12.3%) | ||
| 5+ | 111 (3.9%) | 91 (4.5%) | 50 (3.1%) | 71 (4.5%) | ||
| Total Arterial CABG n (%) | 792 (27.8%) | 386 (19.1%) | <0.0001 | 307 (19.3%) | 319 (20.1%) | 0.5 |
| Multiple Arterial CABG n (%) | 844 (29.6%) | 433 (21.5%) | <0.0001 | 368 (23.2%) | 376 (23.7%) | 0.7 |
| On Pump CABG n (%) | 358 (12.5%) | 333 (16.5%) | <0.0001 | 236 (14.8%) | 254 (16.0%) | 0.3 |
| Priority of Surgery (%) | 0.02 | 0.3 | ||||
| Elective | 1574 (55.2%) | 1037 (51.4%) | 860 (54.1%) | 827 (52.0%) | ||
| Urgent | 1251 (43.9%) | 966 (47.9%) | 712 (44.8%) | 748 (47.1%) | ||
| Emergent | 27 (1.0%) | 16 (0.8%) | 17 (1.1%) | 14 (0.9%) | ||
| Time in OR (Hours) (Median/IQR) | 5.8 (5.1–6.7) | 5.8 (5.2–6.7) | 0.1 | 5.8 (5.1–6.7) | 5.7 (5.1–6.7) | 0.2 |
| All types of blood product transfusions n (%) | 452 (15.9%) | 446 (22.1%) | <0.0001 | 287 (18.1%) | 338 (21.3%) | 0.02 |
| RBC Units n (%) | 368 (12.9%) | 404 (20.0%) | <0.0001 | 238 (15.0%) | 299 (18.8%) | 0.004 |
| Cryoprecipitate Units n (%) | 103 (3.6%) | 84 (4.2%) | 0.3 | 66 (4.1%) | 65 (4.1%) | 0.9 |
| Platelet Units n (%) | 182 (6.4%) | 159 (7.9%) | 0.04 | 117 (7.4%) | 121 (7.6%) | 0.7 |
| FFP Units n (%) | 47 (1.7%) | 60 (3.0%) | 0.002 | 26 (1.6%) | 44 (2.8%) | 0.02 |
| Extubated in OR n (%) | 2290 (80.3%) | 1465 (72.6%) | <0.0001 | 1217 (76.6%) | 1200 (75.5%) | 0.4 |
| Unmatched Patients | Matched Patients | |||||
|---|---|---|---|---|---|---|
| No Diabetes n = 2852 | Diabetes n = 2019 | p-Value | No Diabetes n =1589 | Diabetes n =1589 | p-Value | |
| Total ICU (Hours) (Median/IQR) | 43.6 (24.7–71.8) | 47.0 (25.5–87.6) | <0.0001 | 44.7 (25.1–72.3) | 45.6 (25.0–75.6) | 0.08 |
| Total LOS (Days) (Median/IQR) | 5 (4–6) | 5 (4–7) | <0.0001 | 5 (4–7) | 5 (4–7) | 0.0005 |
| All types of Blood Products Transfusion n (%) | 851 (29.8%) | 689 (34.1%) | 0.002 | 503 (31.7%) | 515 (32.4%) | 0.6 |
| RBC Units n (%) | 826 (29.0%) | 673 (33.3%) | 0.001 | 485 (30.5%) | 501 (31.5%) | 0.5 |
| Cryoprecipitate Units n (%) | 139 (4.9%) | 61 (3.0%) | 0.001 | 76 (4.8%) | 50 (3.15%) | 0.01 |
| Platelet Units n (%) | 188 (6.6%) | 88 (4.4%) | 0.001 | 101 (6.4%) | 66 (4.1%) | 0.004 |
| FFP Units n (%) | 107 (3.8%) | 69 (3.4%) | 0.5 | 65 (4.1%) | 56 (3.5%) | 0.4 |
| Stroke n (%) | 6 (0.2%) | 22 (1.1%) | <0.0001 | 5 (0.3%) | 17 (1.1%) | 0.01 |
| Superficial Sternal Wound Infection n (%) | 4 (0.1%) | 13 (0.6%) | 0.003 | 2 (0.1%) | 9 (0.6%) | 0.03 |
| Deep Sternal Infection n (%) | 5 (0.2%) | 11 (0.5%) | 0.02 | 5 (0.3%) | 4 (0.2%) | 0.7 |
| Reoperation for Bleeding n (%) | 34 (1.2%) | 13 (0.6%) | 0.05 | 18 (1.1%) | 11 (0.7) | 0.1 |
| Prolonged Ventilation > 24 h n (%) | 87 (3.1%) | 116 (5.8%) | <0.0001 | 63 (4.0%) | 80 (5.0%) | 0.1 |
| Renal Failure n (%) | 39 (1.4%) | 53 (2.6%) | 0.001 | 24 (1.5%) | 30 (1.9%) | 0.4 |
| New Dialysis n (%) | 9 (0.3%) | 16 (0.8%) | 0.02 | 6 (0.4%) | 9 (0.6%) | 0.4 |
| New Atrial Fibrillation n (%) | 628 (22.0%) | 468 (23.2%) | 0.3 | 365 (23%) | 376 (24%) | 0.6 |
| 30 Day Readmission n (%) | 210 (7.4%) | 181 (9.0%) | 0.04 | 117 (7.4%) | 136 (8.6%) | 0.2 |
| 30-day mortality n (%) | 22 (0.8%) | 28 (1.4%) | 0.036 | 17 (1.1%) | 17 (1.1%) | 1 |
| Unmatched Patients | Matched Patients | |||||
|---|---|---|---|---|---|---|
| No Diabetes n = 2852 | Diabetes n = 2019 | p-Value | No Diabetes n =1589 | Diabetes n =1589 | p-Value | |
| All-cause Mortality n (%) | 267 (9.4%) | 296 (14.7%) | <0.0001 | 169 (10.6%) | 215 (13.5%) | 0.013 |
| MACCE n (%) | 356 (12.5%) | 363 (18.0%) | <0.0001 | 228 (14.4%) | 264 (16.6%) | 0.04 |
| Non-Fatal Stroke n (%) | 55 (1.9%) | 42 (2.1%) | 0.7 | 35 (2.2%) | 34 (2.1%) | 0.9 |
| Non-Fatal MI n (%) | 62 (2.2%) | 57 (2.8%) | 0.1 | 44 (2.8%) | 37 (2.3%) | 0.4 |
| Reoperation n (%) | 322 (11.3%) | 246 (12.2%) | 0.3 | 182 (11.5%) | 189 (11.9%) | 0.6 |
| Angina n (%) | 303 (10.6%) | 231 (11.4%) | 0.3 | 165 (10.4%) | 182 (11.5%) | 0.3 |
| All-Cause Death | All Patients HR (95% CI) | Diabetes HR (95% CI) | No Diabetes HR (95% CI) |
|---|---|---|---|
| Diabetes | 1.4 (1.2, 1.7) | ||
| Age > 75 years | 1.02 (1.01, 1.03) | 1.04 (1.01, 1.05) | |
| STS-PROM risk score > 4% | 1.04 (1.02, 1.06) | 1.06 (1.03, 1.08) | 1.03 (1.01, 1.1) |
| Creatinine level | |||
| 1.2 to 1.5 mg/dL | 1.3 (1.1, 1.6) | 1.4 (1.1, 1.9) | |
| 1.5 to 2.0 mg/dL | 1.8 (1.3, 2.5) | 2.1 (1.4, 3.2) | |
| >2.0 mg/dL or on dialysis | 3.3 (2.5, 4.4) | 3.1 (2.1, 4.5) | 3.7 (2.4, 6.0) |
| Prior Valve Surgery | 3.3 (1.2, 9.3) | ||
| Prior MI | 1.3 (1.05, 1.5) | 1.6 (1.2, 2.1) | |
| PVD | 1.4 (1.2, 1.7) | 1.4 (1.04, 1.8) | 1.6 (1.2, 2.2) |
| Atrial Fibrillation | 1.5 (1.1, 2.1) | ||
| CBVD | 1.2 (1.01, 1.5) | ||
| COPD | 1.4 (1.2, 1.7) | 1.4 (1.04, 1.8) | 1.7 (1.3, 2.2) |
| BMI > 30 kg/m2 | 0.96 (0.93, 0.99) | ||
| Previous PCI | |||
| Preoperative EF | 0.98 (0.98, 0.99) | 0.98 (0.97, 0.99) | |
| MACCE | HR (95% CI) | HR (95% CI) | HR (95% CI) |
| Diabetes | 1.2 (1.03, 1.3) | ||
| Age > 75 years | 0.99 (0.98, 0.99) | 0.98 (0.98, 0.99) | |
| STS-PROM risk score > 4% | 1.06 (1.04, 1.07) | 1.04 (1.02, 1.07) | 1.06 (1.05, 1.08) |
| Creatinine level mg/dL | |||
| 1.5 to 2.0 mg/dL | 1.5 (1.1, 1.9) | 1.7 (1.3, 2.4) | |
| >2.0 mg/dL or on dialysis | 2.1 (1.6, 2.6) | 2.1 (1.5, 2.9) | 2.1 (1.5, 3.0) |
| PVD | 1.2 (1.02, 1.4) | 1.3 (1.03, 1.6) | |
| COPD | 1.2 (1.1, 1.4) | 1.3 (1.01, 1.6) | |
| CBVD | 1.3 (1.1, 1.5) | 1.3 (1.04, 1.6) | 1.3 (1.04, 1.6) |
| Prior Valve Surgery | 2.7 (1.2, 6.3) | ||
| BMI > 30 kg/m2 | 1.0 (1.0, 1.01) | 1.06 (1.03, 1.1) | |
| Four Diseased Vessels (Ref = 1) | 1.5 (1.04, 2.3) | ||
| Prior Mediastinal Radiation | 2.2 (1.3, 3.9) | 2.6 (1.3, 5.3) | |
| Black Race (Ref = White) | 1.5 (1.1, 1.9) | ||
| Previous PCI | 1.4 (1.2, 1.6) | 1.3 (1.1, 1.6) | 1.4 (1.2, 1.7) |
| STROKE | HR (95% CI) | HR (95% CI) | HR (95% CI) |
| Diabetes | 0.99 (0.7, 1.5) | ||
| Prior MI | 1.7 (1.1, 2.7) | ||
| Black Race (Ref = White) | 1.9 (1.1, 3.4) | 3.2 (1.6, 6.7) | |
| CBVD | 2.2 (1.4, 3.5) | 2.7 (1.4, 5.0) | 2.0 (1.04, 3.9) |
| Four Diseased Vessels (Ref = 1) | 6.1 (1.5, 25.2) | ||
| Preoperative EF | 1.02 (1.01, 1.04) | 1.03 (1.01, 1.06) | |
| MI | HR (95% CI) | HR (95% CI) | HR (95% CI) |
| Diabetes | 1.03 (0.7, 1.5) | ||
| Age > 75 years | 0.98 (0.97, 0.99) | ||
| BMI > 30 kg/m2 | 1.01 (1.01, 1.01) | 1.01 (1.01, 1.01) | 1.08 (1.03, 1.14) |
| Previous PCI | 2.0 (1.4, 2.9) | 2.0 (1.2, 3.4) | 2.1 (1.3, 3.5) |
| Black Race (Ref = White) | 1.8 (1.1, 2.9) | 2.0 (1.02, 3.9) | |
| Hypertension | 2.1 (1.1, 4.2) | ||
| CVBD | 1.7 (1.1, 2.6) | ||
| Three Diseased Vessels (Ref = 1) | 2.8 (1.03, 7.8) | ||
| STS-PROM risk score > 4% | 1.03 (1.01, 1.08) | ||
| Left Main Coronary Artery Stenosis > 50% | 1.8 (1.1, 2.9) | ||
| REOPERATION | HR (95% CI) | HR (95% CI) | HR (95% CI) |
| Diabetes | 1.1 (0.9, 1.3) | ||
| BMI > 30 kg/m2 | 1.0 (1.0, 1.01) | 1.01 (1.0, 1.01) | 1.03 (1.01, 1.06) |
| Age > 75 years | 0.98 (0.98, 0.99) | 0.98 (0.97, 0.99) | 0.98 (0.98, 0.99) |
| Female (Ref = Male) | 1.3 (1.1, 1.6) | 1.3 (1.01, 1.7) | |
| Previous PCI | 1.5 (1.3, 1.8) | 1.6 (1.2, 2.0) | 1.4 (1.1, 1.8) |
| Left Main Stenosis >50% | 1.2 (1.02, 1.5) | 1.4 (1.1, 1.8) | |
| Prior Mediastinal Radiation | 3.1 (1.3, 7.0) | ||
| Preoperative EF | 1.01 (1.0, 1.02) | 1.02 (1.01, 1.03) | 1.01 (1.01, 1.02) |
| Black Race (Ref: White) | 1.6 (1.1, 2.2) | ||
| Severe Proximal LAD Lesion > 70% | 1.6 (1.1, 2.4) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Published by MDPI on behalf of the Lithuanian University of Health Sciences. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license.
Share and Cite
Dokollari, A.; Sicouri, S.; Ramlawi, B.; Wertan, M.; Sutter, F.P. Impact of Periprocedural Risk Predictors on Long-Term Outcomes in Patients with Diabetes Undergoing Coronary Artery Bypass Grafting. Medicina 2026, 62, 71. https://doi.org/10.3390/medicina62010071
Dokollari A, Sicouri S, Ramlawi B, Wertan M, Sutter FP. Impact of Periprocedural Risk Predictors on Long-Term Outcomes in Patients with Diabetes Undergoing Coronary Artery Bypass Grafting. Medicina. 2026; 62(1):71. https://doi.org/10.3390/medicina62010071
Chicago/Turabian StyleDokollari, Aleksander, Serge Sicouri, Basel Ramlawi, MaryAnn Wertan, and Francis P. Sutter. 2026. "Impact of Periprocedural Risk Predictors on Long-Term Outcomes in Patients with Diabetes Undergoing Coronary Artery Bypass Grafting" Medicina 62, no. 1: 71. https://doi.org/10.3390/medicina62010071
APA StyleDokollari, A., Sicouri, S., Ramlawi, B., Wertan, M., & Sutter, F. P. (2026). Impact of Periprocedural Risk Predictors on Long-Term Outcomes in Patients with Diabetes Undergoing Coronary Artery Bypass Grafting. Medicina, 62(1), 71. https://doi.org/10.3390/medicina62010071








