Nationwide Epidemiology of Hospitalized Acute ACL Ruptures in Romania: A 7-Year Analysis (2017–2023)
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design and Data Sources
2.2. Data Extraction and Processing
2.3. Population Data and Incidence Calculation
2.4. Statistical Analysis
3. Results
3.1. General Overview of ACL Rupture Hospitalizations (2017–2023)
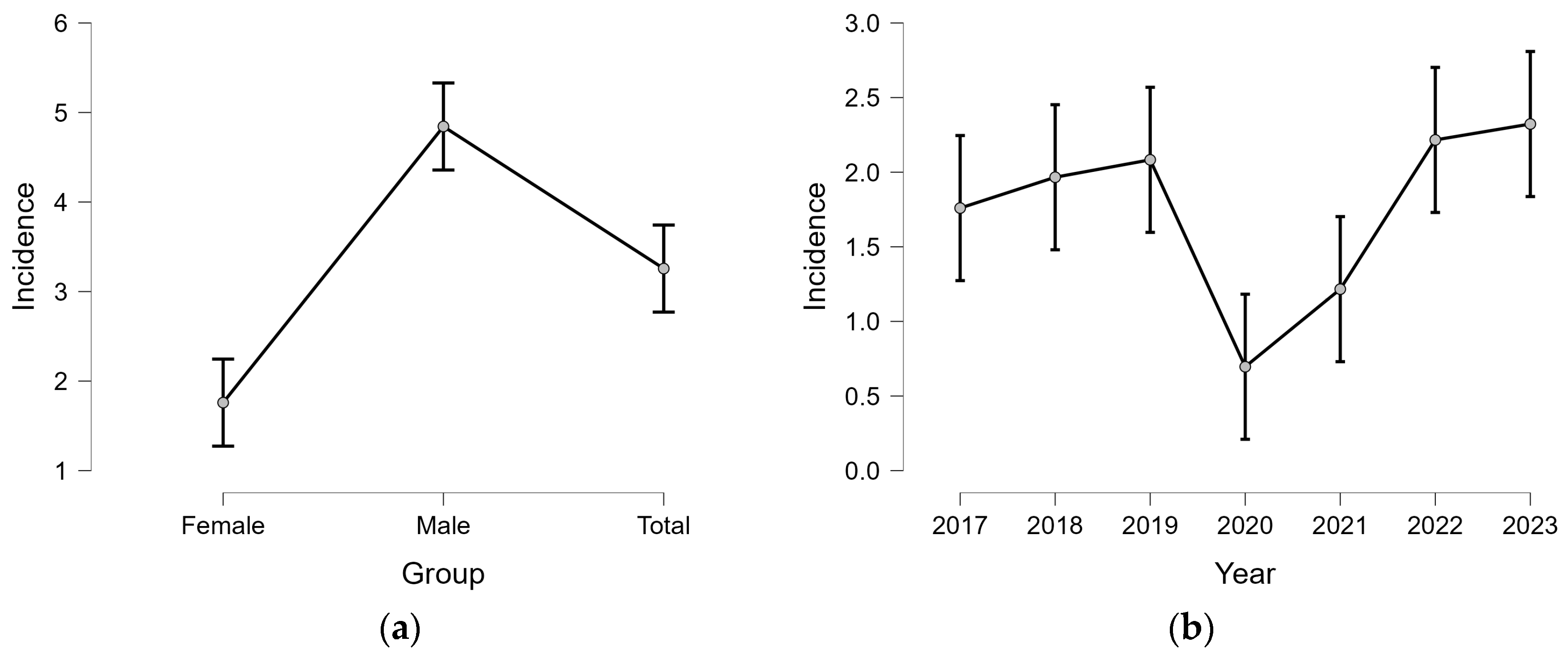
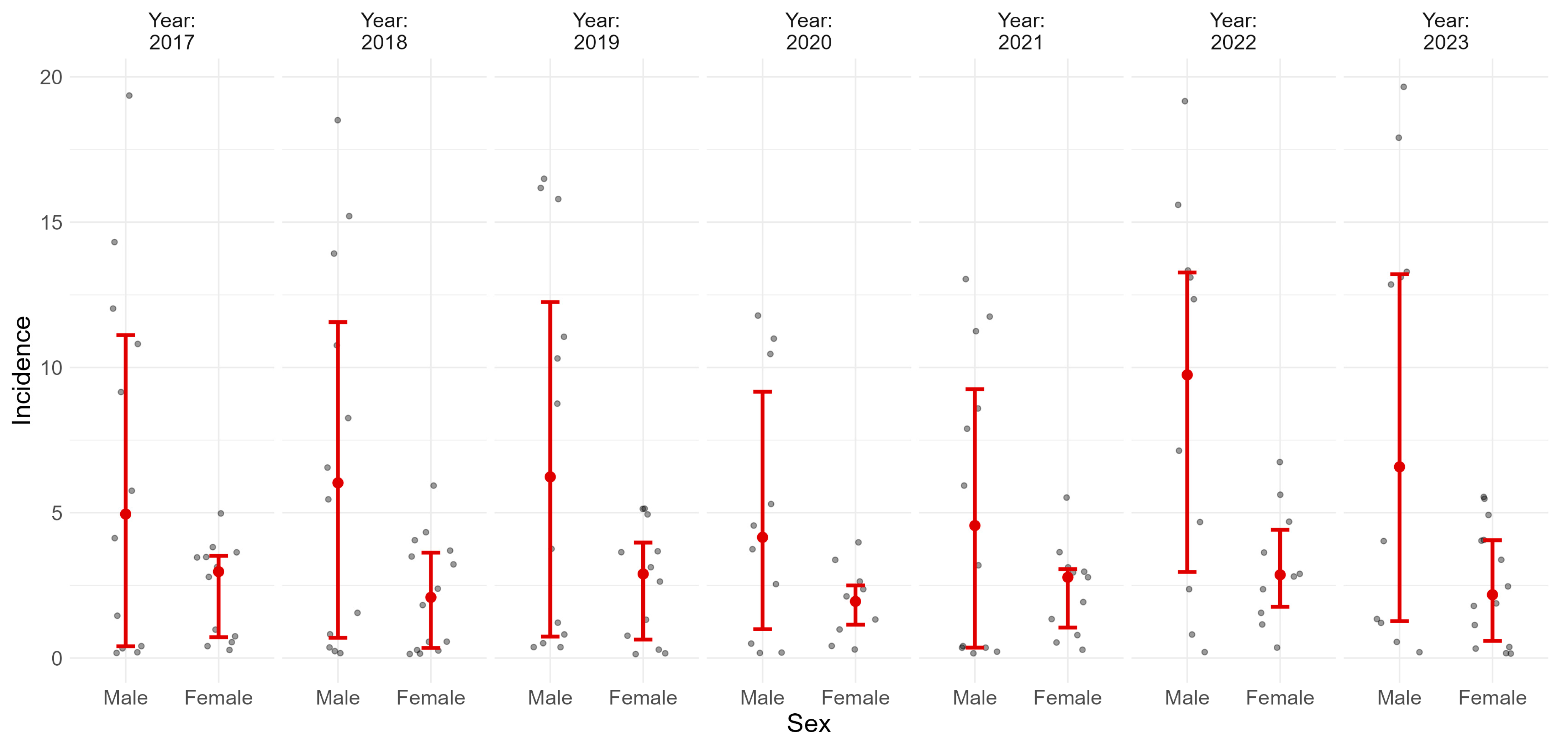
3.2. Temporal Trends and Sex Differences
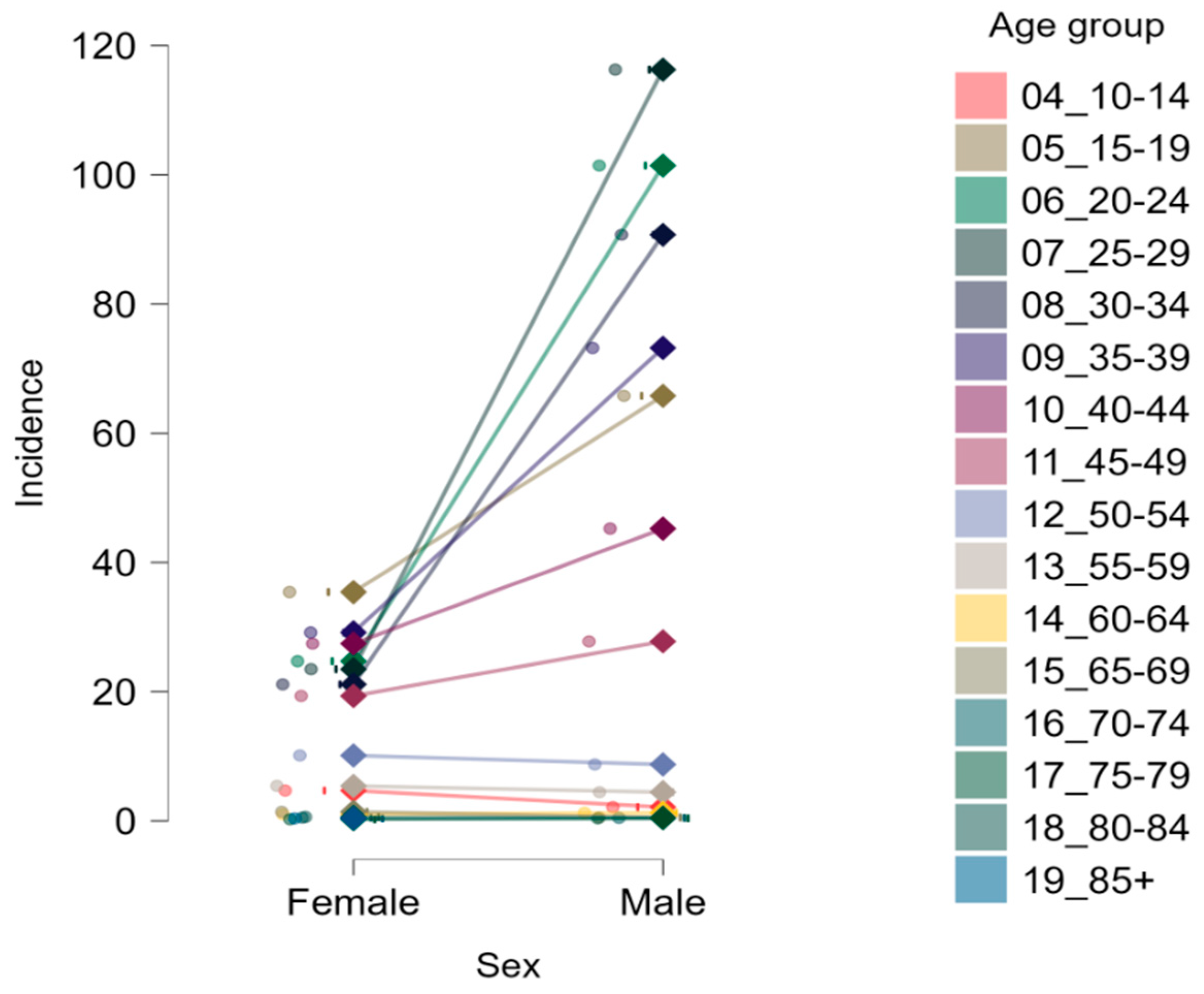
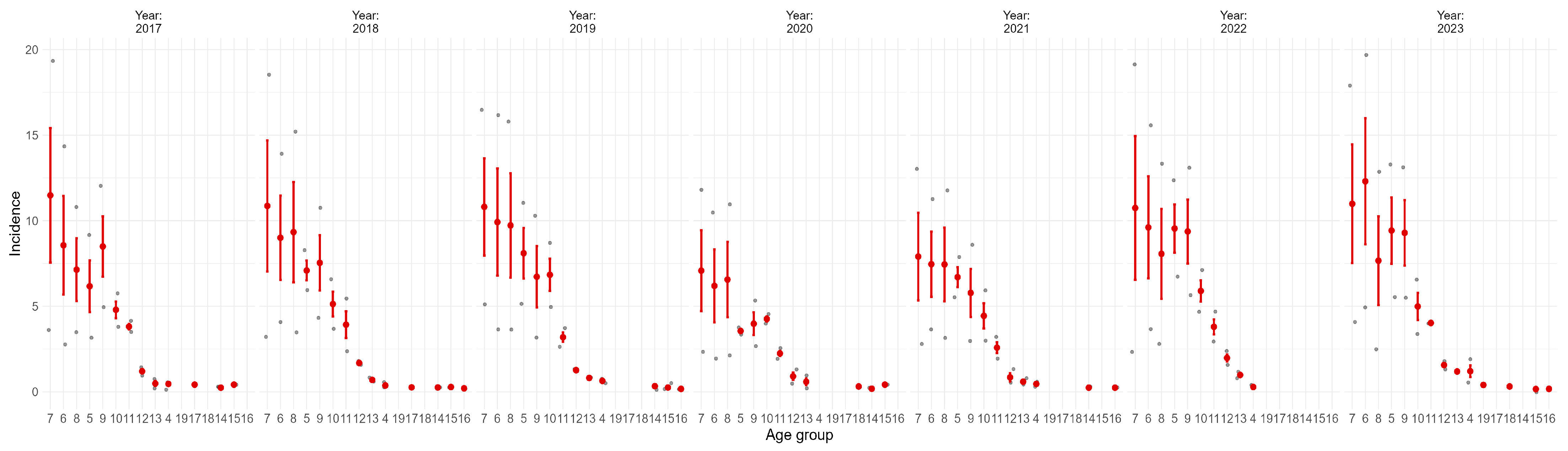
3.3. Age and Sex-Specific Incidence Patterns (2017–2023)
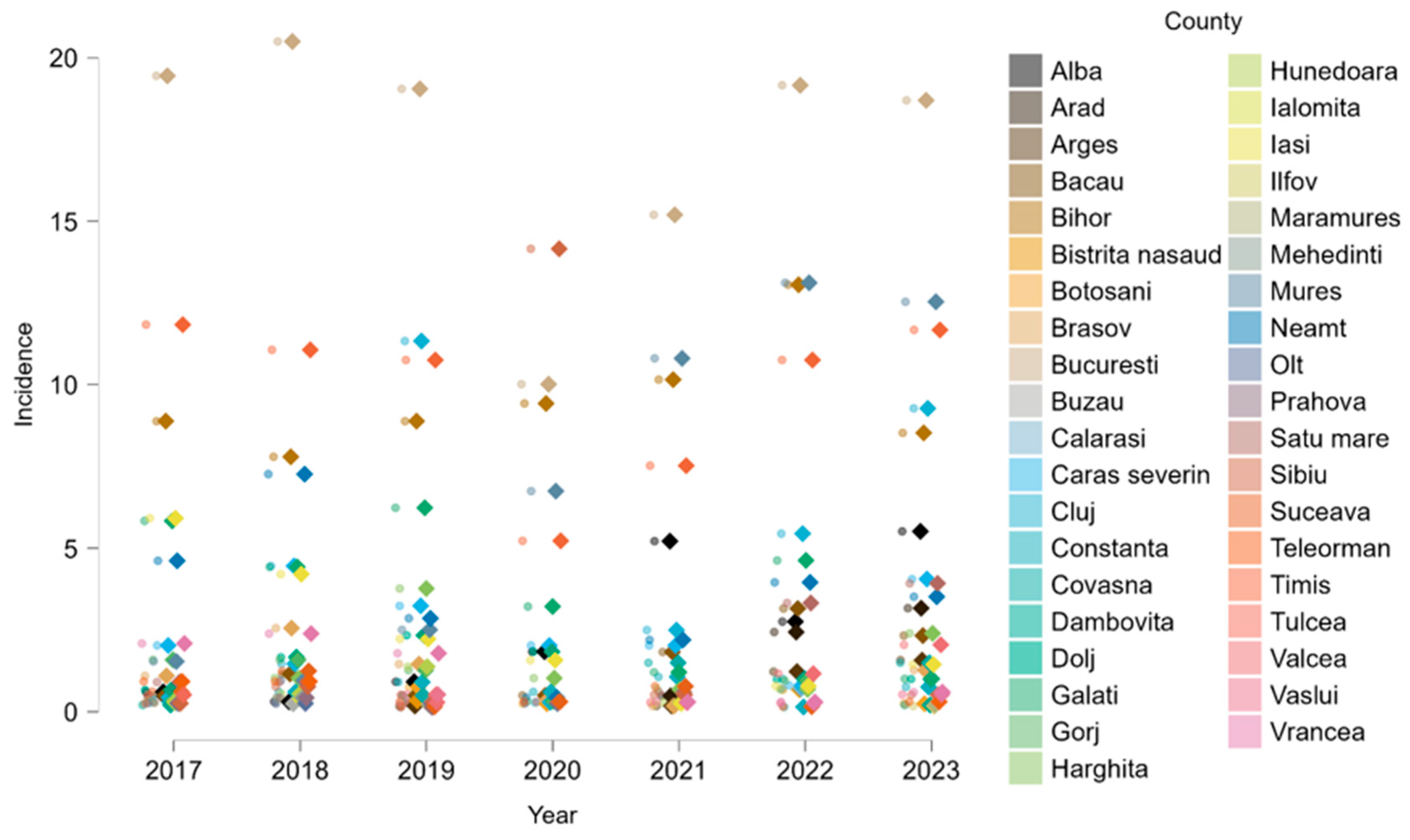
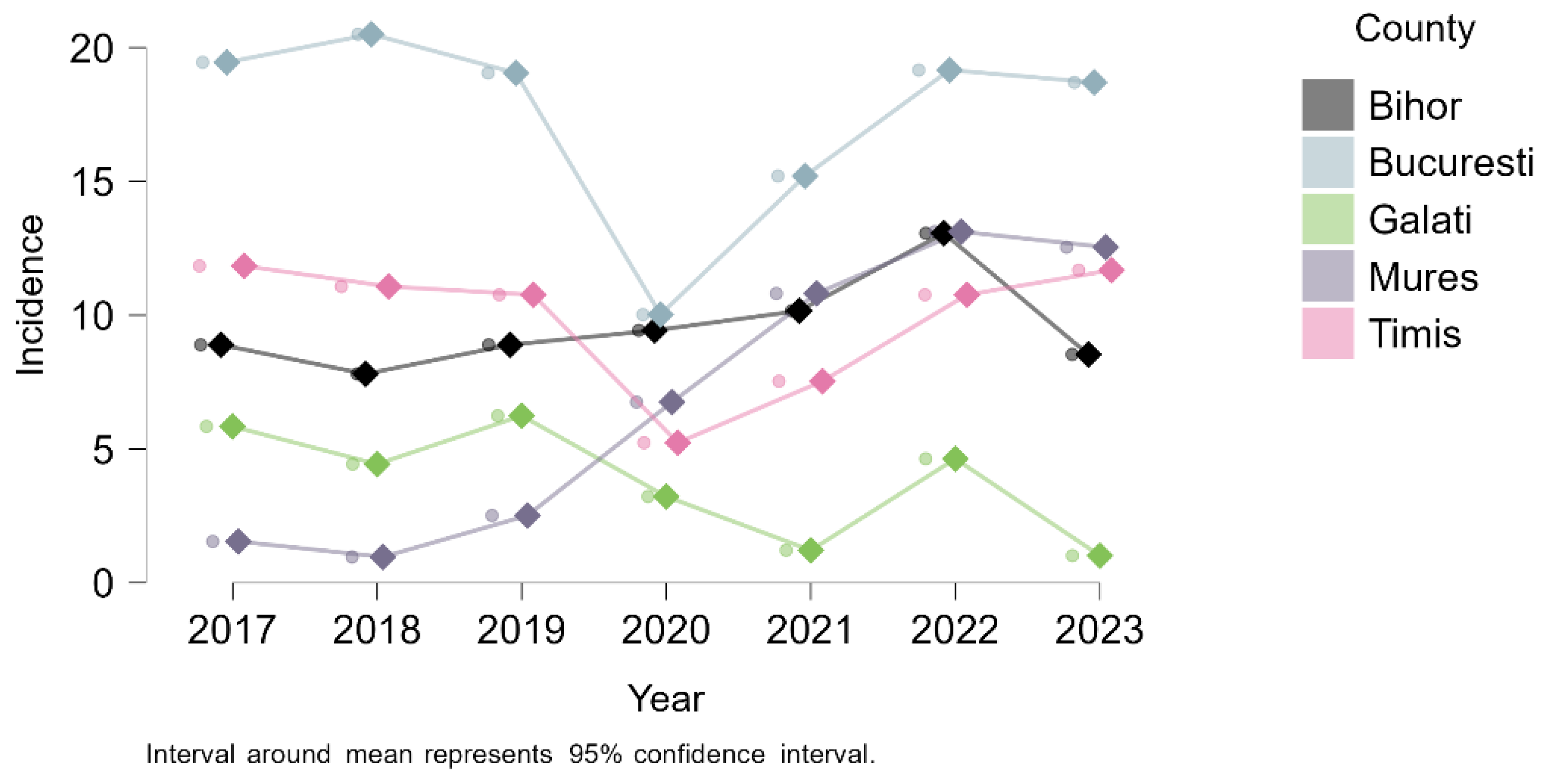
3.4. Geographic Distribution
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| ACL | Anterior cruciate ligament |
| MRI | Magnetic resonance imaging |
| ICD-10 | International Classification of Diseases, 10th Revision |
| M/F | Male-to-Female Ratio |
| ESSKA | European Society of Sports Traumatology, Knee Surgery and Arthroscopy |
| AAOS | American Academy of Orthopaedic Surgeons |
| COVID-19 | Coronavirus Disease 2019 |
References
- Gornitzky, A.L.; Lott, A.; Yellin, J.L.; Fabricant, P.D.; Lawrence, J.T.; Ganley, T.J. Sport-Specific Yearly Risk and Incidence of Anterior Cruciate Ligament Tears in High School Athletes: A Systematic Review and Meta-Analysis. Am. J. Sports Med. 2016, 44, 2716–2723. [Google Scholar] [CrossRef] [PubMed]
- Sanders, T.L.; Kremers, H.M.; Bryan, A.J.; Larson, D.R.; Dahm, D.L.; Levy, B.A.; Stuart, M.J.; Krych, A.J. Incidence of Anterior Cruciate Ligament Tears and Reconstruction: A 21-Year Population-Based Study. Am. J. Sports Med. 2016, 44, 1502–1507. [Google Scholar] [CrossRef] [PubMed]
- Kacprzak, B.; Stańczak, M.; Surmacz, J.; Hagner-Derengowska, M. Biophysics of ACL Injuries. Orthop. Rev. 2024, 16, 126041. [Google Scholar] [CrossRef] [PubMed]
- Martinez-Calderon, J.; Infante-Cano, M.; Matias-Soto, J.; Perez-Cabezas, V.; Galan-Mercant, A.; Garcia-Muñoz, C. The Incidence of Sport-Related Anterior Cruciate Ligament Injuries: An Overview of Systematic Reviews Including 51 Meta-Analyses. J. Funct. Morphol. Kinesiol. 2025, 10, 174. [Google Scholar] [CrossRef]
- Hewett, T.E.; Myer, G.D.; Ford, K.R. Anterior Cruciate Ligament Injuries in Female Athletes: Part 1, Mechanisms and Risk Factors. Am. J. Sports Med. 2006, 34, 299–311. [Google Scholar] [CrossRef]
- Gianakos, A.L.; Arias, C.; Batailler, C.; Servien, E.; Mulcahey, M.K. Sex-Specific Considerations in Anterior Cruciate Ligament Injuries in the Female Athlete: State of the Art. J. ISAKOS 2024, 9, 100325. [Google Scholar] [CrossRef]
- Alrowaili, M.G. The Impact of Age and Gender on Anterior Cruciate Ligament Injuries and Associated Knee Lesions: A Retrospective Study. Cureus 2024, 16, e68200. [Google Scholar] [CrossRef]
- Belozo, F.L.; Belozo, R.S.M.N.; Lopes, C.R.; Yamada, A.K.; Silva, V.R.R. Anterior Cruciate Ligament: A Brief Narrative Review of Main Risk Factors for Injury and Re-Injury. J. Bodyw. Mov. Ther. 2024, 38, 92–99. [Google Scholar] [CrossRef]
- Gupta, R.; Kapoor, A.; Soni, A.; Khatri, S.; Masih, G.D. Anterior Cruciate Ligament Tear Due to Non-Contact Mode of Injury Associated with Higher Incidence of Meniscal and Chondral Damage. J. Clin. Orthop. Trauma 2020, 11 (Suppl. S3), S342–S345. [Google Scholar] [CrossRef]
- Watanabe, S.; Joseph, G.B.; Sato, D.; Lansdown, D.A.; Guimaraes, J.B.; Link, T.M.; Ma, C.B. Longitudinal Changes in Medial Meniscal Extrusion after ACL Injury and Reconstruction and Its Relationship with Cartilage Degeneration Assessed Using MRI-Based T1ρ and T2 Analysis. Am. J. Sports Med. 2025, 53, 350–359. [Google Scholar] [CrossRef]
- Lohmander, L.S.; Englund, P.M.; Dahl, L.L.; Roos, E.M. The Long-Term Consequence of Anterior Cruciate Ligament and Meniscus Injuries: Osteoarthritis. Am. J. Sports Med. 2007, 35, 1756–1769. [Google Scholar] [CrossRef]
- Tayfur, B.; Charuphongsa, C.; Morrissey, D.; Miller, S.C. Neuromuscular Function of the Knee Joint Following Knee Injuries: Does It Ever Get Back to Normal? A Systematic Review with Meta-Analyses. Sports Med. 2021, 51, 321–338. [Google Scholar] [CrossRef] [PubMed]
- Filbay, S.R.; Skou, S.T.; Bullock, G.S.; Le, C.Y.; Räisänen, A.M.; Toomey, C.; Ezzat, A.M.; Hayden, A.; Culvenor, A.G.; Whittaker, J.L.; et al. Long-Term Quality of Life, Work Limitation, Physical Activity, Economic Cost and Disease Burden Following ACL and Meniscal Injury: A Systematic Review and Meta-Analysis for the OPTIKNEE Consensus. Br. J. Sports Med. 2022, 56, 1465–1474. [Google Scholar] [CrossRef] [PubMed]
- American Academy of Orthopaedic Surgeons (AAOS). Management of Anterior Cruciate Ligament Injuries: Clinical Practice Guideline. 2022. Available online: https://www.aaos.org/aclcpg (accessed on 31 July 2025).
- Tischer, T.; Andriolo, L.; Beaufils, P.; Ahmad, S.S.; Bait, C.; Bonomo, M.; Cavaignac, E.; Cristiani, R.; Feucht, M.J.; Fiodorovas, M.; et al. Management of Anterior Cruciate Ligament Revision in Adults: The 2022 ESSKA Consensus Part III—Indications for Different Clinical Scenarios Using the RAND/UCLA Appropriateness Method. Knee Surg. Sports Traumatol. Arthrosc. 2023, 31, 4662–4672. [Google Scholar] [CrossRef] [PubMed]
- ICD-10-GM-2023: S83.53—Rupture of Anterior Cruciate Ligament of Knee. Available online: https://medcode.ch/de/de/icds/ICD10-GM-2023/S83.53 (accessed on 11 May 2025).
- Institutul Național de Statistică (INS). Recensământul Populației și Locuințelor 2021. Available online: https://www.recensamantromania.ro (accessed on 31 July 2025).
- World Health Organization. Health Statistics and Information Systems: Definitions of Key Health Indicators. Available online: https://www.who.int/data/gho/indicator-metadata-registry/imr-details/313 (accessed on 2 August 2025).
- JASP Team. JASP, Version 0.95.0. [Computer software]; JASP Team: Amsterdam, The Netherlands, 2024. Available online: https://jasp-stats.org (accessed on 1 April 2025).
- Bahr, R.; Holme, I. Risk Factors for Sports Injuries—A Methodological Approach. Br. J. Sports Med. 2003, 37, 384–392. [Google Scholar] [CrossRef] [PubMed]
- Montalvo, A.M.; Schneider, D.K.; Webster, K.E.; Yut, L.; Galloway, M.T.; Heidt, R.S., Jr.; Kaeding, C.C.; Kremcheck, T.E.; Magnussen, R.A.; Parikh, S.N.; et al. Anterior Cruciate Ligament Injury Risk in Sport: A Systematic Review and Meta-Analysis of Injury Incidence by Sex and Sport Classification. J. Athl. Train. 2019, 54, 472–482. [Google Scholar] [CrossRef]
- Mallorquín, S.; Martínez-Sañudo, L.; González-Riveiro, M.; Viñas-Noguera, M.; Pizà-Serra, M.D.M.; Pelfort-López, X. Sports Injuries in the Emergency Department: An Observational Study with a Gender Perspective. Int. J. Emerg. Med. 2025, 18, 89. [Google Scholar] [CrossRef]
- Hanreich, C.; Boettner, F.; DeNegre, S.; Jungwirth-Weinberger, A.; Jerabek, S. The Impact of the COVID-19 Associated Shutdown on Orthopedic Patient Care. Arch. Orthop. Trauma Surg. 2023, 143, 2885–2892. [Google Scholar] [CrossRef]
- Nicolini, A.P.; Dantas Júnior, J.M.; Fração, O.C.; Franco, V.P.; Zobiole, A.F.; Carrijo, P.V. Impact of the COVID-19 Pandemic on Elective Knee Surgeries in Athletes. Acta Ortop. Bras. 2024, 32, e11073521. [Google Scholar] [CrossRef]
- Abram, S.G.F.; Price, A.J.; Judge, A.; Beard, D.J. ACL Reconstruction and Meniscal Repair Rates Have Both Increased in the Past 20 Years in England: Hospital Statistics from 1997 to 2017. Br. J. Sports Med. 2020, 54, 286–291. [Google Scholar] [CrossRef]
- Granan, L.P.; Forssblad, M.; Lind, M.; Engebretsen, L. The Scandinavian ACL Registries 2004–2007: Baseline Epidemiology. Acta Orthop. 2009, 80, 563–567. [Google Scholar] [CrossRef] [PubMed]
- Nordenvall, R.; Bahmanyar, S.; Adami, J.; Stenros, C.; Wredmark, T.; Felländer-Tsai, L. A Population-Based Nationwide Study of Cruciate Ligament Injury in Sweden, 2001–2009: Incidence, Treatment, and Sex Differences. Am. J. Sports Med. 2012, 40, 1808–1813. [Google Scholar] [CrossRef] [PubMed]
- Evans, J.; Mabrouk, A.; Nielson, J.L. Anterior Cruciate Ligament Knee Injury. In StatPearls [Internet]; StatPearls Publishing: Treasure Island, FL, USA, 2025. Available online: https://www.ncbi.nlm.nih.gov/books/NBK499848/ (accessed on 3 June 2025).
- Kaeding, C.C.; Léger-St-Jean, B.; Magnussen, R.A. Epidemiology and Diagnosis of Anterior Cruciate Ligament Injuries. Clin. Sports Med. 2017, 36, 1–8. [Google Scholar] [CrossRef] [PubMed]
- Motififard, M.; Aghdam, H.A.; Ravanbod, H.; Jafarpishe, M.S.; Shahsavan, M.; Daemi, A.; Mehrvar, A.; Rezvani, A.; Jamalirad, H.; Jajroudi, M.; et al. Demographic and Injury Characteristics as Potential Risk Factors for Anterior Cruciate Ligament Injuries: A Multicentric Cross-Sectional Study. J. Clin. Med. 2024, 13, 5063. [Google Scholar] [CrossRef]
- Caplan, N.; Kader, D.F. Knee Injury Patterns Among Men and Women in Collegiate Basketball and Soccer: NCAA Data and Review of Literature. In Classic Papers in Orthopaedics; Banaszkiewicz, P., Kader, D., Eds.; Springer: London, UK, 2014; pp. 285–291. [Google Scholar] [CrossRef]
- Hewett, T.E.; Myer, G.D.; Ford, K.R.; Heidt, R.S., Jr.; Colosimo, A.J.; McLean, S.G.; Van Den Bogert, A.J.; Paterno, M.V.; Succop, P. Biomechanical Measures of Neuromuscular Control and Valgus Loading of the Knee Predict Anterior Cruciate Ligament Injury Risk in Female Athletes: A Prospective Study. Am. J. Sports Med. 2005, 33, 492–501. [Google Scholar] [CrossRef]
- Tit, D.M.; Bungau, S.; Iovan, C.; Cseppento, D.C.N.; Endres, L.; Sava, C.; Sabau, A.M.; Furau, G.; Furau, C. Effects of the Hormone Replacement Therapy and of Soy Isoflavones on Bone Resorption in Postmenopause. J. Clin. Med. 2018, 7, 297. [Google Scholar] [CrossRef]
- Longo, U.G.; Nagai, K.; Salvatore, G.; Cella, E.; Candela, V.; Cappelli, F.; Ciccozzi, M.; Denaro, V. Epidemiology of Anterior Cruciate Ligament Reconstruction Surgery in Italy: A 15-Year Nationwide Registry Study. J. Clin. Med. 2021, 10, 223. [Google Scholar] [CrossRef]
- Maher, N.J.; Brogden, C.; Redmond, A.C.; Siddle, H.J.; Jones, G.; Buck, D.; Broadbent, S.; Liversidge, G.; Murr, J.; Tingle, C.; et al. Disparity in Anterior Cruciate Ligament Injury Management: A Case Series Review across Six National Health Service Trusts. BMC Musculoskelet. Disord. 2025, 26, 363. [Google Scholar] [CrossRef]
- Petre, I.; Barna, F.; Gurgus, D.; Tomescu, L.C.; Apostol, A.; Petre, I.; Furau, C.; Năchescu, M.L.; Bordianu, A. Analysis of the Healthcare System in Romania: A Brief Review. Healthcare 2023, 11, 2069. [Google Scholar] [CrossRef]
- Mihelic, R.; Jurdana, H.; Jotanovic, Z.; Madjarevic, T.; Tudor, A. Long-Term Results of Anterior Cruciate Ligament Reconstruction: A Comparison with Non-Operative Treatment with a Follow-Up of 17–20 Years. Int. Orthop. 2011, 35, 1093–1097. [Google Scholar] [CrossRef]
- Ajuied, A.; Wong, F.; Smith, C.; Norris, M.; Earnshaw, P.; Back, D.; Davies, A. Anterior Cruciate Ligament Injury and Radiologic Progression of Knee Osteoarthritis: A Systematic Review and Meta-Analysis. Am. J. Sports Med. 2014, 42, 2242–2252. [Google Scholar] [CrossRef] [PubMed]
- Cinque, M.E.; Dornan, G.J.; Chahla, J.; Moatshe, G.; LaPrade, R.F. High Rates of Osteoarthritis Develop after Anterior Cruciate Ligament Surgery: An Analysis of 4108 Patients. Am. J. Sports Med. 2018, 46, 2011–2019. [Google Scholar] [CrossRef] [PubMed]
- Pavel, R.M.S.; Radu, A.-F.; Nistor-Cseppento, C.D.; Vesa, C.M.; Purza, A.L.; Tit, D.M.; Radu, A.; Bungau, S.G. Integrating Clinimetric and Psychometric Approaches in Enhancing Osteoarthritis Care. Balneo PRM Res. J. 2024, 72, 6. Available online: http://bioclima.ro/Balneo748.pdf (accessed on 3 August 2025). [CrossRef]
- Pavel, R.M.S.; Purza, A.L.; Tit, D.M.; Radu, A.-F.; Iovanovici, D.C.; Vasileva, D.; Uivaraseanu, B.; Bungau, G.; Nistor-Cseppento, C.D. Functional Burden and Quality of Life in Hip and Knee Osteoarthritis: A Cross-Sectional Study. Medicina 2025, 61, 1155. [Google Scholar] [CrossRef]
- Filbay, S.R.; Culvenor, A.G.; Ackerman, I.N.; Russell, T.G.; Marlow, C.K. Quality of Life in Anterior Cruciate Ligament-Deficient Individuals: A Systematic Review and Meta-Analysis. Br. J. Sports Med. 2015, 49, 1033–1041. [Google Scholar] [CrossRef]
- Uivaraseanu, B.; Bungau, S.; Tit, D.M.; Behl, T.; Maghiar, T.A.; Maghiar, O.; Pantis, C.; Zaha, D.C.; Patrascu, J.M. Orthopedic surgery approach with uncemented metallic prosthesis in knee osteoarthritis increases the quality of life of young patients. Exp. Ther. Med. 2021, 21, 541. [Google Scholar] [CrossRef]
- Webster, K.E.; Feller, J.A. Exploring the High Reinjury Rate in Younger Patients Undergoing Anterior Cruciate Ligament Reconstruction. Am. J. Sports Med. 2016, 44, 2827–2832. [Google Scholar] [CrossRef]
- Filbay, S.R.; Ackerman, I.N.; Russell, T.G.; Crossley, K.M. Return to Sport Matters—Longer-Term Quality of Life after ACL Reconstruction in People with Knee Difficulties. Scand. J. Med. Sci. Sports 2017, 27, 514–524. [Google Scholar] [CrossRef]
- Filbay, S.R.; Crossley, K.M.; Ackerman, I.N. Activity Preferences, Lifestyle Modifications and Re-Injury Fears Influence Longer-Term Quality of Life in People with Knee Symptoms Following Anterior Cruciate Ligament Reconstruction: A Qualitative Study. J. Physiother. 2016, 62, 103–110. [Google Scholar] [CrossRef]
- Cierson, T.; Zhao, K.; Belkhelladi, M.; Babouras, A.; Jing, J.; Faith, J.; Corban, J.; Martineau, P.A. The Effect of the FIFA-11+ ACL Injury Prevention Program on Drop Vertical Jump Biomechanics in Varsity Athletes: A Prospective Observational Cohort Study. Orthop. J. Sports Med. 2025, 13, 23259671251333792. [Google Scholar] [CrossRef]
- Gilchrist, J.; Mandelbaum, B.R.; Melancon, H.; Ryan, G.W.; Silvers, H.J.; Griffin, L.Y.; Watanabe, D.S.; Dick, R.W.; Dvorak, J. A Randomized Controlled Trial to Prevent Noncontact Anterior Cruciate Ligament Injury in Female Collegiate Soccer Players. Am. J. Sports Med. 2008, 36, 1476–1483. [Google Scholar] [CrossRef]

| Year | Total Cases | Male | Female | M/F Ratio | Incidence (/100,000) | Total Incidence (/100,000) | |
|---|---|---|---|---|---|---|---|
| Male | Female | ||||||
| 2017 | 620 | 451 | 169 | 2.67 | 4.88 | 1.72 | 3.26 |
| 2018 | 660 | 480 | 180 | 2.67 | 5.19 | 1.83 | 3.46 |
| 2019 | 681 | 500 | 181 | 2.76 | 5.41 | 1.85 | 3.57 |
| 2020 | 420 | 292 | 128 | 2.28 | 3.16 | 1.31 | 2.20 |
| 2021 | 518 | 368 | 150 | 2.45 | 3.98 | 1.53 | 2.72 |
| 2022 | 706 | 518 | 188 | 2.76 | 5.60 | 1.92 | 3.71 |
| 2023 | 727 | 521 | 206 | 2.53 | 5.63 | 2.10 | 3.82 |
| Total | 4332 | 3130 | 1202 | 2.60 | – | – | 3.23 |
| Predictor | Unstandardized Coefficient | Standard Error | t Value | p Value |
|---|---|---|---|---|
| Intercept | 1.76 | 0.223 | 7.886 | <0.001 |
| Group (Male) | 3.084 | 0.182 | 16.93 | |
| Group (Total) | 1.497 | 0.182 | 8.218 | |
| Year | ||||
| 2018 | 0.207 | 0.278 | 0.743 | 0.472 |
| 2019 | 0.323 | 0.278 | 1.162 | 0.268 |
| 2020 | −1.063 | 0.278 | −3.821 | 0.002 |
| 2021 | −0.543 | 0.278 | −1.952 | 0.075 |
| 2022 | 0.457 | 0.278 | 1.641 | 0.127 |
| 2023 | 0.563 | 0.278 | 2.024 | 0.066 |
| Age Group (Years) | Cases | Incidence | Total Cases | M/F Ratio | Total Incidence | ||
|---|---|---|---|---|---|---|---|
| Female | Male | Female | Male | ||||
| 04_10–14 | 25 | 12 | 4.71 | 2.13 | 37 | 0.48 | 3.38 |
| 05_15–19 | 179 | 351 | 35.41 | 65.79 | 530 | 1.96 | 51.01 |
| 06_20–24 | 115 | 495 | 24.72 | 101.42 | 610 | 4.3 | 63.99 |
| 07_25–29 | 110 | 571 | 23.49 | 116.27 | 681 | 5.19 | 70.98 |
| 08_30–34 | 128 | 579 | 21.13 | 90.71 | 707 | 4.52 | 56.83 |
| 09_35–39 | 176 | 469 | 29.17 | 73.2 | 645 | 2.66 | 51.84 |
| 10_40–44 | 194 | 337 | 27.45 | 45.24 | 531 | 1.74 | 36.58 |
| 11_45–49 | 139 | 208 | 19.34 | 27.79 | 347 | 1.5 | 23.65 |
| 12_50–54 | 84 | 73 | 10.13 | 8.74 | 157 | 0.87 | 9.43 |
| 13_55–59 | 28 | 22 | 5.42 | 4.46 | 50 | 0.79 | 4.95 |
| 14_60–64 | 7 | 7 | 1.06 | 1.25 | 14 | 1 | 1.15 |
| 15_65–69 | 10 | 3 | 1.41 | 0.54 | 13 | 0.3 | 1.03 |
| 16_70–74 | 3 | 2 | 0.52 | 0.48 | 5 | 0.67 | 0.5 |
| 17_75–79 | 1 | 1 | 0.26 | 0.42 | 2 | 1 | 0.32 |
| 18_80–84 | 2 | 0 | 0.62 | 0 | 2 | 0 | - |
| 19_85+ | 1 | 0 | 0.4 | 0 | 1 | 0 | - |
| County | Total Cases | Hospitals | |||
|---|---|---|---|---|---|
| Public | Private | ||||
| n | n | % | n | % | |
| Bihor | 368 | 74 | 20.11 | 294 | 79.89 |
| Bucharest | 2096 | 1598 | 76.24 | 498 | 23.76 |
| Galati | 132 | 132 | 100.00 | 0 | 0.00 |
| Mures | 250 | 245 | 98.00 | 5 | 2.00 |
| Timiș | 448 | 410 | 91.52 | 38 | 8.48 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Published by MDPI on behalf of the Lithuanian University of Health Sciences. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Tolan, G.A.; Raducan, I.D.; Uivaraseanu, B.; Tit, D.M.; Bungau, G.S.; Radu, A.-F.; Furau, C.G. Nationwide Epidemiology of Hospitalized Acute ACL Ruptures in Romania: A 7-Year Analysis (2017–2023). Medicina 2025, 61, 1672. https://doi.org/10.3390/medicina61091672
Tolan GA, Raducan ID, Uivaraseanu B, Tit DM, Bungau GS, Radu A-F, Furau CG. Nationwide Epidemiology of Hospitalized Acute ACL Ruptures in Romania: A 7-Year Analysis (2017–2023). Medicina. 2025; 61(9):1672. https://doi.org/10.3390/medicina61091672
Chicago/Turabian StyleTolan, Gloria Alexandra, Ionut Daniel Raducan, Bogdan Uivaraseanu, Delia Mirela Tit, Gabriela S. Bungau, Andrei-Flavius Radu, and Cristian George Furau. 2025. "Nationwide Epidemiology of Hospitalized Acute ACL Ruptures in Romania: A 7-Year Analysis (2017–2023)" Medicina 61, no. 9: 1672. https://doi.org/10.3390/medicina61091672
APA StyleTolan, G. A., Raducan, I. D., Uivaraseanu, B., Tit, D. M., Bungau, G. S., Radu, A.-F., & Furau, C. G. (2025). Nationwide Epidemiology of Hospitalized Acute ACL Ruptures in Romania: A 7-Year Analysis (2017–2023). Medicina, 61(9), 1672. https://doi.org/10.3390/medicina61091672









