Clinical and Radiological Outcomes of Revision Anterior Cruciate Ligament Reconstruction Using a Quadriceps Tendon Autograft with a Bone Block: A Single-Center Case Series
Abstract
1. Introduction
2. Materials and Methods
2.1. Patient Selection
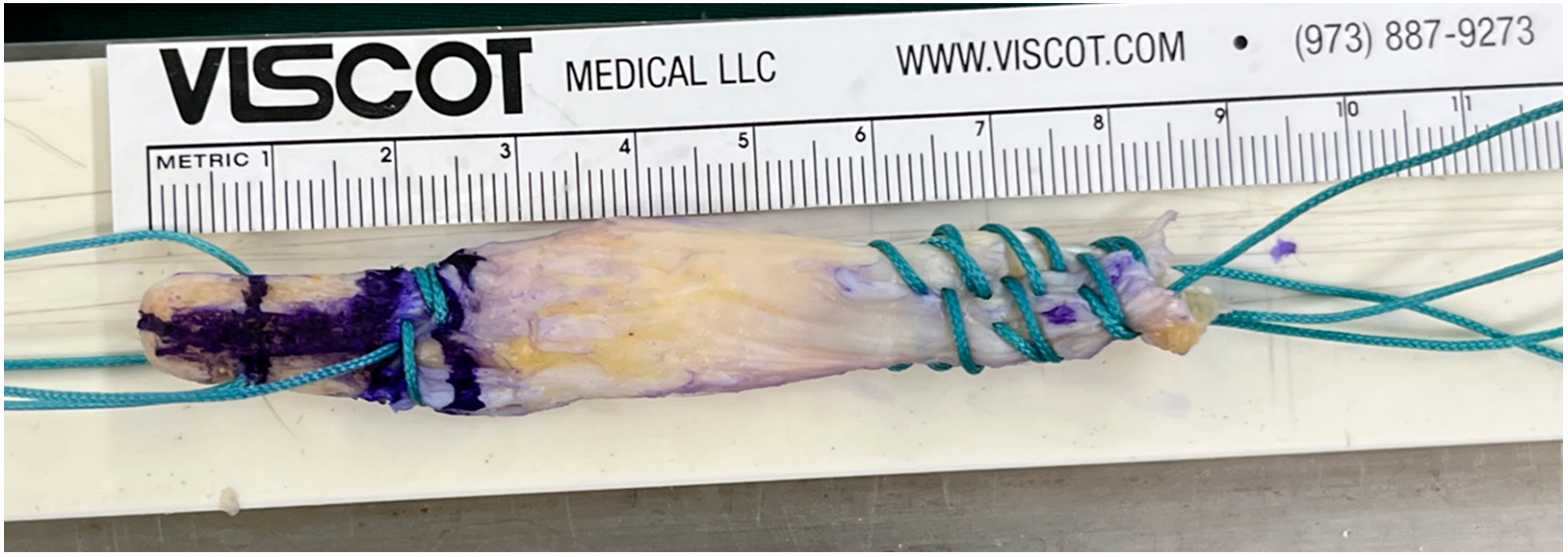
2.2. Surgical Techniques
2.3. Postoperative Rehabilitation
2.4. Clinical Evaluation
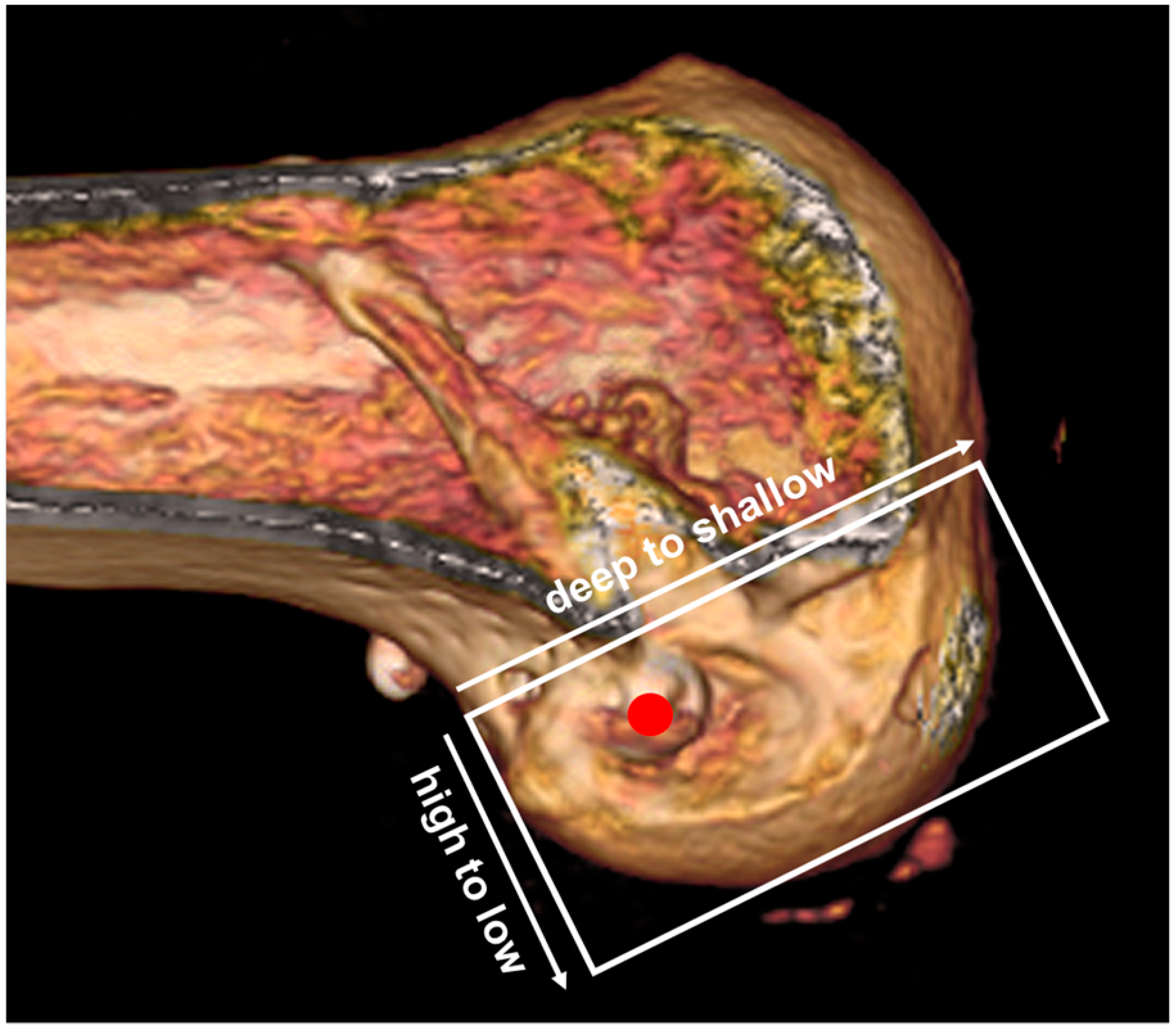
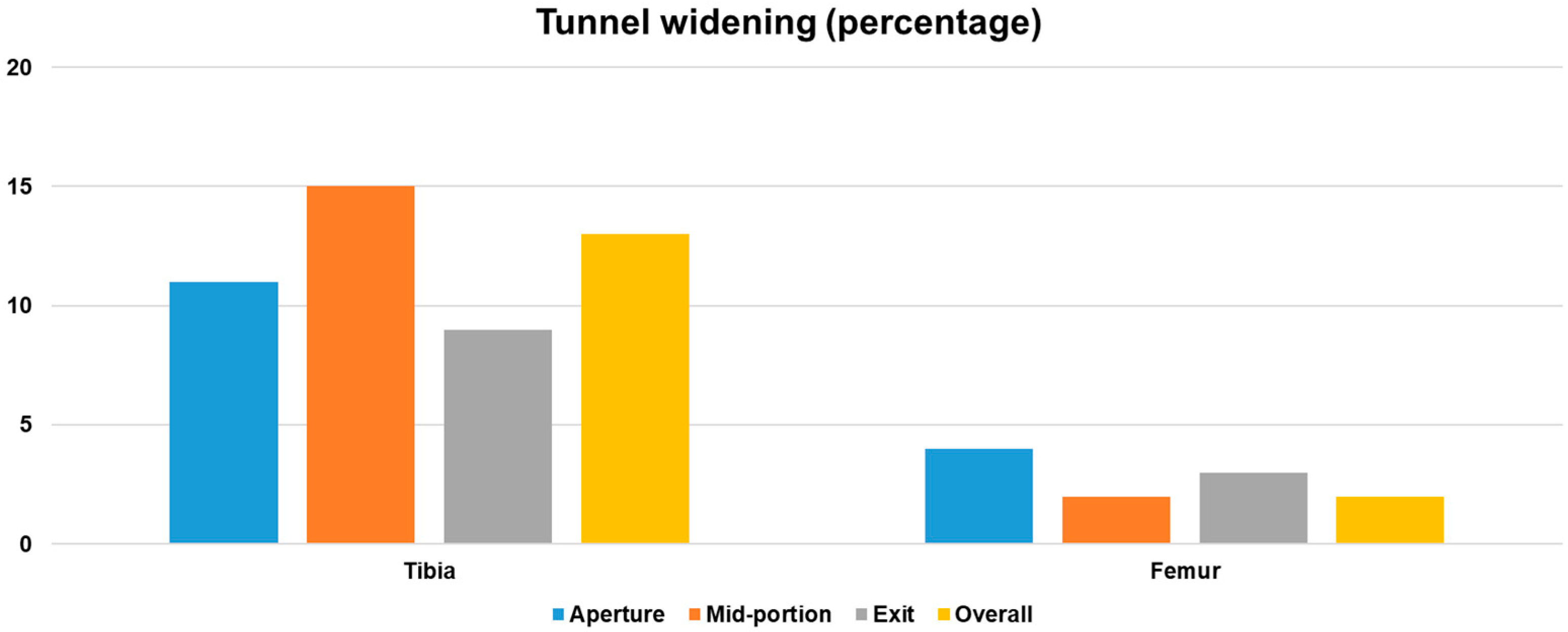
2.5. Radiological Evaluation
2.6. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Jeon, S.W.; Kim, S.H.; Kim, K.I. Optimal Tunnel Positioning and Graft Diameter to Minimize Impingement in Single-Bundle ACL Reconstruction: A 3D CT Simulation Analysis. Medicina 2025, 61, 946. [Google Scholar] [CrossRef]
- Reinerink, J.M.; Vendrig, T.; Keizer, M.N.J.; Hoogeslag, R.A.G.; Brouwer, R.W. One type of graft for reconstruction of the ACL does not suit all patients based on their characteristics and sports: A scoping review. Musculoskelet. Surg. 2025, 109, 115–125. [Google Scholar] [CrossRef]
- Gharpinde, M.R.; Pundkar, A.; Dhanwani, Y.; Chandanwale, R.; Jaiswal, A.M. Navigating Post-operative Challenges: A Comprehensive Review of Complications Following Anterior Cruciate Ligament (ACL) Tear Surgery. Cureus 2024, 16, e67768. [Google Scholar] [CrossRef]
- Chhabra, Y.; Saroha, S.; Hasan, K.; Thakrar, R.; Patel, A. Bone Patella Bone allografts show superior outcomes in revision ACL reconstruction: A systematic review and meta-analysis. Knee 2024, 51, 206–220. [Google Scholar] [CrossRef]
- Ashy, C.; Bailey, E.; Hutchinson, J.; Brennan, E.; Bailey, R.; Michael Pullen, W.; Xerogeanes, J.W.; Slone, H.S. Quadriceps tendon autograft has similar clinical outcomes when compared to hamstring tendon and bone-patellar tendon-bone autografts for revision ACL reconstruction: A systematic review and meta-analysis. Knee Surg. Sports Traumatol. Arthrosc. 2023, 31, 5463–5476. [Google Scholar] [CrossRef]
- Meena, A.; D’Ambrosi, R.; Runer, A.; Raj, A.; Attri, M.; Abermann, E.; Hoser, C.; Fink, C. Quadriceps tendon autograft with or without bone block have comparable clinical outcomes, complications and revision rate for ACL reconstruction: A systematic review. Knee Surg. Sports Traumatol. Arthrosc. 2023, 31, 2274–2288. [Google Scholar] [CrossRef]
- Ifarraguerri, A.M.; Graham, G.D.; White, A.B.; Berk, A.N.; Gachigi, K.K.; Siparsky, P.N.; Trofa, D.P.; Piasecki, D.P.; Fleischli, J.E.; Saltzman, B.M. Two-stage revision anterior cruciate ligament reconstruction reduces failure risk but leads to lesser clinical outcomes than single-stage revision after primary anterior cruciate ligament graft failure: A retrospective cohort study. Knee Surg. Relat. Res. 2025, 37, 5. [Google Scholar] [CrossRef]
- Meena, A.; Farinelli, L.; Hoser, C.; Abermann, E.; Hepperger, C.; Patralekh, M.K.; Herbort, M.; Fink, C. Primary Versus Revision ACL Reconstruction Using Quadriceps Autograft: A Matched-Control Cohort Study. Orthop. J. Sports Med. 2024, 12, 23259671231224501. [Google Scholar] [CrossRef]
- Lin, L.; Wang, H.J.; Wang, Y.J.; Wang, J.; Chen, Y.R.; Yu, J.K. Comparison of the Clinical Outcomes of Revision and Primary ACL Reconstruction: A Matched-Pair Analysis with 3–5 Years of Follow-up. Am. J. Sports Med. 2023, 51, 634–641. [Google Scholar] [CrossRef]
- Koca, F.; Stalman, A.; Vestberg, C.; Cristiani, R.; Faltstrom, A. Poorer patient-reported knee function and quality of life, but not activity level, after revision ACL reconstruction compared with primary ACL reconstruction: A matched-pair analysis with a minimum 5-year follow-up. BMC Musculoskelet. Disord. 2023, 24, 831. [Google Scholar] [CrossRef]
- Yan, X.; Yang, X.G.; Feng, J.T.; Liu, B.; Hu, Y.C. Does Revision Anterior Cruciate Ligament (ACL) Reconstruction Provide Similar Clinical Outcomes to Primary ACL Reconstruction? A Systematic Review and Meta-Analysis. Orthop. Surg. 2020, 12, 1534–1546. [Google Scholar] [CrossRef]
- Grassi, A.; Ardern, C.L.; Marcheggiani Muccioli, G.M.; Neri, M.P.; Marcacci, M.; Zaffagnini, S. Does revision ACL reconstruction measure up to primary surgery? A meta-analysis comparing patient-reported and clinician-reported outcomes, and radiographic results. Br. J. Sports Med. 2016, 50, 716–724. [Google Scholar] [CrossRef]
- Grassi, A.; Nitri, M.; Moulton, S.G.; Marcheggiani Muccioli, G.M.; Bondi, A.; Romagnoli, M.; Zaffagnini, S. Does the type of graft affect the outcome of revision anterior cruciate ligament reconstruction? a meta-analysis of 32 studies. Bone Joint J. 2017, 99-B, 714–723. [Google Scholar] [CrossRef]
- Ajrawat, P.; Dwyer, T.; Whelan, D.; Theodoropoulos, J.; Murnaghan, L.; Bhargava, M.; Ogilvie-Harris, D.; Chahal, J. A Comparison of Quadriceps Tendon Autograft With Bone-Patellar Tendon-Bone Autograft and Hamstring Tendon Autograft for Primary Anterior Cruciate Ligament Reconstruction: A Systematic Review and Quantitative Synthesis. Clin. J. Sport. Med. 2021, 31, 392–399. [Google Scholar] [CrossRef]
- Liau, Z.Q.G.; Ng, M.S.P.; Low, S.S.E.; Chin, B.Z.; Hui, J.H.P.; Kagda, F.H.Y. A novel practical method to predict anterior cruciate ligament hamstring graft size using preoperative MRI. Knee Surg. Relat. Res. 2024, 36, 17. [Google Scholar] [CrossRef]
- Lee, D.W.; Lee, S.; Ro, D.H.; Han, H.S. Satisfactory Clinical Outcomes of Revision Anterior Cruciate Ligament Reconstruction Using Quadriceps Tendon-Patellar Bone Allograft. Clin. Orthop. Surg. 2025, 17, 91–99. [Google Scholar] [CrossRef]
- Winkler, P.W.; Vivacqua, T.; Thomassen, S.; Lovse, L.; Lesniak, B.P.; Getgood, A.M.J.; Musahl, V. Quadriceps tendon autograft is becoming increasingly popular in revision ACL reconstruction. Knee Surg. Sports Traumatol. Arthrosc. 2022, 30, 149–160. [Google Scholar] [CrossRef]
- Marcaccio, S.E.; Morrissey, P.J.; Testa, E.J.; Fadale, P.D. Role of Quadriceps Tendon Autograft in Primary and Revision Anterior Cruciate Ligament Reconstruction. JBJS Rev. 2023, 11, e23.00057. [Google Scholar] [CrossRef]
- Lee, D.W.; Lee, D.H.; Moon, S.G.; Kang, J.H.; Woo, Y.J.; Kim, W.J. Femoral Tunnel Geometry and Graft Inclination Angles in Anterior Cruciate Ligament Reconstruction Using a Flexible Reamer System. Medicina 2023, 59, 1031. [Google Scholar] [CrossRef]
- Kim, M.J.; Moon, S.G.; Kang, J.H.; Lee, D.W. Usefulness of 3-Dimensional Computed Tomography Assessment of Femoral Tunnel after Anterior Cruciate Ligament Reconstruction. Medicina 2023, 59, 1716. [Google Scholar] [CrossRef]
- Lamoria, R.; Sharma, A.; Goyal, D.; Upadhyay, R. Influence of three different fixation methods on femoral tunnel widening in ACL reconstructed patients evaluated using computed tomography (CT) scan. Eur. J. Orthop. Surg. Traumatol. 2020, 30, 411–417. [Google Scholar] [CrossRef]
- Meena, A.; Farinelli, L.; Hoser, C.; Abermann, E.; Raj, A.; Hepperger, C.; Herbort, M.; Fink, C. Revision ACL reconstruction using quadriceps, hamstring and patellar tendon autografts leads to similar functional outcomes but hamstring graft has a higher tendency of graft failure. Knee Surg. Sports Traumatol. Arthrosc. 2023, 31, 2461–2468. [Google Scholar] [CrossRef]
- Fujino, K.; Keith, S.; Kamalitdinov, T.B.; Madi, R.; Jiang, X.; Zgonis, M.H.; Miller, L.M.; Kuntz, A.F.; Dyment, N.A. Compressive Graft Fit Promotes Tendon-to-Bone Integration After Anterior Cruciate Ligament Reconstruction. Am. J. Sports Med. 2025, 53, 2162–2172. [Google Scholar] [CrossRef]
- Tabbaa, A.; Atkins, M.; Montalvo, A.M.; Petit, C.B.; White, M.S.; Petushek, E.J.; Diekfuss, J.A.; Myer, G.D.; Lamplot, J.D. Lower ACLR Failure Rates in Bone-Soft Tissue Versus Soft Tissue-Only Allografts in Adults: A Systematic Review and Meta-analysis. Am. J. Sports Med. 2025, 53, 734–744. [Google Scholar] [CrossRef]
- Daniel, S.J.; Timothy, J.; Kandagaddala, M.; Reka, K.; Poonnoose, P.M.; Oommen, A.T. Decreased femur tunnel widening after augmented suspensory fixation compared to suspensory fixation for single bundle hamstring ACL reconstruction. J. Clin. Orthop. Trauma. 2024, 48, 102331. [Google Scholar] [CrossRef]
- Biswal, U.K.; Balaji, G.; Nema, S.; Poduval, M.; Menon, J.; Patro, D.K. Correlation of tunnel widening and tunnel positioning with short-term functional outcomes in single-bundle anterior cruciate ligament reconstruction using patellar tendon versus hamstring graft: A prospective study. Eur. J. Orthop. Surg. Traumatol. 2016, 26, 647–655. [Google Scholar] [CrossRef]
- Vivekanantha, P.; Kahlon, H.; Hassan, Z.; Slawaska-Eng, D.; Abdel-Khalik, H.; Johnson, J.; de Sa, D. Hamstring autografts demonstrate either similar or inferior outcomes to quadriceps or bone-patellar tendon-bone autografts in revision anterior cruciate ligament reconstruction: A systematic review of comparative studies. Knee Surg. Sports Traumatol. Arthrosc. 2025, 33, 413–427. [Google Scholar] [CrossRef]
- El Khoury, G.; Hardy, A.; Saint-Etienne, A.; Saghbiny, E.; Meyer, A.; Grimaud, O.; Gerometta, A.; Lefevre, N.; Bohu, Y. Return to Sport After Revision ACL Reconstruction: A Comparative Cohort Study of Outcomes After Single- Versus Multiple-Revision Surgeries. Orthop. J. Sports Med. 2022, 10, 23259671221133762. [Google Scholar] [CrossRef]
- Lee, D.W.; Kim, J.G.; Cho, S.I.; Kim, D.H. Clinical Outcomes of Isolated Revision Anterior Cruciate Ligament Reconstruction or in Combination With Anatomic Anterolateral Ligament Reconstruction. Am. J. Sports Med. 2019, 47, 324–333. [Google Scholar] [CrossRef]
- Meena, A.; Das, S.; Runer, A.; Tapasvi, K.; Hegde, P.; D’Ambrosi, R.; Hiemstra, L.; Tapasvi, S. Revision ACL reconstruction in female athletes: Current concepts. J. ISAKOS 2024, 9, 464–470. [Google Scholar] [CrossRef]
- Hughes, J.D.; Burnham, J.M.; Hirsh, A.; Musahl, V.; Fu, F.H.; Irrgang, J.J.; Lynch, A.D. Comparison of Short-term Biodex Results After Anatomic Anterior Cruciate Ligament Reconstruction Among 3 Autografts. Orthop. J. Sports Med. 2019, 7, 2325967119847630. [Google Scholar] [CrossRef] [PubMed]
- Horteur, C.; Rubens Duval, B.; Merlin, A.; Cognault, J.; Ollivier, M.; Pailhe, R. Comparison of knee extensor strength after anterior cruciate ligament reconstruction using either quadriceps tendon or hamstring tendon autografts. Eur. J. Orthop. Surg. Traumatol. 2022, 32, 857–865. [Google Scholar] [CrossRef] [PubMed]
- Setliff, J.C.; Gibbs, C.M.; Musahl, V.; Lesniak, B.P.; Hughes, J.D.; Rabuck, S.J. Harvesting a second graft from the extensor mechanism for revision ACL reconstruction does not delay return of quadriceps function. Knee Surg. Sports Traumatol. Arthrosc. 2023, 31, 2828–2835. [Google Scholar] [CrossRef] [PubMed]


| N = 34 | |
|---|---|
| Age, years | 27.2 ± 5.8 |
| Sex, n, Male/Female | 28/6 |
| Body mass index, kg/m2 | 23.6 ± 4.7 |
| Follow-up duration, months | 37.4 ± 3.2 |
| Concomitant procedure, n (%) | |
| Meniscal repair | 9 (26.5%) |
| Meniscectomy | 7 (20.6%) |
| Cartilage repair | 4 (11.8%) |
| Preoperative | Last Follow-Up | p-Value | |
|---|---|---|---|
| Lysholm score | 62.7 ± 9.6 | 87.1 ± 10.3 | <0.001 |
| IKDC subjective score | 59.0 ± 10.8 | 79.5 ± 11.1 | <0.001 |
| Tegner activity scale | 3.5 ± 1.2 | 5.6 ± 1.3 | <0.001 |
| Pivot shift test (0/1/2/3), n | (0/9/10/15) | (29/2/3/0) | <0.001 |
| Deficit of isokinetic extensor strength (%) | 28.7 ± 12.5 | 12.4 ± 8.1 | <0.001 |
| Deficit of isokinetic flexor strength (%) | 18.3% ± 9.7 | 8.9% ± 6.5 | <0.001 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Published by MDPI on behalf of the Lithuanian University of Health Sciences. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lee, D.W.; Moon, S.G.; Kang, J.H.; Cho, S.I.; Kim, W.J. Clinical and Radiological Outcomes of Revision Anterior Cruciate Ligament Reconstruction Using a Quadriceps Tendon Autograft with a Bone Block: A Single-Center Case Series. Medicina 2025, 61, 1634. https://doi.org/10.3390/medicina61091634
Lee DW, Moon SG, Kang JH, Cho SI, Kim WJ. Clinical and Radiological Outcomes of Revision Anterior Cruciate Ligament Reconstruction Using a Quadriceps Tendon Autograft with a Bone Block: A Single-Center Case Series. Medicina. 2025; 61(9):1634. https://doi.org/10.3390/medicina61091634
Chicago/Turabian StyleLee, Dhong Won, Sung Gyu Moon, Ji Hee Kang, Seung Ik Cho, and Woo Jong Kim. 2025. "Clinical and Radiological Outcomes of Revision Anterior Cruciate Ligament Reconstruction Using a Quadriceps Tendon Autograft with a Bone Block: A Single-Center Case Series" Medicina 61, no. 9: 1634. https://doi.org/10.3390/medicina61091634
APA StyleLee, D. W., Moon, S. G., Kang, J. H., Cho, S. I., & Kim, W. J. (2025). Clinical and Radiological Outcomes of Revision Anterior Cruciate Ligament Reconstruction Using a Quadriceps Tendon Autograft with a Bone Block: A Single-Center Case Series. Medicina, 61(9), 1634. https://doi.org/10.3390/medicina61091634







