Diagnostic Value of Bronchoscopy in Detecting Laryngopharyngeal Disorders: Clinical Utility and Limitations
Abstract
1. Introduction
2. Materials and Methods
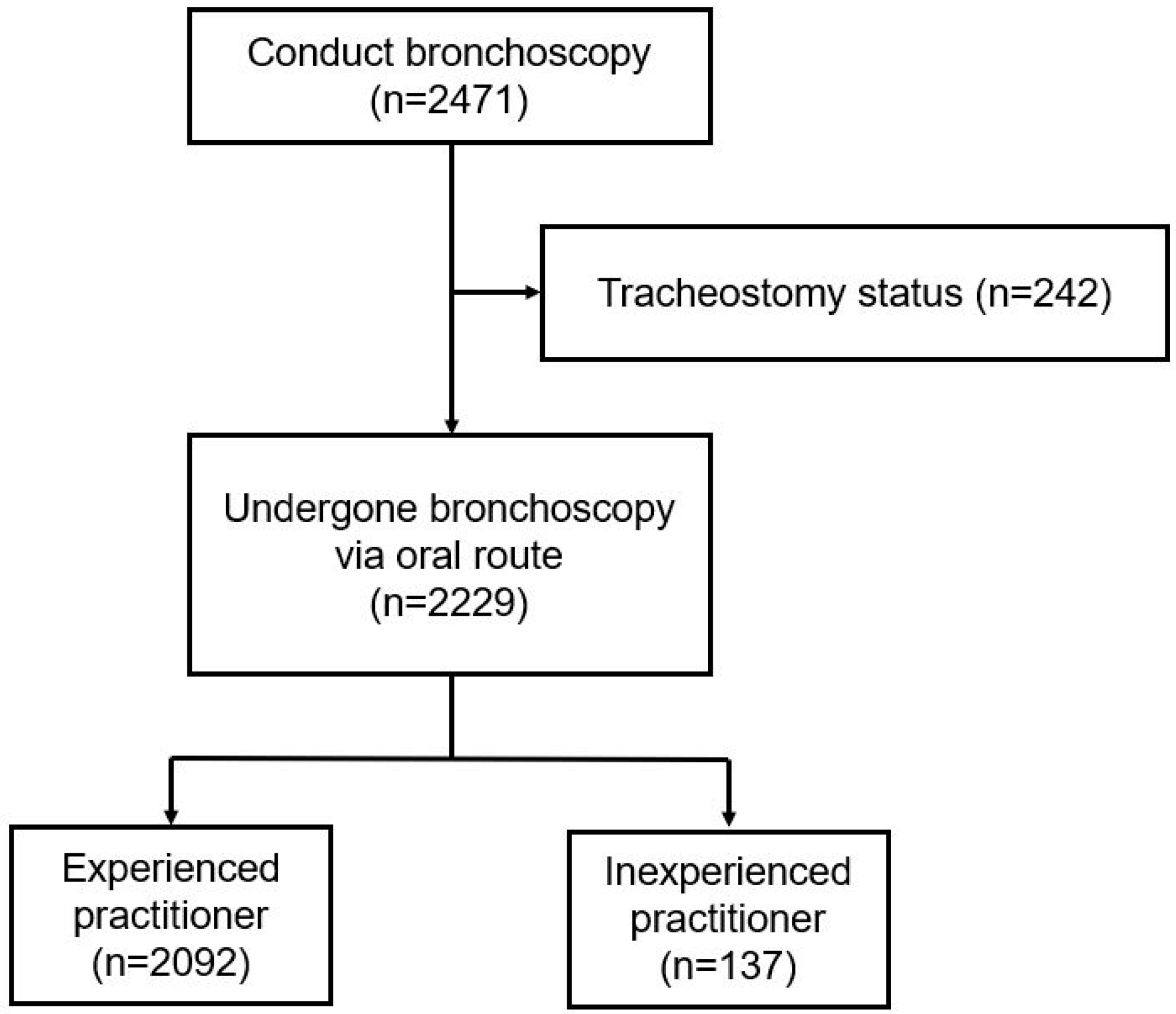
2.1. Study Population
2.2. Data Collection
2.3. Bronchoscopy Operator
2.4. Additional Consultation
2.5. Statistical Analysis
3. Results
3.1. Patients
3.2. Bronchoscopy Operator
3.3. Presence of Malignancy
3.4. Multivariate Analysis for the Abnormal Finding Group
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| CT | Computed tomography |
| MRI | Magnetic resonance imaging |
| OR | Odds ratio |
| OL | Otolaryngology |
| CI | Confidence interval |
| SPSS | Statistical Package for the Social Sciences |
References
- Miller, R.J.; Casal, R.F.; Lazarus, D.R.; Ost, D.E.; Eapen, G.A. Flexible bronchoscopy. Clin. Chest Med. 2018, 39, 1–16. [Google Scholar] [CrossRef] [PubMed]
- Casal, R.F.; Ost, D.E.; Eapen, G.A. Flexible bronchoscopy. Clin. Chest Med. 2013, 34, 341–352. [Google Scholar] [CrossRef]
- Zhang, J.; Perret, J.L.; Chang, A.B.; Idrose, N.S.; Bui, D.S.; Lowe, A.J.; Abramson, M.J.; Walters, E.H.; Lodge, C.J.; Dharmage, S.C. Risk factors for chronic cough in adults: A systematic review and meta-analysis. Respirology 2022, 27, 36–47. [Google Scholar] [CrossRef]
- Athish, K.K.; Guruprasad, T.J.; Padmanabha, S.; Harshitha, K.R. Subglottic adenoid cystic carcinoma mimicking bronchial asthma: A case report. Cureus 2024, 16, e60571. [Google Scholar] [CrossRef]
- Kashif, M.; Singh, T.; Aslam, A.; Khaja, M. Asthma mimic: Case report and literature review of vocal cord nodule associated with wheezing. SAGE Open Med. Case Rep. 2017, 5, 2050313X17744980. [Google Scholar] [CrossRef]
- Kompelli, A.R.; Li, H.; Neskey, D.M. Impact of Delay in Treatment Initiation on Overall Survival in Laryngeal Cancers. Otolaryngol. Head Neck Surg. 2019, 160, 651–657. [Google Scholar] [CrossRef] [PubMed]
- Paul, B.C.; Chen, S.; Sridharan, S.; Fang, Y.; Amin, M.R.; Branski, R.C. Diagnostic accuracy of history, laryngoscopy, and stroboscopy. Laryngoscope 2013, 123, 215–219. [Google Scholar] [CrossRef]
- Mannelli, G.; Cecconi, L.; Gallo, O. Laryngeal preneoplastic lesions and cancer: Challenging diagnosis. Qualitative literature review and meta-analysis. Crit. Rev. Oncol. Hematol. 2016, 106, 64–90. [Google Scholar] [CrossRef]
- Hut, A.-R.; Boia, E.R.; Para, D.; Iovanescu, G.; Horhat, D.; Mikša, L.; Chiriac, M.; Galant, R.; Motofelea, A.C.; Balica, N.C. Laryngeal Cancer in the Modern Era: Evolving Trends in Diagnosis, Treatment, and Survival Outcomes. J. Clin. Med. 2025, 14, 3367. [Google Scholar] [CrossRef]
- Thoeny, H.C.; Delaere, P.R.; Hermans, R. Correlation of local outcome after partial laryngectomy with cartilage abnormalities on CT. AJNR Am. J. Neuroradiol. 2005, 26, 674–678. [Google Scholar] [PubMed]
- Voduc, N.; Adamson, R.; Kashgari, A.; Fenton, M.; Porhownick, N.; Wojnar, M.; Sharma, K.; Gillson, A.M.; Chung, C.; McConnell, M. Development of learning curves for bronchoscopy: Results of a multicenter study of pulmonary trainees. Chest 2020, 158, 2485–2492. [Google Scholar] [CrossRef] [PubMed]
- Mohan, A.; Madan, K.; Hadda, V.; Tiwari, P.; Mittal, S.; Guleria, R.; Khilnani, G.C.; Luhadia, S.K.; Solanki, R.N.; Gupta, K.B.; et al. Guidelines for diagnostic flexible bronchoscopy in adults: Joint Indian Chest Society/National College of Chest Physicians (I)/Indian Association for Bronchology recommendations. Lung India 2019, 36 (Suppl. S2), S37–S89. [Google Scholar] [CrossRef] [PubMed]
- Ernst, A.; Silvestri, G.A.; Johnstone, D. Interventional pulmonary procedures: Guidelines from the American College of Chest Physicians. Chest 2003, 123, 1693–1717. [Google Scholar] [CrossRef]
- Ning, J.; Ge, T.; Jiang, M.; Jia, K.; Wang, L.; Li, W.; Chen, B.; Liu, Y.; Wang, H.; Zhao, S.; et al. Early diagnosis of lung cancer: Which is the optimal choice? Aging 2021, 13, 6214–6227. [Google Scholar] [CrossRef]
- Ong, P.G.; Debiane, L.G.; Casal, R.F. Recent advances in diagnostic bronchoscopy. J. Thorac. Dis. 2016, 8, 3808–3817. [Google Scholar] [CrossRef] [PubMed]
- Kuo, C.H.; Niu, C.K.; Yu, H.R.; Chung, M.Y.; Hwang, C.F.; Hwang, K.P. Applications of flexible bronchoscopy in infants with congenital vocal cord paralysis: A 12-year experience. Pediatr. Neonatol. 2008, 49, 183–188. [Google Scholar] [CrossRef][Green Version]
- Haddad, G.; Sataloff, R.T.; Hamdan, A.L. Laryngeal metastatic lesions: A literature review. J. Voice 2024, 38, 1458–1464. [Google Scholar] [CrossRef]
- Lee, Y.C.; Fang, T.J.; Lin, C.T. Metastatic endometrial adenocarcinoma to the larynx: A case report and discussion of upper airway management. J. Palliat. Med. 2014, 17, 867–869. [Google Scholar] [CrossRef]
- Chen, T.Y.; Hung, G.U.; Hung, C.C.; Chiu, J.S.; Kao, C.H. Asymptomatic metastasis to the larynx detected by FDG PET/CT in a patient with recurrent rectal adenocarcinoma. Clin. Nucl. Med. 2012, 37, e178–e180. [Google Scholar] [CrossRef]
- Glastonbury, C.M.; Parker, E.E.; Hoang, J.K. The postradiation neck: Evaluating response to treatment and recognizing complications. AJR Am. J. Roentgenol. 2010, 195, W164–W171. [Google Scholar] [CrossRef]
- Koroulakis, A.; Agarwal, M. Laryngeal Cancer. In StatPearls [Internet]; StatPearls Publishing: Treasure Island, FL, USA, 2025. [Google Scholar] [PubMed]
- Bhattacharyya, S.; Mandal, S.; Banerjee, S.; Mandal, G.K.; Bhowmick, A.K.; Murmu, N. Cannabis smoke can be a major risk factor for early-age laryngeal cancer—A molecular signaling-based approach. Tumour Biol. 2015, 36, 6029–6036. [Google Scholar] [CrossRef]
- Ferster, A.P.O.; Schubart, J.; Kim, Y.; Goldenberg, D. Association between laryngeal cancer and asbestos exposure: A systematic review. JAMA Otolaryngol. Head Neck Surg. 2017, 143, 409–416. [Google Scholar] [CrossRef] [PubMed]
- Menach, P.; Oburra, H.O.; Patel, A. Cigarette smoking and alcohol ingestion as risk factors for laryngeal squamous cell carcinoma at Kenyatta National Hospital, Kenya. Clin. Med. Insights Ear Nose Throat 2012, 5, 17–24. [Google Scholar] [CrossRef] [PubMed]
- Park, J.O.; Nam, I.C.; Kim, C.S.; Park, S.J.; Lee, D.H.; Kim, H.B.; Han, K.D.; Joo, Y.H. Sex differences in the prevalence of head and neck cancers: A 10-year follow-up study of 10 million healthy people. Cancers 2022, 14, 2521. [Google Scholar] [CrossRef] [PubMed]
- Jang, W.; Kim, S.; Son, Y.; Kim, S.; Lee, S.; Kim, H.J.; Jo, H.; Park, J.; Lee, K.; Lee, H.; et al. Global, regional, and national burden of pharyngeal cancer and projections to 2050 in 185 countries: A population-based systematic analysis of GLOBOCAN 2022. J. Korean Med. Sci. 2025, 40, e177. [Google Scholar] [CrossRef]
| Overall Group (n = 2229) | |
|---|---|
| Age, years | 65.4 ± 13.4 |
| Male gender | 1413 (63.4) |
| Operator | |
| Experienced | 2092 (93.9) |
| Inexperienced | 137 (6.1) |
| Presence of malignancy | |
| Benign disease | 1360 (61.0) |
| Malignant disease | 869 (39.0) |
| Additional consultation | |
| No consultation | 32 (1.4) |
| Consultation | 40 (1.8) |
| Not applicable | 2157 (96.8) |
| Operator | p-Value | |||
|---|---|---|---|---|
| Inexperienced (n = 137) | Experienced (n = 2092) | |||
| Oral cavity | Normal findings | 137 (100) | 2091 (100) | 1.000 |
| Abnormal findings | 0 (0) | 1 (0) | ||
| Larynx | Normal findings | 137 (100) | 2071 (99) | 0.636 |
| Abnormal findings | 0 (0) | 21 (1) | ||
| Vocal cords | Normal findings | 132 (96) | 2045 (98) | 0.248 |
| Abnormal findings | 5 (4) | 47 (2) | ||
| Total | Normal findings | 132 (96) | 2024 (97) | 0.802 |
| Abnormal findings | 5 (4) | 68 (3) | ||
| Presence of Malignancy | p-Value | |||
|---|---|---|---|---|
| Benign (n = 1360) | Malignant (n = 869) | |||
| Oral cavity | Normal findings | 1360 (100) | 868 (100) | 0.390 |
| Abnormal findings | 0 (0) | 1 (0) | ||
| Larynx | Normal findings | 1354 (100) | 854 (98) | 0.002 |
| Abnormal findings | 6 (0) | 15 (2) | ||
| Vocal cords | Normal findings | 1338 (98) | 839 (96) | 0.005 |
| Abnormal findings | 22 (2) | 30 (4) | ||
| Total | Normal findings | 1334 (98) | 822 (95) | 0.000 |
| Abnormal findings | 26 (2) | 47 (5) | ||
| Variables | Category | Abnormality | Univariate Analysis | ||
|---|---|---|---|---|---|
| None (n = 2156) | Presence (n = 73) | OR (95% CI) | p-Value | ||
| Sex | Female | 802 (98) | 14 (2) | Reference | |
| Male | 1354 (96) | 59 (4) | 2.069 (1.138–3.761) | 0.017 | |
| Age | ≥74 | 560 (98) | 11 (2) | Reference | |
| <74 | 1596 (96) | 62 (4) | 2.404 (1.247–4.634) | 0.009 | |
| Operator | Inexperienced | 132 (96) | 5 (4) | Reference | |
| Experienced | 2024 (97) | 68 (3) | 0.648 (0.251–1.672) | 0.370 | |
| Presence of malignancy | Benign disease | 1334 (98) | 26 (2) | Reference | |
| Malignant disease | 822 (95) | 47 (5) | 3.030 (1.829–5.017) | 0.000 | |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Published by MDPI on behalf of the Lithuanian University of Health Sciences. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kim, D.H.; Kang, B.H.; Um, S.-J.; Kim, I. Diagnostic Value of Bronchoscopy in Detecting Laryngopharyngeal Disorders: Clinical Utility and Limitations. Medicina 2025, 61, 1617. https://doi.org/10.3390/medicina61091617
Kim DH, Kang BH, Um S-J, Kim I. Diagnostic Value of Bronchoscopy in Detecting Laryngopharyngeal Disorders: Clinical Utility and Limitations. Medicina. 2025; 61(9):1617. https://doi.org/10.3390/medicina61091617
Chicago/Turabian StyleKim, Deok Hyong, Bo Hyoung Kang, Soo-Jung Um, and Insu Kim. 2025. "Diagnostic Value of Bronchoscopy in Detecting Laryngopharyngeal Disorders: Clinical Utility and Limitations" Medicina 61, no. 9: 1617. https://doi.org/10.3390/medicina61091617
APA StyleKim, D. H., Kang, B. H., Um, S.-J., & Kim, I. (2025). Diagnostic Value of Bronchoscopy in Detecting Laryngopharyngeal Disorders: Clinical Utility and Limitations. Medicina, 61(9), 1617. https://doi.org/10.3390/medicina61091617






