Comparison of a Subepithelial Connective Tissue Graft and a Xenogeneic Collagen Matrix in Combination with a Coronally Advanced Flap for Gingival Recession Coverage with 12-Month Follow-Up: A Systematic Review and Meta-Analysis
Abstract
1. Introduction
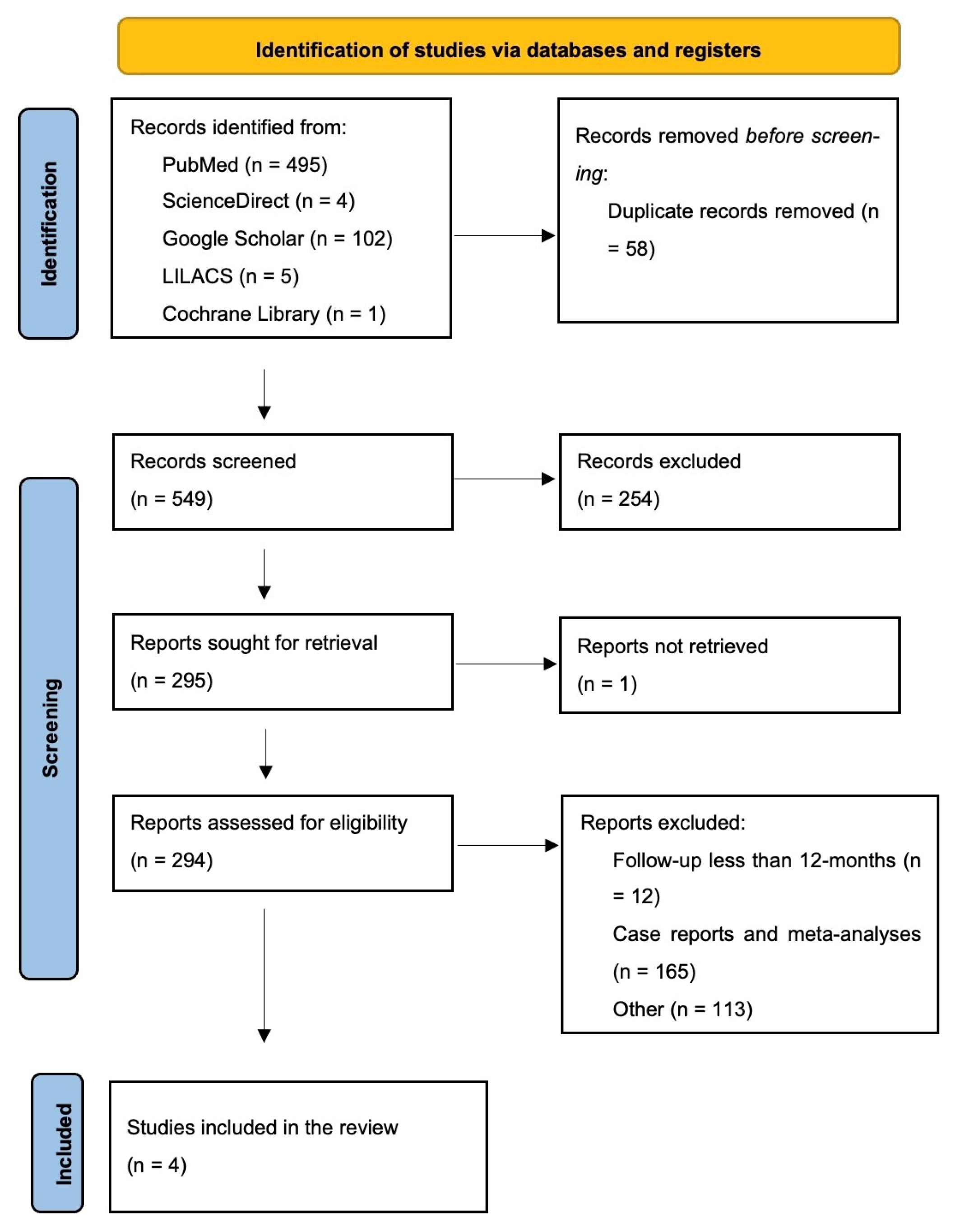
2. Methods
2.1. Protocol and Registration
2.2. Focus Question
2.3. Outcome Variables
- Keratinized tissue width (KTW)
- Clinical attachment level (CAL)
- Gingival recession depth (GRD)
- Complete root coverage (CRC)
- Duration of surgery
- Patient-centered outcomes (esthetics, pain, and satisfaction)
2.4. Type of Publications and Studies
2.5. Information Source
2.6. Search Strategy
2.7. Selection of Studies
2.8. Inclusion Criteria
- (a)
- Randomized controlled clinical trials on humans aged 18 and older.
- (b)
- Use of XCM in the test group and CTG in the control group.
- (c)
- Presentation of sufficient information (KTW, CAL, GR, CRC, surgery time, and patients’ outcomes) on the baseline and at the end of the study.
- (d)
- Comparison of XCM + CAF (test group) vs. CTG + CAF (control group).
- (e)
- Follow-up period of 12 months.
- (f)
- Treatment performed on natural teeth with multiple recessions.
- (g)
- Patients with periodontal and systemic health.
- (h)
- At least 20 patients included in the study.
2.9. Exclusion Criteria
- (a)
- In vitro studies, animal studies, reviews, systematic reviews, meta-analyses, PhD theses, and case reports.
- (b)
- Articles not in English.
- (c)
- Studies lacking comprehensive details.
- (d)
- Follow-up period less than 12 months.
- (e)
- Surgical technique other than CAF.
- (f)
- Use of biomaterials other than XCM.
- (g)
- Treatment performed on implants.
- (h)
- Studies on pregnant or lactating women.
- (i)
- Patients with prior recession treatment in the target area.
- (j)
- Cervical restorations in the teeth under investigation (their presence could interfere with the predictability of the recession root coverage procedure).
2.10. Risk of Bias
2.11. Data Extraction and Collection
- Study details: authors, year, and design.
- Patient characteristics: number, age range of patients, and type/number of treated teeth.
- Clinical outcomes: KTW, CAL, GR, CRC, and surgery time.
- Patient-centered outcomes (esthetics, pain, and discomfort) at baseline and at 12-months of follow-up.
2.12. Data Items
- (a)
- “Author”—name of the first author and year of publication.
- (b)
- “Study design”—type of study conducted.
- (c)
- “Baseline records”—baseline clinical parameters, surgery time and patient-centered outcomes.
- (d)
- “Clinical parameters”—parameters used to evaluate tissues around the teeth with GR: KTW, CAL, GRD, and CRC.
- (e)
- “Patient-centered outcomes”—outcomes related to esthetics, pain, and patient satisfaction.
- (f)
- “Surgery time”—duration of gingival recession coverage.
- (g)
- “Number of patients, Intervention”—number of patients treated, and the treatment protocols used in the test and control groups.
- (h)
- “Follow-up”—duration of follow-up (in months) for both the test and control groups.
- (i)
- “Treatment outcomes”—clinical parameters, surgery time, and patient-centered outcomes with values recorded at baseline and at the end of follow-up (i.e., KTW, CAL, GR, CRC, esthetics, pain, satisfaction, and duration of the surgical procedure of recession coverage).
2.13. Study Design and Characteristics of Patients
2.14. Preoperative Procedures
2.15. Types of Interventions
2.16. Postoperative Care
2.17. Statistical Analysis
3. Results
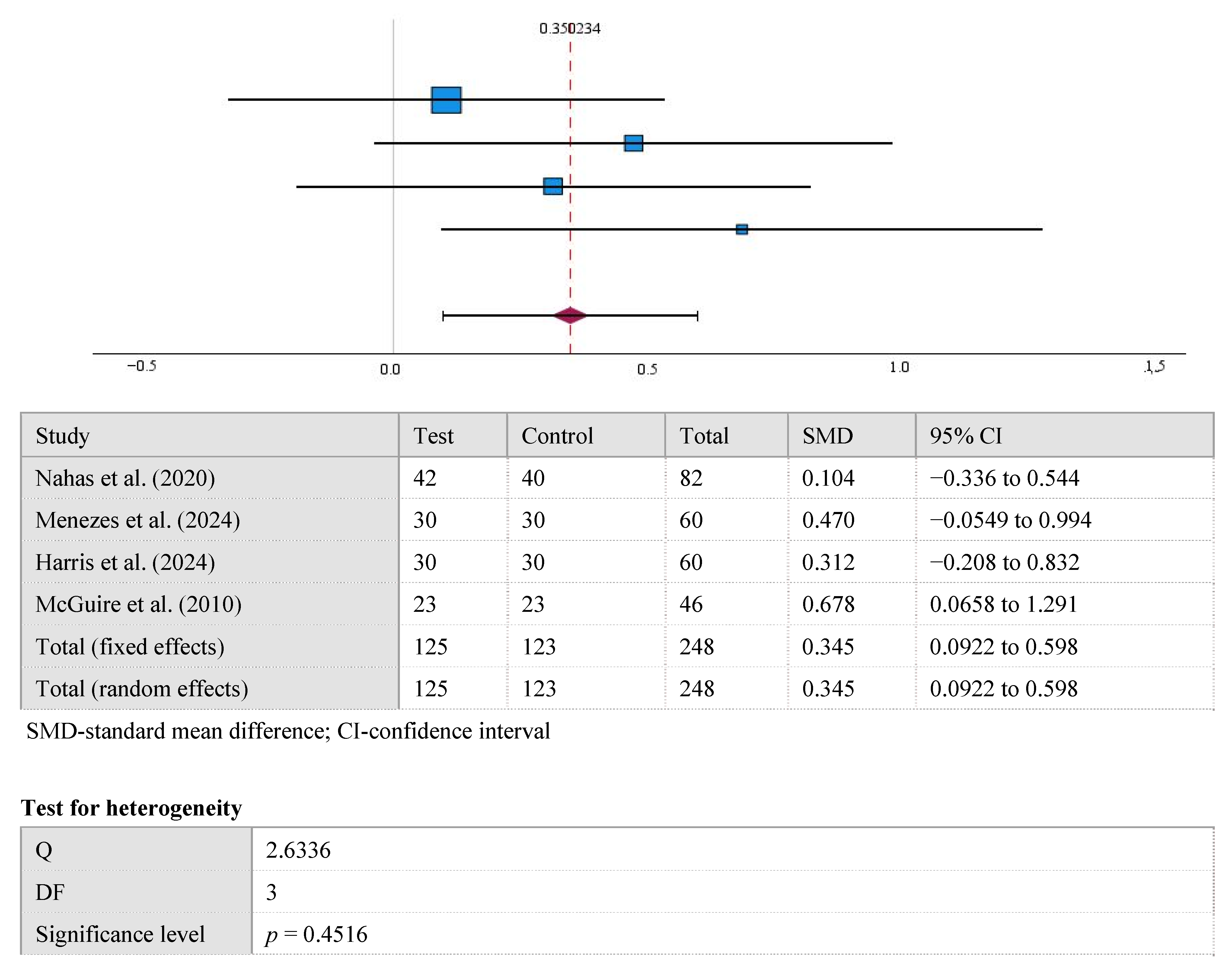
3.1. KTW
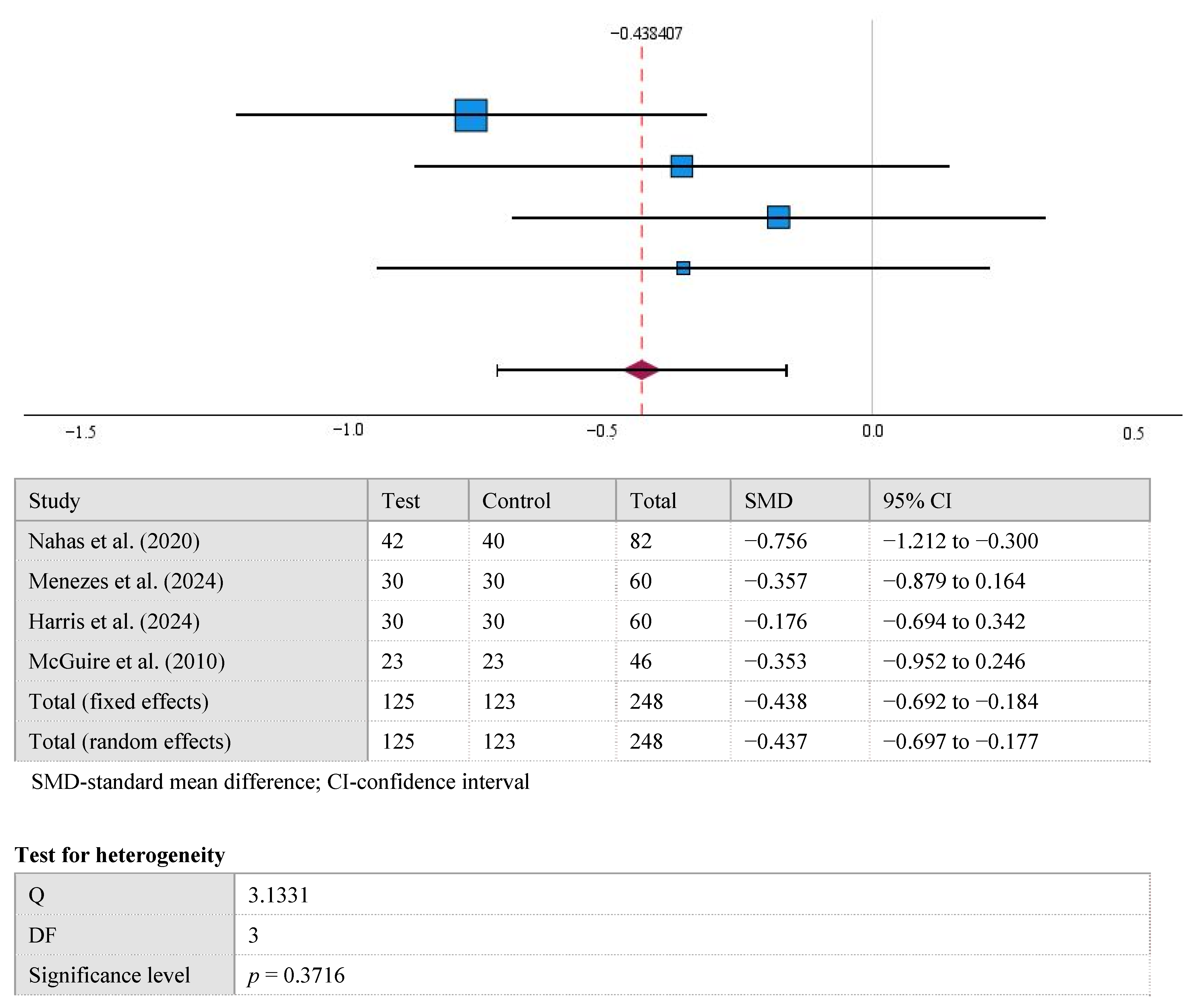
3.2. GR
3.3. CAL
3.4. CRC
3.5. Surgery Time
3.6. Patient-Centered Outcomes
4. Discussion
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Cortellini, P.; Bissada, N.F. Mucogingival conditions in the natural dentition: Narrative review, case definitions, and diagnostic considerations. J. Periodontol. 2018, 89 (Suppl. S1), S204–S213. [Google Scholar] [CrossRef]
- Jati, A.S.; Furquim, L.Z.; Consolaro, A. Gingival recession: Its causes and types, and the importance of orthodontic treatment. Dent. Press J. Orthod. 2016, 21, 18–29. [Google Scholar] [CrossRef] [PubMed]
- Kassab, M.M.; Cohen, R.E. The etiology and prevalence of gingival recession. J. Am. Dent. Assoc. 2003, 134, 220–225. [Google Scholar] [CrossRef]
- Tugnait, A.; Clerehugh, V. Gingival recession—Its significance and management. J. Dent. 2001, 29, 381–394. [Google Scholar] [CrossRef]
- Susin, C.; Haas, A.N.; Oppermann, R.V.; Haugejorden, O.; Albandar, J.M. Gingival recession: Epidemiology and risk indicators in a representative urban Brazilian population. J. Periodontol. 2004, 75, 1377–1386. [Google Scholar] [CrossRef]
- Merijohn, G.K. Management and prevention of gingival recession. Periodontology 2000 2016, 71, 228–242. [Google Scholar] [CrossRef]
- Costa, R.S.; Rios, F.S.; Moura, M.S.; Jardim, J.J.; Maltz, M.; Haas, A.N. Prevalence and risk indicators of dentin hypersensitivity in adult and elderly populations from Porto Alegre, Brazil. J. Periodontol. 2014, 85, 1247–1258. [Google Scholar] [CrossRef]
- Kassab, M.M.; Badawi, H.; Dentino, A.R. Treatment of gingival recession. Dent. Clin. North Am. 2010, 54, 129–140. [Google Scholar] [CrossRef] [PubMed]
- Patel, M.; Nixon, P.J.; Chan, M.F. Gingival recession: Part 1. Aetiology and non-surgical management. Br. Dent. J. 2011, 211, 251–254. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Zegarra-Caceres, L.; Orellano-Merluzzi, A.; Muniz, F.W.M.G.; de Souza, S.L.S.; Faveri, M.; Meza-Mauricio, J. Xenogeneic collagen matrix vs. connective tissue graft for the treatment of multiple gingival recession: A systematic review and meta-analysis. Odontology 2024, 112, 317–340. [Google Scholar] [CrossRef]
- Cairo, F.; Nieri, M.; Pagliaro, U. Efficacy of periodontal plastic surgery procedures in the treatment of localized facial gingival recessions: A systematic review. J. Clin. Periodontol. 2014, 41 (Suppl. S15), S44–S62. [Google Scholar] [CrossRef]
- Thoma, D.S.; Zeltner, M.; Hilbe, M.; Hämmerle, C.H.; Hüsler, J.; Jung, R.E. Randomized controlled clinical study evaluating effectiveness and safety of a volume-stable collagen matrix compared to autogenous connective tissue grafts for soft tissue augmentation at implant sites. J. Clin. Periodontol. 2016, 43, 874–885. [Google Scholar] [CrossRef]
- Amine, K.; El Amrani, Y.; Chemlali, S.; Kissa, J. Alternatives to connective tissue graft in the treatment of localized gingival recessions: A systematic review. J. Stomatol. Oral Maxillofac. Surg. 2018, 119, 25–32. [Google Scholar] [CrossRef]
- AlSarhan, M.A.; Al Jasser, R.; Tarish, M.A.; AlHuzaimi, A.I.; Alzoman, H. Xenogeneic collagen matrix versus connective tissue graft for the treatment of multiple gingival recessions: A systematic review and meta-analysis. Clin. Exp. Dent. Res. 2019, 5, 566–579. [Google Scholar] [CrossRef]
- McGuire, M.K.; Scheyer, E.T. Xenogeneic collagen matrix with coronally advanced flap compared to connective tissue with coronally advanced flap for the treatment of dehiscence-type recession defects. J. Periodontol. 2010, 81, 1108–1117. [Google Scholar] [CrossRef] [PubMed]
- Parashis, A.O.; Kalaitzakis, C.J.; Tatakis, D.N.; Tosios, K. Alveolar ridge preservation using xenogeneic collagen matrix and bone allograft: A case series. Int. J. Dent. 2014, 2014, 172854. [Google Scholar] [CrossRef]
- Stefanini, M.; Jepsen, K.; de Sanctis, M.; Baldini, N.; Greven, B.; Heinz, B.; Wennström, J.; Cassel, B.; Vignoletti, F.; Sanz, M.; et al. Patient-reported outcomes and aesthetic evaluation of root coverage procedures: A 12-month follow-up of a randomized controlled clinical trial. J. Clin. Periodontol. 2016, 43, 1132–1141. [Google Scholar] [CrossRef]
- Jepsen, K.; Jepsen, S.; Zucchelli, G.; Stefanini, M.; de Sanctis, M.; Baldini, N.; Greven, B.; Heinz, B.; Wennström, J.; Cassel, B.; et al. Treatment of gingival recession defects with a coronally advanced flap and a xenogeneic collagen matrix: A multicenter randomized clinical trial. J. Clin. Periodontol. 2013, 40, 82–89. [Google Scholar] [CrossRef] [PubMed]
- Liberati, A.; Altman, D.G.; Tetzlaff, J.; Mulrow, C.; Gøtzsche, P.C.; Ioannidis, J.P.; Clarke, M.; Devereaux, P.J.; Kleijnen, J.; Moher, D. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate healthcare interventions: Explanation and elaboration. BMJ 2009, 339, b2700. [Google Scholar] [CrossRef]
- Rios, L.P.; Ye, C.; Thabane, L. Association between framing of the research question using the PICOT format and reporting quality of randomized controlled trials. BMC Med. Res. Methodol. 2010, 10, 11. [Google Scholar] [CrossRef] [PubMed]
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. BMJ 2021, 372, n71. [Google Scholar] [CrossRef]
- Nahas, R.; Gondim, V.; Carvalho, C.V.; Calderero, L.M.; Rosa, E.F.; Sakiyama, T.; Neto, J.B.C.; Pannuti, C.M.; Romito, G.A. Treatment of multiple recessions with collage matrix versus connective tissue: A randomized clinical trial. Braz. Oral Res. 2020, 33, e123. [Google Scholar] [CrossRef] [PubMed]
- Menezes, K.M.; Borges, S.B.; Medeiros, I.; Gomes, G.E.S.; Roncalli, A.G.; Gurgel, B.C.V. Efficacy of xenogeneic collagen matrix in the treatment of gingival recessions: A controlled clinical trial. Braz. Oral Res. 2024, 38, e111. [Google Scholar] [CrossRef] [PubMed]
- Harris, J.J.; Navya, P.D.; Rajasekar, A. Efficacy of Fibro-Gide® in coronally advanced flap for the treatment of multiple gingival recession: A prospective clinical study. J. Int. Oral Health 2024, 16, 145–149. [Google Scholar] [CrossRef]
- Higgins, J.P.T.; Green, S. (Eds.) Cochrane Handbook for Systematic Reviews of Interventions; Wiley-Blackwell: Chichester, UK, 2008. [Google Scholar] [CrossRef]
- Fageeh, H.I.; Fageeh, H.N.; Bhati, A.K.; Thubab, A.Y.; Sharrahi, H.M.H.; Aljabri, Y.S.; Alotaibi, F.I. Assessing the reliability of Miller’s classification and Cairo’s classification in classifying gingival recession defects: A comparison study. Medicina 2024, 60, 205. [Google Scholar] [CrossRef]
- Cairo, F.; Nieri, M.; Cincinelli, S.; Mervelt, J.; Pagliaro, U. The interproximal clinical attachment level to classify gingival recessions and predict root coverage outcomes: An explorative and reliability study. J. Clin. Periodontol. 2011, 38, 661–666. [Google Scholar] [CrossRef]
- Cohen, J. Statistical Power Analysis for the Behavioral Sciences, 2nd ed.; Lawrence Erlbaum Associates: Hillsdale, NJ, USA, 1988. [Google Scholar]
- Pini-Prato, G.; Magnani, C.; Zaheer, F.; Buti, J.; Rotundo, R. Critical evaluation of complete root coverage as a successful endpoint of treatment for gingival recessions. Int. J. Periodontics Restor. Dent. 2015, 35, 655–663. [Google Scholar] [CrossRef]
- Matoh, U.; Petelin, M.; Gašperšič, R. Split-mouth comparison of coronally advanced flap with connective tissue graft or collagen matrix for treatment of isolated gingival recessions. Int. J. Periodontics Restor. Dent. 2019, 39, 439–446. [Google Scholar] [CrossRef]
- Cardaropoli, D.; Tamagnone, L.; Roffredo, A.; Gaveglio, L. Treatment of gingival recession defects using coronally advanced flap with a porcine collagen matrix compared to coronally advanced flap with connective tissue graft: A randomized controlled clinical trial. J. Periodontol. 2012, 83, 321–328. [Google Scholar] [CrossRef]
- Ashurko, I.; Tarasenko, S.; Esayan, A.; Kurkov, A.; Mikaelyan, K.; Balyasin, M.; Galyas, A.; Kustova, J.; Taschieri, S.; Corbella, S. Connective tissue graft versus xenogeneic collagen matrix for soft tissue augmentation at implant sites: A randomized-controlled clinical trial. Clin. Oral Investig. 2022, 26, 7191–7208. [Google Scholar] [CrossRef]
- Tavelli, L.; Barootchi, S.; Nguyen, T.V.N.; Tattan, M.; Ravidà, A.; Wang, H.-L. Efficacy of tunnel technique in the treatment of localized and multiple gingival recessions: A systematic review and meta-analysis. J. Periodontol. 2018, 89, 1075–1090. [Google Scholar] [CrossRef] [PubMed]
- Cieślik-Wegemund, M.; Wierucka-Młynarczyk, B.; Tanasiewicz, M.; Gilowski, Ł. Tunnel technique with collagen matrix compared with connective tissue graft for treatment of periodontal recession: A randomized clinical trial. J. Periodontol. 2016, 87, 1436–1443. [Google Scholar] [CrossRef]
- Jepsen, K.; Stefanini, M.; Sanz, M.; Zucchelli, G.; Jepsen, S. Long-term stability of root coverage by coronally advanced flap procedures. J. Periodontol. 2017, 88, 626–633. [Google Scholar] [CrossRef]
- Harris, R.J. A short-term and long-term comparison of root coverage with an acellular dermal matrix and a subepithelial graft. J. Periodontol. 2004, 75, 734–743. [Google Scholar] [CrossRef]
- Tonetti, M.S.; Cortellini, P.; Pellegrini, G.; Nieri, M.; Bonaccini, D.; Allegri, M.; Bouchard, P.; Cairo, F.; Conforti, G.; Fourmousis, I.; et al. Xenogenic collagen matrix or autologous connective tissue graft as adjunct to coronally advanced flaps for coverage of multiple adjacent gingival recession: Randomized trial assessing non-inferiority in root coverage and superiority in oral health-related quality of life. J. Clin. Periodontol. 2018, 45, 78–88. [Google Scholar] [CrossRef] [PubMed]
- Kumar, P.M.; Nagate, R.R.; Chaturvedi, S.; Al-Ahmari, M.M.M.; Al-Qarni, M.A.; Gokhale, S.T.; Ahmed, A.R.; Al Bariqi, A.; Cicciù, M.; Minervini, G. Importance of periodontal phenotype in periodontics and restorative dentistry: A systematic review. BMC Oral Health 2024, 24, 41. [Google Scholar] [CrossRef] [PubMed]

| Component | Description |
|---|---|
| Population (P) | Adult patients diagnosed with multiple gingival recessions undergoing root coverage treatments |
| Intervention (I) | Soft tissue augmentation using XCM |
| Comparison (C) | Soft tissue augmentation using CTG |
| Outcome (O) | Primary: KTW, GR, CAL, and CRC Secondary: patient complaints, discomfort, overall satisfaction, and surgery time |
| Time (T) | 12 months after surgery |
| Search # | Search Words |
|---|---|
| 1 | “Collagen matrix” [All Fields] OR “Xenogeneic collagen matrix” [All Fields] OR “CM” [All Fields] OR “XCM” [All Fields] |
| 2 | “Connective tissue graft” [All Fields] OR “CTG” [All Fields] OR “Subepithelial connective tissue graft” [All Fields] OR “SCTG” [All Fields] OR “Palatal connective tissue graft” [All Fields] |
| 3 | “Coronally advanced flap” [All Fields] OR “CAF” [All Fields] |
| 4 | “Multiple recessions” [All Fields] OR “Bilateral recessions” [All Fields] OR “Recessions” [All Fields] OR “RT1 recessions” [All Fields] OR “Miller’s Class 1” [All Fields] OR “RT2 recessions” [All Fields] OR “Miller’s Class 2” [All Fields] |
| 5 | #1 AND #2 AND #3 AND #4 |
| Study | Random Sequence Generation | Allocation Concealment | Blinding of Outcome Assessment | Incomplete Outcome Data | Selective Reporting | Other Sources of Bias |
|---|---|---|---|---|---|---|
| Nahas et al. (2020) [22] | + | + | + | + | + | + |
| Menezes et al. (2024) [23] | + | ? | + | + | + | + |
| Harris et al. (2024) [24] | + | ? | ? | + | + | + |
| McGuire et al. (2010) [15] | + | + | + | + | + | + |
| Study | N—Number of Patients, n—Total Number of Treated Teeth (Test/Control), Type of Teeth | Age of Patients Mean Age (SD) | Patient-Centered Outcomes | Clinical Parameters Investigated |
|---|---|---|---|---|
| Nahas et al. (2020) [22] | N = 15 n = 82 (42/40) Maxillary 100% (canines, first and second premolars) | 32.7 (8.1) | Postoperative pain, DH (VAS) | GRD, KTW, CAL, CRC, PD, Surgery time |
| Menezes et al. (2024) [23] | N = 30 n = 60 (30/30) Maxillary 100% (canines, first and second premolars) | 30.3 (6) | Quality of life (physical, social, and psychological domains) (OHRQoL) | GRD, PD, CAL, BOP, CRC, GT, KTW, Surgery time |
| Harris et al. (2024) [24] | N = 30 n = 60 (30/30) Not specified | 34.8 (6.2) | Pain sensitivity (VAS) | GRD, PD, CAL, GRW, KTW, Surgery time |
| McGuire et al. (2010) [15] | N = 23 n = 46 (23/23) Not specified | 43.7 (12) | Discomfort assessment (ANCOVA) | GRD, CAL, KTW, PD, GRW, BOP, CRC |
| Studies | Prescribed Anti-Inflammatory Drugs | Prescribed Antibiotics |
|---|---|---|
| Nahas et al. (2020) [22] | 100 mg nimesulide (twice a day for 3 days) | - |
| Harris et al. (2024) [24] | Zerodol-SP (twice a day for 3 days) | 500 mg amoxicillin twice daily for 3 days |
| Menezes et al. (2024) [23] | 100 mg nimesulide (every 12 h for 3 days), 500 mg dipyrone (every 6 h for 3 days) | 500 mg amoxicillin (every 8 h for 1 day) |
| McGuire et al. (2010) [15] | ibuprofen or hydrocodone | 100 mg doxycycline daily (for 10 days)/amoxicillin (for 7 days) |
| Study | Clinical Parameters at Baseline (Test vs. Control) Mean (SD) | Clinical Parameters After 12 Months (Test vs. Control) Mean (SD) | Operating Time (Test vs. Control) Mean (SD) | Patient-Centered Outcomes (Test vs. Control) Mean (SD) |
|---|---|---|---|---|
| Nahas et al. (2020) [22] | KTW: 2.2 (1.0) vs. 2.1 (1.0) GR: 2.7 (1.1) vs. 2.8 (1.1) CAL: 3.8 (1.1) vs. 4.0 (1.2) | KTW: 2.5 (0.7) vs. 3.2 (1.1) * GR: 0.6 (1.0) vs. 0.5 (0.9) CAL: 1.9 (1.0) vs. 2.2 (1.2) CRC: 60% vs. 68% | 31.3 (4.3) vs. 47.7 (6.1) * | Postoperative pain: 1.34 (1.63) vs. 2.73 (2.39) * DH: 2.4 (3.6) vs. 2.1 (3.2) |
| Menezes et al. (2024) [23] | KTW: 3.3 (1.3) vs. 3.3 (1.42) GR: 2.4 (0.98) vs. 2.7 (1.24) CAL: 3.9 (1.29) vs. 4.2 (1.45) | KTW: 4 (1.34) vs. 4.5 (1.42) GR: 0.62 (0.79) vs. 0.3 (0.53) CAL: 1.9 (0.86) vs. 2 (1.10) CRC: 66.7% vs. 70% | 45.6 (6.9) vs. 75.5 (11.4) * | Not specified by control and test group Physical domains (t0–t12): 21.3 (0.88)–27.6 (0.51) * Social domains (t0–t12): 18.5 (0.82)–22.4 (0.37) * Psychological domains (t0–t12): 18.1 (0.84)–22.2 (0.42) * |
| Harris et al. (2024) [24] | KTW: 2.2 (0.2) vs. 2.1 (0.2) GR: 3.4 (0.8) vs. 3.5 (0.8) CAL: 5.4 (1.03) vs. 5.4 (1.02) | KTW: 3.2 (0.8) vs. 3.9 (5.5) * GR: 0.3 (0.4) vs. 0.2 (0.2) CAL: 2.4 (0.7) vs. 2.3 (0.7) | Not specified but mentioned that in the test group, the duration of surgery was reduced. | Fewer pain reports in the test group. Reported decrease in dental hypersensitivity after intervention in both groups. |
| McGuire et al. 2010) [15] | KTW: 2.44 (1.02) vs. 2.78 (1.35) GR: 3.14 (0.23) vs. 3.20 (0.35) CAL: 4.40 (0.61) vs. 4.50 (0.61) | KTW: 3.59 (1.04) vs. 3.98 (1.13) GR: 0.37 (0.71) vs. 0.02 (0.1) * CAL: 2.13 (0.90) vs. 1.63 (0.54) * CRC: 88.5% vs. 99.3% * | Not mentioned | Postoperative pain: After 1 week 8 vs. 9 + 3 (donor site); equivalent pain—6 * After 4 weeks 3 vs. 7 + 5 (donor site); equivalent pain—10 * |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Published by MDPI on behalf of the Lithuanian University of Health Sciences. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Pranckevičienė, A.; Chuiko, E.; Vaitkevičienė, I.; Anužytė, R.; Mačiulskienė-Visockienė, V. Comparison of a Subepithelial Connective Tissue Graft and a Xenogeneic Collagen Matrix in Combination with a Coronally Advanced Flap for Gingival Recession Coverage with 12-Month Follow-Up: A Systematic Review and Meta-Analysis. Medicina 2025, 61, 1596. https://doi.org/10.3390/medicina61091596
Pranckevičienė A, Chuiko E, Vaitkevičienė I, Anužytė R, Mačiulskienė-Visockienė V. Comparison of a Subepithelial Connective Tissue Graft and a Xenogeneic Collagen Matrix in Combination with a Coronally Advanced Flap for Gingival Recession Coverage with 12-Month Follow-Up: A Systematic Review and Meta-Analysis. Medicina. 2025; 61(9):1596. https://doi.org/10.3390/medicina61091596
Chicago/Turabian StylePranckevičienė, Alma, Ekaterina Chuiko, Inga Vaitkevičienė, Rugilė Anužytė, and Vita Mačiulskienė-Visockienė. 2025. "Comparison of a Subepithelial Connective Tissue Graft and a Xenogeneic Collagen Matrix in Combination with a Coronally Advanced Flap for Gingival Recession Coverage with 12-Month Follow-Up: A Systematic Review and Meta-Analysis" Medicina 61, no. 9: 1596. https://doi.org/10.3390/medicina61091596
APA StylePranckevičienė, A., Chuiko, E., Vaitkevičienė, I., Anužytė, R., & Mačiulskienė-Visockienė, V. (2025). Comparison of a Subepithelial Connective Tissue Graft and a Xenogeneic Collagen Matrix in Combination with a Coronally Advanced Flap for Gingival Recession Coverage with 12-Month Follow-Up: A Systematic Review and Meta-Analysis. Medicina, 61(9), 1596. https://doi.org/10.3390/medicina61091596







