The Differences Between Intraoperative- and Postoperative-Preferred Music Effects on Emergence Delirium in Elderly Patients: A Single-Center, Prospective Randomized Controlled Trial
Abstract
1. Introduction
2. Materials and Methods
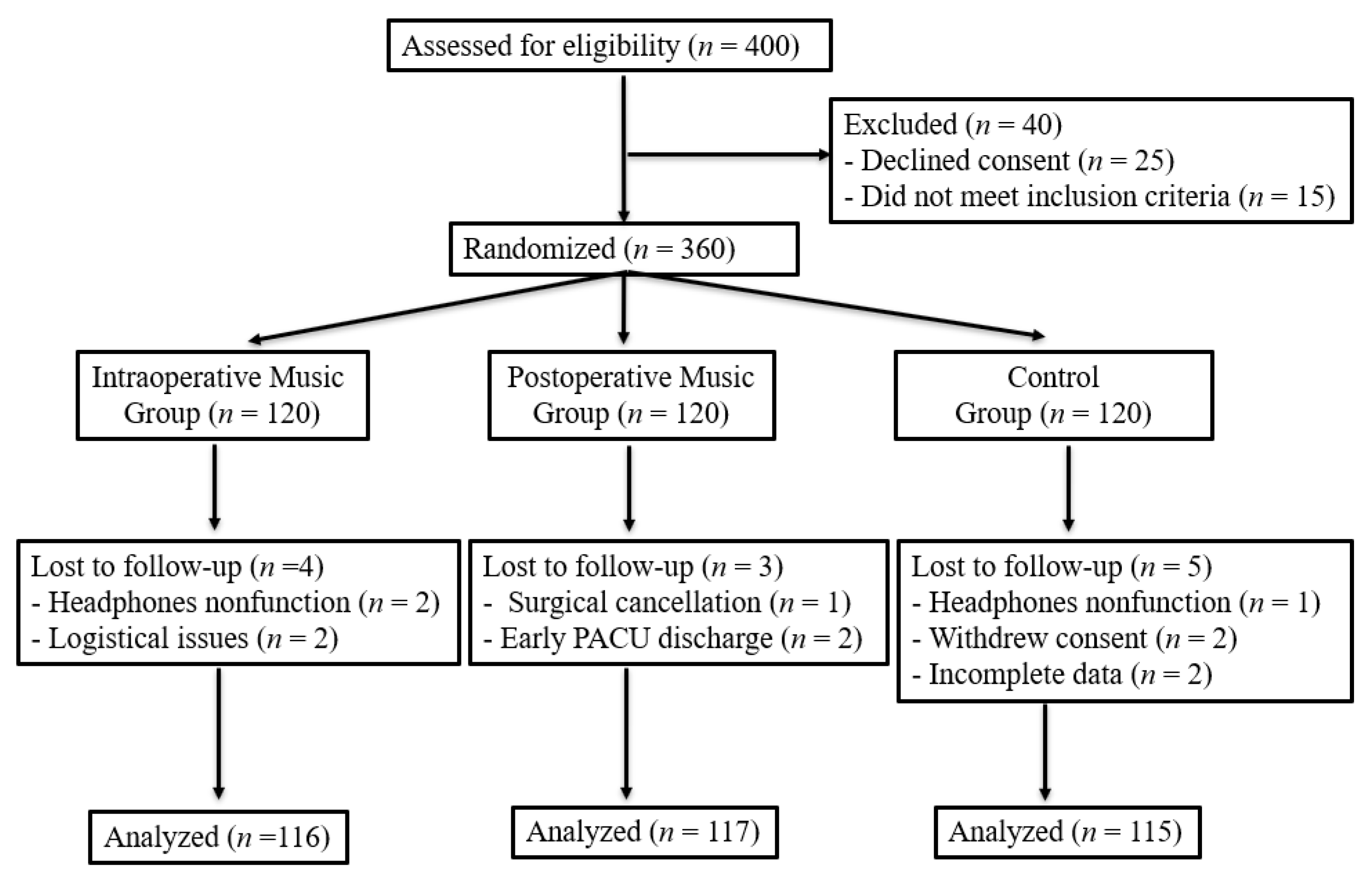
2.1. Study Design and Participants
2.2. Randomization and Blinding
2.3. Interventions
2.4. Outcome Measures
2.5. Sample Size and Statistical Analysis
3. Results
3.1. Baseline Characteristics
3.1.1. Primary Outcome: Incidence and Severity of Emergence Delirium
3.1.2. Secondary Outcomes: Duration of Emergence Delirium, Pain, and Satisfaction
3.1.3. Hemodynamic Parameters and Adverse Events
3.2. Predictors and Subgroup Analysis
3.3. Sensitivity Analysis
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| ED | Emergence Delirium |
| RASS | Richmond Agitation–Sedation Scale |
| VAS | Visual Analogue Scale |
| STAI-S | State–Trait Anxiety Inventory-State |
| PACU | Post-Anesthesia Care Unit |
| ASA | American Society of Anesthesiologists |
| MMSE | Mini-Mental State Examination |
| BIS | Bispectral Index |
| IRB | Institutional Review Board |
| ITT | Intention To Treat |
| PP | Per-Protocol |
| ANOVA | Analysis of Variance |
| BMI | Body Mass Index |
| MAP | Mean Arterial Pressure |
| HR | Heart Rate |
| OR | Odds Ratio |
| CI | Confidence Interval |
| RR | Risk Ratio |
| EEG | Electroencephalogram |
| dB | Decibels |
References
- Lepouse, C.; Lautner, C.; Liu, L.; Gomis, P.; Leon, A. Emergence delirium in adults in the post-anaesthesia care unit. Br. J. Anaesth. 2006, 96, 747–753. [Google Scholar] [CrossRef] [PubMed]
- Card, E.; Pandharipande, P.; Tomes, C.; Lee, C.; Wood, J.; Nelson, D.; Graves, A.; Shintani, A.; Ely, E.W.; Hughes, C. Emergence from general anaesthesia and evolution of delirium signs in the post-anaesthesia care unit. Br. J. Anaesth. 2015, 115, 411–417. [Google Scholar] [CrossRef] [PubMed]
- Ni, K.; Zhu, J.; Ma, Z. Preoperative anxiety and postoperative adverse events: A narrative overview. Anesthesiol. Perioper. Sci. 2023, 1, 23. [Google Scholar] [CrossRef]
- Yu, D.; Chai, W.; Sun, X.; Yao, L. Emergence agitation in adults: Risk factors in 2,000 patients. Can. J. Anesth. 2010, 57, 843. [Google Scholar] [CrossRef] [PubMed]
- Johnson, K.; Fleury, J.; McClain, D. Music intervention to prevent delirium among older patients admitted to a trauma intensive care unit and a trauma orthopaedic unit. Intensive Crit. Care Nurs. 2018, 47, 7–14. [Google Scholar] [CrossRef] [PubMed]
- Xiao, M.; Gong, C.; Mai, M.; Huang, M.; Xiong, A.; Liu, H.; Jiang, R. Efficacy and safety of music therapy for the treatment of anxiety and delirium in ICU patients: A meta-analysis and systematic review of randomized controlled trials. Minerva Anestesiol. 2024, 90, 439–451. [Google Scholar] [CrossRef] [PubMed]
- Park, S.; Williams, R.A.; Lee, D. Effect of preferred music on agitation after traumatic brain injury. West. J. Nurs. Res. 2016, 38, 394–410. [Google Scholar] [CrossRef] [PubMed]
- Hole, J.; Hirsch, M.; Ball, E.; Meads, C. Music as an aid for postoperative recovery in adults: A systematic review and meta-analysis. Lancet 2015, 386, 1659–1671. [Google Scholar] [CrossRef]
- Caponnetto, P.; LaMattina, G.; Quattropani, M.C. Music therapy and psychological-clinical impact in surgery: A systematic review. Health Psychol. Res. 2022, 10, 38615. [Google Scholar] [CrossRef] [PubMed]
- Muzzi, E.; Ronfani, L.; Bossini, B.; Lezcano, C.; Orzan, E.; Barbi, E. Effects of intraoperative auditory stimulation on pain and agitation on awakening after pediatric adenotonsillectomy: A randomized clinical trial. JAMA Otolaryngol.—Head Neck Surg. 2021, 147, 638–645. [Google Scholar] [CrossRef] [PubMed]
- Golubovic, J.; Neerland, B.E.; Aune, D.; Baker, F.A. Music interventions and delirium in adults: A systematic literature review and meta-analysis. Brain Sci. 2022, 12, 568. [Google Scholar] [CrossRef] [PubMed]
- Xin, Y.; Lin, F.C.; Huang, C.; He, B.; Yan, Y.L.; Wang, S.; Zhang, G.M.; Li, R. Nurse anesthetists’ perceptions and experiences of managing emergence delirium: A qualitative study. World J. Psychiatry 2024, 14, 553–562. [Google Scholar] [CrossRef] [PubMed]
- Vetter, T.R.; Ivankova, N.V.; Pittet, J.-F. Patient satisfaction with anesthesia: Beauty is in the eye of the consumer. Anesthesiology 2013, 119, 245–247. [Google Scholar] [CrossRef] [PubMed]
- Bringman, H.; Giesecke, K.; Thörne, A.; Bringman, S. Relaxing music as pre-medication before surgery: A randomised controlled trial. Acta Anaesthesiol. Scand. 2009, 53, 759–764. [Google Scholar] [CrossRef] [PubMed]
- Inouye, S.K.; Westendorp, R.G.; Saczynski, J.S. Delirium in elderly people. Lancet 2014, 383, 911–922. [Google Scholar] [CrossRef] [PubMed]
- Fu, V.X.; Lagarde, S.M.; Favoccia, C.T.; Heisterkamp, J.; van Oers, A.E.; Coene, P.L.O.; Koopman, J.S.H.A.; van den Berg, S.A.A.; Dik, W.A.; Jeekel, J.; et al. Intraoperative music to promote patient outcome (IMPROMPTU): A double-blind randomized controlled trial. J. Surg. Res. 2024, 296, 291–301. [Google Scholar] [CrossRef]
- Bradt, J.; Dileo, C.; Shim, M. Music interventions for preoperative anxiety. Cochrane Database Syst. Rev. 2013, 2013, CD006908. [Google Scholar] [CrossRef] [PubMed]
- Sessler, C.N.; Gosnell, M.S.; Grap, M.J.; Brophy, G.M.; O’Neal, P.V.; Keane, K.A.; Tesoro, E.P.; Elswick, R.K. The Richmond Agitation–Sedation Scale: Validity and reliability in adult intensive care unit patients. Am. J. Respir. Crit. Care Med. 2002, 166, 1338–1344. [Google Scholar] [CrossRef] [PubMed]
| Variable | Intraoperative Music Group (n = 116) | Postoperative Music Group (n = 117) | Control Group (n = 115) | p-Value |
|---|---|---|---|---|
| Age (years) | 72.1 ± 5.7 | 72.6 ± 6.0 | 72.5 ± 5.8 | 0.88 |
| Sex (F/M) | 68/48 | 66/51 | 68/47 | 0.92 |
| BMI (kg/m2) | 23.8 ± 3.4 | 24.0 ± 3.6 | 23.7 ± 3.5 | 0.81 |
| ASA (I/II/III) | 29/58/29 | 31/57/29 | 28/58/29 | 0.97 |
| Surgery type | 0.91 | |||
| Orthopedic surgery | 39 (33.6) | 37 (31.6) | 35 (30.4) | |
| Other | 77 (66.4) | 80 (68.4) | 80 (69.6) | |
| MMSE Score | 25.7 ± 2.6 | 25.5 ± 2.8 | 25.6 ± 2.7 | 0.89 |
| STAI-S Score | 43.4 ± 9.0 | 43.0 ± 9.2 | 43.2 ± 9.1 | 0.94 |
| Preferred music genre | 0.99 | |||
| Classical | 58 (50.0) | 59 (50.4) | 57 (49.6) | |
| Ambient | 35 (30.2) | 35 (29.9) | 34 (29.6) | |
| Jazz | 17 (14.7) | 18 (15.4) | 17 (14.8) | |
| Other | 6 (5.2) | 5 (4.3) | 7 (6.1) |
| Outcome | Intraoperative Music Group (n = 120) | Postoperative Music Group (n = 120) | Control Group (n = 120) | p-Value (Adjusted p-Value) |
|---|---|---|---|---|
| ED Incidence (RASS ≥ +1) | 16 (13.8%) * | 22 (18.8%) * | 33 (28.7%) | 0.00 (N/A) |
| ED Severity (RASS) | 1.3 ± 0.5 * | 1.5 ± 0.6 | 1.8 ± 0.7 | 0.00 (0.00) |
| ED Duration (min) | 18.4 ± 7.0 | 15.2 ± 6.1 *† | 22.5 ± 8.3 | 0.00 (0.00) |
| Pain Score (VAS, 0–10) | 3.5 ± 1.5 | 3.0 ± 1.4 *† | 4.2 ± 1.7 | 0.00 (0.00) |
| Satisfaction (1–5) | 4.2 ± 0.8 * | 4.4 ± 0.7 * | 3.6 ± 0.9 | 0.00 (0.00) |
| MAP (mmHg, PACU 60 min) | 84.8 ± 9.5 | 85.3 ± 9.2 | 84.1 ± 10.1 | 0.72 (0.72) |
| HR (bpm, PACU 60 min) | 71.2 ± 8.3 | 72.0 ± 8.7 | 73.1 ± 9.0 | 0.65 (0.65) |
| Adverse Events (Postoperative Nausea/Vomiting) | 5 (4.3%) | 4 (3.4%) | 6 (5.2%) | 0.81 (N/A) |
| Fentanyl Use (0.5 µg/kg) | 16 (13.8%) * | 14 (12.0%) * | 26 (22.6%) | 0.02 (N/A) |
| Variable | OR (95% CI) | p-Value |
|---|---|---|
| Age (years) | 1.02 (0.98, 1.06) | 0.31 |
| Sex (Female vs. Male) | 1.15 (0.78, 1.70) | 0.48 |
| BMI (kg/m2) | 0.99 (0.93, 1.05) | 0.71 |
| MMSE Score | 0.97 (0.90, 1.04) | 0.39 |
| Preoperative STAI-S Score | 1.06 (1.02, 1.10) * | 0.01 |
| Orthopedic | 1.12 (0.72, 1.74) | 0.62 |
| Other | 0.95 (0.58, 1.56) | 0.84 |
| Intraoperative Music | 0.45 (0.28, 0.72) * | 0.00 |
| Postoperative Music | 0.62 (0.40, 0.95) * | 0.03 |
| Music × STAI-S Interaction | 0.90 (0.84, 0.97) * | 0.03 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Published by MDPI on behalf of the Lithuanian University of Health Sciences. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lee, H.; Park, E.; Kim, B.; Lee, C. The Differences Between Intraoperative- and Postoperative-Preferred Music Effects on Emergence Delirium in Elderly Patients: A Single-Center, Prospective Randomized Controlled Trial. Medicina 2025, 61, 1586. https://doi.org/10.3390/medicina61091586
Lee H, Park E, Kim B, Lee C. The Differences Between Intraoperative- and Postoperative-Preferred Music Effects on Emergence Delirium in Elderly Patients: A Single-Center, Prospective Randomized Controlled Trial. Medicina. 2025; 61(9):1586. https://doi.org/10.3390/medicina61091586
Chicago/Turabian StyleLee, Hayoung, Eunsung Park, Byoungryun Kim, and Cheol Lee. 2025. "The Differences Between Intraoperative- and Postoperative-Preferred Music Effects on Emergence Delirium in Elderly Patients: A Single-Center, Prospective Randomized Controlled Trial" Medicina 61, no. 9: 1586. https://doi.org/10.3390/medicina61091586
APA StyleLee, H., Park, E., Kim, B., & Lee, C. (2025). The Differences Between Intraoperative- and Postoperative-Preferred Music Effects on Emergence Delirium in Elderly Patients: A Single-Center, Prospective Randomized Controlled Trial. Medicina, 61(9), 1586. https://doi.org/10.3390/medicina61091586








