Determinants of Diabetes-Related Quality of Life in Saudi Arabia: A Nationwide Survey-Based Assessment of Demographic, Health, and Complication-Related Influences
Abstract
1. Introduction
2. Method
2.1. Study Design
2.2. Sample Size
2.3. Procedures
2.4. Measures
2.5. Statistical Analysis
3. Results
3.1. Sample’s Characteristics
3.2. Unadjusted Associations of the DQoL with Demographic and Socioeconomic Factors, Access to Health Care, Health Behaviors, Diabetes-Related Factors, Comorbidities, and Diabetes Management
3.3. Adjusted Associations of the DQoL with Demographic and Socioeconomic Factors, Access to Health Care, Health Behaviors, Diabetes-Related Factors, Comorbidities, and Diabetes Management
4. Discussion
5. Limitations
6. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Committee ADAPP. 2. Diagnosis and Classification of Diabetes: Standards of Care in Diabetes—2024. Diabetes Care 2023, 47, S20. [Google Scholar] [CrossRef] [PubMed]
- Abdul Basith Khan, M.; Hashim, M.J.; King, J.K.; Govender, R.D.; Mustafa, H.; Al Kaabi, J. Epidemiology of Type 2 Diabetes—Global Burden of Disease and Forecasted Trends. J. Epidemiol. Glob. Health 2020, 10, 107. [Google Scholar] [CrossRef] [PubMed]
- Ong, K.L.; Stafford, L.K.; McLaughlin, S.A.; Boyko, E.J.; Vollset, S.E.; Smith, A.E.; Dalton, B.E.; Duprey, J.; Cruz, J.A.; Hagins, H.; et al. Global, regional, and national burden of diabetes from 1990 to 2021, with projections of prevalence to 2050: A systematic analysis for the Global Burden of Disease Study 2021. Lancet 2023, 402, 203–234. [Google Scholar] [CrossRef] [PubMed]
- Jarrar, M.T.; Abusalah, M.A.; Albaker, W.; Al-Bsheish, M.; Alsyouf, A.; Al-Mugheed, K.; Issa, M.R.; Alumran, A. Prevalence of Type 2 Diabetes Mellitus in the General Population of Saudi Arabia, 2000–2020: A Systematic Review and Meta-Analysis of Observational Studies. Saudi J. Med. Med. Sci. 2023, 11, 1. [Google Scholar] [CrossRef]
- Debono, M.; Cachia, E. The impact of diabetes on psychological well being and quality of life. The role of patient education. Psychol. Health Med. 2007, 12, 545–555. [Google Scholar] [CrossRef]
- Gebremariam, G.T.; Biratu, S.; Alemayehu, M.; Welie, A.G.; Sander, B.; Gebretekle, G.B. Health-related quality of life of patients with type 2 diabetes mellitus at a tertiary care hospital in Ethiopia. PLoS ONE 2022, 17, e0264199. [Google Scholar] [CrossRef]
- Oluchi, S.E.; Manaf, R.A.; Ismail, S.; Kadir Shahar, H.; Mahmud, A.; Udeani, T.K. Health Related Quality of Life Measurements for Diabetes: A Systematic Review. Int. J. Environ. Res. Public Health 2021, 18, 9245. [Google Scholar] [CrossRef]
- Wong, E.L.; Xu, R.H.; Cheung, A.W. Measurement of health-related quality of life in patients with diabetes mellitus using EQ-5D-5L in Hong Kong, China. Qual. Life Res. 2020, 29, 1913–1921. [Google Scholar] [CrossRef]
- Redekop, W.K.; Koopmanschap, M.A.; Stolk, R.P.; Rutten, G.E.; Wolffenbuttel, B.H.; Niessen, L.W. Health-Related Quality of Life and Treatment Satisfaction in Dutch Patients with Type 2 Diabetes. Diabetes Care 2002, 25, 458–463. [Google Scholar] [CrossRef]
- AlSufyani, M.H.; Alzahrani, A.M.; Allah, A.A.; Abdullah, R.I.; Alzhrani, S.H.; Alsaab, A.A. Prevalence of painful diabetic peripheral neuropathy and its impact on quality of life among diabetic patients in Western region, Saudi Arabia. J. Fam. Med. Prim. Care 2020, 9, 4897. [Google Scholar] [CrossRef]
- Fanelli, E.; Abate Daga, F.; Pappaccogli, M.; Eula, E.; Astarita, A.; Mingrone, G.; Fasano, C.; Magnino, C.; Schiavone, D.; Rabbone, I.; et al. A structured physical activity program in an adolescent population with overweight or obesity: A prospective interventional study. Appl. Physiol. Nutr. Metab. 2022, 47, 253–260. [Google Scholar] [CrossRef]
- Schranz, N.; Tomkinson, G.; Parletta, N.; Petkov, J.; Olds, T. Can resistance training change the strength, body composition and self-concept of overweight and obese adolescent males? A randomised controlled trial. Br. J. Sports Med. 2014, 48, 1482–1488. [Google Scholar] [CrossRef] [PubMed]
- Ramadhan, B.J.; Alramadan, M.J.; Alhassan, R.E.; Almajed, H.A.; Khamseen, M.A.; Billah, B. Adherence to the recommended physical activity duration among Saudis with type 2 diabetes mellitus. J. Family Med. Prim. Care 2019, 8, 3668. [Google Scholar] [CrossRef] [PubMed]
- Cangelosi, G.; Mancin, S.; Pantanetti, P.; Nguyen, C.T.; Morales Palomares, S.; Biondini, F.; Sguanci, M.; Petrelli, F. Lifestyle Medicine Case Manager Nurses for Type Two Diabetes Patients: An Overview of a Job Description Framework—A Narrative Review. Diabetology 2024, 5, 375–388. [Google Scholar] [CrossRef]
- Alakhali, K.M.; Sultan, M.A.; Alavudeen, S.S.; Irawati, L.; Morad, A.A. Health-related quality of life in patients with diabetes using sf-20 questionnaire in aseer region, saudi arabia. Eur. J. Clin. Pharm. Atención Farm. 2020, 22, 142–149. [Google Scholar]
- Alsuwayt, S.; Almesned, M.; Alhajri, S.; Alomari, N.; Alhadlaq, R.; Alotaibi, A. Quality of life among type II diabetic patients attending the primary health centers of King Saud Medical City in Riyadh, Saudi Arabia. J. Family Med. Prim. Care 2021, 10, 3040–3046. [Google Scholar] [CrossRef]
- Von Elm, E.; Altman, D.G.; Egger, M.; Pocock, S.J.; Gøtzsche, P.C.; Vandenbroucke, J.P. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) Statement: Guidelines for Reporting Observational Studies. PLoS Med. 2007, 4, e296. [Google Scholar] [CrossRef]
- Saudi Arabia—International Diabetes Federation n.d. Available online: https://idf.org/our-network/regions-and-members/middle-east-and-north-africa/members/saudi-arabia/ (accessed on 1 November 2023).
- Al-Qerem, W.; Al-Maayah, B.; Ling, J. Developing and validating the arabic version of the diabetes quality of life questionnaire. East. Mediterr. Health J. 2021, 27, 414–426. [Google Scholar] [CrossRef]
- Rubin, R.R.; Peyrot, M.; Saudek, C.D. Effect of diabetes education on self-care, metabolic control, and emotional well-being. Diabetes Care 1989, 12, 673–679. [Google Scholar] [CrossRef]
- Flatz, A.; Casillas, A.; Stringhini, S.; Zuercher, E.; Burnand, B.; Peytremann-Bridevaux, I. Association between education and quality of diabetes care in Switzerland. Int. J. Gen. Med. 2015, 8, 87–92. [Google Scholar] [CrossRef]
- Kavookjian, J.; LaManna, J.B.; Davidson, P.; Davis, J.W.; Fahim, S.M.; McDaniel, C.C.; Ekong, G.; Todd, A.; Yehl, K.; Cox, C. Impact of Diabetes Self-Management Education/Support on Self-Reported Quality of Life in Youth with Type 1 or Type 2 Diabetes. Sci. Diabetes Self-Manag. Care 2022, 48, 406–436. [Google Scholar] [CrossRef] [PubMed]
- Ferreira, P.L.; Morais, C.; Pimenta, R.; Ribeiro, I.; Amorim, I.; Alves, S.M. Empowerment and Knowledge as Determinants for Quality of Life: A Contribution to a Better Type 2 Diabetes Self-Management. Int. J. Environ. Res. Public Health 2023, 20, 4544. [Google Scholar] [CrossRef] [PubMed]
- Pétré, B.; Scheen, A.J.; Ziegler, O.; Donneau, A.F.; Dardenne, N.; Husson, E.; Albert, A.; Guillaume, M. Body image discrepancy and subjective norm as mediators and moderators of the relationship between body mass index and quality of life. Patient Prefer. Adherence 2016, 10, 2261–2270. [Google Scholar] [CrossRef]
- Thiel, D.M.; Al Sayah, F.; Vallance, J.K.; Johnson, S.T.; Johnson, J.A. Association between Physical Activity and Health-Related Quality of Life in Adults with Type 2 Diabetes. Can. J. Diabetes 2017, 41, 58–63. [Google Scholar] [CrossRef] [PubMed]
- Bowen, P.G.; Clay, O.J.; Lee, L.T.; Vice, J.; Ovalle, F.; Crowe, M. Associations of social support and self-efficacy with quality of life in older adults with diabetes. J. Gerontol. Nurs. 2015, 41, 21–29. [Google Scholar] [CrossRef]
- Alenzi, E.O.; Alqahtani, W.I.; Altwegri, M.A.; Alhelal, S.M.; Alyami, W.A.; Almohana, D.M.; Aldrees, R.R.; Alnashar, R.S.; Almugizel, B.H.; Alshabanat, N.M.; et al. Assessment of the capability to adopt a healthy lifestyle: Insights into gender, socioeconomic factors, perceived health, and regional variations. Front. Public Health 2025, 13, 1476401. [Google Scholar] [CrossRef]
- Alenzi, E.O.; Alqahtani, W.I.; Altwegri, M.A.; Alhelal, S.M.; Alyami, W.A.; Almohana, D.M.; Aldrees, R.R.; Alnashar, R.S.; Almugizel, B.H.; Alshabanat, N.M.; et al. Perceived Effectiveness and Utilization of Health Promotion Initiatives in Saudi Arabia: Insights and Recommendations. Healthcare 2024, 12, 2352. [Google Scholar] [CrossRef]
- Venkataraman, K.; Wee, H.L.; Leow, M.K.; Tai, E.S.; Lee, J.; Lim, S.C.; Tavintharan, S.; Wong, T.Y.; Ma, S.; Heng, D.; et al. Associations between complications and health-related quality of life in individuals with diabetes. Clin. Endocrinol. 2013, 78, 865–873. [Google Scholar] [CrossRef]
- Jankowska, A.; Golicki, D. EQ-5D-5L-based quality of life normative data for patients with self-reported diabetes in Poland. PLoS ONE 2021, 16, e0257998. [Google Scholar] [CrossRef]
- Naranjo, C.; Ortega-Jiménez, P.; Del Reguero, L.; Moratalla, G.; Failde, I. Relationship between diabetic neuropathic pain and comorbidity. Their impact on pain intensity, diabetes complications and quality of life in patients with type-2 diabetes mellitus. Diabetes Res. Clin. Pract. 2020, 165, 108236. [Google Scholar] [CrossRef]
- López-López, L.; Losa-Iglesias, M.E.; Gómez-Salgado, J.; Becerro-de-Bengoa-Vallejo, R.; Romero-Morales, C.; López-López, D.; De Labra, C.; Navarro-Flores, E. The implications of diabetic foot health-related with quality of life: A retrospective case control investigation. J. Tissue Viability 2022, 31, 790–793. [Google Scholar] [CrossRef]
- Vileikyte, L.; Rubin, R.R.; Leventhal, H. Psychological aspects of diabetic neuropathic foot complications: An overview. Diabetes Metab. Res. Rev. 2004, 20, S13–S18. [Google Scholar] [CrossRef]
- Sidhu, S.; Gonzalez, P.M.; Petricone-Westwood, D.; Brewis, C.S.; Rabi, D.M.; Campbell, D.J. Approaches to Psychosocial Care Within Tertiary Diabetes Care Centres in Canada: An Environmental Scan. Can. J. Diabetes 2022, 46, 244–252. [Google Scholar] [CrossRef]
- Alenzi, E.O.; Sambamoorthi, U. Depression treatment and health-related quality of life among adults with diabetes and depression. Qual. Life Res. 2016, 25, 1517–1525. [Google Scholar] [CrossRef]
- Chantzaras, A.; Yfantopoulos, J. Association between medication adherence and health-related quality of life of patients with diabetes. Hormones 2022, 21, 691–705. [Google Scholar] [CrossRef]
| Characteristics | Frequency | % | |
|---|---|---|---|
| Age (years) | |||
| Less than 18 | 35 | 6.6 | |
| From 18 to less than 23 | 70 | 13.3 | |
| More than 23 to less than 30 | 43 | 8.2 | |
| From 30 to less than 40 | 60 | 11.14 | |
| From 40 to less than 50 | 103 | 19.5 | |
| From 50 to less than 60 | 100 | 19.0 | |
| From 60 to less than 65 | 59 | 11.2 | |
| ≥65 | 57 | 10.8 | |
| Gender | |||
| Male | 227 | 43.1 | |
| Female | 300 | 56.1 | |
| Marital status | |||
| Single | 144 | 27.3 | |
| Married | 304 | 57.7 | |
| Divorced | 44 | 8.3 | |
| Widowed | 35 | 6.6 | |
| Educational level | |||
| Less than high school | 127 | 24.1 | |
| High school | 174 | 33 | |
| Bachelor’s degree | 196 | 37.2 | |
| Postgraduate | 30 | 5.7 | |
| Occupation | |||
| Student | 69 | 13.1 | |
| Employed | 183 | 34.7 | |
| Housewife | 136 | 25.8 | |
| Unemployed and looking for a job | 38 | 7.2 | |
| Retired | 74 | 14.0 | |
| Business | 27 | 5.1 | |
| Region of residence | |||
| Central region | 213 | 40.4 | |
| Eastern region | 177 | 33.6 | |
| Western region | 63 | 12.0 | |
| Northern region | 7 | 1.3 | |
| Southern region | 67 | 12.7 | |
| Urban or rural | |||
| Urban | 494 | 93.7 | |
| Rural | 33 | 6.3 | |
| Family monthly income | |||
| <3000 SR | 47 | 8.9 | |
| 3000–<5000 SR | 50 | 9.5 | |
| 5000–<10,000 SR | 114 | 21.6 | |
| 10,000–<15,000 SR | 106 | 20.1 | |
| 15,000–<20,000 SR | 85 | 16.1 | |
| 20,000–<25,000 SR | 45 | 8.5 | |
| 25,000–<30,000 SR | 31 | 5.9 | |
| ≥30,000 SR | 49 | 9.3 | |
| Number of family members | |||
| Living alone | 54 | 10.2 | |
| Only two | 31 | 5.9 | |
| 3 | 55 | 10.4 | |
| 4 | 70 | 13.3 | |
| 5 | 90 | 17.1 | |
| 6 | 77 | 14.6 | |
| 7 | 51 | 9.7 | |
| 8 | 37 | 7.0 | |
| ≥9 | 62 | 11.8 | |
| Nationality | |||
| Saudi | 468 | 88.8 | |
| Non-Saudi | 59 | 11.2 | |
| Characteristics | Frequency | % | |
|---|---|---|---|
| Medical insurance status | |||
| Have medical insurance | 177 | 33.6 | |
| Non-insured and use public hospitals and clinics | 285 | 54.1 | |
| Non-insured and use private hospitals and clinics (out-of-pocket) | 65 | 12.3 | |
| Most accessible setting for diabetes-related healthcare | |||
| Public hospitals | 280 | 53.1 | |
| Private hospitals | 107 | 20.3 | |
| Public primary health care centers | 90 | 17.1 | |
| Private healthcare centers/clinics | 50 | 9.5 | |
| Most used healthcare services | |||
| Outpatient clinic services | 421 | 79.9 | |
| Emergency services | 61 | 11.6 | |
| Pharmacy services | 45 | 8.5 | |
| Diabetes out-of-pocket expenditures | |||
| No out-of-pocket expenditures | 269 | 51.0 | |
| <100 SR | 34 | 6.5 | |
| 100–< 250 SR | 68 | 12.9 | |
| 250–< 500 SR | 49 | 9.3 | |
| 500–< 1000 SR | 56 | 10.6 | |
| ≥1000 SR | 51 | 9.7 | |
| Number of hospitalizations due to diabetes or its complications | |||
| 0 | 372 | 70.6 | |
| 1 | 58 | 11.0 | |
| 2 | 56 | 10.6 | |
| ≥3 | 41 | 7.8 | |
| Number of hospitalizations due to other health conditions | |||
| 0 | 338 | 64.1 | |
| 1 | 79 | 15.0 | |
| 2 | 47 | 8.9 | |
| ≥3 | 63 | 12.0 | |
| Characteristics | Frequency | % | |
|---|---|---|---|
| Wight status | |||
| Underweight | 14 | 2.7 | |
| Normal weight | 145 | 27.5 | |
| Overweight | 168 | 31.9 | |
| Obese | 200 | 38.0 | |
| Following a healthy diet | |||
| No | 284 | 53.9 | |
| Yes | 243 | 46.1 | |
| Exercises/physical activities | |||
| No exercises | 188 | 35.7 | |
| 1 or 2 times per week | 206 | 39.1 | |
| 3 or 4 times per week | 99 | 18.8 | |
| ≥5 times per week | 34 | 6.5 | |
| Smoking status | |||
| Non-smoker | 405 | 76.9 | |
| Past smoker | 46 | 8.7 | |
| Current smoker | 76 | 14.4 | |
| Diabetes-related factors | |||
| Diabetes duration (years) | |||
| Less than 5 | 159 | 30.2 | |
| From 5 to less than 10 | 101 | 19.2 | |
| From 10 to less than 15 | 110 | 20.9 | |
| From 15 to less than 20 | 54 | 10.2 | |
| ≥20 | 103 | 19.5 | |
| Family history of diabetes | |||
| No family history | 139 | 26.4 | |
| 2nd grade relatives | 74 | 14.0 | |
| 1st grade relatives | 227 | 43.1 | |
| Both 2nd and 1st grades relative | 87 | 16.5 | |
| Diabetes retinopathy | |||
| No | 462 | 87.7 | |
| Yes | 65 | 12.3 | |
| Diabetes neuropathy | |||
| No | 492 | 93.4 | |
| Yes | 35 | 6.6 | |
| Diabetes nephropathy | |||
| No | 467 | 88.6 | |
| Yes | 60 | 11.4 | |
| Diabetic foot | |||
| No | 501 | 95.1 | |
| Yes | 26 | 4.9 | |
| Diabetic coma | |||
| No | 507 | 96.2 | |
| Yes | 20 | 3.8 | |
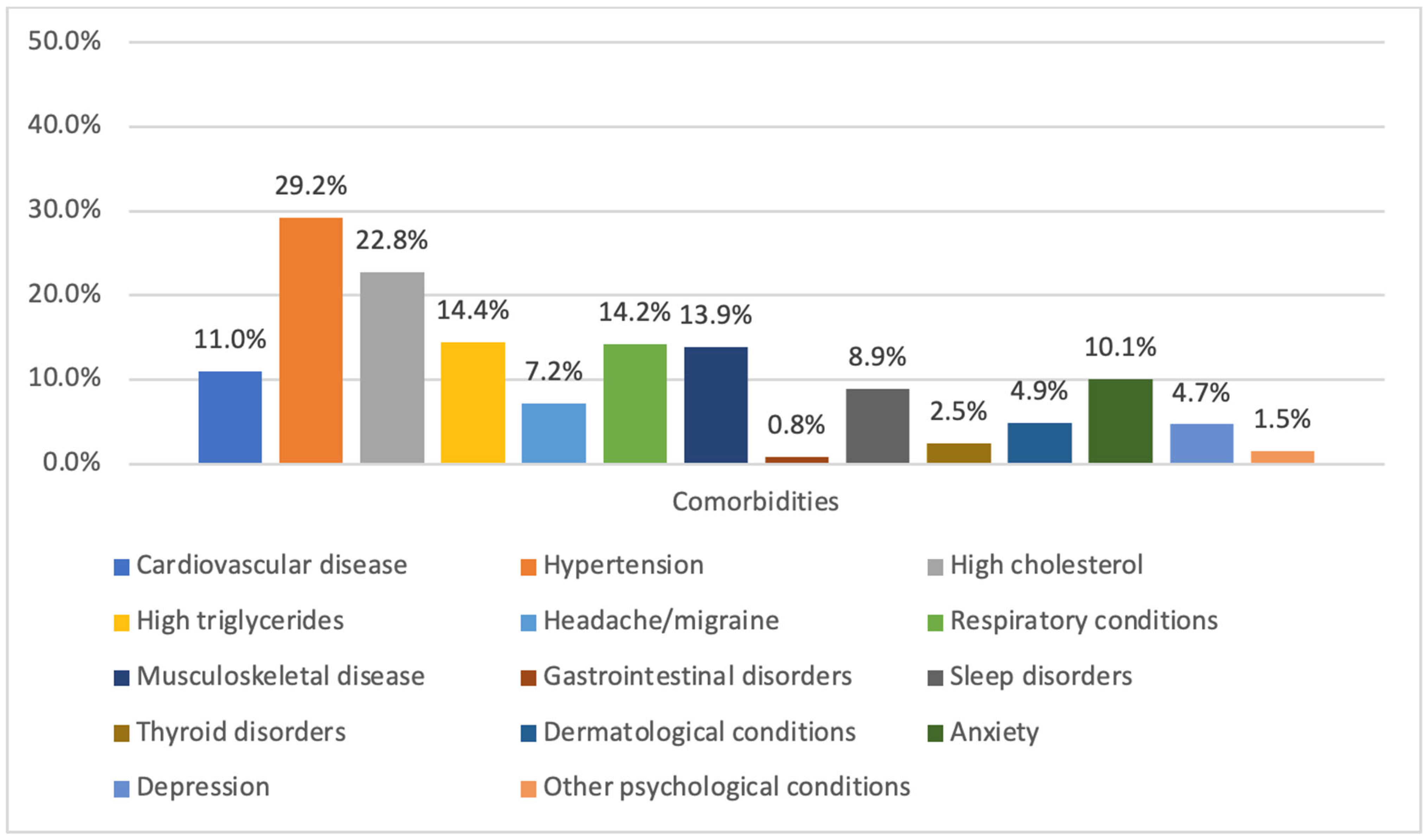
| Comorbidities | |||
| Presence of other comorbid conditions | |||
| No | 214 | 40.6 | |
| Yes | 313 | 59.4 | |
| Diabetes managements | |||
| Metformin use | |||
| No | 187 | 35.5 | |
| Yes | 340 | 64.5 | |
| Other antidiabetic medication use | |||
| No | 318 | 60.3 | |
| Yes | 209 | 39.7 | |
| Insulin injection use | |||
| No | 250 | 47.4 | |
| Yes | 277 | 52.6 | |
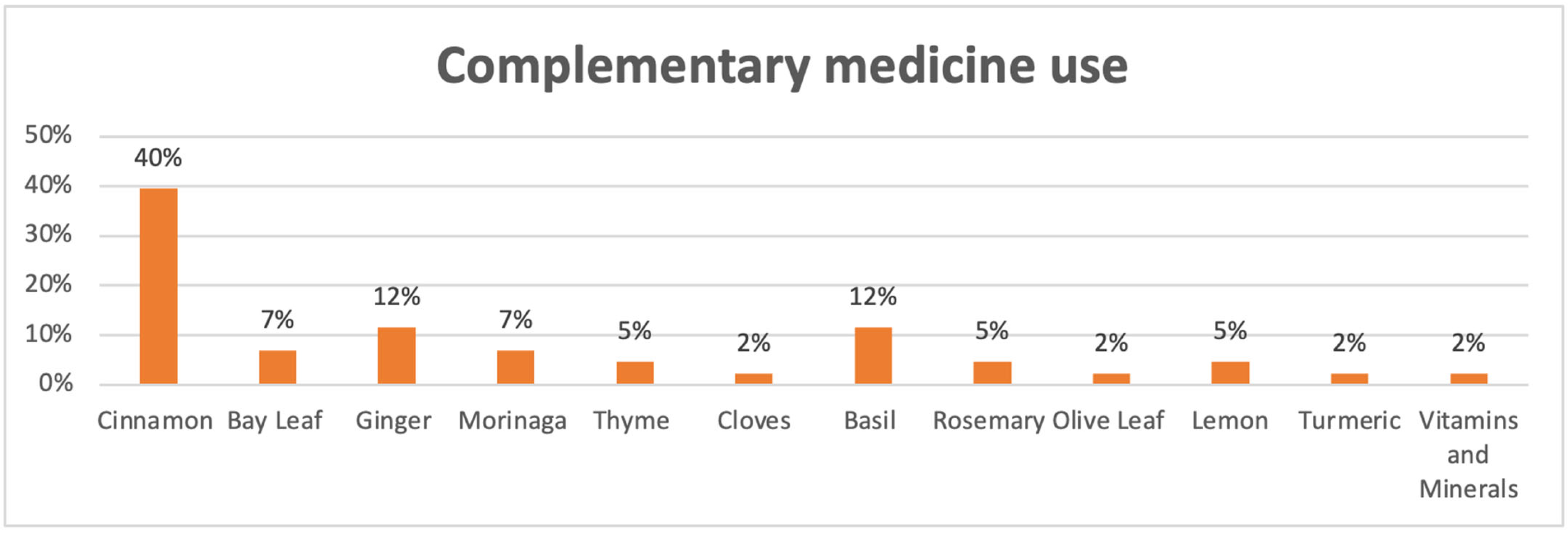
| Complementary medicine use | |||
| No | 474 | 89.9 | |
| Yes | 53 | 10.1 | |
| Characteristics | Mean | SD | p-Value | |
|---|---|---|---|---|
| Total | 3.34 | 0.59 | ||
| Demographic and socioeconomic factors | ||||
| Age (years) | 0.010 a | |||
| Less than 18 | 3.34 | 0.74 | ||
| From 18 to less than 23 | 3.32 | 0.66 | ||
| More than 23 to less than 30 | 3.19 | 0.54 | ||
| From 30 to less than 40 | 3.35 | 0.56 | ||
| From 40 to less than 50 | 3.43 | 0.54 | ||
| From 50 to less than 60 | 3.42 | 0.59 | ||
| From 60 to less than 65 | 3.43 | 0.53 | ||
| ≥65 | 3.09 | 0.58 | ||
| Gender | 0.107 b | |||
| Male | 3.37 | 0.63 | ||
| Female | 3.33 | 0.56 | ||
| Marital status | <0.001 a | |||
| Single | 3.28 | 0.66 | ||
| Married | 3.43 | 0.53 | ||
| Divorced | 3.09 | 0.56 | ||
| Widowed | 3.12 | 0.71 | ||
| Educational level | 0.001 a | |||
| Less than high school | 3.22 | 0.58 | ||
| High school | 3.33 | 0.66 | ||
| Bachelor’s degree | 3.37 | 0.52 | ||
| Postgraduate | 3.70 | 0.52 | ||
| Occupation | 0.787 a | |||
| Student | 3.32 | 0.68 | ||
| Employed | 3.38 | 0.59 | ||
| Housewife | 3.30 | 0.55 | ||
| Unemployed and looking for a job | 3.28 | 0.571 | ||
| Retired | 3.39 | 0.58 | ||
| Business | 3.29 | 0.69 | ||
| Region of residence | <0.001 a | |||
| Central region | 3.51 | 0.58 | ||
| Eastern region | 3.14 | 0.59 | ||
| Western region | 3.42 | 0.65 | ||
| Northern region | 3.25 | 0.59 | ||
| Southern region | 3.30 | 0.38 | ||
| Urban or rural | 0.530 b | |||
| Urban | 3.35 | 0.59 | ||
| Rural | 3.28 | 0.57 | ||
| Family monthly income | 0.001 a | |||
| <3000 SR | 3.09 | 0.55 | ||
| 3000–< 5000 SR | 3.24 | 0.52 | ||
| 5000–< 10,000 SR | 3.27 | 0.50 | ||
| 10,000–< 15,000 SR | 3.33 | 0.58 | ||
| 15,000–< 20,000 SR | 3.38 | 0.61 | ||
| 20,000–< 25,000 SR | 3.58 | 0.68 | ||
| 25,000–< 30,000 SR | 3.50 | 0.62 | ||
| ≥30,000 SR | 3.51 | 0.68 | ||
| Number of family members | <0.001 a | |||
| Living alone | 3.08 | 0.58 | ||
| Only two | 3.21 | 0.48 | ||
| 3 | 3.19 | 1.61 | ||
| 4 | 3.30 | 0.54 | ||
| 5 | 3.41 | 0.64 | ||
| 6 | 3.37 | 0.53 | ||
| 7 | 3.57 | 0.63 | ||
| 8 | 3.42 | 0.51 | ||
| ≥9 | 3.47 | 0.61 | ||
| Nationality | 0.016 b | |||
| Saudi | 3.36 | 0.59 | ||
| Non-Saudi | 3.17 | 0.58 | ||
| Access to healthcare | ||||
| Medical insurance status | 0.022 a | |||
| Have medical insurance | 3.43 | 0.60 | ||
| Non-insured and use public hospitals and clinics | 3.28 | 0.58 | ||
| Non-insured and use private hospitals and clinics (out-of-pocket) | 3.39 | 0.61 | ||
| Most accessible setting for diabetes healthcare | <0.001 a | |||
| Public hospitals | 3.36 | 0.58 | ||
| Private hospitals | 3.56 | 0.61 | ||
| Public primary health care centers | 3.11 | 0.54 | ||
| Private healthcare centers/clinics | 3.20 | 0.55 | ||
| Most used healthcare services | <0.001 a | |||
| Outpatient clinic services | 3.38 | 0.58 | ||
| Emergency services | 2.93 | 0.53 | ||
| Pharmacy services | 3.51 | 0.58 | ||
| Diabetes out-of-pocket expenditures | 0.324 a | |||
| No out-of-pocket expenditures | 3.38 | 0.60 | ||
| <100 SR | 3.50 | 0.50 | ||
| 100–< 250 SR | 3.34 | 0.52 | ||
| 250–< 500 SR | 3.42 | 0.69 | ||
| 500–< 1000 SR | 3.24 | 0.59 | ||
| ≥1000 SR | 3.24 | 0.65 | ||
| Number of hospitalizations due to diabetes or its complications | <0.001 a | |||
| 0 | 3.44 | 0.57 | ||
| 1 | 3.13 | 0.62 | ||
| 2 | 3.06 | 0.47 | ||
| ≥3 | 3.15 | 0.67 | ||
| Number of hospitalizations due to other health conditions | <0.001 a | |||
| 0 | 3.42 | 0.58 | ||
| 1 | 3.27 | 0.63 | ||
| 2 | 3.14 | 0.64 | ||
| ≥3 | 3.15 | 0.47 | ||
| Health behaviors | ||||
| Wight status | 0.024 a | |||
| Underweight | 3.17 | 0.68 | ||
| Normal weight | 3.43 | 0.66 | ||
| Overweight | 3.39 | 0.57 | ||
| Obese | 3.26 | 0.54 | ||
| Following a healthy diet | 0.472 b | |||
| No | 3.36 | 0.60 | ||
| Yes | 3.32 | 0.59 | ||
| Exercises/physical activities | <0.001 a | |||
| No exercises | 3.26 | 0.59 | ||
| 1 or 2 times per week | 3.29 | 0.58 | ||
| 3 or 4 times per week | 3.40 | 0.55 | ||
| ≥5 times per week | 3.94 | 0.50 | ||
| Smoking status | 0.594 a | |||
| Non-smoker | 3.35 | 0.57 | ||
| Past smoker | 3.35 | 0.61 | ||
| Current smoker | 3.28 | 0.69 | ||
| Diabetes-related factors | ||||
| Diabetes duration (years) | 0.415 a | |||
| Less than 5 | 3.42 | 0.53 | ||
| From 5 to less than 10 | 3.30 | 0.62 | ||
| From 10 to less than 15 | 3.33 | 0.60 | ||
| From 15 to less than 20 | 3.34 | 0.69 | ||
| ≥20 | 3.29 | 0.59 | ||
| Family history of diabetes | 0.350 a | |||
| No family history | 3.40 | 0.61 | ||
| 2nd grade relatives | 3.37 | 0.49 | ||
| 1st grade relatives | 3.33 | 0.59 | ||
| Both 2nd and 1st grades relative | 3.26 | 0.65 | ||
| Diabetes retinopathy | 0.149 b | |||
| No | 3.36 | 0.59 | ||
| Yes | 3.24 | 0.64 | ||
| Diabetes neuropathy | <0.001 b | |||
| No | 3.37 | 0.58 | ||
| Yes | 2.95 | 0.55 | ||
| Diabetes nephropathy | <0.001 b | |||
| No | 3.39 | 0.58 | ||
| Yes | 2.94 | 0.56 | ||
| Diabetic foot | <0.001 b | |||
| No | 3.37 | 0.58 | ||
| Yes | 2.88 | 0.58 | ||
| Diabetic coma | 0.010 b | |||
| No | 3.36 | 0.59 | ||
| Yes | 3.01 | 0.44 | ||
| Comorbidities | ||||
| Presence of other comorbid conditions | 0.003 b | |||
| No | 3.43 | 0.58 | ||
| Yes | 3.28 | 0.59 | ||
| Cardiovascular disease | 0.039 b | |||
| No | 3.36 | 0.58 | ||
| Yes | 3.19 | 0.59 | ||
| Hypertension | 0.003 b | |||
| No | 3.39 | 0.58 | ||
| Yes | 3.22 | 0.60 | ||
| High cholesterol | 0.051 b | |||
| No | 3.37 | 0.58 | ||
| Yes | 3.25 | 0.64 | ||
| High triglycerides | <0.001 b | |||
| No | 3.38 | 0.58 | ||
| Yes | 3.12 | 0.60 | ||
| Headache/migraine | 0.444 b | |||
| No | 3.34 | 0.60 | ||
| Yes | 3.41 | 0.49 | ||
| Respiratory conditions | <0.001 b | |||
| No | 3.39 | 0.58 | ||
| Yes | 3.07 | 0.62 | ||
| Musculoskeletal disease | 0.145 b | |||
| No | 3.36 | 0.58 | ||
| Yes | 3.25 | 0.66 | ||
| Gastrointestinal disorders | 0.110 b | |||
| No | 3.35 | 0.59 | ||
| Yes | 2.85 | 0.50 | ||
| Sleep disorders | <0.001 b | |||
| No | 3.37 | 0.58 | ||
| Yes | 3.02 | 0.65 | ||
| Thyroid disorders | 0.669 b | |||
| No | 3.34 | 0.59 | ||
| Yes | 3.27 | 0.63 | ||
| Dermatological conditions | ||||
| No | 3.35 | 0.60 | 0.347 b | |
| Yes | 3.24 | 0.49 | ||
| Anxiety | <0.001 b | |||
| No | 3.38 | 0.59 | ||
| Yes | 3.01 | 0.54 | ||
| Depression | <0.001 b | |||
| No | 3.37 | 0.59 | ||
| Yes | 2.81 | 0.44 | ||
| Other psychological conditions | 0.250 b | |||
| No | 3.35 | 0.59 | ||
| Yes | 3.10 | 0.39 | ||
| Diabetes managements | ||||
| Metformin use | 0.121 b | |||
| No | 3.29 | 0.62 | ||
| Yes | 3.37 | 0.57 | ||
| Other antidiabetic medication use | 0.007 b | |||
| No | 3.40 | 0.60 | ||
| Yes | 3.26 | 0.58 | ||
| Insulin injection use | 0.007 b | |||
| No | 3.41 | 0.56 | ||
| Yes | 3.28 | 0.61 | ||
| Complementary medicine use | 0.999 b | |||
| No | 3.34 | 0.59 | ||
| Yes | 3.34 | 0.60 | ||
| Characteristics | Beta | 95% CI | p-Value | |
|---|---|---|---|---|
| Demographic and socioeconomic factors | ||||
| Age (years) | ||||
| Less than 18 | 0.61 | (−0.83, 2.05) | 0.404 | |
| From 18 to less than 23 | 0.08 | (−1.13, 1.28) | 0.902 | |
| More than 23 to less than 30 | −0.40 | (−1.52, 0.72) | 0.482 | |
| From 30 to less than 40 | 0.03 | (−0.91, 0.95) | 0.956 | |
| From 40 to less than 50 | −0.10 | (−0.95, 0.76) | 0.826 | |
| From 50 to less than 60 | 0.40 | (−0.35, 1.16) | 0.297 | |
| From 60 to less than 65 | 0.36 | (−0.38, 1.10) | 0.341 | |
| ≥65 | Reference group | |||
| Gender | ||||
| Male | 0.30 | (−0.17, 0.77) | 0.212 | |
| Female | Reference group | |||
| Marital status | ||||
| Single | −0.64 | (−1.78, 0.51) | 0.277 | |
| Married | −0.18 | (−1.02, 0.66) | 0.680 | |
| Divorced | −0.19 | (−1.13, 0.74) | 0.685 | |
| Widowed | Reference group | |||
| Educational level | ||||
| Less than high school | −1.09 | (−1.99, −0.18) | 0.018 | |
| High school | −0.83 | (−1.63, −0.03) | 0.043 | |
| Bachelor’s degree | −0.65 | (−1.40, 0.10) | 0.090 | |
| Postgraduate | Reference group | |||
| Occupation | ||||
| Student | −0.11 | (−1.22, 1.00) | 0.851 | |
| Employed | 0.23 | (−0.59, 1.04) | 0.586 | |
| Housewife | 0.63 | (−0.28, 1.54) | 0.175 | |
| Unemployed and looking for a job | 0.54 | (−0.52, 1.61) | 0.316 | |
| Retired | 0.29 | (−0.60, 1.17) | 0.529 | |
| Business | Reference group | |||
| Region of residence | ||||
| Central region | 0.00 | (−0.61, 0.63) | 0.983 | |
| Eastern region | −0.97 | (−1.60, −0.34) | 0.003 | |
| Western region | 0.34 | (−0.36, 1.04) | 0.341 | |
| Northern region | −0.48 | (−2.06, 1.10) | 0.553 | |
| Southern region | Reference group | |||
| Urban or rural | ||||
| Urban | 0.08 | (−0.63, 0.78) | 0.835 | |
| Rural | Reference group | |||
| Family monthly income | ||||
| <3000 SR | −0.72 | (−1.56, 0.11) | 0.089 | |
| 3000–< 5000 SR | −0.42 | (−1.21, 0.36) | 0.290 | |
| 5000–< 10,000 SR | −0.65 | (−1.32, 0.03) | 0.059 | |
| 10,000–< 15,000 SR | −0.60 | (−1.27, 0.07) | 0.079 | |
| 15,000–< 20,000 SR | −0.53 | (−1.21, 0.15) | 0.129 | |
| 20,000–< 25,000 SR | 0.40 | (−0.37, 1.16) | 0.311 | |
| 25,000–< 30,000 SR | −0.37 | (−1.24, 0.50) | 0.404 | |
| ≥30,000 SR | Reference group | |||
| Number of family members | ||||
| Living alone | −0.74 | (−1.52, 0.05) | 0.067 | |
| Only two | 0.11 | (−0.76, 0.99) | 0.802 | |
| 3 | −0.60 | (−1.36, 0.16) | 0.122 | |
| 4 | −0.38 | (−1.07, 0.31) | 0.280 | |
| 5 | 0.31 | (−0.33, 0.94) | 0.341 | |
| 6 | −0.21 | (−0.86, 0.43) | 0.518 | |
| 7 | 0.53 | (−0.18, 1.23) | 0.141 | |
| 8 | 0.01 | (−0.75, 0.78) | 0.968 | |
| ≥9 | Reference group | |||
| Nationality | ||||
| Saudi | 0.56 | (−0.03, 1.16) | 0.065 | |
| Non-Saudi | Reference group | |||
| Access to healthcare | ||||
| Medical insurance status | ||||
| Have medical insurance | −0.08 | (−0.66, 0.50) | 0.797 | |
| Non-insured and use public hospitals and clinics | −0.26 | (−0.90, 0.38) | 0.430 | |
| Non-insured and use private hospitals and clinics (out-of-pocket) | Reference group | |||
| Most accessible setting for diabetes healthcare | ||||
| Public hospitals | 0.62 | (−0.08, 1.31) | 0.083 | |
| Private hospitals | 1.09 | (0.41, 1.77) | 0.002 | |
| Public primary health care centers | −0.12 | (−0.92, 0.68) | 0.763 | |
| Private healthcare centers/clinics | Reference group | |||
| Most used healthcare services | ||||
| Outpatient clinic services | 0.01 | (−0.60, 0.61) | 0.985 | |
| Emergency services | −0.51 | (−1.32, 0.30) | 0.213 | |
| Pharmacy services | Reference group | |||
| Diabetes out-of-pocket expenditures | ||||
| No out-of-pocket expenditures | 0.55 | (−0.08, 1.17) | 0.09 | |
| <100 SR | 0.17 | (−0.72, 1.06) | 0.71 | |
| 100–<250 SR | 0.20 | (−0.54, 0.91) | 0.61 | |
| 250–<500 SR | 0.43 | (−0.33, 1.19) | 0.262 | |
| 500–<1000 SR | −0.40 | (−1.15, 0.35) | 0.29 | |
| ≥1000 SR | Reference group | |||
| Number of hospitalizations due to diabetes or its complications | ||||
| 0 | 0.16 | (−0.55, 0.86) | 0.665 | |
| 1 | 0.01 | (−0.80, 0.82) | 0.983 | |
| 2 | −0.16 | (−0.94, 0.62) | 0.684 | |
| ≥3 | Reference group | |||
| Number of hospitalizations due to other health conditions | ||||
| 0 | 0.16 | (−0.20, 1.01) | 0.186 | |
| 1 | 0.01 | (−0.37, 0.99) | 0.375 | |
| 2 | −0.16 | (−0.62, 0.86) | 0.753 | |
| ≥3 | Reference group | |||
| Health behaviors | ||||
| Wight status | ||||
| Underweight | −0.33 | (−1.45, 0.79) | 0.567 | |
| Normal weight | 0.54 | (0.06, 1.03) | 0.028 | |
| Overweight | −0.01 | (−0.43, 0.41) | 0.953 | |
| Obese | Reference group | |||
| Following a healthy diet | ||||
| No | 0.04 | (−0.33, 040) | 0.84 | |
| Yes | Reference group | |||
| Exercises/physical activities | ||||
| No exercises | −1.83 | (−2.56, −1.10) | <0.001 | |
| 1 or 2 times per week | −1.65 | (−2.38, −0.94) | <0.001 | |
| 3 or 4 times per week | −1.66 | (−2.43, −0.88) | <0.001 | |
| ≥5 times per week | Reference group | |||
| Smoking status | ||||
| Non-smoker | 0.22 | (−0.34, 0.78) | 0.435 | |
| Past smoker | −0.11 | (−0.83, 0.60) | 0.756 | |
| Current smoker | Reference group | |||
| Diabetes-related factors | ||||
| Diabetes duration (years) | ||||
| Less than 5 | 0.09 | (−0.51, 0.70) | 0.765 | |
| From 5 to less than 10 | −0.37 | (−0.98, 0.25) | 0.243 | |
| From 10 to less than 15 | −0.42 | (−0.98, 0.14) | 0.144 | |
| From 15 to less than 20 | −0.10 | (−0.78, 0.58) | 0.772 | |
| ≥20 | Reference group | |||
| Family history of diabetes | ||||
| No family history | −0.22 | (−0.78, 0.33) | 0.433 | |
| 2nd grade relatives | −0.33 | (−0.95, 0.30) | 0.303 | |
| 1st grade relatives | −0.16 | (−0.65, 0.34) | 0.534 | |
| Both 2nd and 1st grades relative | Reference group | |||
| Diabetes retinopathy | ||||
| No | Reference group | |||
| Yes | 0.51 | (−0.03, 1.05) | 0.066 | |
| Diabetes neuropathy | ||||
| No | Reference group | |||
| Yes | −1.14 | (−2.02, −0.26) | 0.011 | |
| Diabetes nephropathy | ||||
| No | Reference group | |||
| Yes | −0.45 | (−1.14, 0.25) | 0.208 | |
| Diabetic foot | ||||
| No | Reference group | |||
| Yes | −1.18 | (−2.01 −0.35) | 0.005 | |
| Diabetic coma | ||||
| No | Reference group | |||
| Yes | −0.68 | (−1.61, 0.25) | 0.153 | |
| Comorbidities | ||||
| Cardiovascular disease | ||||
| No | Reference group | |||
| Yes | 0.17 | (−0.44, 0.79) | 0.581 | |
| Hypertension | ||||
| No | Reference group | |||
| Yes | 0.06 | (−0.40, 0.53) | 0.795 | |
| High cholesterol | ||||
| No | Reference group | |||
| Yes | −0.06 | (−0.55, 0.43) | 0.807 | |
| High triglycerides | ||||
| No | Reference group | |||
| Yes | −0.37 | (−0.97, 0.230) | 0.227 | |
| Headache/migraine | ||||
| No | Reference group | |||
| Yes | 0.52 | (−0.15, 1.19) | 0.130 | |
| Respiratory conditions | ||||
| No | Reference group | |||
| Yes | −0.12 | (−0.904, 0.66) | 0.764 | |
| Musculoskeletal disease | ||||
| No | Reference group | |||
| Yes | 0.19 | (−0.33, 0.70) | 0.470 | |
| Gastrointestinal disorders | ||||
| No | Reference group | |||
| Yes | −0.87 | (−2.84, 1.10) | 0.386 | |
| Sleep disorders | ||||
| No | Reference group | |||
| Yes | −0.37 | (−1.32, 0.59) | 0.452 | |
| Thyroid disorders | ||||
| No | Reference group | |||
| Yes | −0.03 | (−1.07, 1.00) | 0.948 | |
| Dermatological conditions | ||||
| No | Reference group | |||
| Yes | 0.53 | (−0.30, 1.37) | 0.211 | |
| Anxiety | ||||
| No | Reference group | |||
| Yes | −0.31 | (−0.98, 0.37) | 0.369 | |
| Depression | ||||
| No | Reference group | |||
| Yes | −2.01 | (−2.93, − 1.10) | <0.001 | |
| Other psychological conditions | ||||
| No | Reference group | |||
| Yes | 1.05 | (−0.43, 2.53) | 0.164 | |
| Diabetes managements | ||||
| Metformin use | ||||
| No | Reference group | |||
| Yes | 0.33 | (−0.07, 0.72) | 0.108 | |
| Other antidiabetic medication use | ||||
| No | Reference group | |||
| Yes | −0.37 | (−0.75, 0.00) | 0.052 | |
| Insulin injection use | ||||
| No | Reference group | |||
| Yes | −0.01 | (−0.45, 0.42) | 0.958 | |
| Complementary medicine use | ||||
| No | Reference group | |||
| Yes | −0.35 | (−0.91, 0.21) | 0.215 | |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Published by MDPI on behalf of the Lithuanian University of Health Sciences. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Alenzi, E.O.; AlZabin, A.; Almajed, E.; Alqntash, N. Determinants of Diabetes-Related Quality of Life in Saudi Arabia: A Nationwide Survey-Based Assessment of Demographic, Health, and Complication-Related Influences. Medicina 2025, 61, 1583. https://doi.org/10.3390/medicina61091583
Alenzi EO, AlZabin A, Almajed E, Alqntash N. Determinants of Diabetes-Related Quality of Life in Saudi Arabia: A Nationwide Survey-Based Assessment of Demographic, Health, and Complication-Related Influences. Medicina. 2025; 61(9):1583. https://doi.org/10.3390/medicina61091583
Chicago/Turabian StyleAlenzi, Ebtihag O., Alya AlZabin, Ebtesam Almajed, and Norah Alqntash. 2025. "Determinants of Diabetes-Related Quality of Life in Saudi Arabia: A Nationwide Survey-Based Assessment of Demographic, Health, and Complication-Related Influences" Medicina 61, no. 9: 1583. https://doi.org/10.3390/medicina61091583
APA StyleAlenzi, E. O., AlZabin, A., Almajed, E., & Alqntash, N. (2025). Determinants of Diabetes-Related Quality of Life in Saudi Arabia: A Nationwide Survey-Based Assessment of Demographic, Health, and Complication-Related Influences. Medicina, 61(9), 1583. https://doi.org/10.3390/medicina61091583






