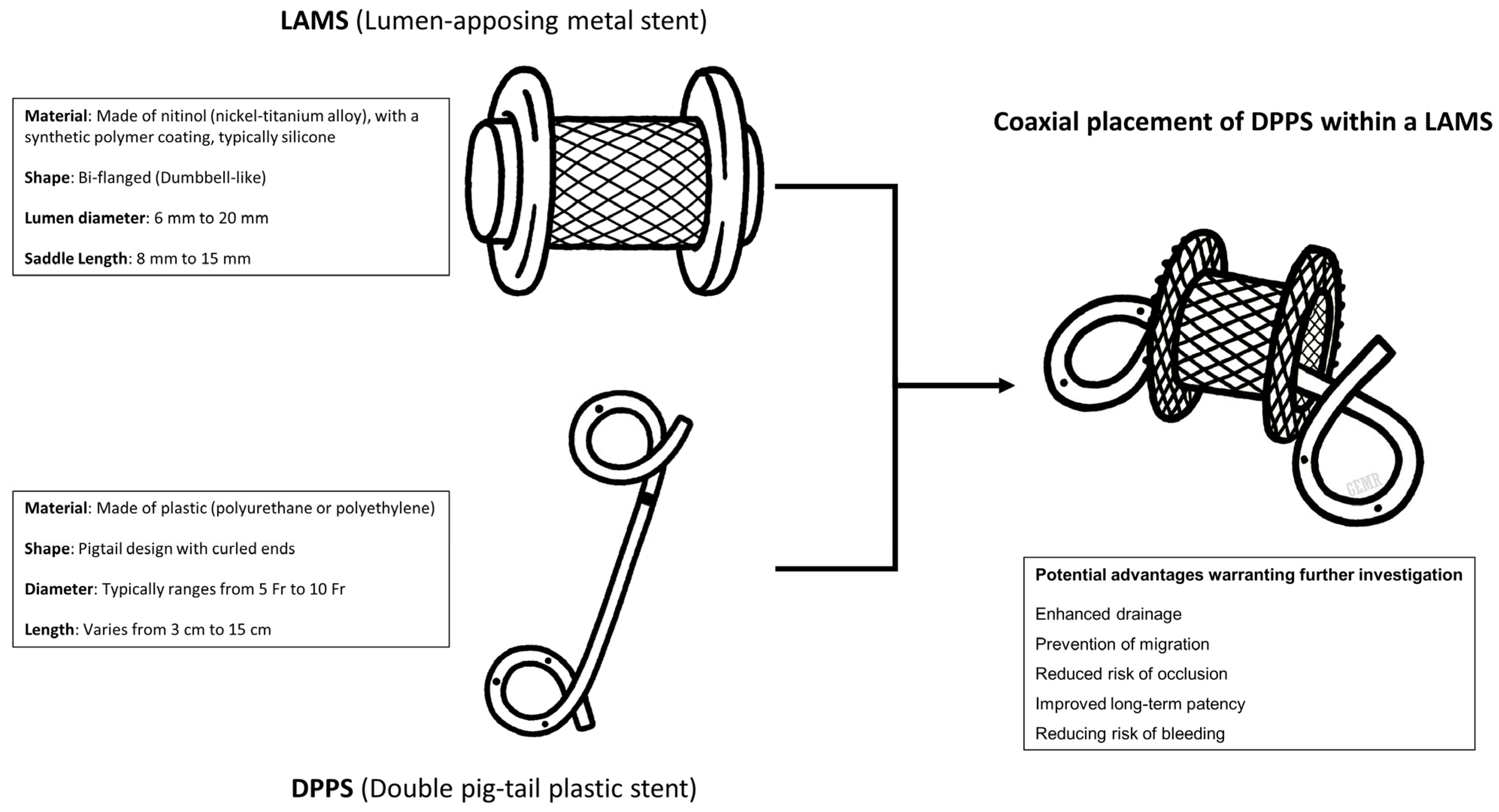
A Critical Narrative Review of Coaxial Double-Pigtail Stenting Within the LAMS in the Management of Pancreatic Fluid Collections
Abstract
1. Introduction
2. Materials and Methods
3. Results
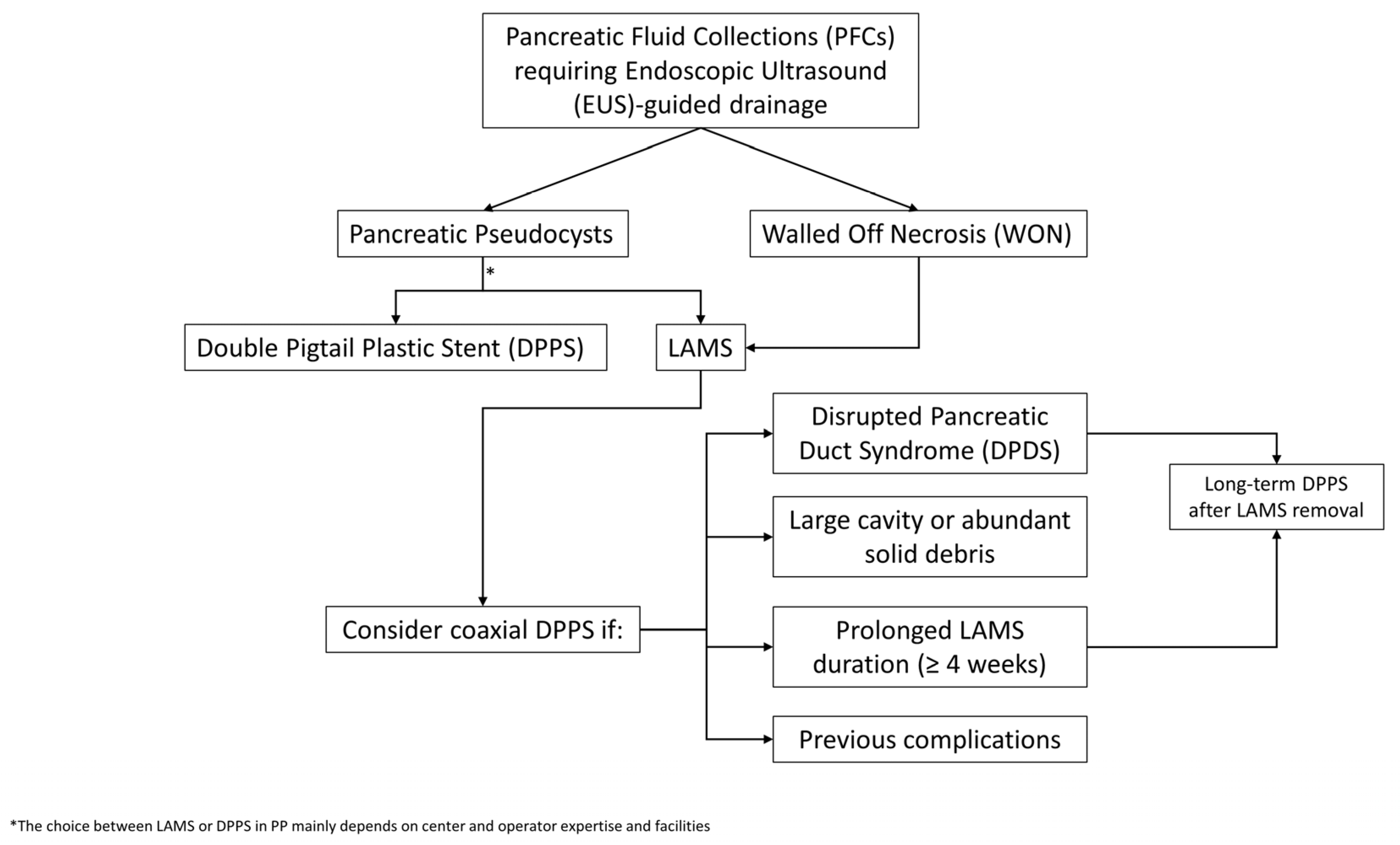
3.1. Clinical Data Comparing LAMSs vs. Coaxial DPPS Within LAMSs
3.2. Summary of Evidence
3.3. Type of LAMS: Does It Matter?
3.4. Optimizing LAMS-To-DPPS Transition in High-Risk Patients: Strategies and Innovation
3.5. A Pragmatic Approach to the Selective Use of Coaxial DPPSs
4. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Dorrell, R.; Pawa, S.; Pawa, R. Endoscopic Management of Pancreatic Fluid Collections. J. Clin. Med. 2021, 10, 284. [Google Scholar] [CrossRef]
- Braden, B.; Dietrich, C.F. Endoscopic ultrasonography-guided endoscopic treatment of pancreatic pseudocysts and walled-off necrosis: New technical developments. World J. Gastroenterol. 2014, 20, 16191. [Google Scholar] [CrossRef]
- Lyu, Y.; Li, T.; Wang, B.; Cheng, Y.; Chen, L.; Zhao, S. Comparison Between Lumen-Apposing Metal Stents and Plastic Stents in Endoscopic Ultrasound–Guided Drainage of Pancreatic Fluid Collection: A Meta-analysis and Systematic Review. Pancreas 2021, 50, 571–578. [Google Scholar] [CrossRef] [PubMed]
- Karstensen, J.G.; Novovic, S.; Hansen, E.F.; Jensen, A.B.; Jorgensen, H.L.; Lauritsen, M.L.; Werge, M.P.; Schmidt, P.N. EUS-guided drainage of large walled-off pancreatic necroses using plastic versus lumen-apposing metal stents: A single-centre randomised controlled trial. Gut 2023, 72, 1167–1173. [Google Scholar] [CrossRef] [PubMed]
- Maida, M.; Rizzo, G.E.M.; Traina, M.; Karstensen, J.G.; Voermans, R.P.; Gornals, J.B.; Jagtap, N.; Ligresti, D.; Carrozza, L.; Rancatore, G.; et al. Optimal timing for lumen-apposing metal stent removal following endoscopic ultrasound-guided drainage of pancreatic fluid collections: A systematic review and meta-analysis. Endoscopy, 2025; Epub ahead of print. [Google Scholar] [CrossRef] [PubMed]
- Law, R.J.; Chandrasekhara, V.; Bhatt, A.; Bucobo, J.C.; Copland, A.P.; Krishnan, K.; Kumta, N.A.; Pannala, R.; Parsi, M.A.; Rahimi, E.F.; et al. Lumen-apposing metal stents (with videos). Gastrointest. Endosc. 2021, 94, 457–470. [Google Scholar] [CrossRef]
- Varadarajulu, S.; Christein, J.D.; Wilcox, C.M. Frequency of complications during EUS-guided drainage of pancreatic fluid collections in 148 consecutive patients. J. Gastroenterol. Hepatol. 2011, 26, 1504–1508. [Google Scholar] [CrossRef] [PubMed]
- Bang, J.Y.; Varadarajulu, S. Lumen-apposing metal stents for endoscopic ultrasonography-guided interventions. Dig. Endosc. 2019, 31, 619–626. [Google Scholar] [CrossRef] [PubMed]
- Binda, C.; Fabbri, S.; Perini, B.; Boschetti, M.; Coluccio, C.; Giuffrida, P.; Gibiino, G.; Petraroli, C.; Fabbri, C. Endoscopic Ultrasound-Guided Drainage of Pancreatic Fluid Collections: Not All Queries Are Already Solved. Medicina 2024, 60, 333. [Google Scholar] [CrossRef]
- Wang, Z.; Wu, X.; Zhao, S.; Li, Z.; Bai, Y.; Wang, D. The role of co-axially placed double-pigtail stents within lumen-apposing metal stents in draining pancreatic fluid collections. Gastrointest. Endosc. 2018, 88, 409–410. [Google Scholar] [CrossRef]
- Aslam, S.; Ansari, Z.; Alani, M.; Srinivasan, I.; Chuang, K.Y. Coaxial Double-Pigtail Stent Placement: A Simple Solution to Decrease Bleeding Risk Associated with Lumen-Apposing Metal Stent? Cureus 2021, 13, e15981. Available online: https://www.cureus.com/articles/60172-coaxial-double-pigtail-stent-placement-a-simple-solution-to-decrease-bleeding-risk-associated-with-lumen-apposing-metal-stent (accessed on 26 May 2025). [CrossRef] [PubMed]
- Lang, G.D.; Fritz, C.; Bhat, T.; Das, K.K.; Murad, F.M.; Early, D.S.; Edmundowicz, S.A.; Kushnir, V.M.; Mullady, D.K. EUS-guided drainage of peripancreatic fluid collections with lumen-apposing metal stents and plastic double-pigtail stents: Comparison of efficacy and adverse event rates. Gastrointest. Endosc. 2018, 87, 150–157. [Google Scholar] [CrossRef]
- Puga, M.; Consiglieri, C.F.; Busquets, J.; Pallarès, N.; Secanella, L.; Peláez, N.; Fabregat, J.; Castellote, J.; Gornals, J.B. Safety of lumen-apposing stent with or without coaxial plastic stent for endoscopic ultrasound-guided drainage of pancreatic fluid collections: A retrospective study. Endoscopy 2018, 50, 1022–1026. [Google Scholar] [CrossRef]
- Aburajab, M.; Smith, Z.; Khan, A.; Dua, K. Safety and efficacy of lumen-apposing metal stents with and without simultaneous double-pigtail plastic stents for draining pancreatic pseudocyst. Gastrointest. Endosc. 2018, 87, 1248–1255. [Google Scholar] [CrossRef]
- Aujla, P.; Aleem, A.; Subramanian, S.K.; Goyal, H.; Patil, P.; Wadhwa, V.; Joseph-Talreja, M.; DaVee, T.; Ramireddy, S.; Guha, S.; et al. Stent Within a Stent: When Lumen Apposing Metal Stent Meets Its Match in Coaxial Double Pigtail Stent. Gastrointest. Endosc. 2023, 97, AB920. [Google Scholar] [CrossRef]
- AbiMansour, J.P.; Jaruvongvanich, V.; Velaga, S.; Law, R.J.; Storm, A.C.; Topazian, M.D.; Levy, M.J.; Alexander, R.; Vargas, E.J.; Bofill-Garcia, A.; et al. Lumen-apposing metal stents with or without coaxial plastic stent placement for the management of pancreatic fluid collections. Gastrointest. Endosc. 2024, 99, 104–107. [Google Scholar] [CrossRef] [PubMed]
- Mukai, S.; Sofuni, A.; Tsuchiya, T.; Tanaka, R.; Tonozuka, R.; Yamamoto, K.; Matsunami, Y.; Nagai, K.; Kojima, H.; Minami, H.; et al. A novel puzzle ring replacement technique of a lumen-apposing metal stent with a double-pigtail plastic stent to prevent walled-off necrosis recurrence (with video). DEN Open 2025, 5, e70020. [Google Scholar] [CrossRef]
- Ali, S.E.; Benrajab, K.; Mardini, H.; Su, L.; Gabr, M.; Frandah, W.M. Anchoring lumen-apposing metal stent with coaxial plastic stent for endoscopic ultrasound-guided drainage of pancreatic fluid collections: Any benefit? Ann. Gastroenterol. 2019, 32, 620–625. Available online: http://www.annalsgastro.gr/files/journals/1/earlyview/2019/ev-09-2019-03-AG4719-0414.pdf (accessed on 25 May 2025).
- Shamah, S.P.; Sahakian, A.B.; Chapman, C.G.; Buxbaum, J.L.; Muniraj, T.; Aslanian, H.A.; Villa, E.; Cho, J.; Haider, H.I.; Waxman, I.; et al. Double pigtail stent placement as an adjunct to lumen-apposing metal stentsfor drainage of pancreatic fluid collections may not affect outcomes: A multicenter experience. Endosc. Ultrasound. 2022, 11, 53–58. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Rossi, G.; Capurso, G.; Petrone, M.; Testoni, S.; Archibugi, L.; Traini, M.; Mariani, A.; Arcidiacono, P. Does Co-Axial Plastic Double Pig Tail Stent Placement into Lumen-Apposing Metal Stents Reduce Risks in Eus-Guided Drainage Of Pancreatic Fluid Collections? Endoscopy 2019, 51, S59–S60. Available online: http://www.thieme-connect.de/DOI/DOI?10.1055/s-0039-1681345 (accessed on 25 May 2025).
- Haddad, J.D.; Tielleman, T.; Fuller, A.; Tavakkoli, A.; Vanderveldt, D.; Goldschmiedt, M.; Kubiliun, N.; Sawas, T. Safety and Efficacy of Lumen-Apposing Metal Stents with and Without Coaxial Plastic Stents for Pancreatic Fluid Collections. Tech. Innov. Gastrointest. Endosc. 2023, 25, 113–118. [Google Scholar] [CrossRef]
- Perez Estrada, C.; Adalberto, R.; Candelario Garrido, C. Efficacy and safety of lumen-apposing metal stents in endoscopic ultrasound-guided drainage of abdominal fluid collections and the influence of inserting a coaxial double pigtail plastic stent. United Eur. Gastroenterol. J. 2022, 10, 984–985. [Google Scholar]
- Vanek, P.; Falt, P.; Vitek, P.; Zoundjiekpon, V.; Horinkova, M.; Zapletalova, J.; Lovecek, M.; Urban, O. EUS-guided transluminal drainage using lumen-apposing metal stents with or without coaxial plastic stents for treatment of walled-off necrotizing pancreatitis: A prospective bicentric randomized controlled trial. Gastrointest. Endosc. 2023, 97, 1070–1080. [Google Scholar] [CrossRef] [PubMed]
- Beran, A.; Mohamed, M.F.H.; Abdelfattah, T.; Sarkis, Y.; Montrose, J.; Sayeh, W.; Musallam, R.; Jaber, F.; Elfert, K.; Montalvan-Sanchez, E.; et al. Lumen-Apposing Metal Stent with and Without Concurrent Double-Pigtail Plastic Stent for Pancreatic Fluid Collections: A Comparative Systematic Review and Meta-Analysis. Gastroenterol. Res. 2023, 16, 59–67. [Google Scholar] [CrossRef]
- Giri, S.; Harindranath, S.; Afzalpurkar, S.; Angadi, S.; Sundaram, S. Does a coaxial double pigtail stent reduce adverse events after lumen apposing metal stent placement for pancreatic fluid collections? A systematic review and meta-analysis. Ther. Adv. Gastrointest. Endosc. 2023, 16, 26317745231199364. [Google Scholar] [CrossRef]
- Gopakumar, H. Endoscopic ultrasound-guided lumen-apposing metal stent with or without coaxial plastic stent for pancreatic fluid collections: A systematic review and meta-analysis comparing safety and efficacy. Ann. Gastroenterol. 2024, 37, 242–250. Available online: http://www.annalsgastro.gr/files/journals/1/earlyview/2024/ev-01-2024-03-AG_7242-0858.pdf (accessed on 25 May 2025). [CrossRef]
- AbiMansour, J.; Jaruvongvanich, V.; Velaga, S.; Law, R.; Storm, A.C.; Topazian, M.; Levy, M.J.; Alexander, R.; Vargas, E.J.; Bofill-Garica, A.; et al. Coaxial plastic stent placement within lumen-apposing metal stents for the management of pancreatic fluid collections: A systemic review and meta-analysis. Clin. Endosc. 2024, 57, 595–603. [Google Scholar] [CrossRef]
- Kamal, F.; Khan, M.A.; Lee-Smith, W.; Sharma, S.; Acharya, A.; Farooq, U.; Gangwani, M.K.; Saeed, A.; Aziz, M.; Hayat, U.; et al. EUS-guided Drainage of Pancreatic Fluid Collections Using Lumen Apposing Metal Stents with or Without Coaxial Plastic Stents: A Systematic Review and Meta-analysis. J. Clin. Gastroenterol. 2025, 59, 47–53. [Google Scholar] [CrossRef] [PubMed]
- Capurso, G.; Rizzo, G.E.M.; Coluccio, C.; Crinò, S.F.; Cucchetti, A.; Facciorusso, A.; Hassan, C.; Amato, A.; Auriemma, F.; Bertani, H.; et al. The i-EUS consensus on the management of pancreatic fluid collections—Part 1. Dig. Liver Dis. 2024, 56, 1663–1674. [Google Scholar] [CrossRef] [PubMed]
- Capurso, G.; Coluccio, C.; Rizzo, G.E.M.; Crinò, S.F.; Cucchetti, A.; Facciorusso, A.; Hassan, C.; Amato, A.; Auriemma, F.; Bertani, H.; et al. The 1st i-EUS consensus on the management of pancreatic fluid collections—Part 2. Dig. Liver Dis. 2024, 56, 1819–1827. [Google Scholar] [CrossRef]
- Bang, J.Y.; Hasan, M.; Navaneethan, U.; Hawes, R.; Varadarajulu, S. Lumen-apposing metal stents (LAMS) for pancreatic fluid collection (PFC) drainage: May not be business as usual. Gut 2017, 66, 2054–2056. [Google Scholar] [CrossRef]
- Brimhall, B.; Han, S.; Tatman, P.D.; Clark, T.J.; Wani, S.; Brauer, B.; Edmundowicz, S.; Wagh, M.S.; Attwell, A.; Hammad, H.; et al. Increased Incidence of Pseudoaneurysm Bleeding with Lumen-Apposing Metal Stents Compared to Double-Pigtail Plastic Stents in Patients with Peripancreatic Fluid Collections. Clin. Gastroenterol. Hepatol. Off. Clin. Pract. J. Am. Gastroenterol. Assoc. 2018, 16, 1521–1528. [Google Scholar] [CrossRef]
- Ramai, D.; Facciorusso, A.; DeLuca, M.; Barakat, M.; Adler, D.G. Adverse events associated with AXIOS stents: Insights from the manufacturer and user facility device experience database. Endosc. Ultrasound 2022, 11, 231–236. [Google Scholar] [CrossRef]
- Jo, S.J.; Moon, J.H.; Lee, Y.N.; Park, J.K.; Lee, T.H.; Park, S.-H.; Park, S.I.; Jeong, S.; Lee, D.H. A novel bipolar electrocautery-enhanced delivery system with a lumen-apposing metal stent for EUS-guided drainage: A porcine study. J. Hepato-Biliary-Pancreat. Sci. 2023, 30, 263–268. [Google Scholar] [CrossRef]
- Mangiavillano, B.; Moon, J.H.; Facciorusso, A.; Di Matteo, F.; Paduano, D.; Bulajic, M.; Ofosu, A.; Auriemma, F.; Lamonaca, L.; Yoo, H.W.; et al. EUS-guided biliary drainage with a novel electrocautery-enhanced lumen apposing metal stent as first approach for distal malignant biliary obstruction: A prospective study. Endosc. Int. Open 2022, 10, E998–E1003. [Google Scholar] [CrossRef]
- Teoh, A.Y.B.; Bapaye, A.; Lakhtakia, S.; Ratanachu, T.; Reknimitr, R.; Chan, S.M.; Choi, H.J.; Gadhikar, H.P.; Kongkam, P.; Korrapati, S.K.; et al. Prospective multicenter international study on the outcomes of a newly developed self-approximating lumen-apposing metallic stent for drainage of pancreatic fluid collections and endoscopic necrosectomy. Dig. Endosc. Off. J. Jpn. Gastroenterol. Endosc. Soc. 2020, 32, 391–398. [Google Scholar] [CrossRef]
- Larghi, A.; Crinò, S.F.; Vanella, G.; Rizzatti, G.; Bernardoni, L.; Arcidiacono, P.G. Preliminary experience of EUS-guided pancreatic fluid collections drainage using a new lumen-apposing metal stent mounted on a cautery device. Endosc. Ultrasound 2022, 11, 84–85. [Google Scholar] [CrossRef] [PubMed]
- Mangiavillano, B.; Lakhtakia, S.; Samanta, J.; Auriemma, F.; Vargas-Madrigal, J.; Arcidiacono, P.G.; Barbera, C.; Ashhab, H.; Song, T.J.; Pham, K.D.-K.; et al. Lumen-apposing metal stents for the treatment of pancreatic and peripancreatic fluid collections and bleeding risk: A propensity matched study. Endoscopy 2024, 56, 249–257. [Google Scholar] [PubMed]
- Suresh Kumar, V.C.; Singh, S.; Moond, V.; Mohan, B.P.; Aswath, G.; Khan, H.M.A.; Sapkota, B.; Adler, D.G. Safety and efficacy of lumen-apposing metal stents for endoscopic ultrasound-guided drainage of pancreatic fluid collections: A systematic review and meta-analysis. Endoscopy 2025, 57, 282–290. [Google Scholar] [PubMed]
- Pawa, R.; Dorrell, R.; Russell, G.; Gilliam, J.; Mishra, G.; Pawa, S. Long-term transmural drainage of pancreatic fluid collections with double pigtail stents following lumen-apposing metal stent placement improves recurrence-free survival in disconnected pancreatic duct syndrome. Dig. Endosc. Off. J. Jpn. Gastroenterol. Endosc. Soc. 2022, 34, 1234–1241. [Google Scholar] [CrossRef]
- Bang, J.Y.; Mel Wilcox, C.; Arnoletti, J.P.; Varadarajulu, S. Importance of Disconnected Pancreatic Duct Syndrome in Recurrence of Pancreatic Fluid Collections Initially Drained Using Lumen-Apposing Metal Stents. Clin. Gastroenterol. Hepatol. 2021, 19, 1275–1281.e2. [Google Scholar] [CrossRef] [PubMed]
- Kato, A.; Yoshida, M.; Kito, Y.; Toyohara, T.; Sahashi, H.; Hori, Y.; Kataoka, H. Innovative coaxial plastic stent within a lumen-apposing metal stent to prevent recurrence of pancreatic fluid collection. Endoscopy 2025, 57 (Suppl. 1), E353–E354. [Google Scholar] [CrossRef] [PubMed]
- Vanella, G.; Leone, R.; Frigo, F.; Rossi, G.; Zaccari, P.; Palumbo, D.; Guazzarotti, G.; Aleotti, F.; Pecorelli, N.; Preatoni, P.; et al. Predicting the need for step-up after EUS-guided drainage of peripancreatic fluid collections, including Quadrant-Necrosis-Infection score validation: A prospective cohort study. Gastrointest. Endosc. 2025, 102, 362–372.e8. Available online: https://linkinghub.elsevier.com/retrieve/pii/S0016510725000446 (accessed on 10 August 2025). [CrossRef] [PubMed]
| Study | Year | Study Design | No. of Pts | Type of PFCs | Technique | Clinical Success (%) | Adverse Events (%) | Main Adverse Event | Conclusion |
|---|---|---|---|---|---|---|---|---|---|
| Puga et al. [13]. | 2018 | Retrospective. Single-center | 41 (21 LAMS; 20 coaxial DPPS within the LAMS) | PP and WON | LAMS ± coaxial- DPPS | LAMS 85.7% Coaxial DPPS within the LAMS 90% p > 0.99 | 42.9% (LAMS) vs. 10% (coaxial DPPS within the LAMS) p = 0.04 | Bleeding (LAMS 23.8% vs. coaxial DPPS within the LAMS 5%) p = 0.18 Infection (LAMS 14.3% vs. coaxial DPPS within the LAMS 5%) p = 0.61 | Coaxial DPPS within the LAMS associated with fewer complications |
| AbiMansour et al. [16]. | 2024 | Retrospective. Single-center | 185 (83 LAMS; 102 coaxial DPPS within the LAMS) | ̴ 75% WON ̴ 25% PP | LAMS ± coaxial-DPPS | 15.7% in both groups LAMS: 75.9% Coaxial DPPS within the LAMS: 69.9% p = 0.34 | 15.7 in both groups p = 0.825 | Bleeding: (LAMS 2.4% vs. coaxial DPPS within the LAMS: 8.8%) p = 0.067 Infection (LAMS 7.22% vs. coaxial DPPS within the LAMS 3.92%) p = 0.322 LAMS migration (LAMS 3.61% vs. coaxial DPPS within the LAMS 0.98%) p = 0.220 LAMS occlusion (LAMS 2.40% vs. coaxial DPPS within the LAMS 2.94%) p = 0.825 | No benefit with coaxial DPPS within the LAMS; may help in select cases (e.g., DPDS) |
| Aburajab et al. [14]. | 2018 | Retrospective. Single-center | 47 (24 LAMS; 23 coaxial DPPS within the LAMS) | PP only | LAMS ± coaxial-DPPS | LAMS: 91% Coaxial DPPS within the LAMS: 100% p = 0.24 | NR | Infection: (LAMS 17% vs. coaxial DPPS within the LAMS 0%) p = 0.054 LAMS migration: (LAMS 4% vs. coaxial DPPS within the LAMS 0%) p = 0.50 Perforation: (LAMS 4% vs. coaxial DPPS within the LAMS 0%) p = 0.51 | Coaxial DPPS within the LAMS may reduce infection risk in PPs by blocking food entryway |
| Ali et al. [18]. | 2019 | Retrospective. Single-center | 57 (21 LAMS; 36 coaxial DPPS within the LAMS) | 75.4% WON 34.6% PP | LAMS ± coaxial-DPPS | LAMS: 71.4% Coaxial DPPS within the LAMS: 58.3% p = 0.32 | LAMS: 28.6% Coaxial DPPS within the LAMS: 38.9% p = 0.43 | Stent obstruction > bleeding/migration Bleeding: (LAMS 16.6% vs. coaxial DPPS within the LAMS 14.2%) LAMS occlusion: (LAMS 66.6% vs. coaxial DPPS within the LAMS 42.8%) LAMS migration (LAMS 16.6% vs. coaxial DPPS within the LAMS 42.8%) | No benefit with coaxial DPPS within the LAMS in terms of efficacy or safety |
| Rossi et al. [20]. | 2020 | Retrospective. Single-center (Congress Abstract) | 49 (32 LAMS; 17 coaxial DPPS within the LAMS) | NR | LAMS ± coaxial-DPPS (Hot AXIOS) | 93.9% overall | Overall AEs 16.3% | Bleeding: (LAMS 15.6% vs. coaxial DPPS within the LAMS 5.9%) p = 0.65 | Trend toward less bleeding with coaxial DPPS within the LAMS, though not significant |
| Estrada et al. [22]. | 2022 | Retrospective. Single-center (Abstract) | 70 overall | 64.2% WON 30% PPs 5.8 post-surgical | LAMS ± coaxial-DPPS | LAMS: 87.9% Coaxial DPPS within the LAMS: 100% | AEs LAMS: 24.1% Coaxial DPPS within the LAMS: 11.1% | Bleeding (LAMS: 3.44% coaxial DPPS within the LAMS: 0%) | No significant difference in the AEs rate between the two groups. Subgroup analysis of patients with WON. Coaxial DPPS within the LAMS was associated with significantly less endoscopic revision (p = 0.042) and shorter time to LAMS removal (p < 0.001). |
| Aujla et al. [15]. | 2023 | Retrospective. Single- center (Abstract) | 101 (21 LAMS; 80 coaxial DPPS within the LAMS) | NR | LAMS ± coaxial-DPPS | NR | Overall AEs: LAMS: 47.6% Coaxial DPPS within the LAMS: 17.5% p = 0.01 | Bleeding (LAMS: 28.6% Coaxial DPPS within the LAMS: 5%) p = 0.01 Perforation (LAMS: 9.5% Coaxial DPPS within the LAMS: 1.3%) p = 0.04 Infection (LAMS: 28.6% Coaxial DPPS within the LAMS: 11.3%) p = 0.04 | The overall AEs rate was significantly lower in the coaxial DPPS within the LAMS group (17.5%) compared to the LAMS-only group (47.6%; p = 0.01) |
| Haddad et al. [21]. | 2023 | Retrospective. Bicentric, propensity-matched | 68 (45 LAMS; 23 coaxial DPPS within the LAMS) | 61.8% WON 30.9% PP 7.3% PSFC | LAMS ± coaxial-DPPS | LAMS: 84.4% Coaxial DPPS within the LAMS: 95.7% p = 0.18 | LAMS 28.9% Coaxial DPPS within the LAMS 17.4% p = 0.27 | LAMS occlusion 8.7% vs. 17.8% (p = 0.38) Infection 8.7% vs. 8.9% (p = 0.97) Bleeding 4.4% vs. 6.7% (p = 0.48) LAMS migration 4.4% vs. 8.9% (p = 0.45) | No significant difference in outcomes |
| Shamah et al. [19]. | 2022 | Retrospective. Multicenter | 68 (35 LAMS; 33 coaxial DPPS within the LAMS) | 25% WON 65% PP 10% PSFC | LAMS ± coaxial-DPPS | LAMS: 96% Coaxial DPPS within the LAMS: 83% p = 0.67 | LAMS 30% Coaxial DPPS within the LAMS 26% p = 0.75 | Bleeding (LAMS 9% vs. coaxial DPPS within the LAMS 8%) p = 0.75 Migration (LAMS 9% vs. coaxial DPPS within the LAMS 15%) p = 0.46 Perforation (LAMS 6% vs. coaxial DPPS within the LAMS 2%) p = 0.78 Occlusion (LAMS 6% vs. coaxial DPPS within the LAMS 0%) p = 0.49 | No significant benefit of coaxial DPPS within the LAMS in clinical or safety outcomes |
| Vanek et al. [23]. | 2023 | Prospective. Bicentric RCT | 67 (33 LAMS; 34 coaxial DPPS within the LAMS) | WON | LAMS ± coaxial-DPPS | LAMS: 81.8% Coaxial DPPS within the LAMS: 91.2% p = 0.305 | LAMS 51.5% Coaxial DPPS within the LAMS 20.7% p = 0.008 | Stent occlusion (14.7% vs. 36.3%. p = 0.042) Bleeding (12.1% vs. 5.9%, p = 0.427) LAMS migration (6.1% vs. 0%, p = 0.239) | Coaxial DPPS within the LAMS significantly reduced global AEs and occlusion |
| Study and Year | No. of Studies | No. of Patients | Technical Success | Clinical Success | Overall AEs | Stent Occlusion | Infection | Perforation | Stent Migration | Bleeding | Conclusion |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Beran et al. [24]. | 5 | 281: overall 137: coaxial DPPS within the LAMS 144: LAMS | RR = 1.01 95% Cl: 0.97–1.04 p = 0.70 | RR = 1.01 95% Cl: 0.88–1.17 p = 0.85 | RR = 0.64 95% Cl: 0.32–1.29 Favorable trend towards coaxial DPPS within the LAMS, but not statistically significant, p = 0.22 | RR = 0.63 95% Cl: 0.27–1.49 Favorable trend towards coaxial DPPS within the LAMS, but not statistically significant, p = 0.29 | RR = 0.50 95% Cl: 0.15–1.64 Favorable trend towards coaxial DPPS within the LAMS, but not statistically significant, p = 0.25 | RR = 0.40 95% Cl: 0.06–2.78 Favorable trend towards coaxial DPPS within the LAMS, but not statistically significant, p = 0.42 | RR = 1.29 95% Cl: 0.50–3.34 p = 0.60 | RR = 0.65 95% Cl: 0.25–1.74 p = 0.39 | Coaxial DPPS within the LAMS did not show statistically significant benefits in terms of efficacy or safety |
| Giri et al. [25]. | 8 | 454: overall | NR | RR = 1.00 95% Cl: 0.87–1.14 p = 0.98 | RR = 1.60 95% Cl: 0.95–2.68 p = 0.08 | RR = 1.72 95% Cl: 0.90–3.27 p = 0.10 | RR = 1.78 95% Cl: 0.34–9.47 p = 0.50 | NR | RR = 0.81 95% Cl: 0.33–2.01 p = 0.65 | RR = 1.80 95% Cl: 0.83–3.88 p = 0.14 | Coaxial DPPS within the LAMS was not associated with decreased AEs rates or better clinical outcomes |
| Gopakumar et al. [26]. | 6 | 348 overall 177: LAMS 171: coaxial DPPS within the LAMS | OR: 0.53 (95% CI 0.15–1.83) | OR: 1.10 (0.598–2.05) | OR: 2.22 (1.37–3.59) | NR | NR | NR | OR: 0.95 (0.40–2.23) | OR: 1.84 (0.77–4.38) | Coaxial DPPS within the LAMS can mitigate the overall adverse events observed with LAMS |
| AbiMansour et al. [27] | 9 | 709 overall 388: LAMS 371: coaxial DPPS within the LAMS | OR: 1.08 (0.59–1.96) | OR: 0.96 (0.48–1.89) | OR: 0.57 (0.25–1.29) | OR: 0.53 (0.29–0.96) | OR: 0.53 (0.29–0.96) | NR | OR:1.03 (0.36–2.90) | OR:0.61 (0.22–1.67) | Coaxial DPPS within the LAMS placement with LAMS for PFCs drainage was associated with a reduced risk of LAMS occlusion and PFCs infection |
| Kamal et al. [28]. | 10 | 685 overall | NR | RR = 1.03 95% CI: 0.94–1.13 p = 0.53 | RR = 0.58 95% CI: 0.40, 0.87 p = 0.007 | RR = 0.57 95% CI: 0.31–1.03 p = 0.06 | RR = 0.46 95% CI: 0.24–0.85 p = 0.01 | NR | RR = 0.89 95% CI: 0.38–2.08 p = 0.78 | RR = 0.58 95% CI: 0.26–1.30 p = 0.18 | Addition of coaxial DPPS within the LAMS decreased the risk of AEs (infection) in patients with PFCs |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Published by MDPI on behalf of the Lithuanian University of Health Sciences. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Infantino, G.; Rancatore, G.; Quintini, D.; Carrozza, L.; Ligresti, D.; Giacchetto, M.; Belluardo, N.; Rizzo, G.; D’Amore, E.; Rizzo, G.E.M.; et al. A Critical Narrative Review of Coaxial Double-Pigtail Stenting Within the LAMS in the Management of Pancreatic Fluid Collections. Medicina 2025, 61, 1500. https://doi.org/10.3390/medicina61081500
Infantino G, Rancatore G, Quintini D, Carrozza L, Ligresti D, Giacchetto M, Belluardo N, Rizzo G, D’Amore E, Rizzo GEM, et al. A Critical Narrative Review of Coaxial Double-Pigtail Stenting Within the LAMS in the Management of Pancreatic Fluid Collections. Medicina. 2025; 61(8):1500. https://doi.org/10.3390/medicina61081500
Chicago/Turabian StyleInfantino, Giuseppe, Gabriele Rancatore, Dario Quintini, Lucio Carrozza, Dario Ligresti, Marco Giacchetto, Nicoletta Belluardo, Giuseppe Rizzo, Elio D’Amore, Giacomo Emanuele Maria Rizzo, and et al. 2025. "A Critical Narrative Review of Coaxial Double-Pigtail Stenting Within the LAMS in the Management of Pancreatic Fluid Collections" Medicina 61, no. 8: 1500. https://doi.org/10.3390/medicina61081500
APA StyleInfantino, G., Rancatore, G., Quintini, D., Carrozza, L., Ligresti, D., Giacchetto, M., Belluardo, N., Rizzo, G., D’Amore, E., Rizzo, G. E. M., & Tarantino, I. (2025). A Critical Narrative Review of Coaxial Double-Pigtail Stenting Within the LAMS in the Management of Pancreatic Fluid Collections. Medicina, 61(8), 1500. https://doi.org/10.3390/medicina61081500






