Influence of Diabetes Mellitus on Perioperative Outcomes Following Surgical Stabilization of Rib Fractures: A National Health Insurance Research Database Analysis
Abstract
1. Introduction
2. Methods
2.1. Data Source
2.2. Ethics Statement
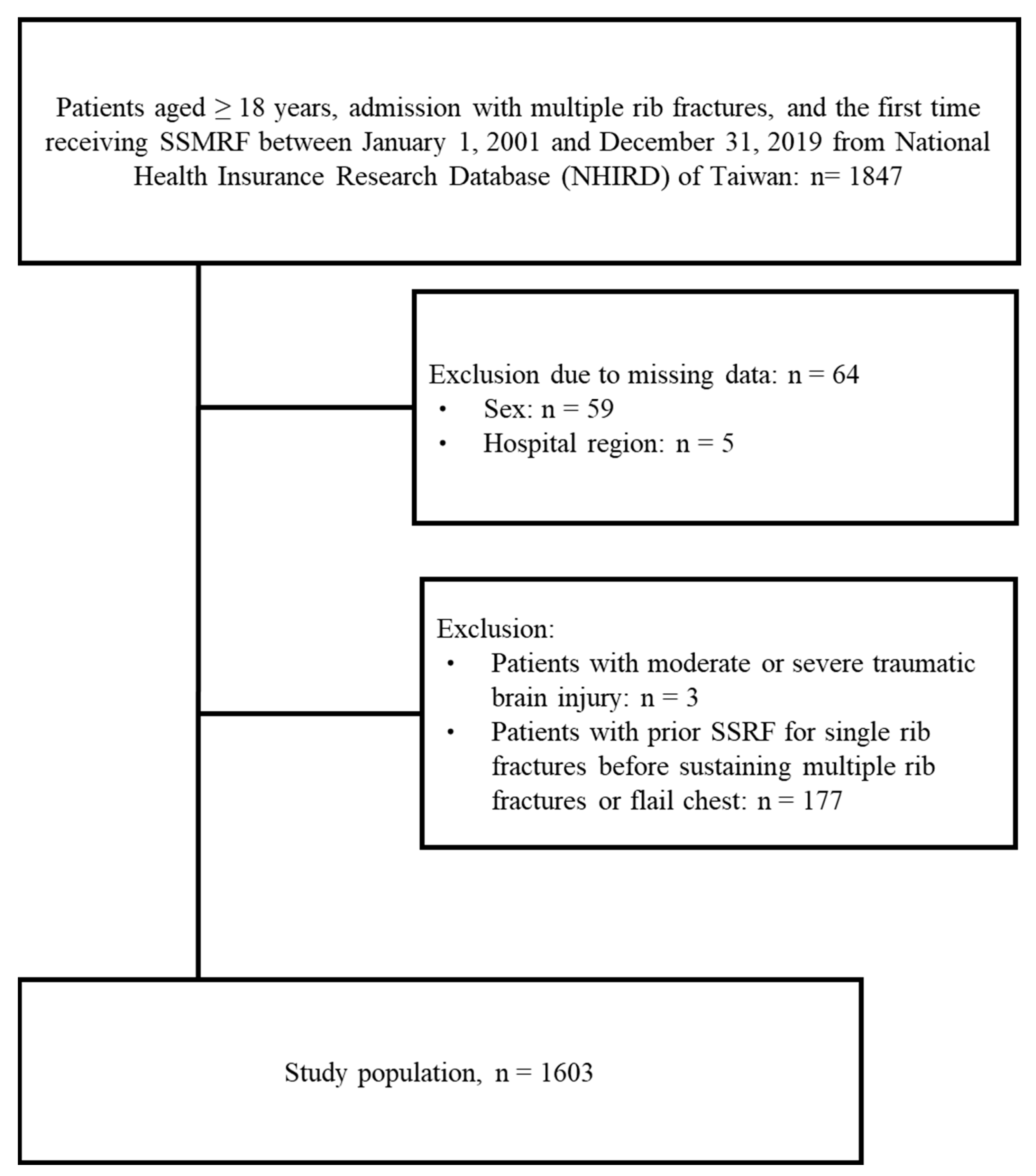
2.3. Study Population
2.4. Study Outcomes and Variables
2.5. Statistical Analysis
3. Results
3.1. Patient Selection
3.2. Patient Characteristics
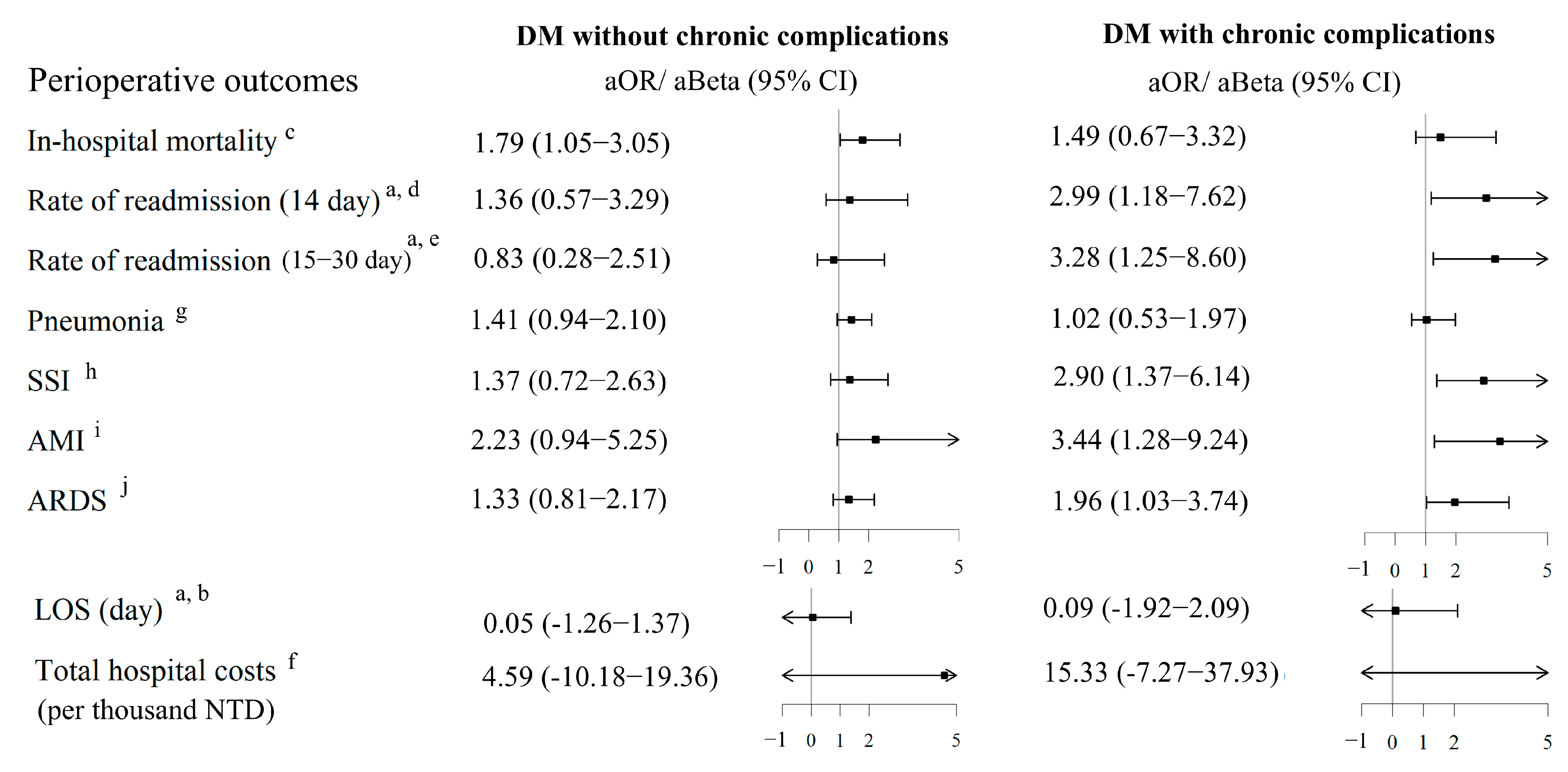
3.3. Associations Between DM and Perioperative Outcomes
4. Discussions
Strengths and Limitations
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Tanios, M.; Brickman, B.; Cage, E.; Abbas, K.; Smith, C.; Atallah, M.; Baroi, S.; Lecka-Czernik, B. Diabetes and Impaired Fracture Healing: A Narrative Review of Recent Literature. Curr. Osteoporos. Rep. 2022, 20, 229–239. [Google Scholar] [CrossRef]
- Jiao, H.; Xiao, E.; Graves, D.T. Diabetes and Its Effect on Bone and Fracture Healing. Curr. Osteoporos. Rep. 2015, 13, 327–335. [Google Scholar] [CrossRef]
- Luc, K.; Schramm-Luc, A.; Guzik, T.J.; Mikolajczyk, T.P. Oxidative stress and inflammatory markers in prediabetes and diabetes. J. Physiol. Pharmacol. 2019, 70, 809–824. [Google Scholar]
- Rehman, K.; Akash, M.S.H. Mechanism of Generation of Oxidative Stress and Pathophysiology of Type 2 Diabetes Mellitus: How Are They Interlinked? J. Cell. Biochem. 2017, 118, 3577–3585. [Google Scholar] [CrossRef]
- Zura, R.; Xiong, Z.; Einhorn, T.; Watson, J.T.; Ostrum, R.F.; Prayson, M.J.; Della Rocca, G.J.; Mehta, S.; McKinley, T.; Wang, Z.; et al. Epidemiology of Fracture Nonunion in 18 Human Bones. JAMA Surg. 2016, 151, e162775. [Google Scholar] [CrossRef]
- Claes, L.; Recknagel, S.; Ignatius, A. Fracture healing under healthy and inflammatory conditions. Nat. Rev. Rheumatol. 2012, 8, 133–143. [Google Scholar] [CrossRef]
- Henderson, S.; Ibe, I.; Cahill, S.; Chung, Y.H.; Lee, F.Y. Bone Quality and Fracture-Healing in Type-1 and Type-2 Diabetes Mellitus. J. Bone Jt. Surg. Am. 2019, 101, 1399–1410. [Google Scholar] [CrossRef]
- Fatima, N.; Faisal, S.M.; Zubair, S.; Ajmal, M.; Siddiqui, S.S.; Moin, S.; Owais, M. Role of Pro-Inflammatory Cytokines and Biochemical Markers in the Pathogenesis of Type 1 Diabetes: Correlation with Age and Glycemic Condition in Diabetic Human Subjects. PLoS ONE 2016, 11, e0161548. [Google Scholar] [CrossRef]
- Devaraj, S.; Venugopal, S.K.; Singh, U.; Jialal, I. Hyperglycemia induces monocytic release of interleukin-6 via induction of protein kinase c-{alpha} and -{beta}. Diabetes 2005, 54, 85–91. [Google Scholar] [CrossRef]
- Kumar, P.; Natarajan, K.; Shanmugam, N. High glucose driven expression of pro-inflammatory cytokine and chemokine genes in lymphocytes: Molecular mechanisms of IL-17 family gene expression. Cell Signal. 2014, 26, 528–539. [Google Scholar] [CrossRef]
- Tanaka, N.; Yonekura, H.; Yamagishi, S.; Fujimori, H.; Yamamoto, Y.; Yamamoto, H. The receptor for advanced glycation end products is induced by the glycation products themselves and tumor necrosis factor-alpha through nuclear factor-kappa B, and by 17beta-estradiol through Sp-1 in human vascular endothelial cells. J. Biol. Chem. 2000, 275, 25781–25790. [Google Scholar] [CrossRef]
- Bragdon, B.C.; Bahney, C.S. Origin of Reparative Stem Cells in Fracture Healing. Curr. Osteoporos. Rep. 2018, 16, 490–503. [Google Scholar] [CrossRef]
- Lafage-Proust, M.H.; Roche, B.; Langer, M.; Cleret, D.; Vanden Bossche, A.; Olivier, T.; Vico, L. Assessment of bone vascularization and its role in bone remodeling. BoneKEy Rep. 2015, 4, 662. [Google Scholar] [CrossRef]
- Pieracci, F.M. Completely thoracoscopic surgical stabilization of rib fractures: Can it be done and is it worth it? J. Thorac. Dis. 2019, 11, S1061–S1069. [Google Scholar] [CrossRef]
- Bethlahmy, J.M.; Hanst, B.A.; Giafaglione, S.M.; Elia, J.M. Perioperative considerations for patients undergoing surgical stabilization of rib fractures: A narrative review. J. Clin. Anesth. 2023, 91, 111275. [Google Scholar] [CrossRef]
- Pieracci, F.M.; Leasia, K.; Bauman, Z.; Eriksson, E.A.; Lottenberg, L.; Majercik, S.; Powell, L.; Sarani, B.; Semon, G.; Thomas, B.; et al. A multicenter, prospective, controlled clinical trial of surgical stabilization of rib fractures in patients with severe, nonflail fracture patterns (Chest Wall Injury Society NONFLAIL). J. Trauma Acute Care Surg. 2020, 88, 249–257. [Google Scholar] [CrossRef]
- Simmonds, A.; Smolen, J.; Ciurash, M.; Alexander, K.; Alwatari, Y.; Wolfe, L.; Whelan, J.F.; Bennett, J.; Leichtle, S.W.; Aboutanos, M.B.; et al. Early surgical stabilization of rib fractures for flail chest is associated with improved patient outcomes: An ACS-TQIP review. J. Trauma Acute Care Surg. 2023, 94, 532–537. [Google Scholar] [CrossRef]
- Loewenstern, J.; Kessler, R.A.; Caridi, J. Diabetes Comorbidity Increases Risk of Postoperative Complications in Traumatic Thoracic Vertebral Fracture Repair: A Propensity Score Matched Analysis. World Neurosurg. 2019, 121, e792–e797. [Google Scholar] [CrossRef]
- Murray-Ramcharan, M.; Valdivieso, S.; Mohamed, I.; Altonen, B.; Safavi, A. Outcomes of surgical stabilization of rib fractures in a minority population: Retrospective analysis of a case series from an acute care facility. JTCVS Open 2023, 14, 581–589. [Google Scholar] [CrossRef]
- American Diabetes Association. 14. Diabetes Care in the Hospital: Standards of Medical Care in Diabetes-2018. Diabetes Care 2018, 41, S144–S151. [Google Scholar] [CrossRef]
- CPOC. Guideline for Perioperative Care for People with Diabetes Mellitus Undergoing Elective and Emergency Surgery. 2022. Available online: https://www.cpoc.org.uk/sites/cpoc/files/documents/2022-12/CPOC-Diabetes-Guideline-Updated2022.pdf (accessed on 25 June 2025).
- American Diabetes Association. Standards of Medical Care in Diabetes-2016 Abridged for Primary Care Providers. Clin. Diabetes. 2016, 34, 3–21. [Google Scholar] [CrossRef]
- Hsieh, C.Y.; Su, C.C.; Shao, S.C.; Sung, S.F.; Lin, S.J.; Kao Yang, Y.H.; Lai, E.C. Taiwan’s National Health Insurance Research Database: Past and future. Clin. Epidemiol. 2019, 11, 349–358. [Google Scholar] [CrossRef]
- Olland, A.; Puyraveau, M.; Guinard, S.; Seitlinger, J.; Kadoche, D.; Perrier, S.; Renaud, S.; Falcoz, P.E.; Massard, G. Surgical stabilization for multiple rib fractures: Whom the benefit? -a prospective observational study. J. Thorac. Dis. 2019, 11, S130–S140. [Google Scholar] [CrossRef]
- Wang, Z.; Jia, Y.; Li, M. The effectiveness of early surgical stabilization for multiple rib fractures: A multicenter randomized controlled trial. J. Cardiothorac. Surg. 2023, 18, 118. [Google Scholar] [CrossRef]
- Liu, Y.F.; Chen, T.L.; Tseng, C.H.; Wang, J.Y.; Wang, W.C. Impact of obesity on outcomes after surgical stabilization of multiple rib fractures: Evidence from the US nationwide inpatient sample. PLoS ONE 2024, 19, e0299256. [Google Scholar] [CrossRef]
- Demir, S.; Nawroth, P.P.; Herzig, S.; Ekim Üstünel, B. Emerging Targets in Type 2 Diabetes and Diabetic Complications. Adv. Sci. 2021, 8, e2100275. [Google Scholar] [CrossRef]
- Le, T.; Salas Sanchez, A.; Nashawi, D.; Kulkarni, S.; Prisby, R.D. Diabetes and the Microvasculature of the Bone and Marrow. Curr. Osteoporos. Rep. 2024, 22, 11–27. [Google Scholar] [CrossRef]
- Murray, C.E.; Coleman, C.M. Impact of Diabetes Mellitus on Bone Health. Int. J. Mol. Sci. 2019, 20, 4873. [Google Scholar] [CrossRef]
- Ding, Z.C.; Zeng, W.N.; Rong, X.; Liang, Z.M.; Zhou, Z.K. Do patients with diabetes have an increased risk of impaired fracture healing? A systematic review and meta-analysis. ANZ J. Surg. 2020, 90, 1259–1264. [Google Scholar] [CrossRef]
- Gortler, H.; Rusyn, J.; Godbout, C.; Chahal, J.; Schemitsch, E.H.; Nauth, A. Diabetes and Healing Outcomes in Lower Extremity Fractures: A Systematic Review. Injury 2018, 49, 177–183. [Google Scholar] [CrossRef]
- Marin, C.; Luyten, F.P.; Van der Schueren, B.; Kerckhofs, G.; Vandamme, K. The Impact of Type 2 Diabetes on Bone Fracture Healing. Front. Endocrinol. 2018, 9, 6. [Google Scholar] [CrossRef]
- Ricci, W.M.; Streubel, P.N.; Morshed, S.; Collinge, C.A.; Nork, S.E.; Gardner, M.J. Risk factors for failure of locked plate fixation of distal femur fractures: An analysis of 335 cases. J. Orthop. Trauma 2014, 28, 83–89. [Google Scholar] [CrossRef]
- Adegbala, O.; Martin, K.D.; Otuada, D.; Akinyemiju, T. Diabetes Mellitus with Chronic Complications in Relation to Carotid Endarterectomy and Carotid Artery Stenting Outcomes. J. Stroke Cerebrovasc. Dis. 2017, 26, 217–224. [Google Scholar] [CrossRef]
- Wang, G.; Yang, F.; Zhou, W.; Xiao, N.; Luo, M.; Tang, Z. The initiation of oxidative stress and therapeutic strategies in wound healing. Biomed. Pharmacother. 2023, 157, 114004. [Google Scholar] [CrossRef]
- Moris, D.; Spartalis, M.; Spartalis, E.; Karachaliou, G.S.; Karaolanis, G.I.; Tsourouflis, G.; Tsilimigras, D.I.; Tzatzaki, E.; Theocharis, S. The role of reactive oxygen species in the pathophysiology of cardiovascular diseases and the clinical significance of myocardial redox. Ann. Transl. Med. 2017, 5, 326. [Google Scholar] [CrossRef]
- Kellner, M.; Noonepalle, S.; Lu, Q.; Srivastava, A.; Zemskov, E.; Black, S.M. ROS Signaling in the Pathogenesis of Acute Lung Injury (ALI) and Acute Respiratory Distress Syndrome (ARDS). Adv. Exp. Med. Biol. 2017, 967, 105–137. [Google Scholar]
- Liu, J.W.; Ahn, J.; Raspovic, K.M.; Liu, G.T.; Nakonezny, P.A.; Lavery, L.A.; Wukich, D.K. Increased Rates of Readmission, Reoperation, and Mortality Following Open Reduction and Internal Fixation of Ankle Fractures Are Associated with Diabetes Mellitus. J. Foot Ankle Surg. 2019, 58, 470–474. [Google Scholar] [CrossRef]
- Moser, J.; Mensink, R.; Onrust, M.; Blokzijl, F.; Koeze, J. Unveiling the hidden burden: The impact of undiagnosed comorbidities on health-related quality of life in ICU survivors. Crit. Care 2024, 28, 229. [Google Scholar] [CrossRef]
- Freedman, M.K.; Hilibrand, A.S.; Blood, E.A.; Zhao, W.; Albert, T.J.; Vaccaro, A.R.; Oleson, C.V.; Morgan, T.S.; Weinstein, J.N. The impact of diabetes on the outcomes of surgical and nonsurgical treatment of patients in the spine patient outcomes research trial. Spine 2011, 36, 290–307. [Google Scholar] [CrossRef]
- American Diabetes Association. Standards of medical care for patients with diabetes mellitus. Diabetes Care 2003, 26 (Suppl. S1), S33–S50. [Google Scholar] [CrossRef]
- Chen, J.Y.; Nassereldine, H.; Cook, S.B.; Thornblade, L.W.; Dellinger, E.P.; Flum, D.R. Paradoxical Association of Hyperglycemia and Surgical Complications Among Patients with and Without Diabetes. JAMA Surg. 2022, 157, 765–770. [Google Scholar] [CrossRef]
- Jang, S.A.; Min Kim, K.; Jin Kang, H.; Heo, S.J.; Sik Kim, C.; Won Park, S. Higher mortality and longer length of stay in hospitalized patients with newly diagnosed diabetes. Diabetes Res. Clin. Pract. 2024, 210, 111601. [Google Scholar] [CrossRef]
- Wan, E.Y.F.; Fung, C.S.C.; Jiao, F.F.; Yu, E.Y.T.; Chin, W.Y.; Fong, D.Y.T.; Wong, C.K.H.; Chan, A.K.C.; Chan, K.H.Y.; Kwok, R.L.P.; et al. Five-Year Effectiveness of the Multidisciplinary Risk Assessment and Management Programme-Diabetes Mellitus (RAMP-DM) on Diabetes-Related Complications and Health Service Uses-A Population-Based and Propensity-Matched Cohort Study. Diabetes Care 2018, 41, 49–59. [Google Scholar] [CrossRef]
- Dogra, P.; Anastasopoulou, C.; Jialal, I. Diabetic Perioperative Management. In StatPearls; StatPearls Publishing: Florida, FL, USA, 2024. [Google Scholar]
- Forrester, J.D.; Sarani, B.; Forssten, M.P.; Cao, Y.; Hildebrand, F.; Mohammad Ismail, A.; Ribeiro, M.A.F., Jr.; Mohseni, S. Time to surgical stabilization of rib fractures: Does it impact outcomes? Trauma Surg. Acute Care Open 2024, 9, e001233. [Google Scholar] [CrossRef]
| Total (n = 1603) | Without DM | DM Without Chronic Complications | DM with Chronic Complications | p | |
|---|---|---|---|---|---|
| (n = 1312) | (n = 209) | (n = 82) | |||
| Demography | |||||
| Age, years | 52.0 (44.0–61.0) | 51.0 (42.0–59.0) | 58.0 (51.0–65.0) | 62.5 (55.0–69.0) | <0.001 |
| 18–39 | 254 (15.8) | 243 (18.5) | 8 (3.8) | 3 (3.7) | <0.001 |
| 40–59 | 876 (54.6) | 742 (56.6) | 106 (50.7) | 28 (34.1) | |
| ≥60 | 473 (29.5) | 327 (24.9) | 95 (45.5) | 51 (62.2) | |
| Sex | 0.815 | ||||
| Male | 1131 (70.6) | 926 (70.6) | 145 (69.4) | 60 (73.2) | |
| Female | 472 (29.4) | 386 (29.4) | 64 (30.6) | 22 (26.8) | |
| Monthly income, TWD a | 0.004 | ||||
| >25,000 | 349 (21.8) | 309 (23.6) | 27 (12.9) | 13 (15.9) | |
| 20,000–25,000 | 155 (9.7) | 119 (9.1) | 25 (12.0) | 11 (13.4) | |
| <20,000 | 1099 (68.6) | 884 (67.4) | 157 (75.1) | 58 (70.7) | |
| Flail chest | 48 (3.0) | 34 (2.6) | 10 (4.8) | 4 (4.9) | 0.133 |
| Hospital region | 0.490 | ||||
| Urban | 834 (52.0) | 680 (51.8) | 115 (55.0) | 39 (47.6) | |
| Non-urban | 769 (48.0) | 632 (48.2) | 94 (45.0) | 43 (52.4) | |
| Number of Comorbidities | <0.001 | ||||
| 0 | 898 (56.0) | 834 (63.6) | 55 (26.3) | 9 (11.0) | |
| 1 | 380 (23.7) | 282 (21.5) | 73 (34.9) | 25 (30.5) | |
| 2 | 183 (11.4) | 107 (8.2) | 49 (23.4) | 27 (32.9) | |
| 3+ | 142 (8.9) | 89 (6.8) | 32 (15.3) | 21 (25.6) | |
| Comorbidities | |||||
| Hypertension | 484 (30.2) | 303 (23.1) | 119 (56.9) | 62 (75.6) | <0.001 |
| Ischemic heart disease | 231 (14.4) | 140 (10.7) | 56 (26.8) | 35 (42.7) | <0.001 |
| Congestive heart failure | 75 (4.7) | 46 (3.5) | 19 (9.1) | 10 (12.2) | <0.001 |
| Anemia | 83 (5.2) | 60 (4.6) | 16 (7.7) | 7 (8.5) | 0.065 |
| COPD | 212 (13.2) | 151 (11.5) | 43 (20.6) | 18 (22.0) | <0.001 |
| Rheumatic disease | 60 (3.7) | 42 (3.2) | 12 (5.7) | 6 (7.3) | 0.043 |
| Any malignancy | 73 (4.6) | 48 (3.7) | 16 (7.7) | 9 (11.0) | 0.001 |
| Perioperative Outcomes | Total (n = 1603) | Without DM | DM Without Chronic Complications | DM with Chronic Complications | p |
|---|---|---|---|---|---|
| (n = 1312) | (n = 209) | (n = 82) | |||
| LOS, day a | 8.0 (5.0–12.0) | 8.0 (5.0–11.0) | 9.0 (5.0–13.0) | 8.0 (5.0–13.0) | 0.088 |
| In-hospital mortality | 92 (5.7) | 63 (4.8) | 21 (10.0) | 8 (9.8) | 0.003 |
| Rate of readmission (14 day) a | 42 (2.8) | 28 (2.2) | 7 (3.7) | 7 (9.5) | 0.001 |
| Rate of readmission (15–30 day) a | 35 (2.3) | 24 (1.9) | 4 (2.1) | 7 (9.5) | 0.002 |
| Total hospital costs, per thousand TWD | 40.9 (28.8–86.6) | 39.3 (28.6–81.3) | 47.2 (30.6–108.7) | 46.8 (32.0–130.4) | 0.001 |
| Pneumonia | 204 (12.7) | 154 (11.7) | 38 (18.2) | 12 (14.6) | 0.030 |
| SSI | 74 (4.6) | 53 (4.0) | 12 (5.7) | 9 (11.0) | 0.010 |
| AMI | 34 (2.1) | 18 (1.4) | 9 (4.3) | 7 (8.5) | <0.001 |
| ARDS | 136 (8.5) | 96 (7.3) | 25 (12.0) | 15 (18.3) | <0.001 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Published by MDPI on behalf of the Lithuanian University of Health Sciences. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Liu, Y.-F.; Chen, T.-L.; Guo, J.-W.; Liu, S.-C.; Wang, W.-C. Influence of Diabetes Mellitus on Perioperative Outcomes Following Surgical Stabilization of Rib Fractures: A National Health Insurance Research Database Analysis. Medicina 2025, 61, 1358. https://doi.org/10.3390/medicina61081358
Liu Y-F, Chen T-L, Guo J-W, Liu S-C, Wang W-C. Influence of Diabetes Mellitus on Perioperative Outcomes Following Surgical Stabilization of Rib Fractures: A National Health Insurance Research Database Analysis. Medicina. 2025; 61(8):1358. https://doi.org/10.3390/medicina61081358
Chicago/Turabian StyleLiu, Yang-Fan, Te-Li Chen, Jian-Wei Guo, Shih-Ching Liu, and Wen-Ching Wang. 2025. "Influence of Diabetes Mellitus on Perioperative Outcomes Following Surgical Stabilization of Rib Fractures: A National Health Insurance Research Database Analysis" Medicina 61, no. 8: 1358. https://doi.org/10.3390/medicina61081358
APA StyleLiu, Y.-F., Chen, T.-L., Guo, J.-W., Liu, S.-C., & Wang, W.-C. (2025). Influence of Diabetes Mellitus on Perioperative Outcomes Following Surgical Stabilization of Rib Fractures: A National Health Insurance Research Database Analysis. Medicina, 61(8), 1358. https://doi.org/10.3390/medicina61081358





