Effectiveness and Safety of Acupuncture for Nausea and Vomiting in Cancer Patients: A Systematic Review and Meta-Analysis
Abstract
1. Introduction
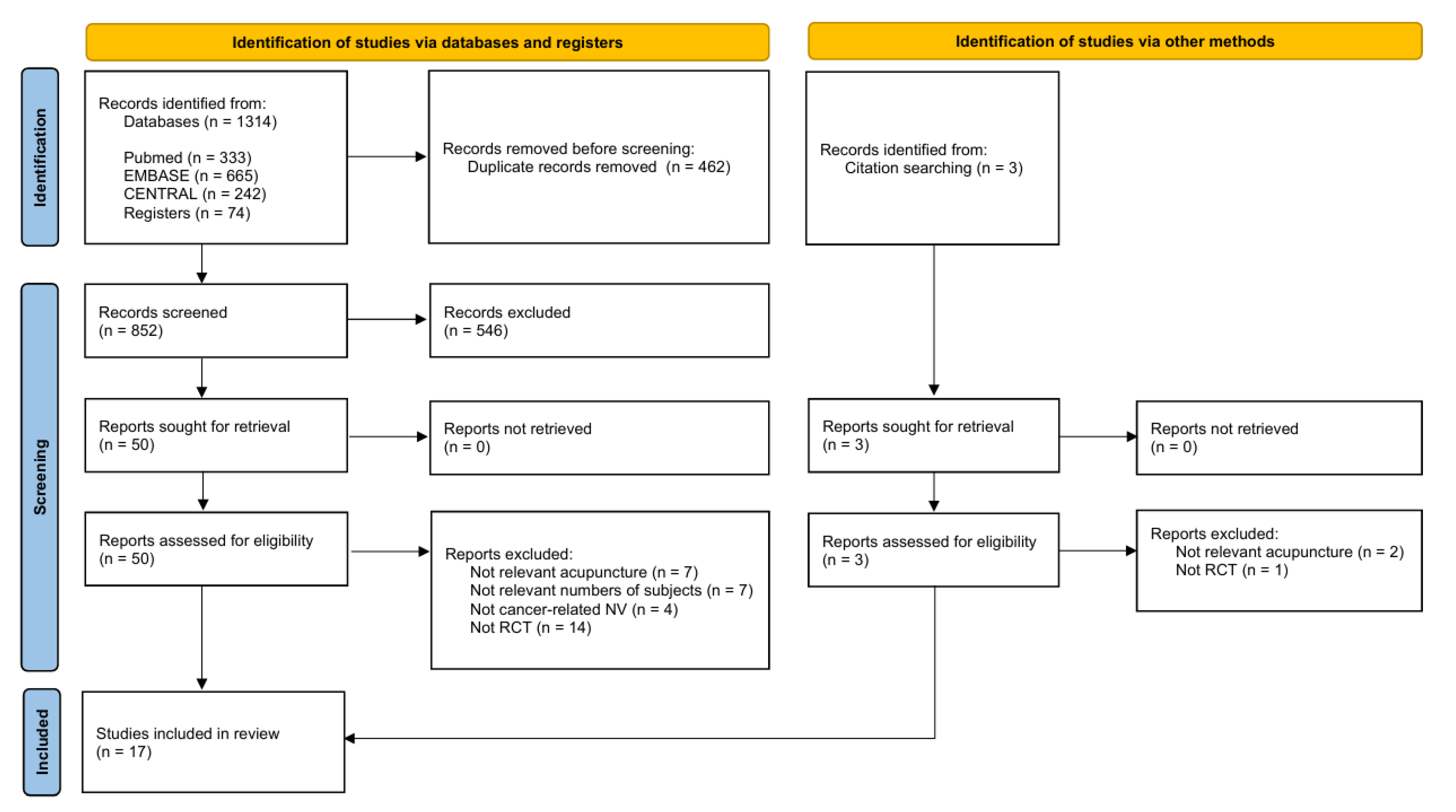
2. Materials and Methods
2.1. Criteria for Inclusion and Exclusion
2.1.1. Types of Studies
2.1.2. Types of Participants
2.1.3. Types of Interventions
2.1.4. Types of Comparators
2.1.5. Types of Outcome Measures
2.2. Literature Searches
2.3. Data Selection
2.4. Data Extraction
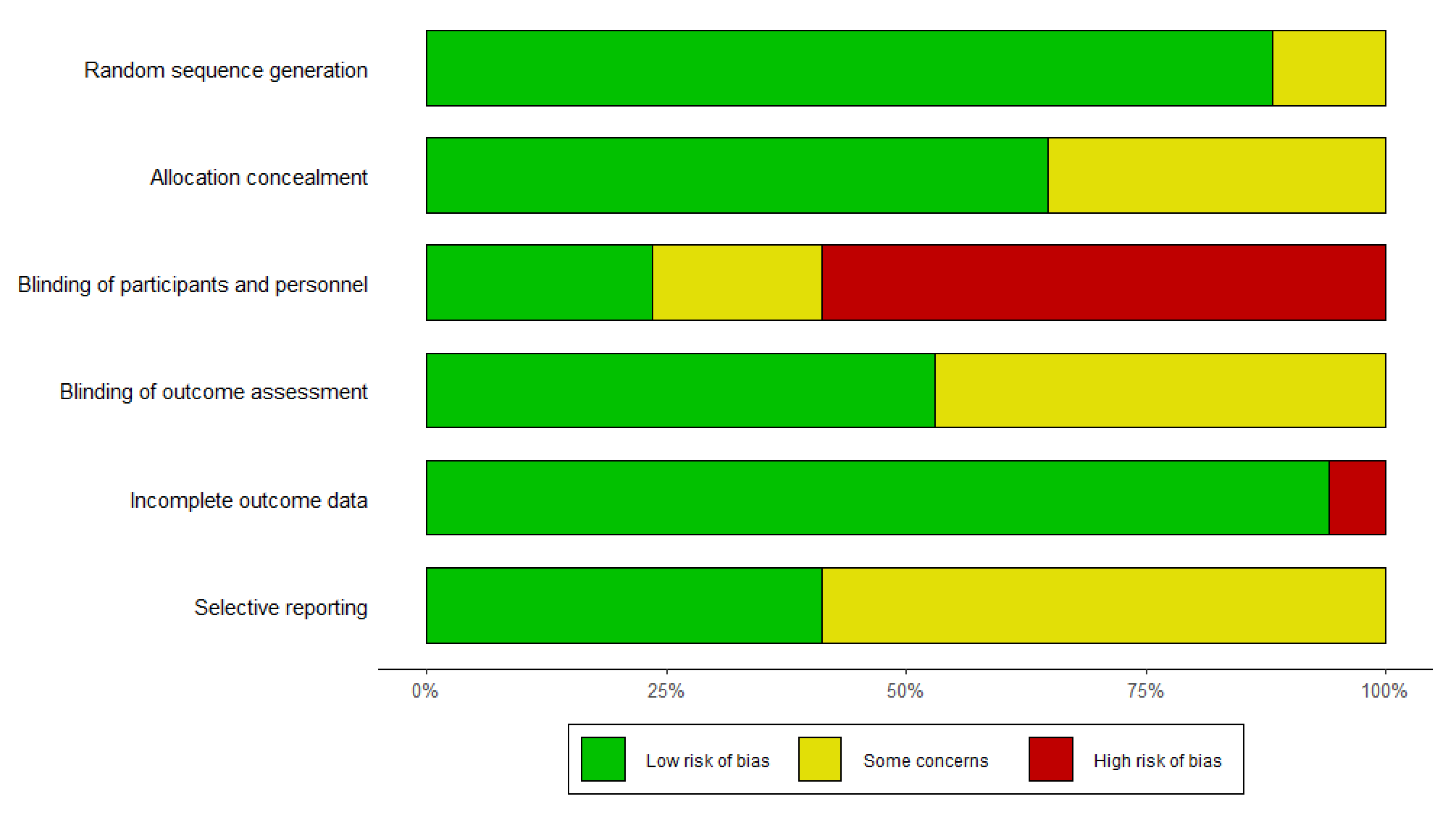
2.5. Quality Assessment of Included Studies
2.6. Data Analysis
3. Results
3.1. Study Characteristics
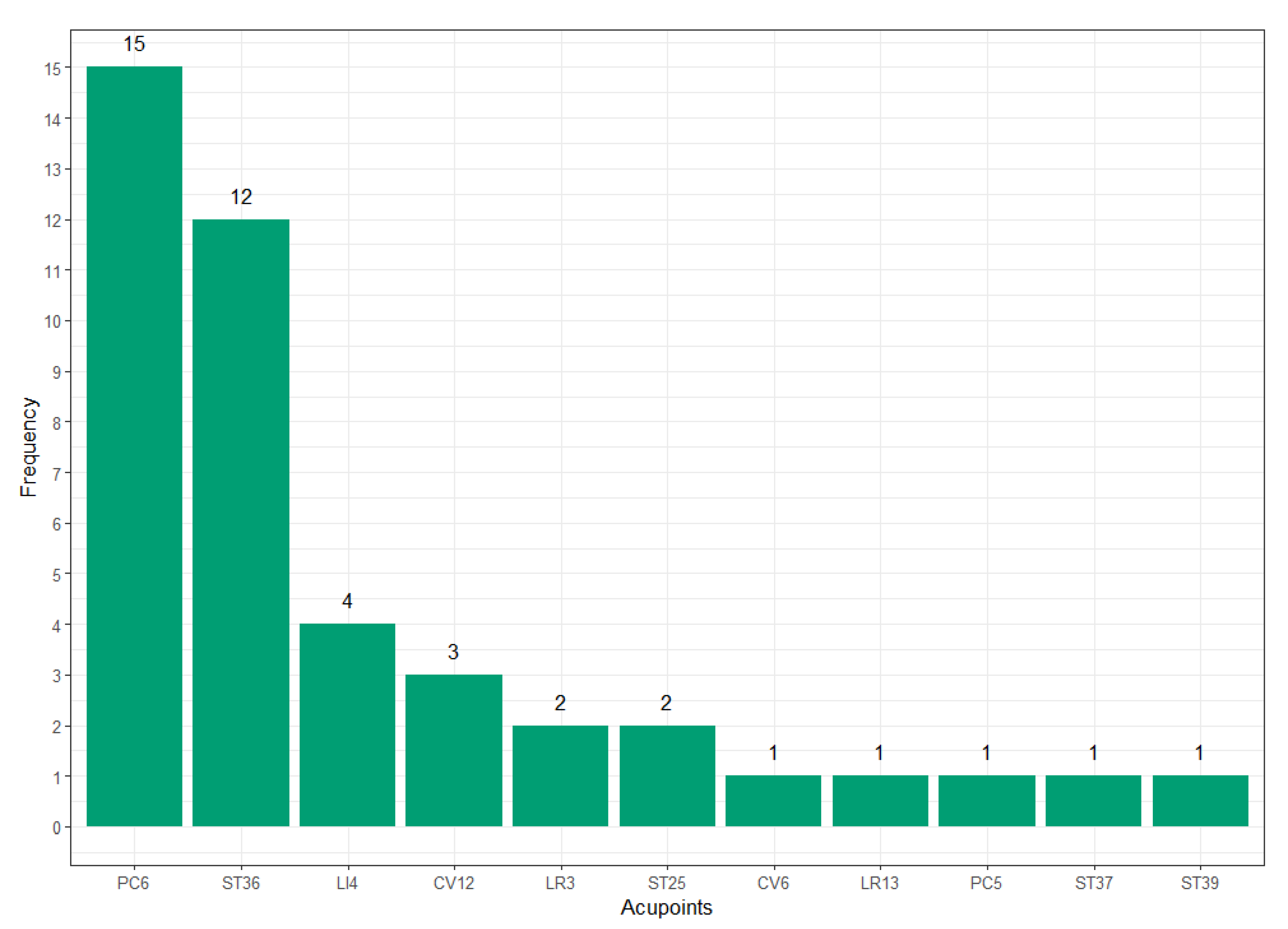
3.2. Acupuncture Treatment Protocol Analysis
3.3. Quality of Included Studies
3.4. Effects of Acupuncture on Nausea
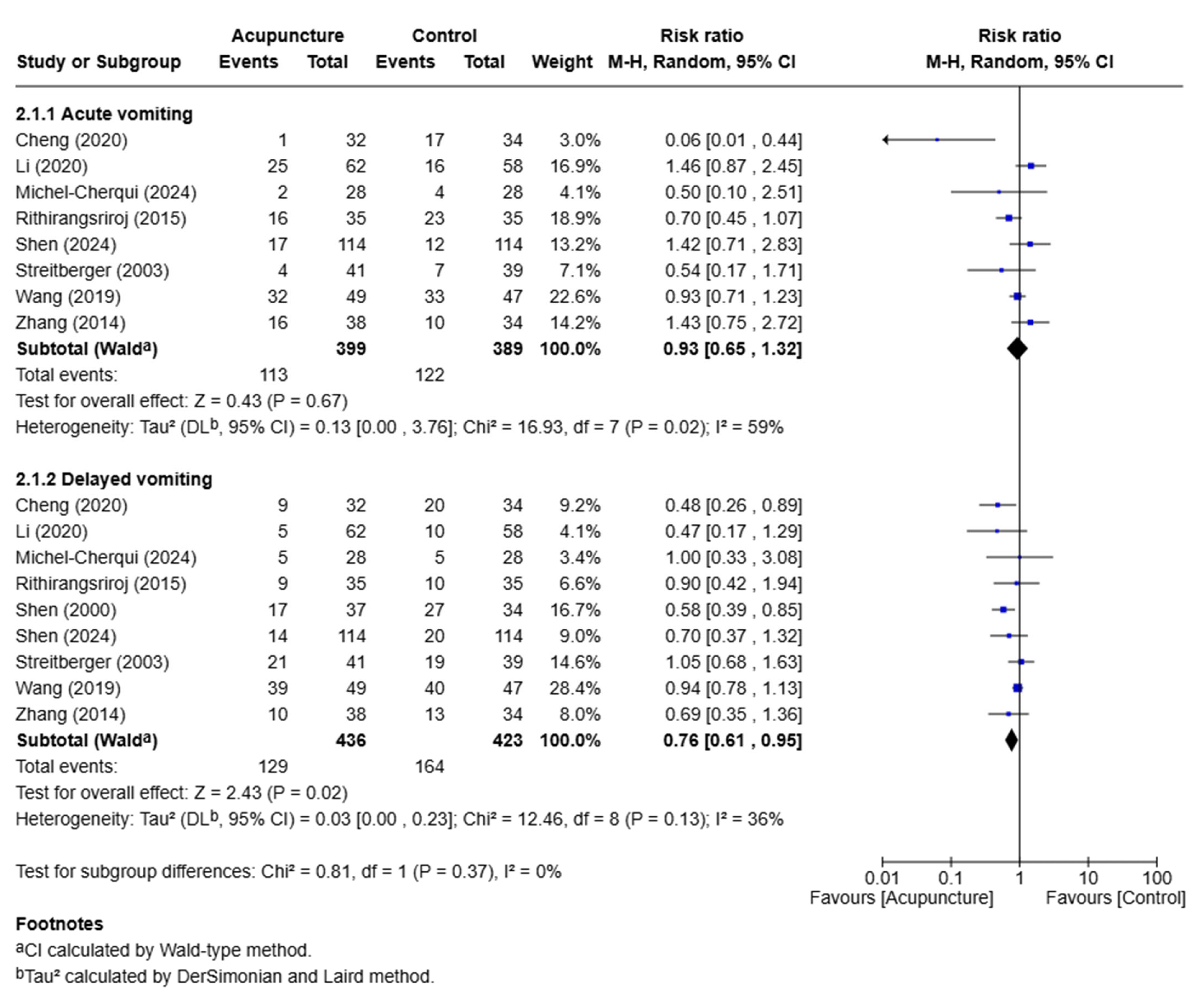
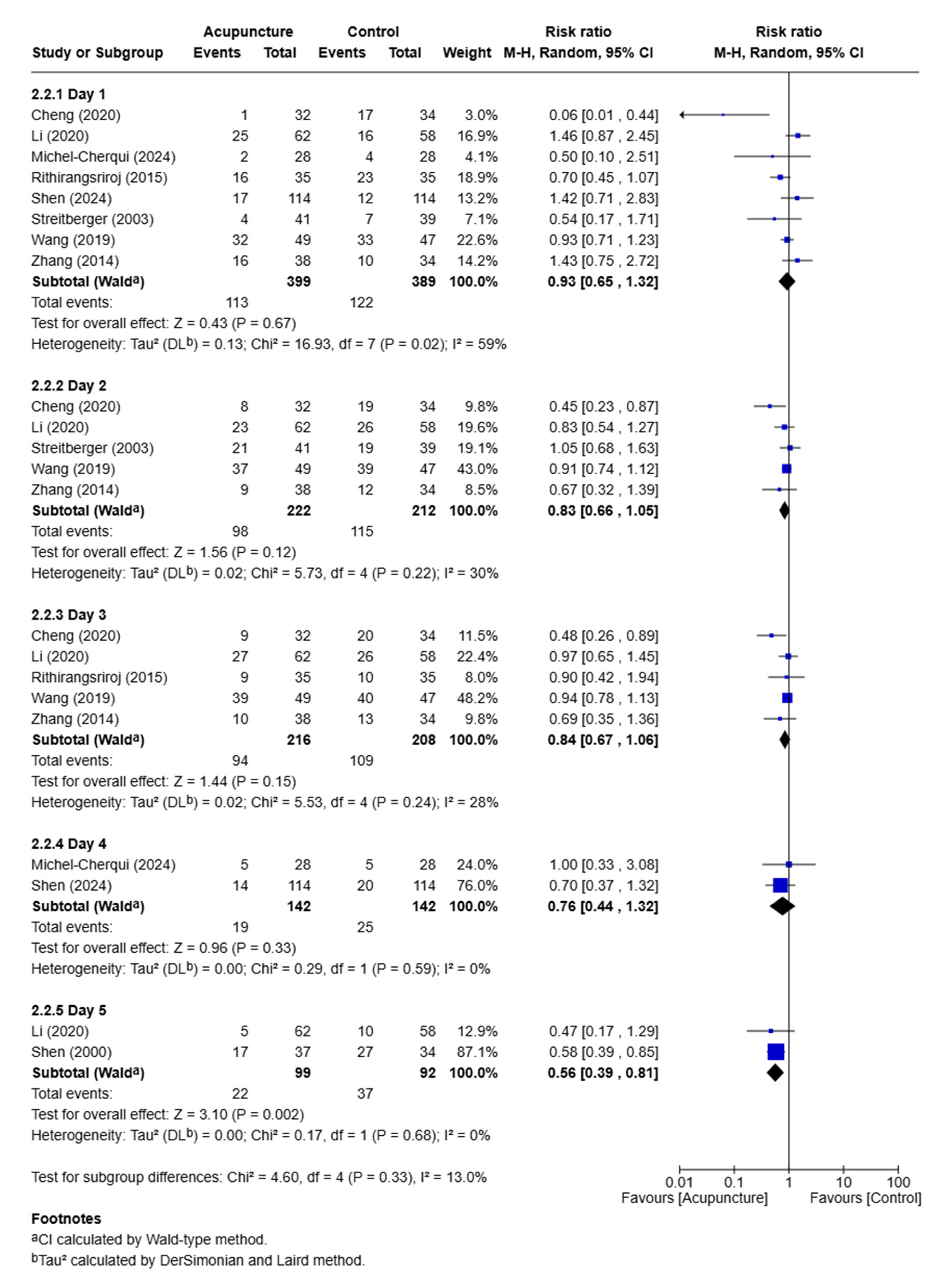
3.5. Effects of Acupuncture on Vomiting
3.6. Safety of Acupuncture
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Appendix A
| PC6 | On the anterior aspect of the forearm, between the tendons of the palmaris longus and the flexor carpi radialis, 2 cun proximal to the palmar wrist crease. With the fist clenched, the wrist supinated and the elbow slightly flexed, the two tendons become more prominent. PC6 is located 2 cun proximal to PC7. The posterior point corresponding to PC6 is TE5. |
| ST36 | On the anterior aspect of the leg, on the line connecting ST35 with ST41, 3 cun inferior to ST35. ST36 is located on the tibialis anterior muscle. |
| CV12 | On the upper abdomen, 4 cun superior to the center of the umbilicus, on the anterior median line. CV12 is located at the midpoint of the line connecting the xiphisternal junction and the center of umbilicus. |
| LI4 | On the dorsum of the hand, radial to the midpoint of the second metacarpal bone. |
| LR3 | On the dorsum of the foot, between the first and second metatarsal bones, in the depression distal to the junction of the bases of the two bones, over the dorsalis pedis artery. LR3 can be felt in the depression when moving proximally from LR2 in the gap between the first and second metatarsal bones towards the base of two metatarsal bones. |
| ST25 | On the upper abdomen, 2 cun lateral to the center of the umbilicus. |
| CV6 | On the lower abdomen, 1.5 cun inferior to the center of the umbilicus, on the anterior median line. |
| LR13 | On the lateral abdomen, inferior to the free extremity of the 11th rib. LR13 can be located while the subject is lying on the side with the shoulder flexed. The free extremity of the 11th rib can be palpated below the inferior border of the costal arch. |
| PC5 | On the anterior aspect of the forearm, between the tendons of the palmaris longus and the flexor carpi radialis, 3 cun proximal to the palmar wrist crease. With the fist clenched, the wrist supinated and the elbow slightly flexed, the two tendons become more prominent. PC5 is located 3 cun proximal to PC7. |
| ST37 | On the anterior aspect of the leg, on the line connecting ST35 with ST41, 6 cun inferior to ST35. ST37 is located on the tibialis anterior muscle. |
| ST39 | On the anterior aspect of the leg, on the line connecting ST35 with ST41, 9 cun inferior to ST35. ST39 is located on the tibialis anterior muscle, at the same level as GB35 and GB36. |
| Grade 1 (Mild) | Grade 2 (Moderate) | Grade 3~5 | |||||
|---|---|---|---|---|---|---|---|
| Intervention | Control | Intervention | Control | Intervention | Control | ||
| Constipation | 19 | 33 | 0 | 0 | 0 | 0 | |
| Diarrhea | 2 | 9 | 0 | 0 | 0 | 0 | |
| Dizziness | 8 | 5 | 0 | 0 | 0 | 0 | |
| Dyspepsia | 8 | 7 | 0 | 0 | 0 | 0 | |
| Electric shock sensation | 1 | 0 | 0 | 0 | 0 | 0 | |
| Headache | 9 | 10 | 0 | 0 | 0 | 0 | |
| Insomnia | 2 | 11 | 0 | 0 | 0 | 0 | |
| Localized bleeding around needle points | 78 | 10 | 0 | 0 | 0 | 0 | |
| Localized skin irritation | 5 | 0 | 0 | 0 | 0 | 0 | |
| Needle scratch | 0 | 10 | 0 | 0 | 0 | 0 | |
| Needling pain | 26 | 0 | 0 | 0 | 0 | 0 | |
| Symptom aggravation | |||||||
| Symptoms of CINV (e.g., tingling sensation) | 12 | 1 | 17 | 22 | 0 | 0 | |
| Increased Alanine transaminase (ALT) | 0 | 1 | 0 | 0 | 0 | 0 | |
| Increased urea nitrogen and creatinine | 1 | 0 | 0 | 0 | 0 | 0 | |
| Sedation | 6 | 4 | 0 | 0 | 0 | 0 | |
| Tiredness | 15 | 15 | 0 | 0 | 0 | 0 | |
| Not mentioned | 0 | 0 | 0 | 0 | 4 | 1 | |
| Total | 192 | 116 | 17 | 22 | 4 | 1 | |
References
- Morran, C.; Smith, D.C.; Anderson, D.A.; McArdle, C.S. Incidence of nausea and vomiting with cytotoxic chemotherapy: A prospective randomised trial of antiemetics. Br. Med. J. 1979, 1, 1323–1324. [Google Scholar] [CrossRef]
- Bossi, P.; Airoldi, M.; Aloe Spiriti, M.A.; Antonuzzo, A.; Bonciarelli, G.; Campagna, A.; Cassano, A.; Murialdo, R.; Musio, D.; Silvano, G. A multidisciplinary expert opinion on CINV and RINV, unmet needs and practical real-life approaches. Expert. Opin. Drug Saf. 2020, 19, 187–204. [Google Scholar] [CrossRef]
- Berger, M.J.; Ettinger, D.S.; Aston, J.; Barbour, S.; Bergsbaken, J.; Bierman, P.J.; Brandt, D.; Dolan, D.E.; Ellis, G.; Kim, E.J. NCCN guidelines insights: Antiemesis, version 2.2017. J. Natl. Compr. Cancer Netw. 2017, 15, 883–893. [Google Scholar] [CrossRef]
- Keefe, D.L. The cardiotoxic potential of the 5-HT(3) receptor antagonist antiemetics: Is there cause for concern? Oncologist 2002, 7, 65–72. [Google Scholar] [CrossRef]
- Samuels, N. Acupuncture for nausea: How does it work? Harefuah 2003, 142, 297–300, 316. [Google Scholar]
- Streitberger, K.; Ezzo, J.; Schneider, A. Acupuncture for nausea and vomiting: An update of clinical and experimental studies. Auton. Neurosci. 2006, 129, 107–117. [Google Scholar] [CrossRef]
- Stöckigt, D.m.B.; Kirschbaum, B.; Carstensen, D.m.M.; Witt, D.m.C.M.; Brinkhaus, D.m.B. Prophylactic acupuncture treatment during chemotherapy in patients with breast cancer–results of a qualitative study nested in a randomized pragmatic trial. Integr. Cancer Ther. 2021, 20, 15347354211058207. [Google Scholar] [CrossRef]
- Höxtermann, M.D.; Haller, H.; Aboudamaah, S.; Bachemir, A.; Dobos, G.; Cramer, H.; Voiss, P. Safety of acupuncture in oncology: A systematic review and meta-analysis of randomized controlled trials. Cancer 2022, 128, 2159–2173. [Google Scholar] [CrossRef]
- Kong, F.; Wang, Z.; Wang, N.; Zhao, L.; Mei, Q.; Yu, Y.; Zhang, D.; Li, X.; Jia, Y. The clinical observation of acupuncture combined with antiemetic drugs in the prevention and treatment of CINV in breast cancer patients. Front. Oncol. 2022, 12, 888651. [Google Scholar] [CrossRef]
- Martínez García, E.; Nishishinya Aquino, M.B.; Cruz Martínez, O.; Ren, Y.; Xia, R.; Fei, Y.; Fernández-Jané, C. Efficacy and Safety of Acupuncture and Related Techniques in the Management of Oncological Children and Adolescent Patients: A Systematic Review. Cancers 2024, 16, 3197. [Google Scholar] [CrossRef]
- Kim, S.-A.; Lim, S.; Won, T.; Yeo, S. Acupuncture for cancer patients with nausea and vomiting: A protocol for systematic review and meta-analysis. Medicine 2023, 102, e31478. [Google Scholar] [CrossRef]
- MacPherson, H.; Altman, D.G.; Hammerschlag, R.; Youping, L.; Taixiang, W.; White, A.; Moher, D. Revised standards for reporting interventions in clinical trials of acupuncture (STRICTA): Extending the CONSORT statement. J. Altern. Complement. Med. 2010, 16, ST-1–ST-14. [Google Scholar] [CrossRef]
- Cumpston, M.; Li, T.; Page, M.J.; Chandler, J.; Welch, V.A.; Higgins, J.P.; Thomas, J. Updated guidance for trusted systematic reviews: A new edition of the Cochrane Handbook for Systematic Reviews of Interventions. Cochrane Database Syst. Rev. 2019, 10, ED000142. [Google Scholar] [CrossRef] [PubMed]
- Chandler, J.; Cumpston, M.; Li, T.; Page, M.J.; Welch, V. Cochrane Handbook for Systematic Reviews of Interventions; Wiley: Hoboken, NJ, USA, 2019; Volume 4. [Google Scholar]
- Shah, S. Common terminology criteria for adverse events. Natl. Cancer Inst. USA 2022, 784, 785. [Google Scholar]
- Shen, J.; Wenger, N.; Glaspy, J.; Hays, R.D.; Albert, P.S.; Choi, C.; Shekelle, P.G. Electroacupuncture for control of myeloablative chemotherapy-induced emesis: A randomized controlled trial. JAMA 2000, 284, 2755–2761. [Google Scholar] [CrossRef] [PubMed]
- Streitberger, K.; Friedrich-Rust, M.; Bardenheuer, H.; Unnebrink, K.; Windeler, J.r.; Goldschmidt, H.; Egerer, G. Effect of acupuncture compared with placebo-acupuncture at P6 as additional antiemetic prophylaxis in high-dose chemotherapy and autologous peripheral blood stem cell transplantation: A randomized controlled single-blind trial. Clin. Cancer Res. 2003, 9, 2538–2544. [Google Scholar]
- Mehling, W.E.; Jacobs, B.; Acree, M.; Wilson, L.; Bostrom, A.; West, J.; Acquah, J.; Burns, B.; Chapman, J.; Hecht, F.M. Symptom Management with Massage and Acupuncture in Postoperative Cancer Patients: A Randomized Controlled Trial. J. Pain Symptom Manag. 2007, 33, 258–266. [Google Scholar] [CrossRef]
- Yang, Y.; Zhang, Y.; Jing, N.; Lu, Y.; Xiao, H.; Xu, G.; Wang, X.; Wang, L.; Zhang, Y.; Zhang, D. Electroacupuncture at Zusanli (ST 36) for treatment of nausea and vomiting caused by the chemotherapy of the malignant tumor: A multicentral randomized controlled trial. Zhongguo Zhen Jiu Chin. Acupunct. Moxibustion 2009, 29, 955–958. [Google Scholar]
- Enblom, A.; Johnsson, A.; Hammar, M.; Onelöv, E.; Steineck, G.; Börjeson, S. Acupuncture compared with placebo acupuncture in radiotherapy-induced nausea-A randomized controlled study. Ann. Oncol. 2012, 23, 1353–1361. [Google Scholar] [CrossRef]
- Beith, J.M.; Oh, B.; Chatfield, M.D.; Davis, E.; Venkateswaran, R. Electroacupuncture for nausea, vomiting, and myelosuppression in women receiving adjuvant Chemotherapy for Early Breast Cancer: A Randomized Controlled Pilot Trial. Med. Acupunct. 2012, 24, 241–248. [Google Scholar] [CrossRef]
- Zhang, X.; Fan, Y. Effects of electroacupuncture on chemotherapy-induced nausea and vomiting and its mechanism. Zhongguo Zhen Jiu Chin. Acupunct. Moxibustion 2014, 34, 1061–1064. [Google Scholar]
- McKeon, C.; Smith, C.A.; Gibbons, K.; Hardy, J.; Haugstetter, C.; Anderson, H. EA versus sham acupuncture and no acupuncture for the control of acute and delayed chemotherapy-induced nausea and vomiting: A pilot study. Acupunct. Med. J. Br. Med. Acupunct. Soc. 2015, 33, 277–283. [Google Scholar] [CrossRef]
- Rithirangsriroj, K.; Manchana, T.; Akkayagorn, L. Efficacy of acupuncture in prevention of delayed chemotherapy induced nausea and vomiting in gynecologic cancer patients. Gynecol. Oncol. 2015, 136, 82–86. [Google Scholar] [CrossRef]
- Wang, T.Y.; Meng, J.H.; Mai, S.C. Electroacupuncture Treatment Conduced Before and After Surgery Is Better in Promoting Reco-very of Gastrointestinal Function in Colorectal Cancer Patients Undergoing Radical Resection. Zhen Ci Yan Jiu Acupunct. Res. 2018, 43, 797–800. [Google Scholar] [CrossRef]
- Wang, Y.L.; Li, J.X.; Guo, X.Q.; Fu, R.Y.; Guan, X.J. Effect of acupuncture in different time on nausea and vomiting induced by chemotherapy of lung cancer. Zhongguo Zhen Jiu Chin. Acupunct. Moxibust. 2019, 39, 1269–1273. [Google Scholar] [CrossRef]
- Li, Q.-W.; Yu, M.-W.; Wang, X.-M.; Yang, G.-W.; Wang, H.; Zhang, C.-X.; Xue, N.; Xu, W.-R.; Zhang, Y.; Cheng, P.-Y. Efficacy of acupuncture in the prevention and treatment of chemotherapy-induced nausea and vomiting in patients with advanced cancer: A multi-center, single-blind, randomized, sham-controlled clinical research. Chin. Med. 2020, 15, 57. [Google Scholar] [CrossRef] [PubMed]
- Cheng, P.; Wang, X. The effects of acupuncture at different intervention time points on nausea and vomiting caused by cisplatin chemotherapy in patients with lung cancer. Int. J. Clin. Exp. Med. 2020, 13, 7965–7971. [Google Scholar]
- Maeng, C.H.; Lee, S.; Han, J.J.; Kim, H.J.; Nam, D.; Lee, J.; Baek, S.K. Effect of Acupuncture on Delayed Emesis for the Patients Who Received High-Emetogenic Chemotherapy with Standard Antiemetic Prophylaxis (KHMC-HO-01): An Open-Label, Randomized Study. Evid. Based Complement. Altern. Med. 2022, 2022, 688727. [Google Scholar] [CrossRef]
- Bintoro, D.A.; Nareswari, I.; Andriastuti, M. Efficacy of Press Needle at PC6 Neiguan and ST36 Zusanli as Adjuvant Therapy in Reducing Symptoms of Chemotherapy-Induced Nausea and Vomiting in Pediatric Cancer Patients Undergoing Chemotherapy. Med. Acupunct. 2022, 34, 123–130. [Google Scholar] [CrossRef]
- Michel-Cherqui, M.; Ma, S.; Bacrie, J.; Huguet, S.; Lemaire, N.; Le Guen, M.; Fischler, M. Auriculotherapy and acupuncture treatments for chemotherapy-induced nausea and vomiting: A multicenter clinical trial. Support. Care Cancer 2024, 32, 560. [Google Scholar] [CrossRef]
- Shen, G.; Ren, D.; Zhao, F.; Wang, M.; Liu, Z.; Feng, X.; He, Y.; Liu, X.; Ling, X.; Zhao, Y.; et al. Effect of Adding Electroacupuncture to Standard Triple Antiemetic Therapy on Chemotherapy-Induced Nausea and Vomiting: A Randomized Controlled Clinical Trial. J. Clin. Oncol. 2024, 42, 4051–4059. [Google Scholar] [CrossRef]
- World Health Organization, Regional Office for the Western Pacific. WHO Standard Acupuncture Point Locations in the Western Pacific Region; World Health Organization: Geneva, Switzerland, 2008. [Google Scholar]
- Yan, Y.; López-Alcalde, J.; Zhang, L.; Siebenhüner, A.R.; Witt, C.M.; Barth, J. Acupuncture for the prevention of chemotherapy-induced nausea and vomiting in cancer patients: A systematic review and meta-analysis. Cancer Med. 2023, 12, 12504–12517. [Google Scholar] [CrossRef]
- Navari, R.M.; Aapro, M. Antiemetic prophylaxis for chemotherapy-induced nausea and vomiting. N. Engl. J. Med. 2016, 374, 1356–1367. [Google Scholar] [CrossRef]
- Rapoport, B.L. Delayed chemotherapy-induced nausea and vomiting: Pathogenesis, incidence, and current management. Front. Pharmacol. 2017, 8, 19. [Google Scholar] [CrossRef] [PubMed]
- Lee, E.J.; Warden, S. The effects of acupuncture on serotonin metabolism. Eur. J. Integr. Med. 2016, 8, 355–367. [Google Scholar] [CrossRef]
- Takahashi, T. Mechanism of acupuncture on neuromodulation in the gut—A review. Neuromodulation Technol. Neural Interface 2011, 14, 8–12. [Google Scholar] [CrossRef] [PubMed]
- Zhang, J.; Zhang, Z.; Huang, S.; Qiu, X.; Lao, L.; Huang, Y.; Zhang, Z.-J. Acupuncture for cancer-related insomnia: A systematic review and meta-analysis. Phytomedicine 2022, 102, 154160. [Google Scholar] [CrossRef] [PubMed]
- Moon, H.; Ryu, Y.; Lee, I.-S.; Chae, Y. Acupuncture treatment for functional gastrointestinal disorders: Identification of major acupoints using network analysis. Integr. Med. Res. 2023, 12, 100970. [Google Scholar] [CrossRef]
- Liu, S.; Wang, Z.; Su, Y.; Qi, L.; Yang, W.; Fu, M.; Jing, X.; Wang, Y.; Ma, Q. A neuroanatomical basis for electroacupuncture to drive the vagal–adrenal axis. Nature 2021, 598, 641–645. [Google Scholar] [CrossRef]
- Mosa, A.S.M.; Hossain, A.M.; Lavoie, B.J.; Yoo, I. Patient-Related Risk Factors for Chemotherapy-Induced Nausea and Vomiting: A Systematic Review. Front. Pharmacol. 2020, 11, 329. [Google Scholar] [CrossRef]
- Jang, A.; Brown, C.; Lamoury, G.; Morgia, M.; Boyle, F.; Marr, I.; Clarke, S.; Back, M.; Oh, B. The effects of acupuncture on cancer-related fatigue: Updated systematic review and meta-analysis. Integr. Cancer Ther. 2020, 19, 1534735420949679. [Google Scholar] [CrossRef]
- Chan, M.W.; Wu, X.Y.; Wu, J.C.; Wong, S.Y.; Chung, V.C. Safety of acupuncture: Overview of systematic reviews. Sci. Rep. 2017, 7, 3369. [Google Scholar] [CrossRef]
- Bauer, M.; McDonald, J.L.; Saunders, N. Is acupuncture dose dependent? Ramifications of acupuncture treatment dose within clinical practice and trials. Integr. Med. Res. 2020, 9, 21–27. [Google Scholar] [CrossRef]
- Roscoe, J.A.; Morrow, G.R.; Aapro, M.S.; Molassiotis, A.; Olver, I. Anticipatory nausea and vomiting. Support. Care Cancer 2011, 19, 1533–1538. [Google Scholar] [CrossRef]
- Bang, H.; Ni, L.; Davis, C.E. Assessment of blinding in clinical trials. Control. Clin. Trials 2004, 25, 143–156. [Google Scholar] [CrossRef]

| Author Year | Country | Cancer Type | Cause of NV | Sample Size | Mean Age (years) | Intervention | Control | Outcome Measures | Main Findings | Adverse Events |
|---|---|---|---|---|---|---|---|---|---|---|
| Shen 2000 [16] | USA | Breast cancer | Chemotherapy (Cyclophosphamide, cisplatin, carmustine) | 104 | 46 | EA + PT | (1) SEA + PT (2) PT | Episodes of vomiting | Adjunct EA was more effective in controlling emesis than minimal needling or antiemetic pharmacotherapy alone although the observed effect had a limited duration. | Minor adverse events (electrical shock sensation, tingling sensation aggravation) |
| Streitberger 2003 [17] | Germany | Multiple myeloma, breast cancer, hodgkin lymphoma, etc. | Chemotherapy (mainly melphalan), BSCT | 80 | 54 | AT + PT | SA + PT | Number of patients with NV, vomiting, episodes of NV | AT has no additional effect for the prevention of acute NV in high-dose chemotherapy. | None observed |
| Mehling 2007 [18] | USA | Abdominal/pelvic, prostate/testicular, bladder/kidney, breast cancer | Surgery | 138 | 56 | AT + Massage | Usual care+ Massage | NRS | A bedside service of massage and AT resulted in decreased pain and depressive mood among postoperative cancer patients when compared with usual care alone. | Not mentioned |
| Yang 2009 [19] | China | Diverse cancer (not reported) | Chemotherapy | 246 | 51 | EA + PT | PT | Effective rate, NRS | EA at ST36 can significantly alleviate the symptoms such as NV caused by chemotherapy of the patients. | Minor adverse events (bleeding around acupoints) |
| Enblom 2012 [20] | Sweden | Gynecologic, colon, rectal, anal, testicular cancer, etc. | Radiotherapy | 324 | 54 | AT + PT | SA + PT | Episodes of NV | AT is not more effective than sham in radiotherapy-induced nausea, but in this study, nearly all patients in both groups experienced that the treatment was effective for nausea. | Minor adverse events (bleeding around acupoints, tiredness, dizziness, needle scratch on skin) |
| Beith 2012 [21] | Australia | Breast cancer | Chemotherapy (Doxorubicin, cyclophosphamide, others) | 32 | 52 | EA + PT | SEA + PT | MAT, episodes of NV, number of patients with NV | EA during chemotherapy is a promising option for controlling the side effects of chemotherapy. | None observed |
| Zhang 2014 [22] | China | Lung, colon, breast cancer, etc. | Chemotherapy | 72 | 59 | EA + PT | SEA + PT | Episodes of NV, complete control rate | EA at PC6 and PC5 combined with Granisetron could obviously relieve nausea in chemotherapy patients at the delay stage. | None observed |
| McKeon 2015 [23] | Australia | Breast, colorectal, gynecological cancer, etc. | Chemotherapy | 60 | 58 | EA + PT | (1) SEA + PT (2) PT | FLIE, NRS, episodes of nausea and vomiting | It was not possible to determine whether EA improved CINV compared to standard care. | Minor adverse events (needling pain, bruising, localized skin irritation) |
| Rithirangsriroj 2015 [24] | Thailand | Gynecologic cancer | Chemotherapy (Paclitaxel, carboplatin) | 70 | 52 | AT + PT | PT | Complete response rate, functional assessment of cancer therapy-general | AT is effective in preventing delayed CINV and promoting a better quality of life with fewer adverse effects. | Minor adverse events (needling pain, soreness) |
| Wang 2018 [25] | China | Colorectal cancer | Surgery | 80 | 51 | EA (1) 1 sessions of treatment (2) 2 sessions of treatment (3) 3 sessions of treatment | No treatment | Number of patients with nausea, vomiting | EA treatment combined with intravenous anesthesia conducted before and after surgery is effective in promoting the recovery of gastrointestinal function in patients undergoing colorectal cancer laparotomy and is obviously better than simple pre-operative EA. | None observed |
| Wang 2019 [26] | China | Lung cancer | Chemotherapy | 140 | 54 | AT + PT (1) before chemotherapy (2) after chemotherapy | PT | Effective rate, Karnofsky performance scale | AT combined with the slow intravenous injection of Tropisetron hydrochloride achieves a satisfactory effect in prevention and treatment. AT before chemotherapy greatly improves the effect on the NV induced by chemotherapy of lung cancer. | Minor adverse events (dizziness) |
| Li 2020 [27] | China | Breast, ovarian, cervical, endometrial, lung cancer, etc. | Chemotherapy (Cisplatinum, anthracycline, taxane) | 134 | 59 | EA + PT | SEA + PT | Complete control rate, common terminology criteria for adverse events | AT as an adjunctive approach could alleviate the severity of CINV compared to the sham control, even though the effect of AT in preventing CINV occurrence is relatively modest. | None observed |
| Cheng 2020 [28] | China | Lung cancer | Chemotherapy (cisplatin) | 100 | 59 | AT + PT (1) before chemotherapy (2) after chemotherapy | PT | Complete control rate, INVR, national cancer institute common toxicity criteria 4.0 | AT before chemotherapy can effectively reduce the frequency of NV associated with cisplatin chemotherapy in lung cancer patients, improve the effectiveness of CINV treatment, and be widely promoted in clinics. | Not mentioned |
| Maeng 2022 [29] | Republic of Korea | Solid tumor | Chemotherapy (Cisplatin, doxorubicin, cyclophosphamide) | 42 | 64 | AT + PT | PT | RINVR, MAT | Delayed nausea after highly emetogenic chemotherapy tended to decrease with AT using the RINVR score, though it was also not significant. With the MAT assessment, delayed NV was significantly improved with AT, suggesting a promising effect of AT. | None observed |
| Bintoro 2022 [30] | Indonesia | Leukemia, renal, liver cancer, etc. | Chemotherapy | 60 | 11 | IA + PT | SIA + PT | RINVR | IA treatment is able to reduce the RINVR score and can be applied to pediatric patients because of its minimal side effects. | None observed |
| Michel-Cherqui 2024 [31] | France | Solid tumor | Chemotherapy | 115 | 64 | IA | Usual care | Number of patients with nausea, vomiting, MAT | IA treatment reduces intensity of acute and delayed nausea in patients treated by optimal antiemetic treatment. | Minor adverse events (discomfort) |
| Shen 2024 [32] | China | Breast cancer | Chemotherapy | 239 | 51 | EA + PT | SEA + PT | Complete control rate, VAS | Adding EA to standard triple antiemetic therapy significantly enhances the efficacy of CINV treatment in patients with breast cancer receiving highly emetogenic chemotherapy. | One discontinuation. Minor adverse events (bruising) |
| Author Year | Names of Acupoints | Number of Needle Insertions | Depth of Insertion (mm) | Needle Type | Needle Stimulation | Needle Retention Time | Number of Treatment Sessions | Treatment Time | Setting and Context of Treatment | Description of Participating Acupuncturists |
|---|---|---|---|---|---|---|---|---|---|---|
| Shen 2000 [16] | PC6, ST36 | 4 | 30~45 | 36-gauge (Seirin, Shizuoka, Japan) | Electrical (2~10 Hz, <26 mA), De qi (rotation) | 20 min | 5 | 2 h before chemotherapy | Inpatient (oncology center at a university medical center) | Acupuncture clinician with 3 and 20 years of acupuncture training |
| Streitberger 2003 [17] | PC6 | 2 | NM | 0.25 × 40 mm (Asia med, Pullach im Isartal, Germany) | Manual, De qi | 20 min | 2 | 30 min before chemotherapy | University of Heidelberg | Two trained acupuncturists |
| Mehling 2007 [18] | PC6, ST36, additional points according to patients | 4~14 | 3~90 | 34-gauge (Seirin, Shizuoka, Japan) | Manual, De qi | 20 min | 2 | 1, 2 days after surgery | University of California, San Francisco | Two licensed acupuncturists |
| Yang 2009 [19] | ST36 | 2 | 25~30 | 0.30 × 40 mm | Electrical (NM), De qi (rotation) | 30 min | 10 | 30 min before chemotherapy | Jilin Hospital at Changchun, China | NM |
| Enblom 2012 [20] | PC6 | 2 | 15 | 0.30 × 40 mm (Dongbang, Seongnam, Republic of Korea) | Manual, De qi (twirling and lifting) | 30 min | 12 | Before or after the radiotherapy session | Two Swedish university hospitals | Seven acupuncture-trained physiotherapists with experience (range 2–12 years) |
| Beith 2012 [21] | PC6, ST36, LI4, | 4 | NM | 0.20 × 25 mm (Viva, China) | Electrical (2 Hz, for a 1.5-s duration pulse width), De qi (rotation) | 20 min | 4 | 2 h before chemotherapy (each first, second cycles of chemotherapy) | Oncology clinic at the Royal Prince Alfred Hospital, Australia | Two acupuncturists with more than 6 years of training and 10 years of experience |
| Zhang 2014 [22] | PC6, PC5 | 4 | 13~23 | 0.30 × 25 mm (Jiangsu med, Changzhou, China.) | Electrical (20 Hz, 0~10 mA), De qi | 60 min | 6 | 30 min before chemotherapy | Inpatient of first affiliated hospital of China medical university, Zhejiang, China | NM |
| McKeon 2015 [23] | PC6, ST36, LI4, LR3 | 8 | 2~15 | 0.20 × 30 mm (Sensei, Melbourne, Australia) | Electrical (10 Hz, <10 mA), De qi (thrusting, twirling) | 30 min | 2 | 10 min before chemotherapy | Mater Health Services Adults Day Oncology Unit, Brisbane, Australia | A trained acupuncturist with an advanced diploma of acupuncture with 6 years of clinical practice at the time of the study |
| Rithirangsriroj 2015 [24] | PC6 | 2 | NM | NM | Manual, De qi (rotation) | 30 min | 2 | 30 min before chemotherapy | King Chulalongkorn Memorial Hospital Bangkok, Thailand | A third author of this study |
| Wang 2018 [25] | PC6, ST36, ST37, ST39 (+CV12, ST25) | 6 | 30~70 | NM | Electrical (2 Hz, 2~3 mA), De qi (rotation) | 30 min | 1~3 | (1) 1 day before chemotherapy (2) 1 day and 30 min before chemotherapy (3) 1 day, 30 min before, 1 day after chemotherapy | Ningxia Medical University, Yinchuan, China | NM |
| Wang 2019 [26] | PC6, CV12, ST36 | 5 | 20~30 | 0.25 × 40 mm | Manual, De qi | 30 min | 3 | 30 min before or after chemotherapy | Zhejiang Chinese Medical University, China | NM |
| Li 2020 [27] | PC6, CV12, CV6, ST25, ST36, LR13 | 10 | 10–35 | 0.25 × 40 mm (Ande, Guizhou, China) | Electrical (2/100 Hz), De qi | 30 min | 6 | Twice on the first day of chemotherapy and once consecutively on the following 4 days | Beijing Shijitan Hospital, Beijing Friendship Hospital, Beijing Hospital of Traditional Chinese Medicine, and Guang’ Anmen Hospital | All the acupuncturists who participated in this trial were major in acupuncture for more than 3 years with Chinese medicine practitioner license and had undergone rigorous training in conducting this trial |
| Cheng 2020 [28] | PC6, ST36 | 4 | NM | 0.25 × 40 mm (Andi med, China) | Manual, De qi (twirling, rotating) | 30 min | 5 | 30 min before or after chemotherapy | Beijing Traditional Chinese Medicine Hospital | Physicians with 3 years of experience performed the acupuncture for patients |
| Maeng 2022 [29] | PC6, ST36, LI4, LR3 + (HT8, SP2, LR1, SP1, or GB41, SI5, LI1, ST45) | 8 | NM | 0.25 × 40 mm (Dongbang, Seongnam, Republic of Korea) | Manual, NM | 20 min | 3 | 1 h before chemotherapy | Kyung Hee University Hospital | Korean medical doctors |
| Bintoro 2022 [30] | PC6, ST36 | 4 | NM | NM | Intradermal, NM | 3 days | 1 | Before chemotherapy | Inpatient, Dr. Cipto Mangunkusumo Hospital, Jakarta | NM |
| Michel-Cherqui 2024 [31] | PC6, diaphragm, additional ear points | 5 | NM | 0.2 × 0.9 mm (semi-permanent needles, Seirin, Shizuoka, Japan) | NM | 4 days | 1 | Before chemotherapy | Multi-center (tertiary-care university hospital/cancer center/general hospital) | Experienced physicians with more than seven years of practice |
| Shen 2024 [32] | PC6, ST36, LI4 | 6 | NM | NM | Electrical (2 Hz, <10 mA), De qi | 45 min | 4 | Before chemotherapy | Multi-center (six centers in China) | Trained acupuncturists, each with over 3 years of experience in oncology |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Published by MDPI on behalf of the Lithuanian University of Health Sciences. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kim, S.-A.; Yeo, S.; Lim, S. Effectiveness and Safety of Acupuncture for Nausea and Vomiting in Cancer Patients: A Systematic Review and Meta-Analysis. Medicina 2025, 61, 1287. https://doi.org/10.3390/medicina61071287
Kim S-A, Yeo S, Lim S. Effectiveness and Safety of Acupuncture for Nausea and Vomiting in Cancer Patients: A Systematic Review and Meta-Analysis. Medicina. 2025; 61(7):1287. https://doi.org/10.3390/medicina61071287
Chicago/Turabian StyleKim, Sung-A, Sujung Yeo, and Sabina Lim. 2025. "Effectiveness and Safety of Acupuncture for Nausea and Vomiting in Cancer Patients: A Systematic Review and Meta-Analysis" Medicina 61, no. 7: 1287. https://doi.org/10.3390/medicina61071287
APA StyleKim, S.-A., Yeo, S., & Lim, S. (2025). Effectiveness and Safety of Acupuncture for Nausea and Vomiting in Cancer Patients: A Systematic Review and Meta-Analysis. Medicina, 61(7), 1287. https://doi.org/10.3390/medicina61071287







