Dens Invaginatus: A Comprehensive Review of Classification and Clinical Approaches
Abstract
1. Introduction
2. Evolution of Dens Invaginatus Classifications
3. Overview of Dens Invaginatus Classification
- Hallet’s (1953) [16]
- -
- Type I: A small, enamel-lined invagination confined to the crown that does not extend beyond the cementoenamel junction (CEJ).
- -
- Type II: An invagination that extends beyond the CEJ into the root but remains a blind sac. It may or may not communicate with the pulp.
- -
- Type III: An invagination that penetrates deeply into the root and may form a second foramen, potentially communicating with the periapical tissues. There is usually no direct communication with the pulp, although it is often associated with periapical lesions despite the pulp remaining vital.
- -
- Type IV: A complex or dilated invagination in which the entire tooth structure is distorted. This type may resemble a dilated composite odontoma.
- Oehlers (1957) [17]
- -
- Type I: The invagination is confined to the crown and does not extend beyond the CEJ.
- -
- Type II: The invagination extends beyond the CEJ and may involve the root, but it remains a blind sac. It may or may not communicate with the pulp.
- -
- Type III: The invagination penetrates through the root and communicates with the periodontal ligament, laterally in Type IIIa and apically in Type IIIb, without direct communication with the pulp chamber.
- Ulmansky & Hermel (1964) [18]
- -
- Enamel-lined tracts;
- -
- Communication with the pulp;
- -
- Irregularities in the surrounding dentin;
- -
- The presence of connective tissue or pulp-like remnants within the invagination.
- Schulze & Brand (1972) [19]
- -
- The extent and shape of the invagination;
- -
- Communication with the pulp or periodontal ligament;
- -
- The number and direction of the invaginations;
- -
- The effect on surrounding tooth structures (e.g., dentin, enamel, and pulp).
- Vincent Townend (1974) [20]
- -
- The extent of the invagination: Similar to Oehlers’ classification, ranging from coronal-only involvement to deep extensions into the root.
- -
- Communication with the pulp and periodontium: Whether or not the invagination communicates with the pulp chamber or periapical tissues.
- -
- Morphological complexity: Whether the invagination results in distorted crown or root morphology, as seen in dilated odontomes.
- -
- Radiographic appearance: Assessment based on the visibility and characteristics of the invagination in radiographic imaging.
4. Anatomic Distribution and Pathological Prevalence of Dens Invaginatus Types
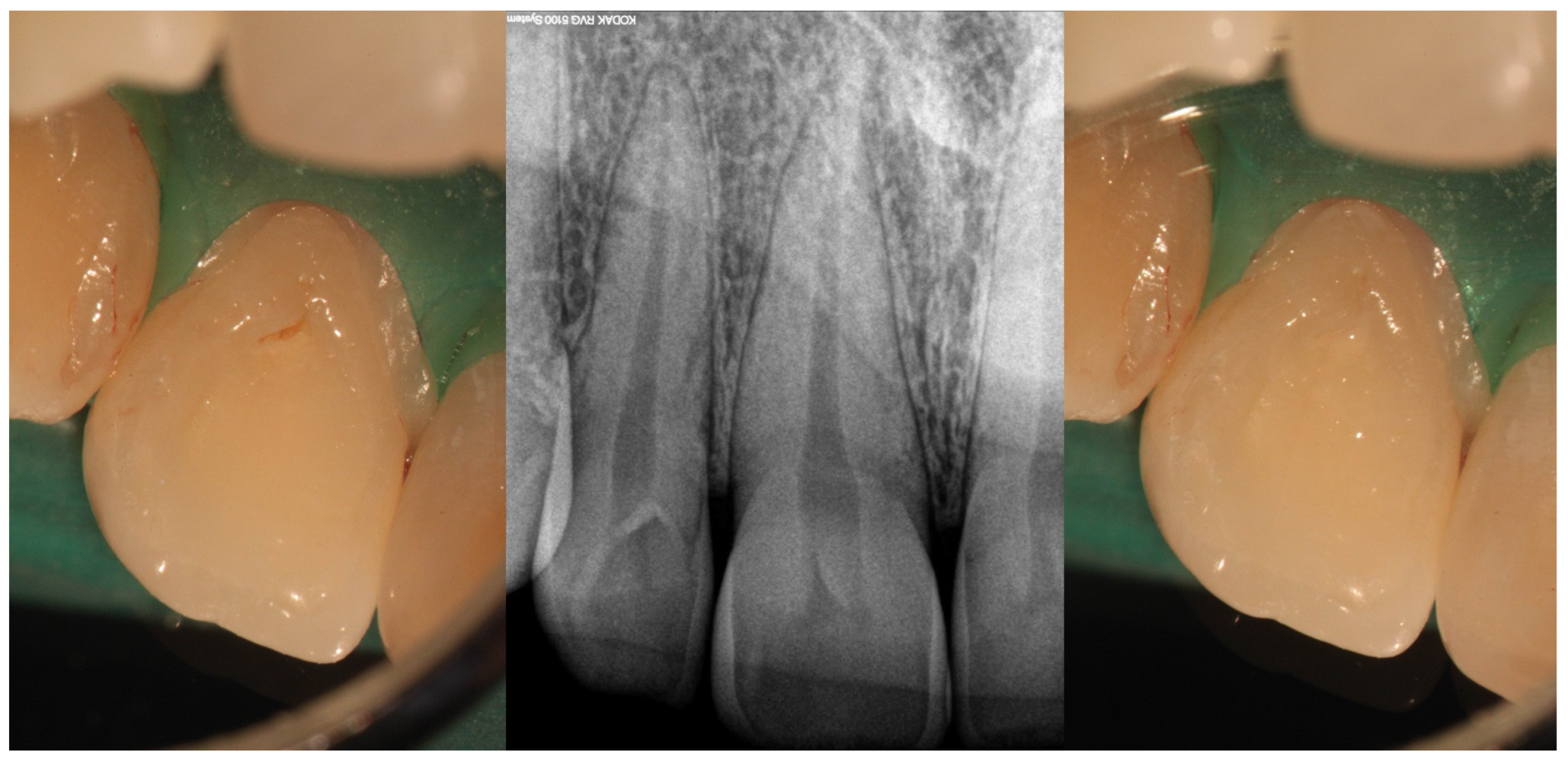
5. Clinical Features, Diagnostic Considerations, and Management
- Type I
- Type II
- Type III
6. Associated Dental Anomalies
7. Advancements and Future Perspectives in the Management of Dens Invaginatus
8. Final Remarks
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Ali, A.; Zoya, A.; Ali, S.; Arslan, H. Rare variant of dens invaginatus with accessory root and labial talon cusp in maxillary lateral incisor—Case report. Aust. Endod. J. 2023, 49, 192–201. [Google Scholar] [CrossRef] [PubMed]
- Siqueira, J.F., Jr.; Rôças, I.N.; Hernández, S.R.; Brisson-Suárez, K.; Baasch, A.C.; Pérez, A.R.; Alves, F.R. Dens invaginatus: Clinical implications and antimicrobial endodontic treatment considerations. J. Endod. 2022, 48, 161–170. [Google Scholar] [CrossRef] [PubMed]
- Hülsmann, M. Dens invaginatus: Aetiology, classification, prevalence, diagnosis and treatment considerations. Int. Endod. J. 1997, 30, 79–90. [Google Scholar] [CrossRef] [PubMed]
- Versiani, M.A.; Martins, J.N.; Basrani, B. 3D visual glossary of terminology in root and root canal anatomy. In The Root Canal Anatomy in Permanent Dentition; Springer: Cham, Switzerland, 2019; pp. 391–425. [Google Scholar]
- Chaturvedula, B.B.; Muthukrishnan, A.; Bhuvaraghan, A.; Sandler, J.; Thiruvenkatachari, B. Dens invaginatus: A review and orthodontic implications. Br. Dent. J. 2021, 230, 345–350. [Google Scholar] [CrossRef] [PubMed]
- Sisodia, S.; Maria, R.; Maria, A. Dens invaginatus—A review & case report. Endodontology 2010, 22, 75–82. [Google Scholar]
- Gallacher, A.; Ali, R.; Bhakta, S. Dens invaginatus: Diagnosis and management strategies. Br. Dent. J. 2016, 221, 383–387. [Google Scholar] [CrossRef] [PubMed]
- Grahnen, H. Dens invaginatus. I. A clinical, roentgenological and genetical study of permanent upper lateral incisors. Odontol. Revy. 1959, 10, 115–137. [Google Scholar]
- Pokala, P.; Acs, G. A constellation of dental anomalies in a chromosomal deletion syndrome (7q32): Case report. Pediatr. Dent. 1994, 16, 306–309. [Google Scholar] [PubMed]
- Soares, J.; Santos, S.; Silveira, F.; Nunes, E. Calcium hydroxide barrier over the apical root-end of a type III dens invaginatus after endodontic and surgical treatment. Int. Endod. J. 2007, 40, 146–155. [Google Scholar] [CrossRef] [PubMed]
- Alani, A.; Bishop, K. Dens invaginatus. Part 1: Classification, prevalence and aetiology. Int. Endod. J. 2008, 41, 1123–1136. [Google Scholar] [CrossRef] [PubMed]
- Gündüz, K.; Çelenk, P.; Canger, E.M.; Zengin, Z.; Sümer, P. A retrospective study of the prevalence and characteristics of dens invaginatus in a sample of the Turkish population. Med. Oral Patol. Oral Cir. Bucal. 2013, 18, e27. [Google Scholar] [CrossRef] [PubMed]
- Patel, S. The use of cone beam computed tomography in the conservative management of dens invaginatus: A case report. Int. Endod. J. 2010, 43, 707–713. [Google Scholar] [CrossRef] [PubMed]
- George, R.; Moule, A.J.; Walsh, L.J. A rare case of dens invaginatus in a mandibular canine. Aust. Endod. J. 2010, 36, 83–86. [Google Scholar] [CrossRef] [PubMed]
- Shrestha, A.; Marla, V.; Shrestha, S.; Maharjan, I.K. Developmental anomalies affecting the morphology of teeth—A review. Rev. Sul-Bras. Odontol. 2015, 12, 68–78. [Google Scholar] [CrossRef]
- Hallett, G.E.M. The incidence, nature, and clinical significance of palatal invaginations in the maxillary incisor teeth. Br. Dent. J. 1953, 95, 491–499. [Google Scholar] [CrossRef] [PubMed]
- Oehlers, F.A. Dens invaginatus (dilated composite odontome): I. Variations of the invagination process and associated anterior crown forms. Oral Surg. Oral Med. Oral Pathol. 1957, 10, 1204–1218. [Google Scholar] [CrossRef] [PubMed]
- Ulmansky, M.; Hermel, J. Double dens in dente in a single tooth: Report of a case and radiologic study of the incidence of small dens in dente. Oral Surg. Oral Med. Oral Pathol. 1964, 17, 92–97. [Google Scholar] [CrossRef] [PubMed]
- Schulze, C.; Brand, E. Über den dens invaginatus (Dens in dente). Zahnärztl. Welt Zahnärztl. Reform 1972, 81, 569–573. [Google Scholar]
- Vincent-Townend, J. Dens invaginatus. J. Dent. 1974, 2, 234–238. [Google Scholar] [CrossRef] [PubMed]
- Ahmed, H.M.; Dummer, P.M. A new system for classifying tooth, root and canal anomalies. Int. Endod. J. 2018, 51, 389–404. [Google Scholar] [CrossRef] [PubMed]
- Gul, M.; Adnan, S.; Umer, F. A variant of the current dens invaginatus classification. Front. Dent. 2020, 17, 28. [Google Scholar] [CrossRef] [PubMed]
- Wang, Y.; Su, S.; Chen, X.; Jia, X. CBCT analysis of the incidence of maxillary lateral incisor dens invaginatus and its impact on periodontal supporting tissues. BMC Oral Health 2024, 24, 1569. [Google Scholar] [CrossRef] [PubMed]
- Gu, Y.C. A micro–computed tomographic analysis of maxillary lateral incisors with radicular grooves. J. Endod. 2011, 37, 789–792. [Google Scholar] [CrossRef] [PubMed]
- Kirzioğlu, Z.; Ceyhan, D. The prevalence of anterior teeth with dens invaginatus in the western Mediterranean region of Turkey. Int. Endod. J. 2009, 42, 727–734. [Google Scholar] [CrossRef] [PubMed]
- Capar, I.D.; Ertas, H.; Arslan, H.; Ertas, E.T. A retrospective comparative study of cone-beam computed tomography versus rendered panoramic images in identifying the presence, types, and characteristics of dens invaginatus in a Turkish population. J. Endod. 2015, 41, 473–478. [Google Scholar] [CrossRef] [PubMed]
- Hamasha, A.A.; Alomari, Q.D. Prevalence of dens invaginatus in Jordanian adults. Int. Endod. J. 2004, 37, 307–310. [Google Scholar] [CrossRef] [PubMed]
- Bishop, K.; Alani, A.J. Dens invaginatus. Part 2: Clinical, radiographic features and management options. Int. Endod. J. 2008, 41, 1137–1154. [Google Scholar] [CrossRef] [PubMed]
- Pires, M.D.; Baruwa, A.O.; Martins, J.N.; Quaresma, S.A.; da Costa, R.P.; Ginjeira, A. Endodontic management of developmental anomalies: Conservation of invaginated tissues in Type II dens invaginatus–case series. Rev. Port. Estomatol. Med. Dent. Cir. Maxilofac. 2019, 60, 18–26. [Google Scholar] [CrossRef]
- Gonçalves, A.; Gonçalves, M.; Oliveira, D.P.; Goncalves, N. Dens invaginatus type III: Report of a case and 10-year radiographic follow-up. Int. Endod. J. 2002, 35, 873–879. [Google Scholar] [CrossRef] [PubMed]
- Zhou, W.; Jiang, R.; Gu, Y.; Tang, Y. Unique anatomy of a rare type II dens invaginatus in a maxillary lateral incisor: A case report. BMC Oral Health 2025, 25, 452. [Google Scholar] [CrossRef] [PubMed]
- Martins, J.N.; da Costa, R.P.; Anderson, C.; Quaresma, S.A.; Corte-Real, L.S.; Monroe, A.D. Endodontic management of dens invaginatus Type IIIb: Case series. Eur. J. Dent. 2016, 10, 561–565. [Google Scholar] [CrossRef] [PubMed]
- Ricucci, D.; Milovidova, I.; Siqueira, J.F., Jr. Unusual location of dens invaginatus causing a difficult-to-diagnose pulpal involvement. J. Endod. 2020, 46, 1522–1529. [Google Scholar] [CrossRef] [PubMed]
- De Sousa, S.M.; Tavano, S.M.; Bramante, C.M. Unusual case of bilateral talon cusp associated with dens invaginatus. Int. Endod. J. 1999, 32, 494–498. [Google Scholar] [CrossRef] [PubMed]
- Segura, J.J.; Jiménez-Rubio, A. Talon cusp affecting permanent maxillary lateral incisors in two family members. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. Endod. 1999, 88, 90–92. [Google Scholar] [CrossRef] [PubMed]
- Prabhu, R.V.; Rao, P.K.; Veena, K.M.; Shetty, P.; Chatra, L.; Shenai, P. Prevalence of Talon cusp in Indian population. J. Clin. Exp. Dent. 2012, 4, e23. [Google Scholar] [CrossRef] [PubMed]
- Kim, J.H.; Choi, N.K.; Kim, S.M. A retrospective study of association between peg-shaped maxillary lateral incisors and dental anomalies. J. Clin. Pediatr. Dent. 2017, 41, 150–153. [Google Scholar] [CrossRef] [PubMed]
- Gowans, L.J.; Cameron-Christie, S.; Slayton, R.L.; Busch, T.; Romero-Bustillos, M.; Eliason, S.; Sweat, M.; Sobreira, N.; Yu, W.; Kantaputra, P.N.; et al. Missense pathogenic variants in KIF4A affect dental morphogenesis resulting in X-linked Taurodontism, Microdontia and Dens-Invaginatus. Front. Genet. 2019, 10, 800. [Google Scholar] [CrossRef] [PubMed]
- Ridell, K.; Mejare, I.; Matsson, L. Dens invaginatus: A retrospective study of prophylactic invagination treatment. Int. J. Paediatr. Dent. 2001, 11, 92–97. [Google Scholar] [CrossRef] [PubMed]
- Mabrouk, R.; Berrezouga, L.; Frih, N. The accuracy of CBCT in the detection of dens invaginatus in a Tunisian population. Int. J. Dent. 2021, 2021, 8826204. [Google Scholar] [CrossRef] [PubMed]
- Murray, P.E. Review of guidance for the selection of regenerative endodontics, apexogenesis, apexification, pulpotomy, and other endodontic treatments for immature permanent teeth. Int. Endod. J. 2023, 56, 188–199. [Google Scholar] [CrossRef] [PubMed]






| Classification System | Key Feature | Usage | Relevance | Limitations |
|---|---|---|---|---|
| Hallet (1953) [16] | Clinical and radiographic appearance | Historical | Foundation for dens invaginatus taxonomy | Complex and has limited applicability |
| Oehlers (1957) [17] | Radiographic depth and communication | Widely adopted for clinical and research | Simple and easy radiographic application Correlates with clinical complexity Most relevant clinical classification | Limited to single description of invagination Lacks 3D anatomical variation |
| Ulmansky & Hermel (1964) [18] | Morphological variations and histology | Rarely used | Highlights spectrum of severity Emphasizes developmental and histological characteristics | Lacks radiographic criteria Less practical for diagnosis and treatment planning |
| Schulze & Brand (1972) [19] | Radiographic and clinical types | Research and academic focus | Covers full spectrum of morphological variations Useful for detailed anatomic documentation | No simple numerical system Complex for daily clinical use |
| Vincent-Townend (1974) [20] | Radiographic | Limited use | Useful in assessing severity and treatment planning Links morphology to clinical management | Not structured and lacks clinical details as it is reliant on radiographic appearance |
| Ahmed & Dummer (2018) [21] | Cone beam computed tomography and pulp morphology | Emerging | 3D visualization. Identifies true pulp involvement Describes multiple invaginations | Coding system requires a learning curve High-resolution scans always required |
| Gul et al. (2021) [22] | Cone beam computed tomography | Emerging | 3D visualization Enhanced Oehlers’ classification with additional Type IV proposed | High-resolution scans always required |
| Pulp/Periapical Involvement | Diagnostic Tool | Clinical Management | Prognosis and Follow Up | |
|---|---|---|---|---|
| Type I | Minimal risk to pulp unless caries or bacterial ingress occurs | Periapical radiograph may be adequate | Preventive sealing of palatal pit or groove with resin-based materials Restoration if necessary Endodontic treatment only if secondary infection occurs | Good prognosis and early intervention help preserve pulp vitality Regular clinical and radiographic monitoring |
| Type II | Moderate to high risk of pulp involvement | CBCT recommended to assess depth and pulp communication | Preventive sealing or minimally invasive restoration If pulp compromised, vital pulp therapy or root canal treatment depending on health state of pulp | Good to fair prognosis if depth is within coronal third and detected early Radiographic follow-up needed to monitor healing |
| Type IIIa/IIIb | High risk of periapical/periodontal infection | CBCT essential to determine anatomy and extent | Selective treatment of infected invagination if pulp unaffected Often requires surgical access and debridement Orthograde or retrograde obturation with biocompatible materials Combined endodontic and periodontal approach in complex cases | Prognosis depends on anatomical complexity and extent of infection Long-term monitoring essential due to risk of reinfection |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Published by MDPI on behalf of the Lithuanian University of Health Sciences. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Baruwa, A.O.; Anderson, C.; Monroe, A.; Cracel Nogueira, F.; Corte-Real, L.; Martins, J.N.R. Dens Invaginatus: A Comprehensive Review of Classification and Clinical Approaches. Medicina 2025, 61, 1281. https://doi.org/10.3390/medicina61071281
Baruwa AO, Anderson C, Monroe A, Cracel Nogueira F, Corte-Real L, Martins JNR. Dens Invaginatus: A Comprehensive Review of Classification and Clinical Approaches. Medicina. 2025; 61(7):1281. https://doi.org/10.3390/medicina61071281
Chicago/Turabian StyleBaruwa, Abayomi O., Craig Anderson, Adam Monroe, Flávia Cracel Nogueira, Luís Corte-Real, and Jorge N. R. Martins. 2025. "Dens Invaginatus: A Comprehensive Review of Classification and Clinical Approaches" Medicina 61, no. 7: 1281. https://doi.org/10.3390/medicina61071281
APA StyleBaruwa, A. O., Anderson, C., Monroe, A., Cracel Nogueira, F., Corte-Real, L., & Martins, J. N. R. (2025). Dens Invaginatus: A Comprehensive Review of Classification and Clinical Approaches. Medicina, 61(7), 1281. https://doi.org/10.3390/medicina61071281









