Sex-Based Risk Evaluation in Acute Coronary Events—A Study Conducted on an Eastern-European Population
Abstract
1. Introduction
2. Materials and Methods
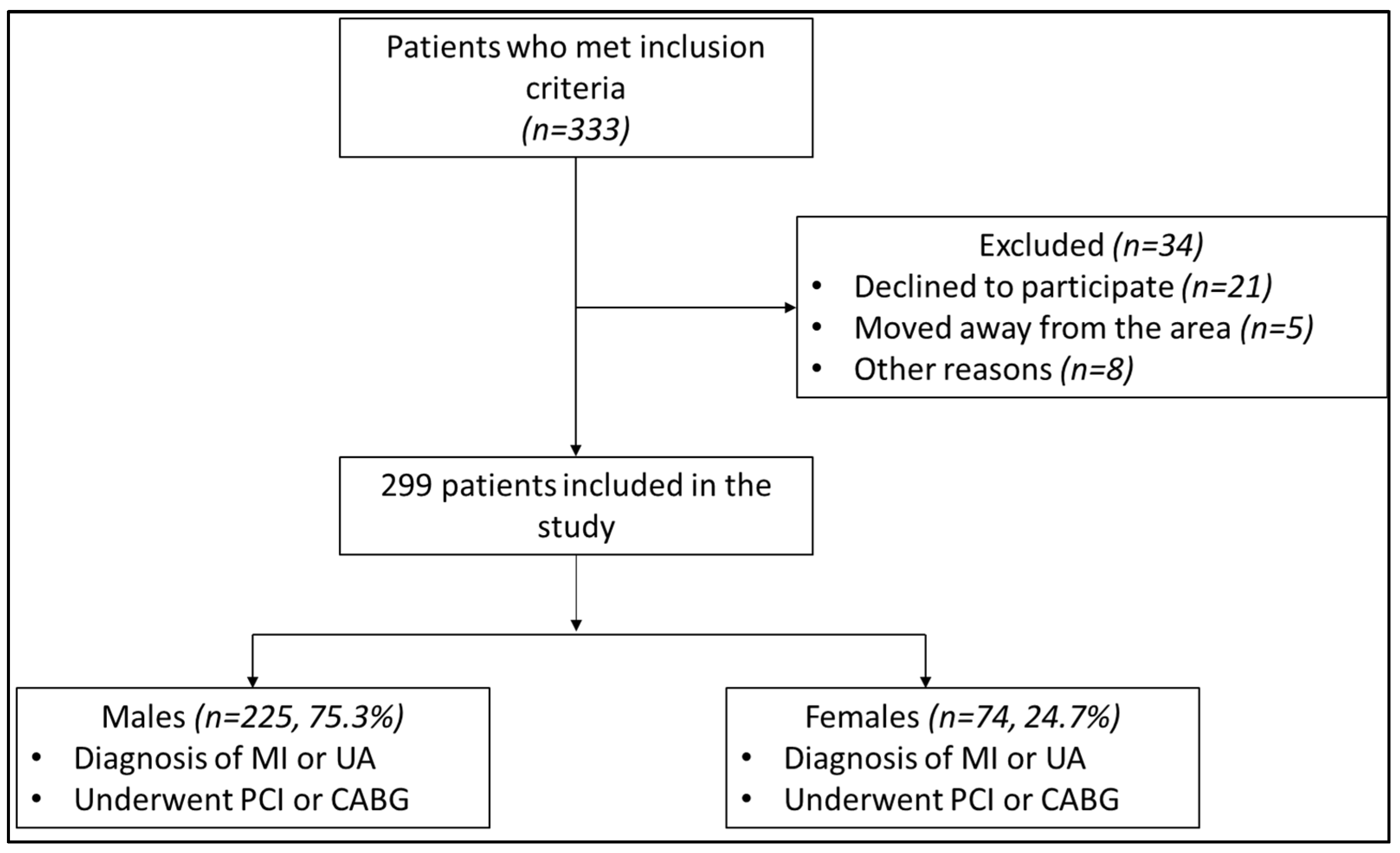
2.1. Patient Recruitment
2.2. Data Collection
2.3. Statistical Analysis
3. Results
3.1. Patient Characteristics
- 1.
- Myocardial Infarction (MI) vs. Unstable Angina (UA) by sex
| Male | Female | |
|---|---|---|
| MI | 116 | 30 |
| UA | 109 | 44 |
- Odds Ratio (OR): (116/109) (30/44) = 116 × 44/109 × 30 ≈ 1.56
- 95% Confidence Interval (CI): 0.92 − 2.650.92 − 2.65
- Interpretation: Males had 1.56 times higher odds of MI compared to UA than females, but this association was not statistically significant (p = 0.100).
- 2.
- CABG vs. PCI by sex
| Male | Female | |
|---|---|---|
| CABG | 53 | 11 |
| PCI | 172 | 63 |
- Odds Ratio (OR): (53/172) (11/63) = 53 × 63/172 × 11 ≈ 1.77
- 95% Confidence Interval (CI): 0.87 − 3.59.
- Interpretation: Males had 1.77 times higher odds of undergoing CABG compared to PCI than females, but this association was not statistically significant (p = 0.114).
3.2. Age-Adjusted Sex Comparisons
3.3. Smoking Habits
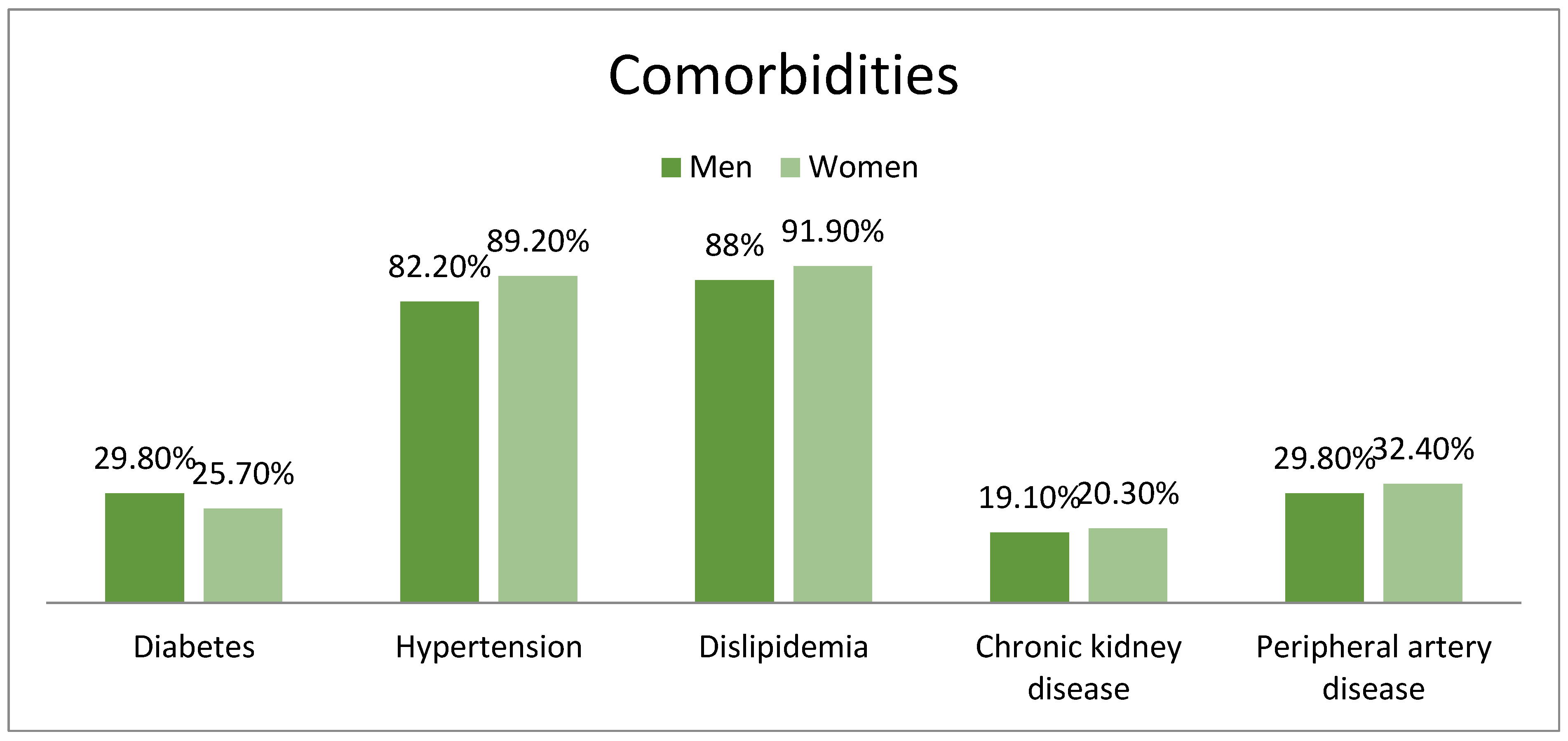
3.4. Comorbidities
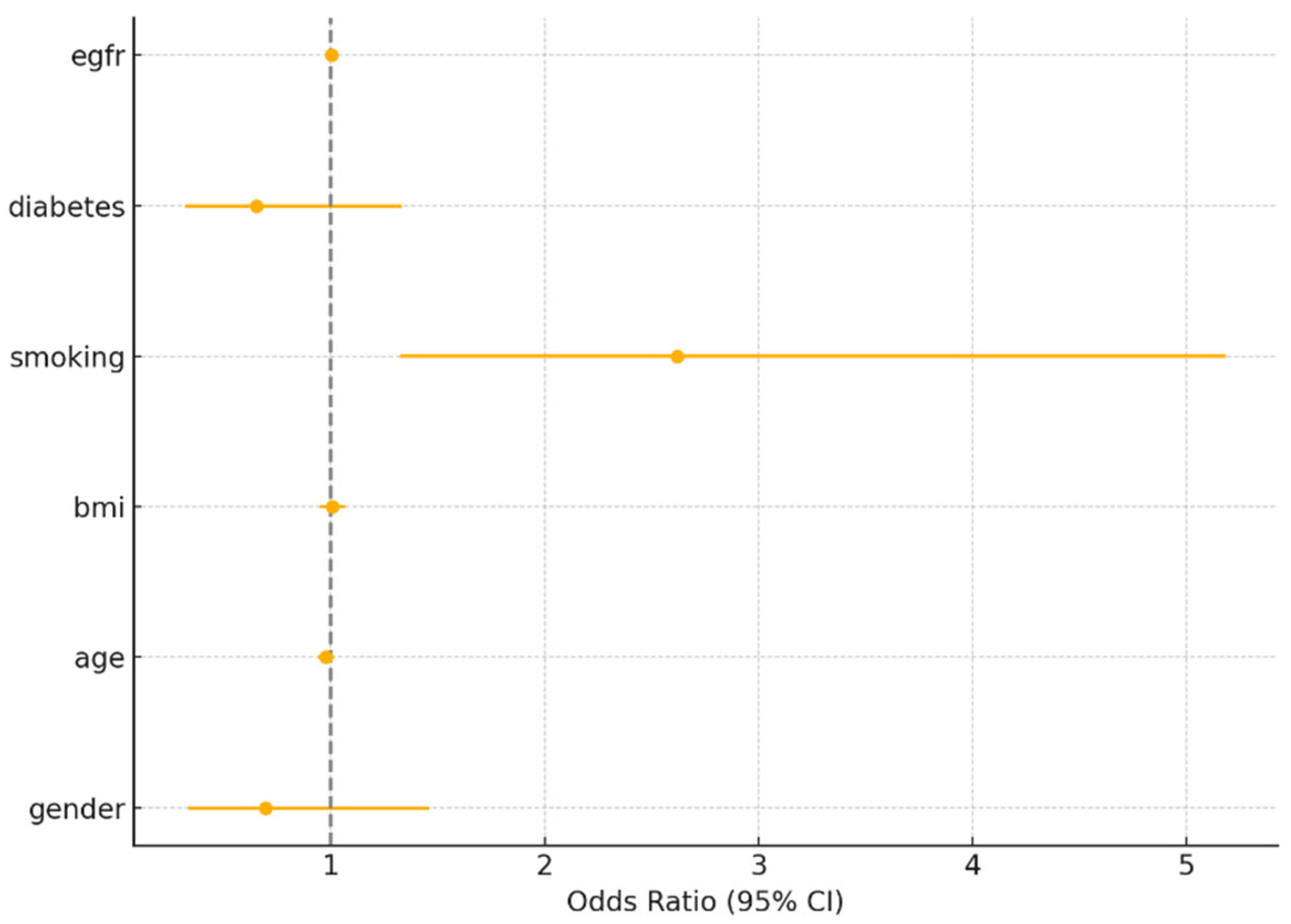
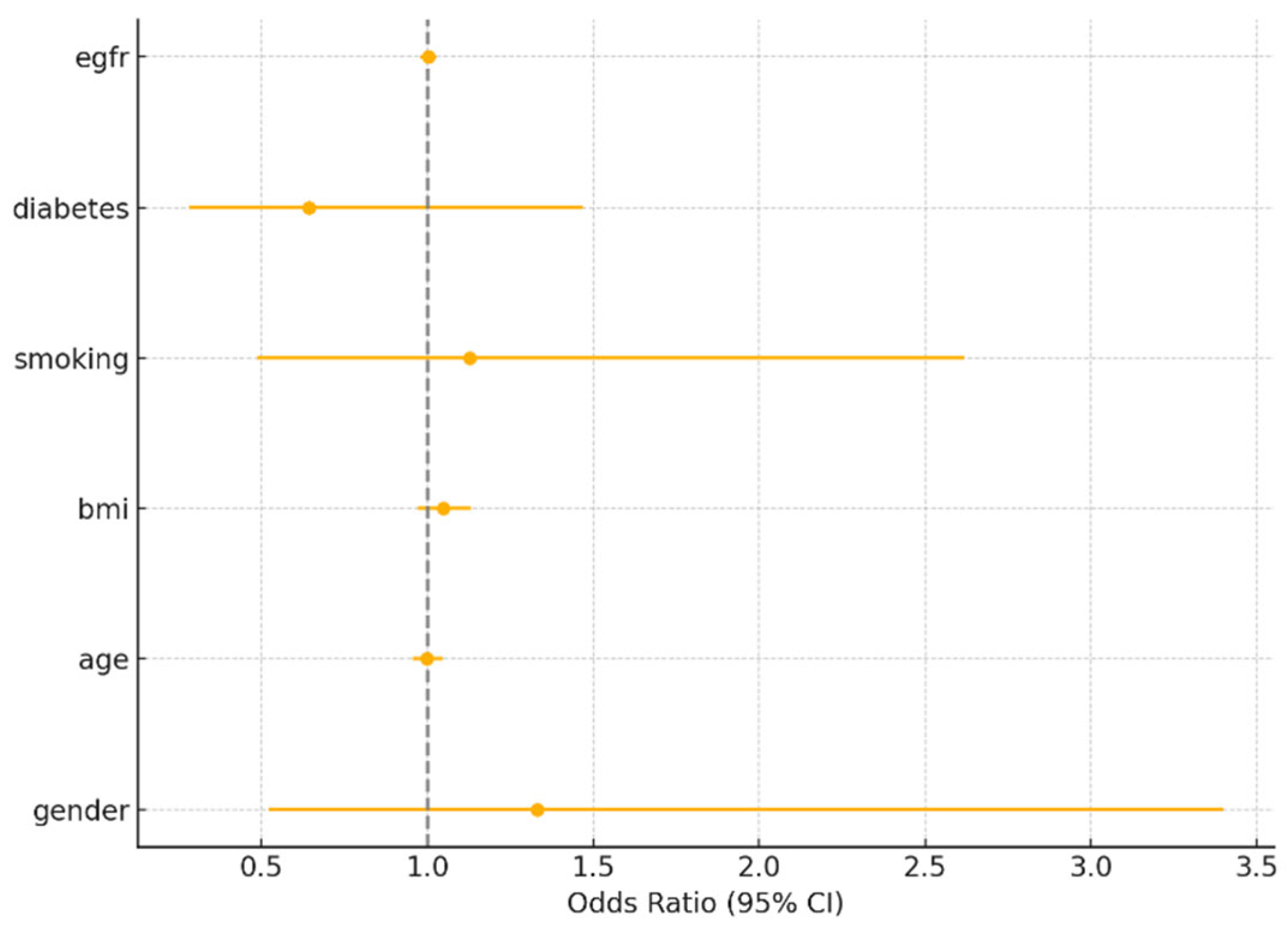
3.5. Multivariate Logostic Regression
3.6. Follow-Up
4. Discussion
Limitations of the Study
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Available online: https://ehnheart.org/library/cvd-statistics/european-cardiovascular-disease-statistics-2017/ (accessed on 30 December 2022).
- Timmis, A.; Townsend, N.; Gale, C.P.; Torbica, A.; Lettino, M.; Petersen, S.E.; Mossialos, E.A.; Maggioni, A.P.; Kazakiewicz, D.; May, H.T.; et al. European Society of Cardiology: Cardiovascular Disease Statistics 2019. Eur. Heart J. 2020, 41, 12–85. [Google Scholar] [CrossRef] [PubMed]
- Cardiovascular Diseases Statistics. Available online: https://ec.europa.eu/eurostat/statistics-explained/index.php?title=Cardiovascular_diseases_statistics#Deaths_from_cardiovascular_diseases (accessed on 14 December 2022).
- Raportul National al Starii de Sanatate 2020. Ministerul Sanatatii, Institutul National de Sanatate Publica, Centrul National de Evaluare si Promovare a Starii de Sanatate. Available online: https://insp.gov.ro/2021/12/29/raportul-national-al-starii-de-sanatate-a-populatiei-2020/ (accessed on 23 June 2024).
- Cushman, M.; Shay, C.M.; Howard, V.J.; American Heart Association. Ten-Year Differences in Women′s Awareness Related to Coronary Heart Disease: Results of the 2019 American Heart Association National Survey: A Special Report from the American Heart Association. Circulation 2021, 143, e239–e248. [Google Scholar] [CrossRef] [PubMed]
- Smolderen, K.G.; Brush, A.; Dreyer, R.P. Psychosocial Factors and Recovery After Acute Myocardial Infarction in Younger Women. Curr. Cardiol. Rep. 2019, 21, 50. [Google Scholar] [CrossRef] [PubMed]
- Mancia, G.; Kreutz, R.; Brunström, M.; Burnier, M.; Grassi, G.; Januszewicz, A.; Muiesan, M.L.; Tsioufis, K.; Agabiti-Rosei, E.; Alghara-bly, E.A.E.; et al. 2023 ESH Guidelines for the management of arterial hypertension The Task Force for the management of arterial hypertension of the European Society of Hypertension: Endorsed by the International Society of Hypertension (ISH) and the European Renal Association (ERA). J. Hypertens. 2023, 41, 1874–2071, Erratum in J. Hypertens. 2024, 42, 194. [Google Scholar]
- Inal, B.B.; Oguz, O.; Emre, T.; Usta, M.; Inal, H.; Altunoglu, E.; Topkaya, C. Evaluation of MDRD, Cockcroft-Gault, and CKD-EPI formulas in the estimated glomerular filtration rate. Clin. Lab. 2014, 60, 1685–1694. [Google Scholar] [CrossRef] [PubMed]
- Gevaert, S.A.; De Bacquer, D.; Evrard, P.; Convens, C.; Dubois, P.; Boland, J.; Renard, M.; Beauloye, C.; Coussement, P.; De Raedt, H.; et al. Gender, TIMI risk score and in-hospital mortality in STEMI patients undergoing primary PCI: Results from the Belgian STEMI registry. EuroIntervention 2014, 9, 1095–1101. [Google Scholar] [CrossRef] [PubMed]
- Dallongevillle, J.; De Bacquer, D.; Heidrich, J.; De Backer, G.; Prugger, C.; Kotseva, K.; Montaye, M.; Amouyel, P.; Group, E.S. Gender differences in the implementation of cardiovascular prevention measures after an acute coronary event. Heart 2010, 96, 1744–1749. [Google Scholar] [CrossRef] [PubMed]
- De Smedt, D.; De Bacquer, D.; De Sutter, J.; Dallongeville, J.; Gevaert, S.; De Backer, G.; Bruthans, J.; Kotseva, K.; Reiner, Z.; Tokgozoglu, L.; et al. The gender gap in risk factor control: Effects of age and education on the control of cardiovascular risk factors in male and female coronary patients. The EUROASPIRE IV study by the European Society of Cardiology. Int. J. Cardiol. 2016, 209, 284–290. [Google Scholar] [CrossRef] [PubMed]
- Vynckier, P.; Kotseva, K.; Gevaert, S.; De Bacquer, D.; De Smedt, D.; Investigators, E.V. Gender differences in cardiovascular risk factor awareness: Results from the ESC EORP EUROASPIRE V Registry. Int. J. Cardiol. 2022, 352, 152–157. [Google Scholar] [CrossRef] [PubMed]
- Huxley, R.R.; Woodward, M. Cigarette smoking as a risk factor for coronary heart disease in women compared with men: A systematic review and meta-analysis of prospective cohort studies. Lancet 2011, 378, 1297–1305. [Google Scholar] [CrossRef] [PubMed]
- Pomp, E.R.; Rosendaal, F.R.; Doggen, C.J. Smoking increases the risk of venous thrombosis and acts synergistically with oral contraceptive use. Am. J. Hematol. 2008, 83, 97–102. [Google Scholar] [CrossRef] [PubMed]
- Young, L.; Cho, L. Unique cardiovascular risk factors in women. Heart 2019, 105, 1656–1660. [Google Scholar] [CrossRef] [PubMed]
- Wilson, P.W.; D’Agostino, R.B.; Sullivan, L.; Parise, H.; Kannel, W.B. Overweight and obesity as determinants of cardio-vascular risk: The Framingham experience. Arch. Intern. Med. 2002, 162, 1867–1872. [Google Scholar] [CrossRef] [PubMed]
- Bikbov, B.; Perico, N.; Remuzzi, G.; on behalf of the GBD Genitourinary Diseases Expert Group. Disparities in Chronic Kidney Disease Prevalence among Males and Females in 195 Countries: Analysis of the Global Burden of Disease 2016 Study. Nephron 2018, 139, 313–318. [Google Scholar] [CrossRef] [PubMed]
- Wei, F.F.; Xue, R.; Wu, Y.; Liang, W.; He, X.; Zhou, Y.; Owusu-Agyeman, M.; Wu, Z.; Zhu, W.; He, J.; et al. Sex-Specific Associations of Risks and Cardiac Structure and Function With Microalbumin/Creatinine Ratio in Diastolic Heart Failure. Front. Cardiovasc. Med. 2020, 7, 579400. [Google Scholar] [CrossRef] [PubMed]
- Sambola, A.; Del Blanco, B.G.; Kunadian, V.; Vogel, B.; Chieffo, A.; Vidal, M.; Ratcovich, H.; Botti, G.; Wilkinson, C.; Mehran, R. Sex-based Differences in Percutaneous Coronary Intervention Outcomes in Patients with Ischaemic Heart Disease. Eur. Cardiol. 2023, 18, e06. [Google Scholar] [CrossRef] [PubMed]
- Vynckier, P.; De Sutter, J.; De Pauw, M.; Vandekerckhove, H.; De Backer, G.; Vervaet, P.; Deweerdt, N.; Dendale, P.; Persu, A.; Janssen, A. Gender differences in risk factor management and pharmacological treatment among CHD patients: Belgian results of the EUROASPIRE IV and EU-ROASPIRE V surveys. Acta Cardiol. 2023, 78, 607–613. [Google Scholar] [CrossRef] [PubMed]
- Zhao, M.; Vaartjes, I.; Graham, I.; Grobbee, D.; Spiering, W.; Klipstein-Grobusch, K.; Woodward, M.; Peters, S.A. Sex differences in risk factor management of coronary heart disease across three regions. Heart 2017, 103, 1587–1594. [Google Scholar] [CrossRef] [PubMed]
- Marzà-Florensa, A.; Vaartjes, I.; Graham, I.; Klipstein-Grobusch, K.; Grobbee, D.E.; Surf CHD II collaborators. A Global Perspective on Cardiovascular Risk Factors by Educational Level in CHD Patients: SURF CHD II. Glob. Heart 2024, 19, 60. [Google Scholar] [CrossRef] [PubMed]
- European Commission: Directorate-General for Justice and Consumers; Franklin, P.; Bambra, C.; Albani, V. Gender Equality and Health in the EU; Publications Office of the European Union: Luxembourg, 2021; Available online: https://data.europa.eu/doi/10.2838/991480 (accessed on 23 April 2024).
- Go Red for Women. About Go Red for Women. Available online: https://www.goredforwomen.org/en/about-go-red-for-women (accessed on 30 December 2022).
| Variable | All Patients (n = 299) | Males (n = 225) | Females (n = 74) | p-Value |
|---|---|---|---|---|
| Demographics and clinical | ||||
| Age, years | 61.21 ± 9.4 | 60.51 ± 9.3 | 63.32 ± 9.3 | 0.026 |
| Height, m | 1.7 ± 0.08 | 1.73 ± 0.1 | 1.61 ± 0.1 | <0.001 |
| Weight, kg | 86.59 ± 16.2 | 88.35 ± 15.7 | 81.24 ± 16.7 | 0.001 |
| BMI, kg/m2 | 29.9 ± 5.3 | 29.48 ± 4.99 | 31.20 ± 6.1 | 0.029 |
| Abdominal circumference, cm | 105.19 ± 13.6 | 105.92 ± 13.5 | 102.98 ± 13.5 | 0.107 |
| Neck circumference, cm | 38.27 ± 4.8 | 39.09 ± 4.7/8 | 35.75 ± 3.8 | <0.001 |
| Systolic blood pressure, mmHg | 136.7 ± 19.8 | 137.87 ± 20.2 | 132.98 ± 18.1 | 0.053 |
| Diastolic blood pressure, mmHg | 81.31 ± 11.2 | 82.13 ± 11.4 | 79.10 ± 10.3 | 0.034 |
| Heart rate, bpm | 70.18 ± 39.8 | 70.83 ± 45.6 | 68.21 ± 8.95 | 0.416 |
| CO, p.p.m. (mean, IQR) | 3.0 (2.0) | 4.5 (5.7) | 4.67 (6.5) | 0.908 * |
| Blood glucose, mmol/L (mean, IQR) | 7.0 (2.2) | 7.75 (2.71) | 7.30 (1.9) | 0.125 * |
| Albumin/creatinine ratio, mg/g (mean, IQR) | 6.3 (7.3) | 24.19 (79.9) | 14.24 (21.5) | 0.042 * |
| Ejection fraction, % (mean, IQR) | 50.0 (5.0) | 47.07 (8.1) | 48.92 (5.6) | 0.121 * |
| Serum creatinine, mg/dL (mean, IQR) | 1.20 (0.3) | 1.29 (0.5) | 1.10 (0.3) | <0.001 * |
| Admission diagnosis and procedures | ||||
| Myocardial infarction, n (%) | 146 (49) | 116 (79.45) | 30 (20.54) | 0.100 |
| Unstable angina, n (%) | 153 (51) | 109 (71.24) | 44 (28.75) | |
| CABG, n (%) | 64 (21) | 53 (82.81) | 11 (18) | 0.114 |
| PCI, n (%) | 235 (79) | 172 (73.19) | 63 (26.80) | |
| Comparison | Age-Adjusted OR | 95% CI | p Value | Interpretation |
|---|---|---|---|---|
| Female vs. male—myocardial infarction | 0.69 | 0.41–1.19 | 0.18 | Women had 31% lower odds of MI than men after adjusting for age, but not significant. |
| Female vs. male—PCI | 1.83 | 0.90–3.74 | 0.097 | Women had 83% higher odds of undergoing PCI compared to men, but not significant. |
| Female vs. male—bypass | 0.56 | 0.27–1.14 | 0.108 | Women had 44% lower odds of undergoing bypass compared to men, after age adjustment, not significant. |
| Males (n = 225) | Females (n = 74) | p Value | |
|---|---|---|---|
| Active smokers, n (%) | 86 (38.2) | 24 (32.4) | 0.538 |
| Former smoker, n (%) | 92 (40.9) | 17 (23.0) | 0.049 ** |
| Non-smokers, n (%) | 47 (20.9) | 33 (44.6) | 0.003 ** |
| Years spent smoking, mean ± SD | 32.71 ± 9.1 | 30.56 ± 10.7 | 0.387 |
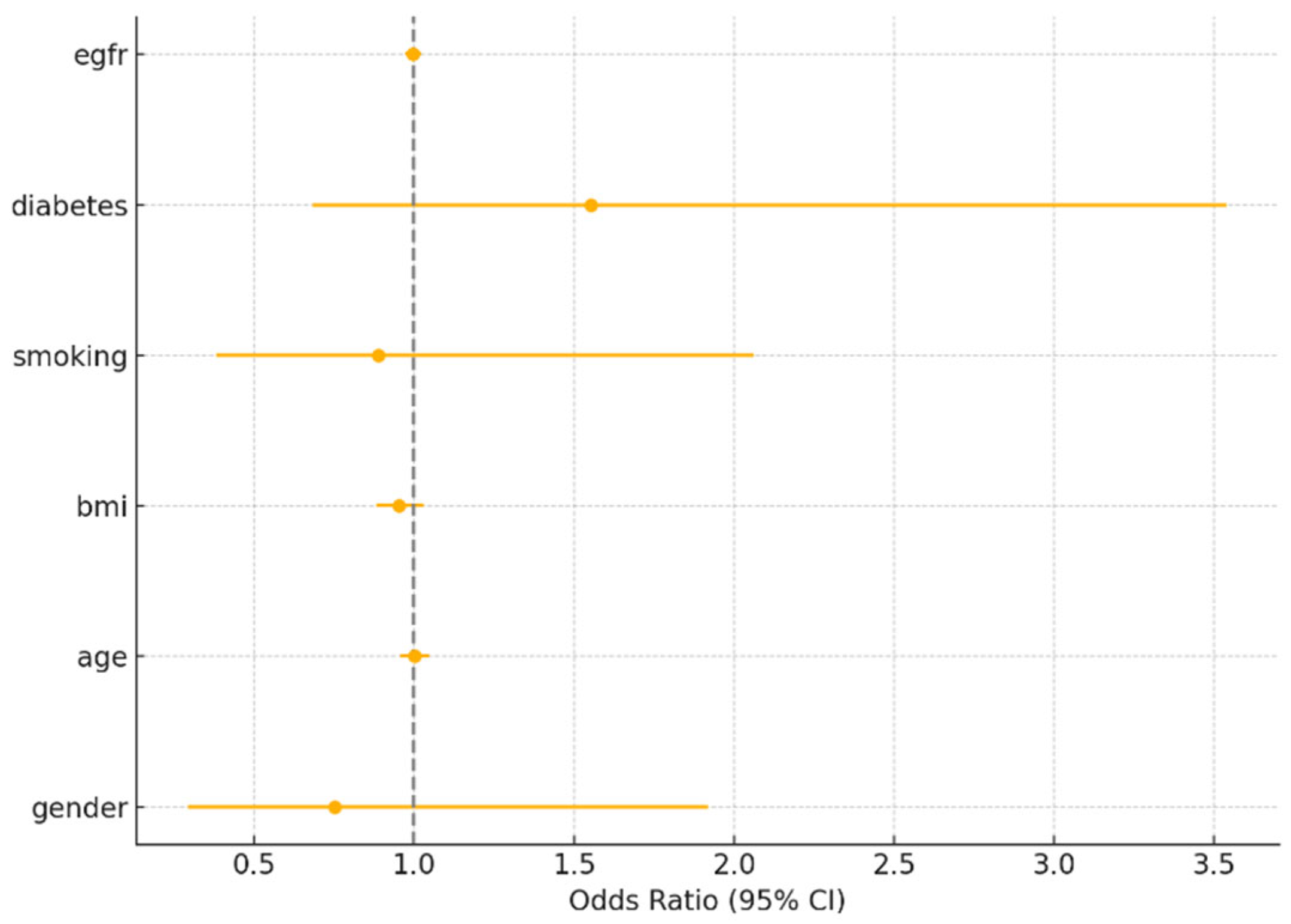
| Unnamed: 0 | Variable | Odds Ratio | 95%CI | p > [z] |
|---|---|---|---|---|
| 1 | Gender | 0.69 | 0.33–1.46 | 0.3363875661672745 |
| 2 | Age | 0.98 | 0.94–1.01 | 0.2193649896124957 |
| 3 | BMI | 1.01 | 0.95–1.07 | 0.8361810081296472 |
| 4 | Smoking | 2.62 | 1.32–5.18 | 0.0056811920613911 |
| 5 | Diabetes | 0.65 | 0.32–1.33 | 0.2410744833789785 |
| 6 | eGFR | 1.0 | 0.98–1.02 | 0.8713422945143566 |
| Unnamed: 0. | Variable | Odds Ratio | 95%CI | p > [z] |
|---|---|---|---|---|
| 1 | Gender | 1.33 | 0.52–3.40 | 0.5497505352473568 |
| 2 | Age | 1.0 | 0.95–1.04 | 0.9498877752218704 |
| 3 | BMI | 1.05 | 0.97–1.13 | 0.2230201164506067 |
| 4 | Smoking | 1.13 | 0.49–2.62 | 0.781233636744233 |
| 5 | Diabetes | 0.64 | 0.28–1.47 | 0.2947966736083327 |
| 6 | eGFR | 1.0 | 0.98–1.03 | 0.852235818270531 |
| Unnamed: 0 | Variable | Odds Ratio | 95%CI | p > [z] |
|---|---|---|---|---|
| 1 | Gender | 0.75 | 0.29–1.92 | 0.5497505352473575 |
| 2 | Age | 1.0 | 0.96–1.05 | 0.9498877752218718 |
| 3 | BMI | 0.95 | 0.88–1.03 | 0.2230201164506084 |
| 4 | Smoking | 0.89 | 0.38–2.06 | 0.7812336367442339 |
| 5 | Diabetes | 1.55 | 0.68–3.54 | 0.2947966736083329 |
| 6 | eGFR | 1.0 | 0.97–1.02 | 0.8522358182705314 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Published by MDPI on behalf of the Lithuanian University of Health Sciences. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Mosteoru, S.; Kundnani, N.R.; Sharma, A.; Pleava, R.; Gaita, L.; Gaiță, D.I. Sex-Based Risk Evaluation in Acute Coronary Events—A Study Conducted on an Eastern-European Population. Medicina 2025, 61, 1227. https://doi.org/10.3390/medicina61071227
Mosteoru S, Kundnani NR, Sharma A, Pleava R, Gaita L, Gaiță DI. Sex-Based Risk Evaluation in Acute Coronary Events—A Study Conducted on an Eastern-European Population. Medicina. 2025; 61(7):1227. https://doi.org/10.3390/medicina61071227
Chicago/Turabian StyleMosteoru, Svetlana, Nilima Rajpal Kundnani, Abhinav Sharma, Roxana Pleava, Laura Gaita, and Dan Ion Gaiță. 2025. "Sex-Based Risk Evaluation in Acute Coronary Events—A Study Conducted on an Eastern-European Population" Medicina 61, no. 7: 1227. https://doi.org/10.3390/medicina61071227
APA StyleMosteoru, S., Kundnani, N. R., Sharma, A., Pleava, R., Gaita, L., & Gaiță, D. I. (2025). Sex-Based Risk Evaluation in Acute Coronary Events—A Study Conducted on an Eastern-European Population. Medicina, 61(7), 1227. https://doi.org/10.3390/medicina61071227







