Systematic Review and Meta-Analysis of AI-Assisted Mammography and the Systemic Immune-Inflammation Index in Breast Cancer: Diagnostic and Prognostic Perspectives
Abstract
1. Introduction
1.1. Background and Rationale
1.2. Aims and Scope of the Current Meta-Analysis and Review
2. Materials and Methods
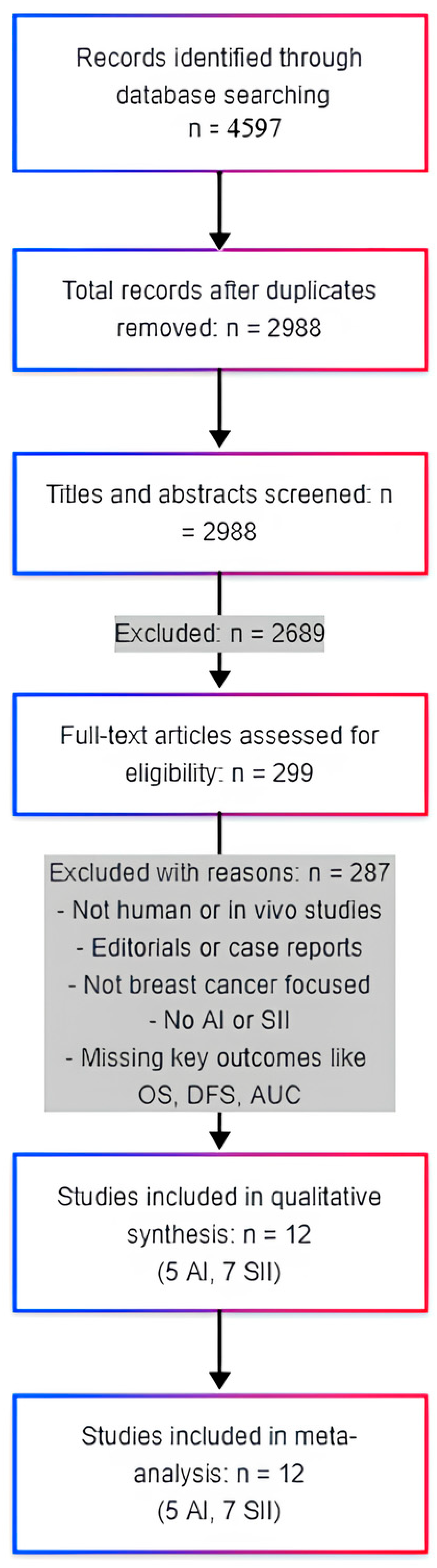
2.1. Study Design, Search Strategy, and Eligibility Criteria
2.2. Study Selection, Data Extraction, Quality Assessment, and Data Synthesis
3. Results
3.1. Overview of Included Studies
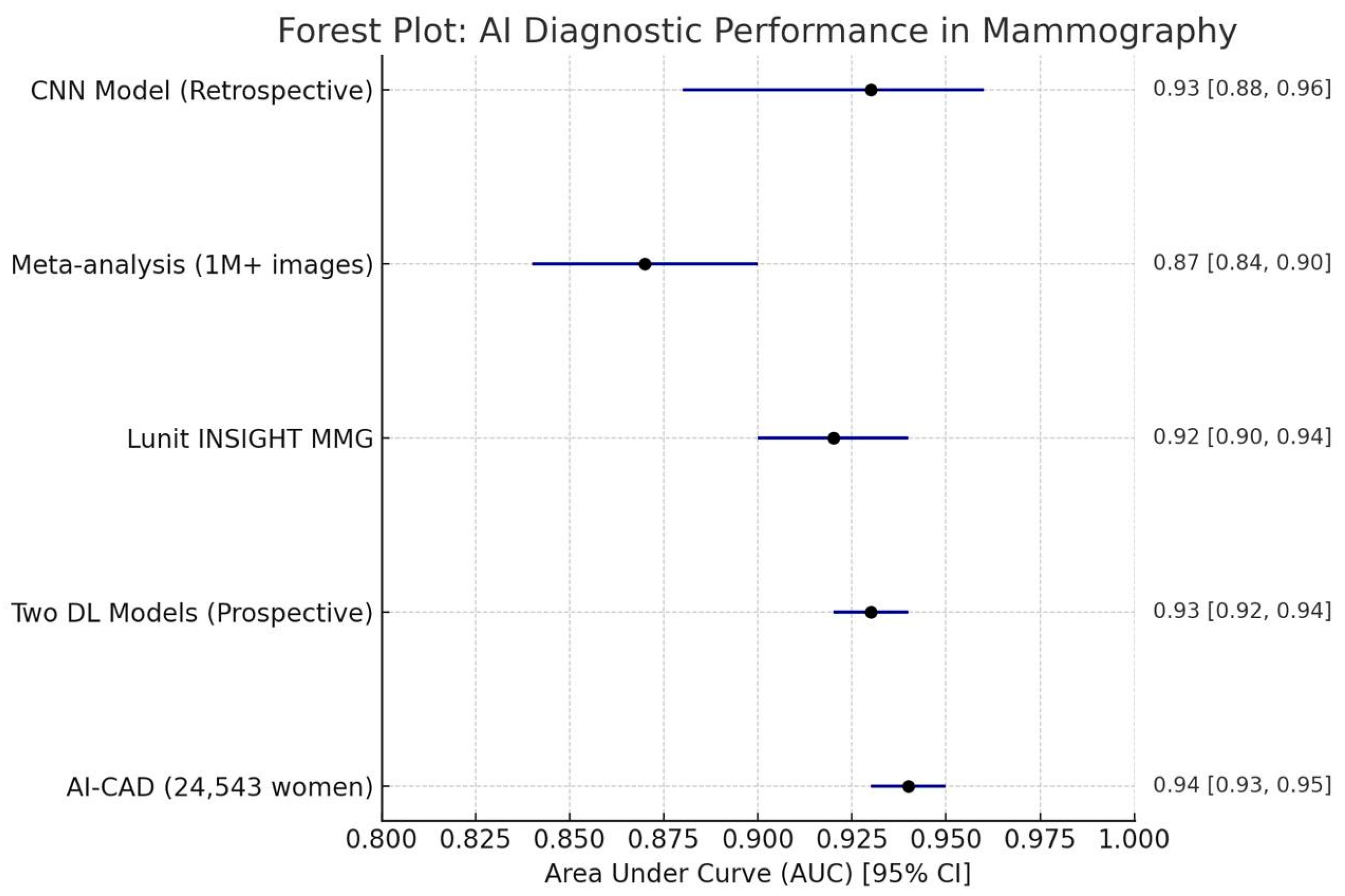
3.2. AI in Mammography: Diagnostic Performance and Clinical Utility
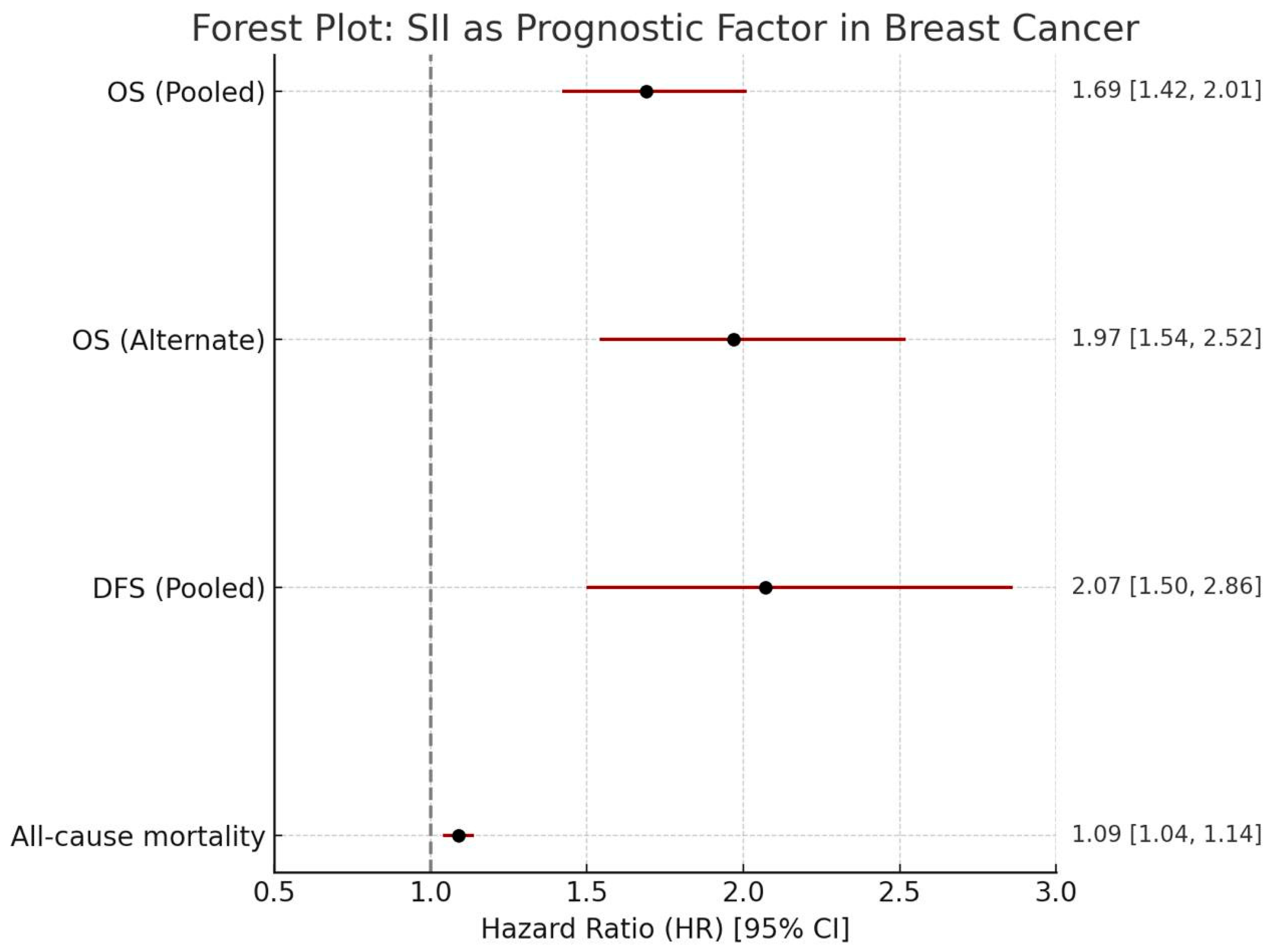
3.3. SII as a Prognostic Factor in Breast Cancer
4. Discussion
4.1. Interpretation of Key Findings: AI in Mammography
4.2. Interpretation of Key Findings: SII as a Prognostic Factor
4.3. Study Limitations
4.4. Future Directions
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
Abbreviations
| AI | AI |
| SII | Systemic Immune-Inflammation Index |
| OS | Overall Survival |
| DFS | Disease-Free Survival |
| PFS | Progression-Free Survival |
| pCR | Pathological Complete Response |
| CNN | Convolutional Neural Network |
| DBT | Digital Breast Tomosynthesis |
| NLR | Neutrophil-to-Lymphocyte Ratio |
| PLR | Platelet-to-Lymphocyte Ratio |
| AUC | Area Under the Curve |
| PPV | Positive Predictive Value |
| NPV | Negative Predictive Value |
| CAD | Computer-Aided Detection |
| RCT | Randomized Controlled Trial |
| QUADAS-2 | Quality Assessment of Diagnostic Accuracy Studies 2 |
| NOS | Newcastle–Ottawa Scale |
| HR | Hazard Ratio |
| OR | Odds Ratio |
| CI | Confidence Interval |
| TTR | Time to Recurrence |
| CSS | Cancer-Specific Survival |
| RFS | Recurrence-Free Survival |
References
- Ciurescu, S.; Cerbu, S.; Dima, C.N.; Borozan, F.; Pârvănescu, R.; Ilaș, D.-G.; Cîtu, C.; Vernic, C.; Sas, I. AI in 2D Mammography: Improving Breast Cancer Screening Accuracy. Medicina 2025, 61, 809. [Google Scholar] [CrossRef] [PubMed]
- Ramli Hamid, M.T.; Ab Mumin, N.; Abdul Hamid, S.; Mohd Ariffin, N.; Mat Nor, K.; Saib, E.; Mohamed, N.A. Comparative Analysis of Diagnostic Performance in Mammography: A Reader Study on the Impact of AI Assistance. PLoS ONE 2025, 20, e0322925. [Google Scholar] [CrossRef] [PubMed]
- Martiniussen, M.A.; Larsen, M.; Hovda, T.; Kristiansen, M.U.; Dahl, F.A.; Eikvil, L.; Brautaset, O.; Bjørnerud, A.; Kristensen, V.; Bergan, M.B.; et al. Performance of Two Deep Learning-Based AI Models for Breast Cancer Detection and Localization on Screening Mammograms from BreastScreen Norway. Radiol. Artif. Intell. 2025, 7, e240039. [Google Scholar] [CrossRef] [PubMed]
- Cheng, H.W.; Wang, T.; Yu, G.C.; Xie, L.Y.; Shi, B. Prognostic Role of the Systemic Immune-Inflammation Index and Pan-Immune Inflammation Value for Outcomes of Breast Cancer: A Systematic Review and Meta-Analysis. Eur. Rev. Med. Pharmacol. Sci. 2024, 28, 180–190. [Google Scholar] [CrossRef]
- Yang, R.; Chang, Q.; Meng, X.; Gao, N.; Wang, W. Prognostic Value of Systemic Immune-Inflammation Index in Cancer: A Meta-Analysis. J. Cancer 2018, 9, 3295. [Google Scholar] [CrossRef]
- Li, Y.; Yu, M.; Yang, M.; Yang, J. The Association of Systemic Immune-Inflammation Index with Incident Breast Cancer and All-Cause Mortality: Evidence from a Large Population-Based Study. Front. Immunol. 2025, 16, 1528690. [Google Scholar] [CrossRef]
- Giovanardi, F.; Casartelli, C.; Di Cicilia, R.; Bologna, A.; Gasparini, E.; Moretti, G.; Degli Esposti, C.; Bisagni, G.; Pinto, C. Systemic Inflammatory Markers in Neoadjuvant Pembrolizumab Therapy for Triple-Negative Breast Cancer: Prognostic Insights and Nomogram Construction. J. Clin. Oncol. 2024, 42, e12649. [Google Scholar] [CrossRef]
- Chen, L.; Kong, X.; Wang, Z.; Wang, X.; Fang, Y.; Wang, J. Pre-Treatment Systemic Immune-Inflammation Index Is a Useful Prognostic Indicator in Patients with Breast Cancer Undergoing Neoadjuvant Chemotherapy. J. Cell. Mol. Med. 2020, 24, 2993–3021. [Google Scholar] [CrossRef]
- Jiang, C.; Lu, Y.; Zhang, S.; Huang, Y. Systemic Immune-Inflammation Index Is Superior to Neutrophil to Lymphocyte Ratio in Prognostic Assessment of Breast Cancer Patients Undergoing Neoadjuvant Chemotherapy. BioMed Res. Int. 2020, 2020, 7961568. [Google Scholar] [CrossRef]
- Guo, W.; Lu, X.; Liu, Q.; Zhang, T.; Li, P.; Qiao, W.; Deng, M. Prognostic Value of Neutrophil-to-lymphocyte Ratio and Platelet-to-lymphocyte Ratio for Breast Cancer Patients: An Updated Meta-analysis of 17079 Individuals. Cancer Med. 2019, 8, 4135. [Google Scholar] [CrossRef]
- Yoon, J.H.; Kim, E.K. Deep Learning-Based Artificial Intelligence for Mammography. Korean J. Radiol. 2021, 22, 1225. [Google Scholar] [CrossRef] [PubMed]
- Vedantham, S.; Shazeeb, M.S.; Chiang, A.; Vijayaraghavan, G.R. Artificial Intelligence in Breast X-Ray Imaging. Semin. Ultrasound CT MRI 2022, 44, 2. [Google Scholar] [CrossRef] [PubMed]
- Wang, L. Mammography with Deep Learning for Breast Cancer Detection. Front. Oncol. 2024, 14, 1281922. [Google Scholar] [CrossRef] [PubMed]
- Chang, Y.-W.; Ryu, J.K.; An, J.K.; Choi, N.; Park, Y.M.; Ko, K.H.; Han, K. Artificial Intelligence for Breast Cancer Screening in Mammography (AI-STREAM): Preliminary Analysis of a Prospective Multicenter Cohort Study. Nat. Commun. 2025, 16, 2248. [Google Scholar] [CrossRef]
- Cadrin-Chênevert, A. Beyond Double Reading: Multiple Deep Learning Models Enhancing Radiologist-Led Breast Screening. Radiol. Artif. Intell. 2025, 7, e250125. [Google Scholar] [CrossRef]
- Altobelli, E.; Angeletti, P.M.; Ciancaglini, M.; Petrocelli, R. The Future of Breast Cancer Organized Screening Program Through Artificial Intelligence: A Scoping Review. Healthcare 2025, 13, 378. [Google Scholar] [CrossRef]
- Gilbert, F.J.; Pinker-Domenig, K. Diagnosis and Staging of Breast Cancer: When and How to Use Mammography, Tomosynthesis, Ultrasound, Contrast-Enhanced Mammography, and Magnetic Resonance Imaging. In Diseases of the Chest, Breast, Heart and Vessels 2019–2022. Diagnostic and Interventional Imaging; Springer: Cham, Switzerland, 2019; pp. 155–166. [Google Scholar] [CrossRef]
- Steyerova, P.; Burgetova, A. Current Imaging Techniques and Impact on Diagnosis and Survival—A Narrative Review. Ann. Breast Surg. 2022, 6. [Google Scholar] [CrossRef]
- Alabousi, M.; Zha, N.; Salameh, J.P.; Samoilov, L.; Sharifabadi, A.D.; Pozdnyakov, A.; Sadeghirad, B.; Freitas, V.; McInnes, M.D.F.; Alabousi, A. Digital Breast Tomosynthesis for Breast Cancer Detection: A Diagnostic Test Accuracy Systematic Review and Meta-Analysis. Eur. Radiol. 2020, 30, 2058–2071. [Google Scholar] [CrossRef]
- Sunarti, S.; Fadzlul Rahman, F.; Naufal, M.; Risky, M.; Febriyanto, K.; Masnina, R. Artificial Intelligence in Healthcare: Opportunities and Risk for Future. Gac. Sanit. 2021, 35, S67–S70. [Google Scholar] [CrossRef]
- Ciurescu, S.; Tomescu, L.; Șerban, D.; Nicolae, N.; Nan, G.; Buciu, V.; Ilaș, D.G.; Cîtu, C.; Vernic, C.; Sas, I. The Prognostic Value of Systemic Inflammation Index in Breast Cancer: A Retrospective Study in Western Romania. J. Clin. Med. 2025, 14, 1081. [Google Scholar] [CrossRef]
- Ni, J.; Qi, X.; Jin, C.; Xu, W.; Li, X.; Song, L.; Zhang, X.; Liu, Y.; Gwark, S.; Shi, H.; et al. Efficacy Prediction of Systemic Immune-Inflammation Index and Prognostic Nutritional Index in Breast Cancer Patients and Their Variations after Neoadjuvant Chemotherapy. Front. Immunol. 2025, 16, 1514736. [Google Scholar] [CrossRef] [PubMed]
- Ethier, J.L.; Desautels, D.; Templeton, A.; Shah, P.S.; Amir, E. Prognostic Role of Neutrophil-to-Lymphocyte Ratio in Breast Cancer: A Systematic Review and Meta-Analysis. Breast Cancer Res. 2017, 19, 1–13. [Google Scholar] [CrossRef] [PubMed]
- Fu, H.; Zheng, J.; Cai, J.; Zeng, K.; Yao, J.; Chen, L.; Li, H.; Zhang, J.; Zhang, Y.; Zhao, H.; et al. Systemic Immune-Inflammation Index (SII) Is Useful to Predict Survival Outcomes in Patients after Liver Transplantation for Hepatocellular Carcinoma within Hangzhou Criteria. Cell. Physiol. Biochem. 2018, 47, 293–301. [Google Scholar] [CrossRef]
- Zhou, Y.; Guo, X.; Shen, L.; Liu, K.; Sun, Q.; Wang, Y.; Wang, H.; Fu, W.; Yao, Y.; Wu, S.; et al. Predictive Significance of Systemic Immune-Inflammation Index in Patients with Breast Cancer: A Retrospective Cohort Study. Onco Targets Ther. 2023, 16, 939–960. [Google Scholar] [CrossRef]
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. The PRISMA 2020 Statement: An Updated Guideline for Reporting Systematic Reviews. BMJ 2021, 372, n71. [Google Scholar] [CrossRef]
- Borah, R.; Brown, A.W.; Capers, P.L.; Kaiser, K.A. Analysis of the Time and Workers Needed to Conduct Systematic Reviews of Medical Interventions Using Data from the PROSPERO Registry. BMJ Open 2017, 7, e012545. [Google Scholar] [CrossRef]
- Horton, J.; Vandermeer, B.; Hartling, L.; Tjosvold, L.; Klassen, T.P.; Buscemi, N. Systematic Review Data Extraction: Cross-Sectional Study Showed That Experience Did Not Increase Accuracy. J. Clin. Epidemiol. 2010, 63, 289–298. [Google Scholar] [CrossRef]
- Gopalakrishnan, S.; Ganeshkumar, P. Systematic Reviews and Meta-Analysis: Understanding the Best Evidence in Primary Healthcare. J. Family Med. Prim. Care 2013, 2, 9. [Google Scholar] [CrossRef]
- Hill, H.; Roadevin, C.; Duffy, S.; Mandrik, O.; Brentnall, A. Cost-Effectiveness of AI for Risk-Stratified Breast Cancer Screening. JAMA Netw. Open 2024, 7, e2431715. [Google Scholar] [CrossRef]
- Fridman, W.H.; Zitvogel, L.; Sautès-Fridman, C.; Kroemer, G. The Immune Contexture in Cancer Prognosis and Treatment. Nat. Rev. Clin. Oncol. 2017, 14, 717–734. [Google Scholar] [CrossRef]
- Mittelstadt, B. Principles Alone Cannot Guarantee Ethical AI. Nat. Mach. Intell. 2019, 1, 501–507. [Google Scholar] [CrossRef]
- Nelson, C.A.; Pérez-Chada, L.M.; Creadore, A.; Li, S.J.; Lo, K.; Manjaly, P.; Pournamdari, A.B.; Tkachenko, E.; Barbieri, J.S.; Ko, J.M.; et al. Patient Perspectives on the Use of Artificial Intelligence for Skin Cancer Screening: A Qualitative Study. JAMA Dermatol. 2020, 156, 501–512. [Google Scholar] [CrossRef]
- Zhang, Z.; Zeng, Y.; Liu, W. The Role of Systemic Immune-Inflammation Index in Predicting Pathological Complete Response of Breast Cancer after Neoadjuvant Therapy and the Establishment of Related Predictive Model. Front. Oncol. 2024, 14, 1437140. [Google Scholar] [CrossRef] [PubMed]
- Templeton, A.J.; McNamara, M.G.; Šeruga, B.; Vera-Badillo, F.E.; Aneja, P.; Ocaña, A.; Leibowitz-Amit, R.; Sonpavde, G.; Knox, J.J.; Tran, B.; et al. Prognostic Role of Neutrophil-to-Lymphocyte Ratio in Solid Tumors: A Systematic Review and Meta-Analysis. J. Natl. Cancer Inst. 2014, 106, dju124. [Google Scholar] [CrossRef] [PubMed]
- Wan, X.; Zhan, J.; Ye, S.; Chen, C.; Li, R.; Shen, M. Construction of a Prognostic Model and Analysis of Related Mechanisms in Breast Cancer Based on Multiple Datasets. Transl. Cancer Res. 2025, 14, 930–948. [Google Scholar] [CrossRef]
| (A) | |||||
| Year | Study Design | Population (N) | AI Model/Algorithm | Comparator | Key Findings |
| 2025 | Retrospective | 578 images | CNN | Radiologist | Accuracy 88.5%, AUC 0.93, high specificity (92.7%), reduced false positives. |
| 2025 | Retrospective | 434 mammograms | Lunit INSIGHT MMG | Radiologists | AI assistance significantly improved diagnostic performance for all readers (p < 0.05), especially for less experienced ones. |
| 2024 | Prospective | Screening mammograms | Two DL-based AI models | Radiologist | AUC 0.93 for both models; identified 81.8–82.5% of screen-detected cancers at threshold 1. |
| 2025 | Prospective | 24,543 women | AI-CAD | Radiologist | CDR was significantly higher with AI-CAD (5.70‰ vs. 5.01‰, p < 0.001) in the single-read setting; no significant difference in RRs. |
| (B) | |||||
| Year | Study Design | Population (N) | AI Model/Algorithm | Comparator | Key Findings |
| 2025 | Meta-analysis | 1,108,328 mammograms, 497,091 women | AI/ML algorithms | Radiologists | AI standalone AUCs were significantly higher than radiologists (0.87 vs. 0.81, p = 0.002) and reduced reading time (17–91%). |
| AI Application | Sensitivity (95% CI) | Specificity (95% CI) | AUC (95% CI) | Recall Rate | Cancer Detection Rate | Reading Time Reduction |
|---|---|---|---|---|---|---|
| Classification | - | 92.7% | 0.93 | - | - | - |
| Detection | 0.75 (0.65–0.83) | 0.90 (0.82–0.95) | 0.89 (0.84–0.98) | - | - | 17–91% |
| Detection | - | - | 0.93 (0.92, 0.94) | - | 81.8–93.7% (Model A/B) | - |
| Detection | - | - | - | No significant difference | 5.70‰ (with AI) vs. 5.01‰ (without AI) | - |
| Inflammatory Marker | Outcome | Pooled HR/OR (95% CI) or AUC | Comparative Statement |
|---|---|---|---|
| SII | OS | AUC: 0.625 | Superior to NLR (AUC 0.555) and PLR (AUC 0.571) |
| NLR | OS | HR: 1.78 (1.49–2.13) | Elevated NLR associated with poor prognosis |
| PLR | OS | HR: 1.32 (1.11–1.57) | Elevated PLR associated with worse prognosis |
| SII | Chemotherapy Response | AUC: 0.751 | May eclipse NLR/PLR as a predictor |
| Year | Study Design | Patient Population (N) | Breast Cancer Subtype Distribution | SII Cut-off Value Used | Key Prognostic Outcomes Assessed |
|---|---|---|---|---|---|
| 2024 | Meta-analysis | BC patients (pooled) | - | Varied | OS, DFS |
| 2025 | Cohort Study | 21,058 females (557 BC) | - | SII/100: 5.09 (incidence), 5.22 (mortality) | Incidence, all-cause mortality |
| 2024 | Cohort Study | 112 BC patients | - | 598.5 | pCR |
| 2024 | Cohort Study | 1808 BC patients | HR-positive, HER2-negative, TNBC | 586.40 (chemo response), 900 (relapse) | Chemotherapy response, Recurrence |
| 2020 | Cohort Study | 249 BC patients | - | 547 | OS, pCR (comparison to NLR/PLR) |
| 2024 | Cohort Study | 112 BC patients | - | 598.5 | pCR |
| 2018 | Meta-analysis | 7657 cancer patients | Various cancers (incl. BC) | 300–1600 (varied) | OS, TTR, PFS, CSS, DFS, RFS |
| Outcome | Number of Studies | Number of Patients | Pooled HR/OR (95% CI) | Heterogeneity (I2, p-Value) |
|---|---|---|---|---|
| OS | - | HR: 1.97 (1.54, 2.52) | I2 = 76% | |
| OS | 7196 | HR: 1.69 (1.42, 2.01) | - | |
| DFS | - | HR: 2.07 (1.50, 2.86) | I2 = 79% | |
| pCR | 112 | OR: (SII independent predictor) | - | |
| All-cause mortality | 557 (BC subset) | HR: 1.09 (1.04, 1.14) (above SII/100 = 5.22) | - |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Published by MDPI on behalf of the Lithuanian University of Health Sciences. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ciurescu, S.; Ciupici-Cladovan, M.; Buciu, V.B.; Ilaș, D.G.; Cîtu, C.; Sas, I. Systematic Review and Meta-Analysis of AI-Assisted Mammography and the Systemic Immune-Inflammation Index in Breast Cancer: Diagnostic and Prognostic Perspectives. Medicina 2025, 61, 1170. https://doi.org/10.3390/medicina61071170
Ciurescu S, Ciupici-Cladovan M, Buciu VB, Ilaș DG, Cîtu C, Sas I. Systematic Review and Meta-Analysis of AI-Assisted Mammography and the Systemic Immune-Inflammation Index in Breast Cancer: Diagnostic and Prognostic Perspectives. Medicina. 2025; 61(7):1170. https://doi.org/10.3390/medicina61071170
Chicago/Turabian StyleCiurescu, Sebastian, Maria Ciupici-Cladovan, Victor Bogdan Buciu, Diana Gabriela Ilaș, Cosmin Cîtu, and Ioan Sas. 2025. "Systematic Review and Meta-Analysis of AI-Assisted Mammography and the Systemic Immune-Inflammation Index in Breast Cancer: Diagnostic and Prognostic Perspectives" Medicina 61, no. 7: 1170. https://doi.org/10.3390/medicina61071170
APA StyleCiurescu, S., Ciupici-Cladovan, M., Buciu, V. B., Ilaș, D. G., Cîtu, C., & Sas, I. (2025). Systematic Review and Meta-Analysis of AI-Assisted Mammography and the Systemic Immune-Inflammation Index in Breast Cancer: Diagnostic and Prognostic Perspectives. Medicina, 61(7), 1170. https://doi.org/10.3390/medicina61071170






