Short-Term Clinical Evaluation of Tibial Tunnel Angle and Position in Anatomical Anterior Cruciate Ligament Reconstruction
Abstract
1. Introduction
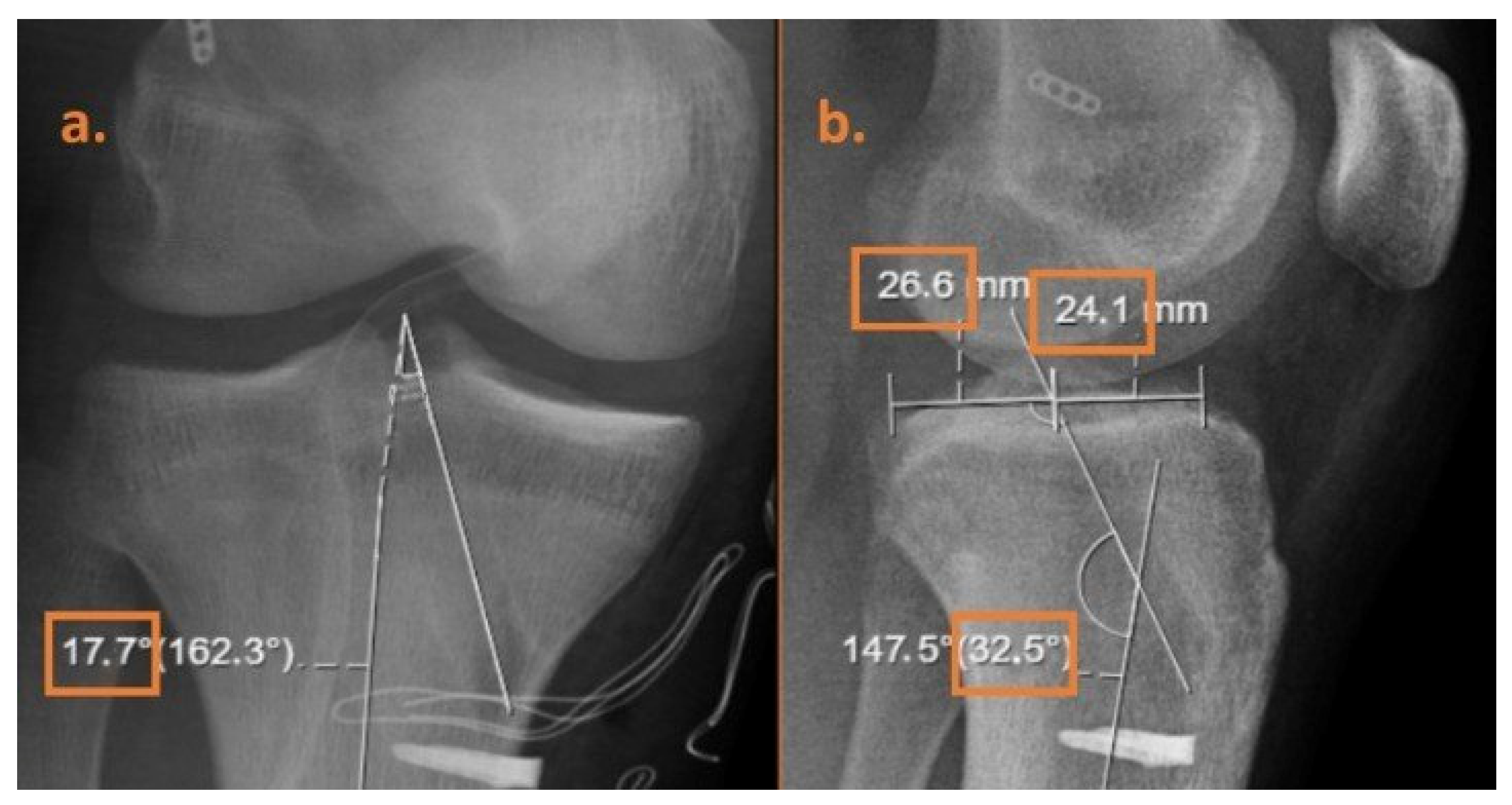
2. Materials and Methods
Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| ACL | Anterior Cruciate Ligament |
| ACLR | Anterior Cruciate Ligament Reconstruction |
| AM | Anteromedial |
| AP | Anteroposterior |
| IKDC | International Knee Documentation Committee |
| Lysholm | Lysholm Knee Score |
| VAS | Visual Analogue Scale |
| TOTBID | Türk Ortopedi ve Travmatoloji Birliği Derneği |
| SD | Standard Deviation |
References
- Nagai, K.; Araki, D.; Matsushita, T.; Nishizawa, Y.; Hoshino, Y.; Matsumoto, T.; Takayama, K.; Nakano, N.; Nagamune, K.; Kurosaka, M.; et al. Biomechanical function of anterior cruciate ligament remnants: Quantitative measurement with a 3-dimensional electromagnetic measurement system. Arthrosc. J. Arthrosc. Relat. Surg. 2016, 32, 1359–1366. [Google Scholar] [CrossRef] [PubMed]
- Mok, Y.R.; Wong, K.L.; Panjwani, T.; Chan, C.X.; Toh, S.J.; Krishna, L. Anterior cruciate ligament reconstruction performed within 12 months of the index injury is associated with a lower rate of medial meniscus tears. Knee Surg. Sports Traumatol. Arthrosc. 2019, 27, 117–123. [Google Scholar] [CrossRef] [PubMed]
- Abram, S.G.F.; Judge, A.; Beard, D.J.; Price, A.J. Rates of Adverse Outcomes and Revision Surgery After Anterior Cruciate Ligament Reconstruction: A Study of 104,255 Procedures Using the National Hospital Episode Statistics Database for England, UK. Am. J. Sports Med. 2019, 47, 2533–2542. [Google Scholar] [CrossRef]
- Piussi, R.; Magnusson, C.; Andersson, S.; Mannerkorpi, K.; Thomeé, R.; Samuelsson, K.; Senorski, E.H. Some, but not all, patients experience full symptom resolution and a positive rehabilitation process after ACL reconstruction: An interview study. Knee Surg. Sports Traumatol. Arthrosc. 2023, 31, 2927–2935. [Google Scholar] [CrossRef]
- Gopinatth, V.; Smith, M.V.; Matava, M.J.; Brophy, R.H.; Knapik, D.M. Most Anterior Cruciate Ligament Injuries in Professional Athletes Occur Without Contact to the Injured Knee: A Systematic Review of Video Analysis Studies. Arthrosc. J. Arthrosc. Relat. Surg. 2024, 41, 1155–1162.e1. [Google Scholar] [CrossRef]
- Topliss, C.; Webb, J. An audit of tunnel position in anterior cruciate ligament reconstruction. Knee 2001, 8, 59–63. [Google Scholar] [CrossRef]
- Sharma, M.; Jain, H.; Raichandani, K.; Agarwal, S. Evaluation of Location of Femoral and Tibial Tunnels after Arthroscopic Anterior Cruciate Ligament Reconstruction: A Longitudinal Study. J. Clin. Diagn. Res. 2021, 15, RC5–RC9. [Google Scholar] [CrossRef]
- Howell, S.M.; Gittins, M.E.; Gottlieb, J.E.; Traina, S.M.; Zoellner, T.M. The Relationship between the Angle of the Tibial Tunnel in the Coronal Plane and Loss of Flexion and Anterior Laxity after Anterior Cruciate Ligament Reconstruction. Am. J. Sports Med. 2001, 29, 567–574. [Google Scholar] [CrossRef] [PubMed]
- Choi, N.-H.; Lee, S.-J.; Park, S.-C.; Victoroff, B.N. Comparison of postoperative tunnel widening after hamstring anterior cruciate ligament reconstructions between anatomic and nonanatomic femoral tunnels. Arthrosc. J. Arthrosc. Relat. Surg. 2020, 36, 1105–1111. [Google Scholar] [CrossRef]
- Yao, J.; Wen, C.Y.; Zhang, M.; Cheung, J.T.-M.; Yan, C.; Chiu, K.-Y.; Lu, W.W.; Fan, Y. Effect of tibial drill-guide angle on the mechanical environment at bone tunnel aperture after anatomic single-bundle anterior cruciate ligament reconstruction. Int. Orthop. 2014, 38, 973–981. [Google Scholar] [CrossRef]
- Sim, J.-A.; Kim, J.-M.; Lee, S.; Song, E.-K.; Seon, J.-K. No difference in graft healing or clinical outcome between trans-portal and outside-in techniques after anterior cruciate ligament reconstruction. Knee Surg. Sports Traumatol. Arthrosc. 2018, 26, 2338–2344. [Google Scholar] [CrossRef] [PubMed]
- Sundemo, D.; Mårtensson, J.; Hamrin Senorski, E.; Svantesson, E.; Kartus, J.; Sernert, N.; Karlsson, J.; Samuelsson, K. No correlation between femoral tunnel orientation and clinical outcome at long-term follow-up after non-anatomic anterior cruciate ligament reconstruction. Knee Surg. Sports Traumatol. Arthrosc. 2019, 27, 3400–3410. [Google Scholar] [CrossRef] [PubMed]
- Behrend, H.; Stutz, G.; Kessler, M.A.; Rukavina, A.; Giesinger, K.; Kuster, M.S. Tunnel placement in anterior cruciate ligament (ACL) reconstruction: Quality control in a teaching hospital. Knee Surg. Sports Traumatol. Arthrosc. 2006, 14, 1159–1165. [Google Scholar] [CrossRef]
- Inderhaug, E.; Strand, T.; Fischer-Bredenbeck, C.; Solheim, E. Effect of a too posterior placement of the tibial tunnel on the outcome 10–12 years after anterior cruciate ligament reconstruction using the 70-degree tibial guide. Knee Surg. Sports Traumatol. Arthrosc. 2014, 22, 1182–1189. [Google Scholar] [CrossRef]
- Santhamoorthy, T.; Xavier, A.A.; Krun, K.; Dubey, D.K. The Influence of Tunnel Parameters and Graft Inclination Angle on Clinical and Radiological Outcome at Long-term Follow-up after Arthroscopic Anterior Cruciate Ligament Reconstruction. Rev. Bras. Ortop. 2024, 59, 189–198. [Google Scholar]
- Ristić, V.; Ristić, N.; Harhaji, V.; Bjelobrk, M.; Milankov, V. Radiographic analysis of the tibial tunnel position after anterior cruciate ligament reconstruction. Med. Pregl. 2018, 71, 15–20. [Google Scholar] [CrossRef]
- Júnior, O.d.M.S.; do Nascimento Ohashi, B.; de Almeida, M.O.; Gonçalves, M.R. Functional result relating to the positioning of the graft in anterior cruciate ligament reconstruction. Rev. Bras. Ortop. Engl. Ed. 2015, 50, 57–67. [Google Scholar]
- Simmons, R.; Howell, S.M.; Hull, M.L. Effect of the angle of the femoral and tibial tunnels in the coronal plane and incremental excision of the posterior cruciate ligament on tension of an anterior cruciate ligament graft: An in vitro study. J. Bone Jt. Surg. 2003, 85, 1018–1029. [Google Scholar] [CrossRef]
- Romano, V.M.; Graf, B.K.; Keene, J.S.; Lange, R.H. Anterior cruciate ligament reconstruction: The effect of tibial tunnel placement on range of motion. Am. J. Sports Med. 1993, 21, 415–418. [Google Scholar] [CrossRef]
- Miller, M.D.; Laidlaw, M.S.; Buyukdogan, K. Anterior versus Posterior Tibial Tunnel Placement in ACL Reconstruction. Orthop. J. Sports Med. 2018, 6, 2325967118S00001. [Google Scholar] [CrossRef]
- Büyükdoğan, K.; Laidlaw, M.S.; Fox, M.A.; Kew, M.E.; Miller, M.D. Effect of Tibial Tunnel Placement Using the Lateral Meniscus as a Landmark on Clinical Outcomes of Anatomic Single-Bundle Anterior Cruciate Ligament Reconstruction. Am. J. Sports Med. 2021, 49, 1451–1459. [Google Scholar] [CrossRef] [PubMed]
- Hatayama, K.; Terauchi, M.; Saito, K.; Higuchi, H.; Yanagisawa, S.; Takagishi, K. The importance of tibial tunnel placement in anatomic double-bundle anterior cruciate ligament reconstruction. Arthrosc. J. Arthrosc. Relat. Surg. 2013, 29, 1072–1078. [Google Scholar] [CrossRef]
- Bedi, A.; Maak, T.; Musahl, V.; Citak, M.; O’Loughlin, P.F.; Choi, D.; Pearle, A.D. Effect of Tibial Tunnel Position on Stability of the Knee After Anterior Cruciate Ligament Reconstruction: Is the Tibial Tunnel Position Most Important? Am. J. Sports Med. 2011, 39, 366–373. [Google Scholar] [CrossRef] [PubMed]
- Azer, A.; Ge, D.; Chan, F.J. Eccentric Reaming to Correct Nonanatomic Anterior Cruciate Ligament Tibial Tunnel Placement. Arthrosc. Tech. 2024, 14, 103261. [Google Scholar] [CrossRef]
- Allen, C.R.; Giffin, J.R.; Harner, C.D. Revision anterior cruciate ligament reconstruction. Orthop. Clin. 2003, 34, 79–98. [Google Scholar] [CrossRef] [PubMed]
- Yücel, M.O.; Dalaslan, R.E.; Sağlam, S.; Karaduman, Z.O.; Arıcan, M.; Akar, B.; Tural, V. Comparison of a new radiographic technique with MRI measurements for tibial tunnel evaluation in ACL reconstruction. Diagnostics 2025, 15, 1237. [Google Scholar] [CrossRef]
- Harput, G.; Bozkurt, İ.; Öçgüder, D.A. Ön çapraz bağ rekonstrüksiyonu sonrası takip ve rehabilitasyon. Türk Ortop. Ve Travmatoloji Birliği Derneği TOTBİD Derg. 2020, 19, 640–646. [Google Scholar] [CrossRef]
- Ra, H.J.; Kim, H.S.; Choi, J.Y.; Ha, J.K.; Kim, J.Y.; Kim, J.G. Comparison of the ceiling effect in the Lysholm score and the IKDC subjective score for assessing functional outcome after ACL reconstruction. Knee 2014, 21, 906–910. [Google Scholar] [CrossRef]
- Do Nascimento, B.F.D.; Lima, M.B.D.R.; Dias, J.M.; Antunes Filho, J.; Campos, T.V.D.O.; Mendes, A.F. Calculation of the minimal important clinical difference of the Lysholm and IKDC scores after anterior cruciate ligament reconstruction. Rev. Bras. Ortop. 2023, 58, 79–84. [Google Scholar]
- Bodkin, S.G.; Hertel, J.; Bruce, A.S.; Diduch, D.R.; Saliba, S.A.; Novicoff, W.M.; Hart, J. Patient function in serial assessments throughout the post-ACL reconstruction progression. Phys. Ther. Sport 2021, 47, 85–90. [Google Scholar] [CrossRef]
- Mann, O.; Al-Dadah, O. Anterior cruciate ligament reconstruction: Effect of graft tunnel position on early to mid-term clinical outcomes. World J. Orthop. 2024, 15, 744. [Google Scholar] [CrossRef] [PubMed]
| Measured Tibial Tunnel Angle (°) | In Coronal Plane (n, %) | In Sagittal Plane (n, %) |
|---|---|---|
| 10–20 | - | 9 (22.5%) |
| 20–30 | 1 (2.5%) | 12 (30.0%) |
| 30–40 | 22 (55.0%) | 11 (27.5%) |
| 40–50 | 14 (35.0%) | 6 (15.0%) |
| 50–60 | 2 (5.0%) | 2 (5.0%) |
| 70–80 | 1 (2.5%) | - |
| Tibial Tunnel Position | In Sagittal Plane (n, %) | |
| 0.4–0.6 | 17 (42.5%) | |
| 0.6–0.8 | 12 (30.0%) | |
| 0.8–1.0 | 7 (17.5%) | |
| 1.0–1.2 | 3 (7.5%) | |
| 1.2–1.4 | 1 (2.5%) | |
| Measured Tibial Tunnel Angle | In Coronal Plane 30–40° (n = 22) | In Coronal Plane 40–50° (n = 14) | |
|---|---|---|---|
| Mean ± SD | Mean ± SD | p Value | |
| IKDC (Preop) | 43.14 ± 11.91 | 42.50 ± 13.29 | 0.882 a |
| IKDC (Month 1) | 43.32 ± 11.70 | 45.64 ± 12.60 | 0.576 a |
| IKDC (Month 2) | 48.09 ± 13.74 | 52.50 ± 12.01 | 0.332 a |
| IKDC (Month 4) | 48.82 ± 14.13 | 55.64 ± 13.34 | 0.158 a |
| LYSHOLM (Preop) | 64.14 ± 15.67 | 54.29 ± 21.02 | 0.117 a |
| LYSHOLM (Month 1) | 60.36 ± 16.31 | 70.86 ± 18.28 | 0.081 a |
| LYSHOLM (Month 2) | 66.95 ± 17.81 | 81.43 ± 15.32 | 0.017 a |
| LYSHOLM (Month 4) | 69.09 ± 16.66 | 81.07 ± 14.77 | 0.035 a |
| Knee Flexion (Preop) | 108.09 ± 28.27 | 112.36 ± 23.48 | 0.785 b |
| Knee Flexion (Month 1) | 87.95 ± 19.12 | 88.43 ± 20.39 | 0.936 b |
| Knee Flexion (Month 2) | 113.91 ± 12.86 | 113.93 ± 13.47 | 0.911 b |
| Knee Flexion (Month 4) | 118.00 ± 11.73 | 116.29 ± 9.15 | 0.343 b |
| Knee Extension (Preop) | 2.59 ± 3.81 | 2.36 ± 2.46 | 0.835 b |
| Knee Extension (Month 1) | 2.55 ± 3.23 | 1.86 ± 1.46 | 0.810 b |
| Knee Extension (Month 2) | 1.14 ± 1.24 | 1.07 ± 2.12 | 0.395 b |
| Knee Extension (Month 4) | 0.82 ± 1.18 | 1.00 ± 1.46 | 0.761 b |
| VAS (Preop) | 1.50 ± 2.17 | 2.21 ± 2.00 | 0.227 b |
| VAS (Month 1) | 1.45 ± 2.24 | 0.93 ± 1.14 | 0.885 b |
| VAS (Month 2) | 1.27 ± 2.05 | 0.71 ± 0.99 | 0.689 b |
| VAS (Month 4) | 0.86 ± 1.49 | 0.57 ± 1.08 | 0.575 b |
| Measured Tibial Tunnel Angle in Sagittal Plane | |||||
|---|---|---|---|---|---|
| 10–20° (n = 9) | 20–30° (n = 12) | 30–40° (n = 11) | 40–50° (n = 6) | ||
| Mean ± SD | Mean ± SD | Mean ± SD | Mean ± SD | p Value | |
| IKDC (Preop) | 40.00 ± 11.80 | 39.83 ± 12.77 | 49.00 ± 13.36 | 48.00 ± 9.61 | 0.197 d |
| IKDC (Month 1) | 42.44 ± 8.51 | 39.58 ± 12.08 | 50.64 ± 13.12 | 46.00 ± 10.23 | 0.199 d |
| IKDC (Month 2) | 45.67 ± 9.51 | 43.83 ± 10.96 | 62.88 ± 11.29 | 45.33 ± 7.68 | 0.004 d |
| IKDC (Month 4) | 46.33 ± 8.98 | 45.92 ± 11.45 | 65.73 ± 13.13 | 45.83 ± 8.70 | 0.004 d |
| LYSHOLM (Preop) | 60.33 ± 17.79 | 63.50 ± 21.58 | 60.82 ± 16.67 | 51.83 ± 18.25 | 0.603 d |
| LYSHOLM (Month 1) | 63.89 ± 24.35 | 63.92 ± 15.68 | 62.73 ± 16.34 | 67.83 ± 26.60 | 0.833 d |
| LYSHOLM (Month 2) | 69.56 ± 26.24 | 69.92 ± 18.28 | 74.82 ± 17.34 | 73.83 ± 17.94 | 0.933 d |
| LYSHOLM (Month 4) | 62.11 ± 20.48 | 75.42 ± 17.49 | 76.00 ± 16.22 | 74.83 ± 19.55 | 0.398 d |
| Knee Flexion (Preop) | 107.56 ± 27.54 | 96.25 ± 33.17 | 123.18 ± 10.78 | 113.83 ± 16.19 | 0.109 d |
| Knee Flexion (Month 1) | 86.67 ± 17.13 | 84.58 ± 23.97 | 93.91 ± 18.71 | 89.17 ± 9.70 | 0.837 d |
| Knee Flexion (Month 2) | 111.67 ± 12.03 | 111.25 ± 13.49 | 113.91 ± 14.59 | 121.33 ± 7.78 | 0.343 d |
| Knee Flexion (Month 4) | 119.78 ± 10.39 | 115.25 ± 13.63 | 117.55 ± 9.55 | 127.17 ± 6.49 | 0.673 d |
| Knee Extension (Preop) | 3.67 ± 4.87 | 3.08 ± 3.17 | 1.27 ± 1.73 | 0.50 ± 0.83 | 0.115 d |
| Knee Extension (Month 1) | 3.33 ± 3.04 | 2.92 ± 4.10 | 1.45 ± 1.36 | 1.67 ± 0.81 | 0.460 d |
| Knee Extension (Month 2) | 1.33 ± 1.58 | 0.83 ± 1.40 | 1.27 ± 2.45 | 1.00 ± 0.63 | 0.533 d |
| Knee Extension (Month 4) | 0.89 ± 0.92 | 1.00 ± 0.34 | 1.27 ± 11.55 | 0 (0–0) | 0.118 d |
| VAS (Preop) | 1.89 ± 1.83 | 1.67 ± 2.18 | 1.18 ± 1.77 | 2.67 ± 2.80 | 0.594 d |
| VAS (Month 1) | 1.78 ± 2.58 | 1.25 ± 1.48 | 0.91 ± 1.92 | 1.50 ± 1.04 | 0.380 d |
| VAS (Month 2) | 1.00 ± 1.00 | 1.42 ± 2.23 | 0.73 ± 1.84 | 0.83 ± 0.98 | 0.546 d |
| VAS (Month 4) | 1.11 ± 1.45 | 0.50 ± 0.90 | 0.64 ± 1.80 | 0.67 ± 0.81 | 0.545 d |
| Tibial Tunnel Position Relative to the Sagittal Plane | ||||
|---|---|---|---|---|
| 0.4–0.6 (n = 17) | 0.6–0.8 (n = 12) | 0.8–1.0 (n = 7) | ||
| Mean ± SD | Mean ± SD | Mean ± SD | p Value | |
| IKDC (Preop) | 42.82 ± 12.07 | 44.42 ± 12.13 | 47.86 ± 17.91 | 0.703 d |
| IKDC (Month 1) | 42.94 ± 15.20 | 43.08 ± 6.50 | 48.29 ± 9.08 | 0.470 d |
| IKDC (Month 2) | 48.71 ± 13.85 | 51.42 ± 10.29 | 47.57 ± 14.38 | 0.668 d |
| IKDC (Month 4) | 50.18 ± 14.38 | 53.67 ± 12.95 | 54.29 ± 17.15 | 0.706 d |
| LYSHOLM (Preop) | 62.29 ± 18.46 | 55.58 ± 18.72 | 65.57 ± 18.87 | 0.409 d |
| LYSHOLM (Month 1) | 64.12 ± 14.23 | 57.67 ± 21.69 | 62.14 ± 24.23 | 0.770 d |
| LYSHOLM (Month 2) | 68.53 ± 16.34 | 69.58 ± 22.30 | 73.14 ± 27.60 | 0.549 d |
| LYSHOLM (Month 4) | 70.12 ± 16.54 | 70.67 ± 18.30 | 76.14 ± 25.59 | 0.568 d |
| Knee Flexion (Preop) | 104.59 ± 30.49 | 114.58 ± 15.44 | 114.29 ± 18.12 | 0.573 d |
| Knee Flexion (Month 1) | 85.00 ± 22.50 | 89.83 ± 19.05 | 92.86 ± 3.93 | 0.828 d |
| Knee Flexion (Month 2) | 111.00 ± 13.46 | 109.17 ± 13.28 | 119.71 ± 10.90 | 0.126 d |
| Knee Flexion (Month 4) | 111.18 ± 9.82 | 118.75 ± 8.82 | 127.71 ± 3.54 | <0.001 d |
| Knee Extension (Preop) | 2.06 ± 3.17 | 2.08 ± 1.83 | 1.57 ± 1.51 | 0.830 d |
| Knee Extension (Month 1) | 2.47 ± 3.48 | 1.92 ± 1.67 | 3.00 ± 3.55 | 0.946 d |
| Knee Extension (Month 2) | 1.06 ± 1.14 | 1.42 ± 2.35 | 0.86 ± 1.86 | 0.555 d |
| Knee Extension (Month 4) | 1.41 ± 1.06 | 0.42 ± 1.44 | 0.14 ± 0.37 | <0.001 d |
| VAS (Preop) | 1.65 ± 2.23 | 2.08 ± 2.31 | 0.57 ± 0.97 | 0.360 d |
| VAS (Month 1) | 0.65 ± 0.86 | 0.75 ± 1.13 | 1.29 ± 1.49 | 0.594 d |
| VAS (Month 2) | 0.94 ± 1.91 | 0.92 ± 1.16 | 0.29 ± 0.48 | 0.624 d |
| VAS (Month 4) | 0.24 ± 0.56 | 0.58 ± 0.90 | 0.14 ± 0.37 | 0.272 d |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Published by MDPI on behalf of the Lithuanian University of Health Sciences. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Yücel, M.O.; Dalaslan, R.E.; Sağlam, S.; Arıcan, M.; Karaduman, Z.O.; Akar, B. Short-Term Clinical Evaluation of Tibial Tunnel Angle and Position in Anatomical Anterior Cruciate Ligament Reconstruction. Medicina 2025, 61, 1107. https://doi.org/10.3390/medicina61061107
Yücel MO, Dalaslan RE, Sağlam S, Arıcan M, Karaduman ZO, Akar B. Short-Term Clinical Evaluation of Tibial Tunnel Angle and Position in Anatomical Anterior Cruciate Ligament Reconstruction. Medicina. 2025; 61(6):1107. https://doi.org/10.3390/medicina61061107
Chicago/Turabian StyleYücel, Mücahid Osman, Raşit Emin Dalaslan, Sönmez Sağlam, Mehmet Arıcan, Zekeriya Okan Karaduman, and Bedrettin Akar. 2025. "Short-Term Clinical Evaluation of Tibial Tunnel Angle and Position in Anatomical Anterior Cruciate Ligament Reconstruction" Medicina 61, no. 6: 1107. https://doi.org/10.3390/medicina61061107
APA StyleYücel, M. O., Dalaslan, R. E., Sağlam, S., Arıcan, M., Karaduman, Z. O., & Akar, B. (2025). Short-Term Clinical Evaluation of Tibial Tunnel Angle and Position in Anatomical Anterior Cruciate Ligament Reconstruction. Medicina, 61(6), 1107. https://doi.org/10.3390/medicina61061107







