Effects of Different Patient and Prosthetic Variables on Marginal Bone Behavior in Dental Implants: A Clinical Retrospective Study
Abstract
1. Introduction
2. Materials and Methods
2.1. Patients and Implants
2.2. Data Collected from Clinical Observation Files
2.3. Data Collected from Radiological Images
2.3.1. Types of Radiological Images Used
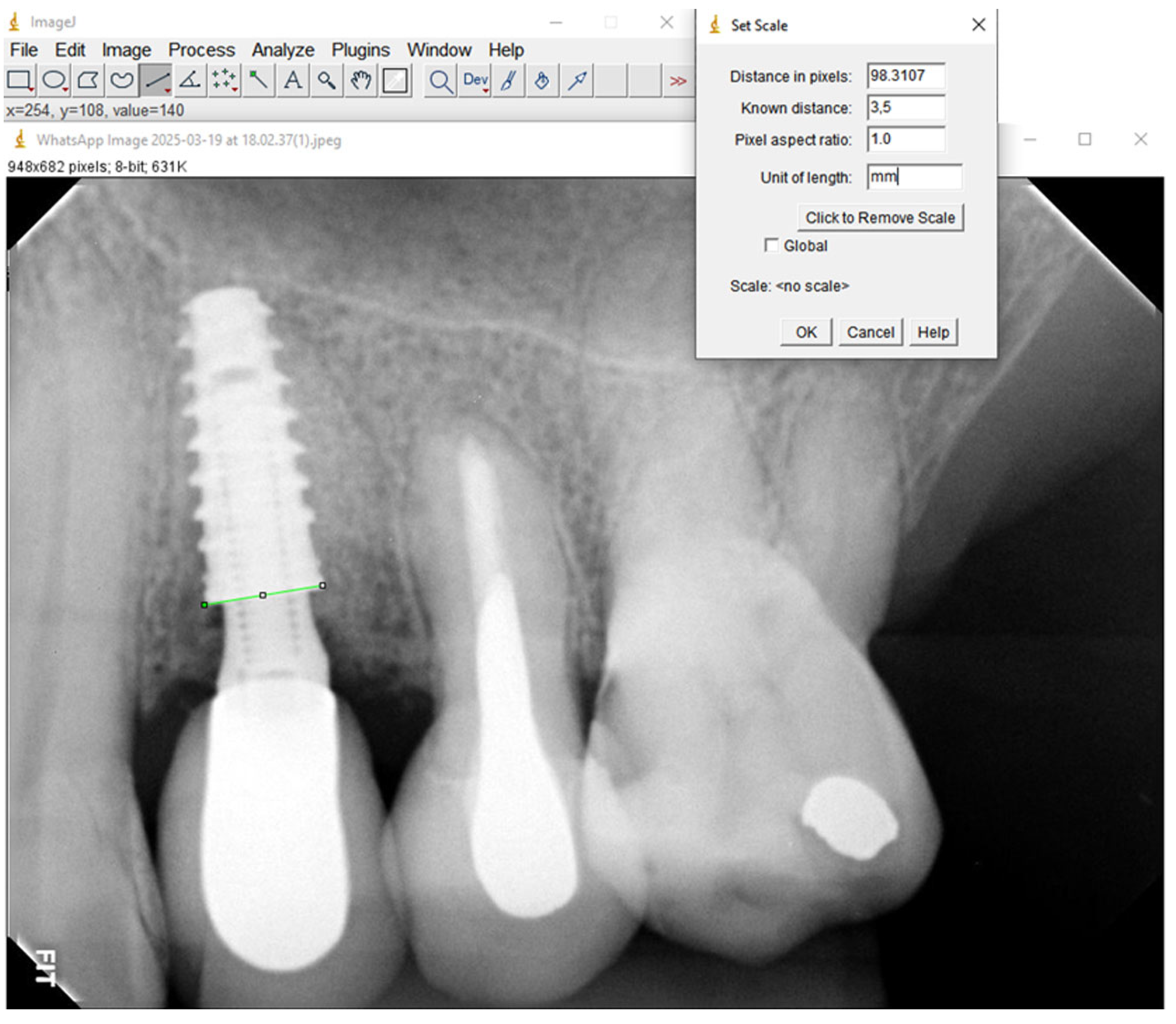
2.3.2. Processing of Radiological Images Using the Software
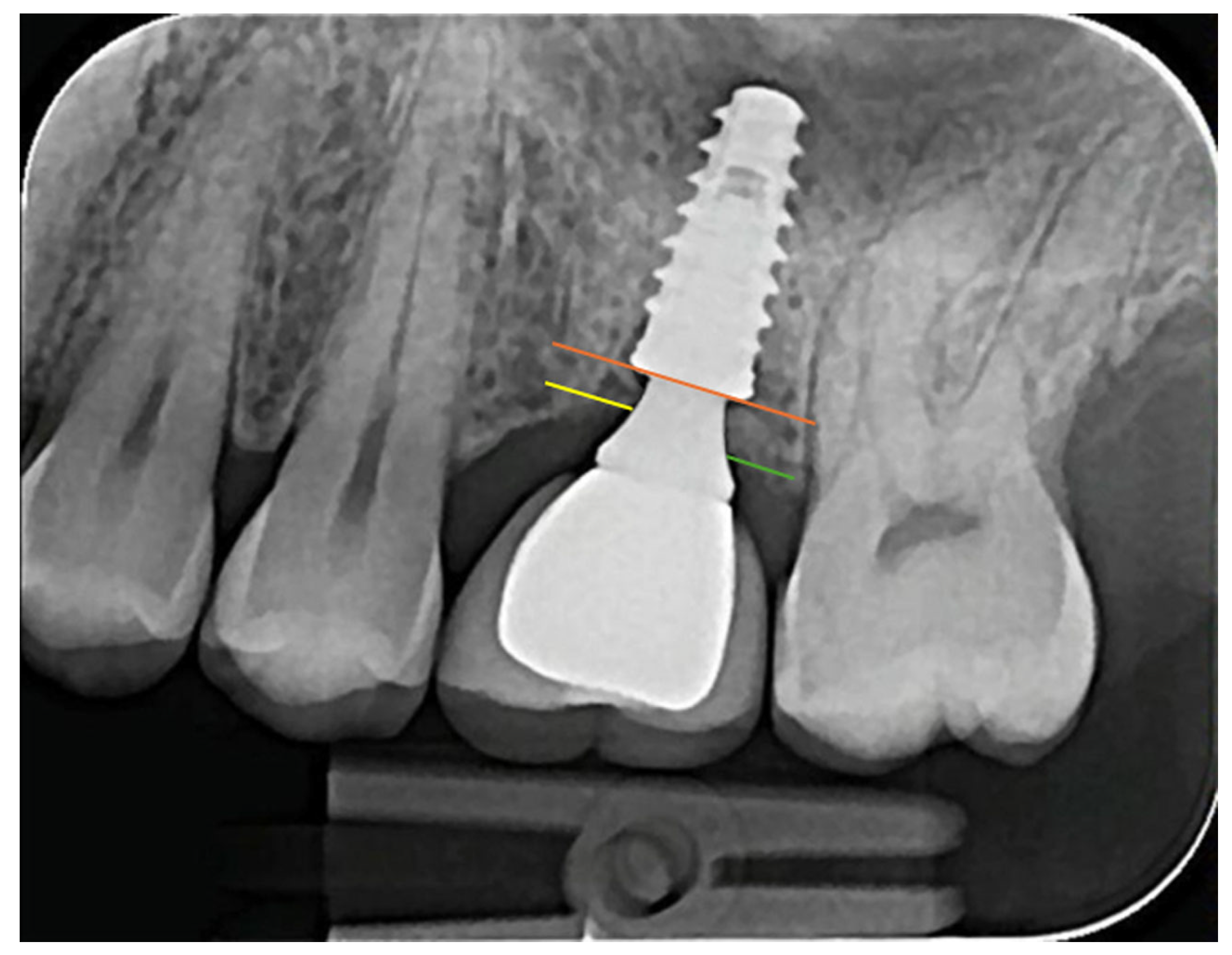
2.3.3. MBL Distance Measurement
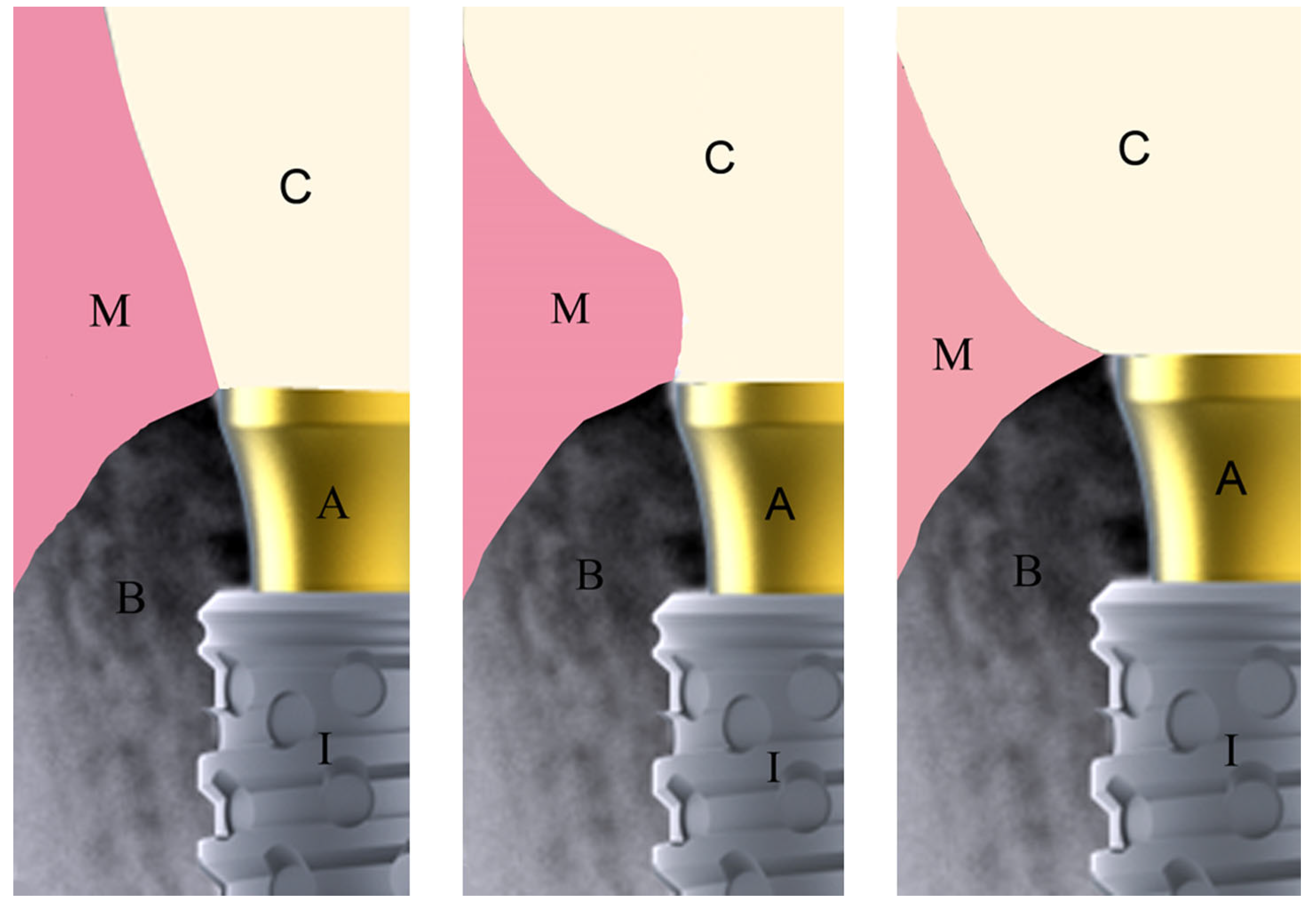
2.3.4. Emergence Profile Measurement
2.4. Examination Data and Error Calculation
2.5. Statistical Analysis
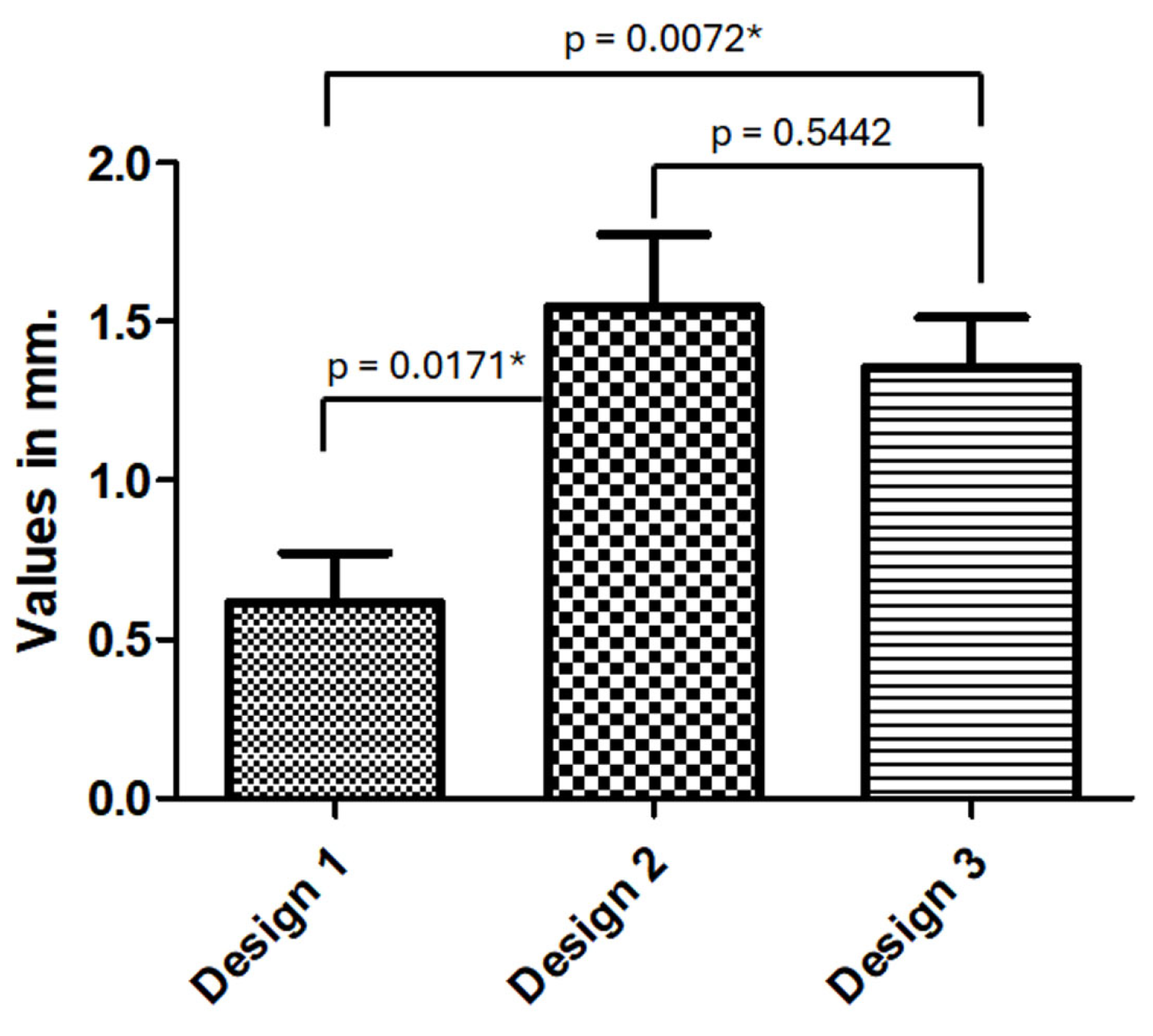
3. Results
4. Discussion
4.1. Influence of Demographic and Anatomic Variables
4.2. Prosthetic Factors: Abutment Height
4.3. Crown Emergence Profile and MBL
4.4. Clinical Implications
4.5. Limitations
- Imaging Modality: MBL was assessed using periapical radiographs, which, while standardized using the parallel cone technique and digital calibration, may be less precise than cone-beam computed tomography (CBCT). Radiographs primarily capture 2D mesial–distal bone changes and may underestimate buccal or lingual bone loss [24].
- Follow-Up Period: The average follow-up time of approximately 12.7 months, although clinically meaningful, does not allow conclusions to be drawn about long-term outcomes. Marginal bone remodeling is a dynamic process that may evolve beyond the first year after loading.
- Sample Size and Study Design: Although 111 IA sets were evaluated, the number of implants in some subgroups (e.g., emergence profile designs) was limited, which could affect the statistical power. Moreover, as a retrospective study, inherent biases related to patient selection, data completeness, and lack of randomization may affect the generalizability of the results.
- Confounding Variables: Despite efforts to control for systemic diseases and smoking, other factors such as oral hygiene, prosthetic material, occlusal loading, and surgical technique could also influence MBL and were not comprehensively analyzed.
- Intra-Observer Reliability: While intra-examiner reliability was assessed (error margin: 0.05 mm), we did not perform inter-observer calibration and measurements.
4.6. Future Directions
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Duong, H.; Roccuzzo, A.; Stähli, A.; Salvi, G.E.; Lang, N.P.; Sculean, A. Oral health-related quality of life of patients rehabilitated with fixed and removable implant-supported dental prostheses. Periodontology 2000 2022, 88, 201–237. [Google Scholar] [CrossRef] [PubMed]
- Sartoretto, S.C.; Shibli, J.A.; Javid, K.; Cotrim, K.; Canabarro, A.; Louro, R.S.; Lowenstein, A.; Mourão, C.F.; Moraschini, V. Comparing the Long-Term Success Rates of Tooth Preservation and Dental Implants: A Critical Review. J. Funct. Biomater. 2023, 14, 142. [Google Scholar] [CrossRef]
- Faur, C.I.; Herman, A.; Leahu, I.; Megiesan, S.; Caluian, I. Marginal Bone Loss Around the Implant: A Retrospective Analysis of Bone Remodeling Over Five Years of Follow-Up. Cureus 2024, 16, e76228. [Google Scholar] [CrossRef]
- Galindo-Moreno, P.; Catena, A.; Pérez-Sayáns, M.; Fernández-Barbero, J.E.; O’Valle, F.; Padial-Molina, M. Early marginal bone loss around dental implants to define success in implant dentistry: A retrospective study. Clin. Implant. Dent. Relat. Res. 2022, 24, 630–642. [Google Scholar] [CrossRef] [PubMed]
- Gehrke, S.A.; Scarano, A.; Cortellari, G.C.; Fernandes, G.V.O.; Mesquita, A.M.M.; Bianchini, M.A. Marginal Bone Level and Biomechanical Behavior of Titanium-Indexed Abutment Base of Conical Connection Used for Single Ceramic Crowns on Morse-Taper Implant: A Clinical Retrospective Study. J. Funct. Biomater. 2023, 14, 128. [Google Scholar] [CrossRef]
- Chankhore, P.; Khubchandani, S.R.; Reche, A.; Paul, P. Prosthetic Design Factors Influencing Peri-Implant Disease: A Comprehensive Review. Cureus 2023, 15, e48737. [Google Scholar] [CrossRef]
- Izzetti, R.; Cinquini, C.; Nisi, M.; Covelli, M.; Alfonsi, F.; Barone, A. Influence of Prosthetic Emergence Profile on Peri-Implant Marginal Bone Stability: A Comprehensive Review. Medicina 2025, 61, 517. [Google Scholar] [CrossRef]
- Doolgindachbaporn, G.; Ongthiemsak, C.; Ruengrungsom, C. Marginal bone changes in cement-retained implant-supported crowns: A systematic review and meta-analysis. J. Prosthet. Dent. 2025, in press. [Google Scholar] [CrossRef] [PubMed]
- Atieh, M.A.; Shah, M.; Hakam, A.; Albalushi, A.; Abdulmunim, A.; AlAli, F.; Alsabeeha, N.H.M. Angled Screw Channel-Retained vs. Cement-Retained Implant Crowns in Nonmolar Sites: A Systematic Review and Meta-Analysis. J. Esthet. Restor. Dent. 2025, in press. [Google Scholar] [CrossRef]
- Jain, R.; Pisulkar, S.G.; Dubey, S.A.; Bansod, A.; Beri, A.; Deshmukh, S. Influence of Crown Height and Width on Marginal Bone Loss and Long-Term Stability of Dental Implants: A Systematic Review. Cureus 2024, 16, e65109. [Google Scholar] [CrossRef]
- Lops, D.; Romeo, E.; Stocchero, M.; Palazzolo, A.; Manfredi, B.; Sbricoli, L. Marginal Bone Maintenance and Different Prosthetic Emergence Angles: A 3-Year Retrospective Study. J. Clin. Med. 2022, 11, 2014. [Google Scholar] [CrossRef] [PubMed]
- Janda, M.; Mattheos, N. Prosthetic design and choice of components for maintenance of optimal peri-implant health: A comprehensive review. Br. Dent. J. 2024, 236, 765–771. [Google Scholar] [CrossRef] [PubMed]
- Ceresuela, P.; Montero, J. Biomechanical Factors in the Prognosis of Implants: A Clinical Study. Prosthesis 2024, 6, 896–912. [Google Scholar] [CrossRef]
- Kowalski, J.; Lapinska, B.; Nissan, J.; Lukomska-Szymanska, M. Factors Influencing Marginal Bone Loss around Dental Implants: A Narrative Review. Coatings 2021, 11, 865. [Google Scholar] [CrossRef]
- Sabău, D.T.; Juncar, R.I.; Moca, A.E.; Bota, T.; Moca, R.T.; Juncar, M. Impact of Prosthetic Material and Restoration Type on Peri-Implant Bone Resorption: A Retrospective Analysis in a Romanian Sample. J. Clin. Med. 2024, 13, 1794. [Google Scholar] [CrossRef]
- Lee, J.-W.; An, J.H.; Park, S.-H.; Chong, J.-H.; Kim, G.-S.; Han, J.; Jung, S.; Kook, M.-S.; Oh, H.-K.; Ryu, S.-Y.; et al. Retrospective clinical study of an implant with a sandblasted, large-grit, acid-etched surface and internal connection: Analysis of short-term success rate and marginal bone loss. Maxillofac. Plast. Reconstr. Surg. 2016, 38, 42. [Google Scholar] [CrossRef]
- Yousefi, F.; Eskandarloo, A.; Arabi, R.; Bidgoli, M.; Poorolajal, J. Association between Marginal Bone Loss and Bone Quality at Dental Implant Sites Based on Evidence from Cone Beam Computed Tomography and Periapical Radiographs. Contemp. Clin. Dent. 2019, 10, 36–41. [Google Scholar] [CrossRef]
- Ayele, S.; Sharo, N.; Chrcanovic, B.R. Marginal bone loss around dental implants: Comparison between diabetic and non-diabetic patients-a retrospective clinical study. Clin. Oral Investig. 2023, 27, 2833–2841. [Google Scholar] [CrossRef]
- Velasco-Ortega, E.; Jiménez-Guerra, A.; Ortiz-Garcia, I.; Garrido, N.M.; Moreno-Muñoz, J.; Núñez-Márquez, E.; Rondón-Romero, J.L.; Cabanillas-Balsera, D.; López-López, J.; Monsalve-Guil, L. Implant Treatment by Guided Surgery Supporting Overdentures in Edentulous Mandible Patients. Int. J. Environ. Res. Public Health 2021, 18, 11836. [Google Scholar] [CrossRef]
- Flanagan, D. Osseous Remodeling Around Dental Implants. J. Oral Implant. 2019, 45, 239–246. [Google Scholar] [CrossRef]
- Gehrke, S.A.; Bercianos, M.; Aguerrondo, J.G.; Calvo-Guirado, J.L.; Prados-Frutos, J.C. Influence of Mucosal Thickness, Implant Dimensions and Stability in Cone Morse Implant Installed at Subcrestal Bone Level on the Peri-Implant Bone: A Prospective Clinical and Radiographic Study. Symmetry 2019, 11, 1138. [Google Scholar] [CrossRef]
- Yi, Y.; Koo, K.; Schwarz, F.; Ben Amara, H.; Heo, S. Association of prosthetic features and peri-implantitis: A cross-sectional study. J. Clin. Periodontol. 2020, 47, 392–403. [Google Scholar] [CrossRef] [PubMed]
- Katafuchi, M.; Weinstein, B.F.; Leroux, B.G.; Chen, Y.; Daubert, D.M. Restoration contour is a risk indicator for peri-implantitis: A cross-sectional radiographic analysis. J. Clin. Periodontol. 2017, 45, 225–232. [Google Scholar] [CrossRef] [PubMed]
- Atieh, M.A.; Shah, M.; Ameen, M.; Tawse-Smith, A.; Alsabeeha, N.H.M. Influence of implant restorative emergence angle and contour on peri-implant marginal bone loss: A systematic review and meta-analysis. Clin. Implant. Dent. Relat. Res. 2023, 25, 840–852. [Google Scholar] [CrossRef]
- Inoue, M.; Nakano, T.; Shimomoto, T.; Kabata, D.; Shintani, A.; Yatani, H. Multivariate analysis of the influence of prosthodontic factors on peri-implant bleeding index and marginal bone level in a molar site: A cross-sectional study. Clin. Implant. Dent. Relat. Res. 2020, 22, 713–722. [Google Scholar] [CrossRef]
- Lin, I.; Chen, S.; Chang, C.; Chang, J.Z.; Sun, J.; Chang, C.H. Morphology of Peri-Implant Tissues Around Permanent Prostheses With Various Emergence Angles Following Free Gingival Grafting. J. Prosthodont. 2022, 31, 681–688. [Google Scholar] [CrossRef]
- Soulami, S.; Slot, D.E.; van der Weijden, F. Implant-abutment emergence angle and profile in relation to peri-implantitis: A systematic review. Clin. Exp. Dent. Res. 2022, 8, 795–806. [Google Scholar] [CrossRef]


| Inclusion Criteria | Exclusion Criteria |
|---|---|
| Individuals who had implant-supported rehabilitation installed at least one year before the initiation of the study | Individuals who had taken medications influencing bone remodeling within the preceding six months (e.g., bisphosphonates) |
| Individuals receiving either single or multiple implants | Pregnant or lactating women |
| Patients aged 18 years or older | Cases with missing or incomplete information |
| Implants featuring a 3.5 mm diameter and Morse taper connection | Physical disorders which would interfere with the ability to maintain oral health care |
| No systemic diseases (e.g., diabetes, osteoporosis, hypertension, etc.) | |
| Controlled periodontal conditions | |
| Individuals who smoked fewer than 10 cigarettes per day |
| Independent Variables (in mm) | MBLm | MBLd | p-Value |
|---|---|---|---|
| General | (n = 111) −1.34 ± 1.24 | (n = 111) −1.29 ± 1.22 | 0.3214 |
| Female | (n = 54) −1.04 ± 0.93 | (n = 54) −1.16 ± 0.91 | 0.7916 |
| Male | (n = 57) −1.71 ± 1.57 | (n = 57) −1.41 ± 1.44 | 0.1205 |
| Age (33 to 64) | (n = 49) −1.48 ± 1.42 | (n = 49) −1.49 ± 1.43 | 0.7411 |
| Age (65 to 81) | (n = 62) −1.30 ± 1.27 | (n = 62) −1.13 ± 0.99 | 0.3348 |
| Maxilla | (n = 76) −1.67 ± 1.44 | (n = 76) −1.57 ± 1.33 | 0.6879 |
| Mandible | (n = 35) −0.72 ± 0.72 | (n = 35) −0.63 ± 0.46 | 0.0885 |
| Anterior | (n = 23) −1.84 ± 1.37 | (n = 23) −1.79 ± 1.29 | 0.8778 |
| Posterior | (n = 88) −1.26 ± 1.31 | (n = 88) −1.15 ± 1.17 | 0.2717 |
| Comparison | Mean Diff. | t | p-Value | 95% CI of Diff. |
|---|---|---|---|---|
| TMh1 vs. TMh2 | 0.5949 | 2.166 | 0.0024 | −0.06780 to 1.258 |
| TMh1 vs. TMh3 | 1.039 | 4.182 | 0.0033 | 0.4396 to 1.638 |
| TMh2 vs. TMh3 | 0.4441 | 2.322 | 0.0017 | −0.01728 to 0.9056 |
| n (%) | MBLr (±SD) | p-Value | F-Value | df | Angle (±SD) | p-Value | F-Value | df | |
|---|---|---|---|---|---|---|---|---|---|
| D.E. profile | 0.0176 * | 3.913 | <0.0001 * | 10.70 | |||||
| Design 1 | 19 (17.1%) | 0.62 (±0.68) | 2 (df 1) | 14.74 (±5.65) | 2 (df 1) | ||||
| Design 2 | 33 (29.7%) | 1.54 (±1.32) | 108 (df 2) | 23.26 (±13.25) | 108 (df 2) | ||||
| Design 3 | 59 (53.2%) | 1.35 (±1.23) | 110 (df 3) | 31.05 (±15.98) | 110 (df 3) | ||||
| M.E. profile | 0.0545 | 3.573 | <0.0001 * | 3.272 | |||||
| Design 1 | 16 (14.4%) | 1.54 (±1.72) | 2 (df 1) | 16.07 (±6.35) | 2 (df 1) | ||||
| Design 2 | 39 (35.1%) | 1.78 (±1.51) | 108 (df 2) | 23.67 (±9.54) | 108 (df 2) | ||||
| Design 3 | 56 (50.5%) | 1.06 (±0.98) | 110 (df 3) | 35.05 (±13.36) | 110 (df 3) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Published by MDPI on behalf of the Lithuanian University of Health Sciences. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Gehrke, S.A.; Scarano, A.; Lorusso, F.; Balduino, T.Y.; Bianchini, M.A. Effects of Different Patient and Prosthetic Variables on Marginal Bone Behavior in Dental Implants: A Clinical Retrospective Study. Medicina 2025, 61, 1041. https://doi.org/10.3390/medicina61061041
Gehrke SA, Scarano A, Lorusso F, Balduino TY, Bianchini MA. Effects of Different Patient and Prosthetic Variables on Marginal Bone Behavior in Dental Implants: A Clinical Retrospective Study. Medicina. 2025; 61(6):1041. https://doi.org/10.3390/medicina61061041
Chicago/Turabian StyleGehrke, Sergio Alexandre, Antonio Scarano, Felice Lorusso, Thalles Yurgen Balduino, and Marco Aurélio Bianchini. 2025. "Effects of Different Patient and Prosthetic Variables on Marginal Bone Behavior in Dental Implants: A Clinical Retrospective Study" Medicina 61, no. 6: 1041. https://doi.org/10.3390/medicina61061041
APA StyleGehrke, S. A., Scarano, A., Lorusso, F., Balduino, T. Y., & Bianchini, M. A. (2025). Effects of Different Patient and Prosthetic Variables on Marginal Bone Behavior in Dental Implants: A Clinical Retrospective Study. Medicina, 61(6), 1041. https://doi.org/10.3390/medicina61061041









