Non-Thyroidal Illness Syndrome: A Predictor of Non-Invasive Ventilation Failure and Mortality in Critically Ill Patients
Abstract
1. Introduction
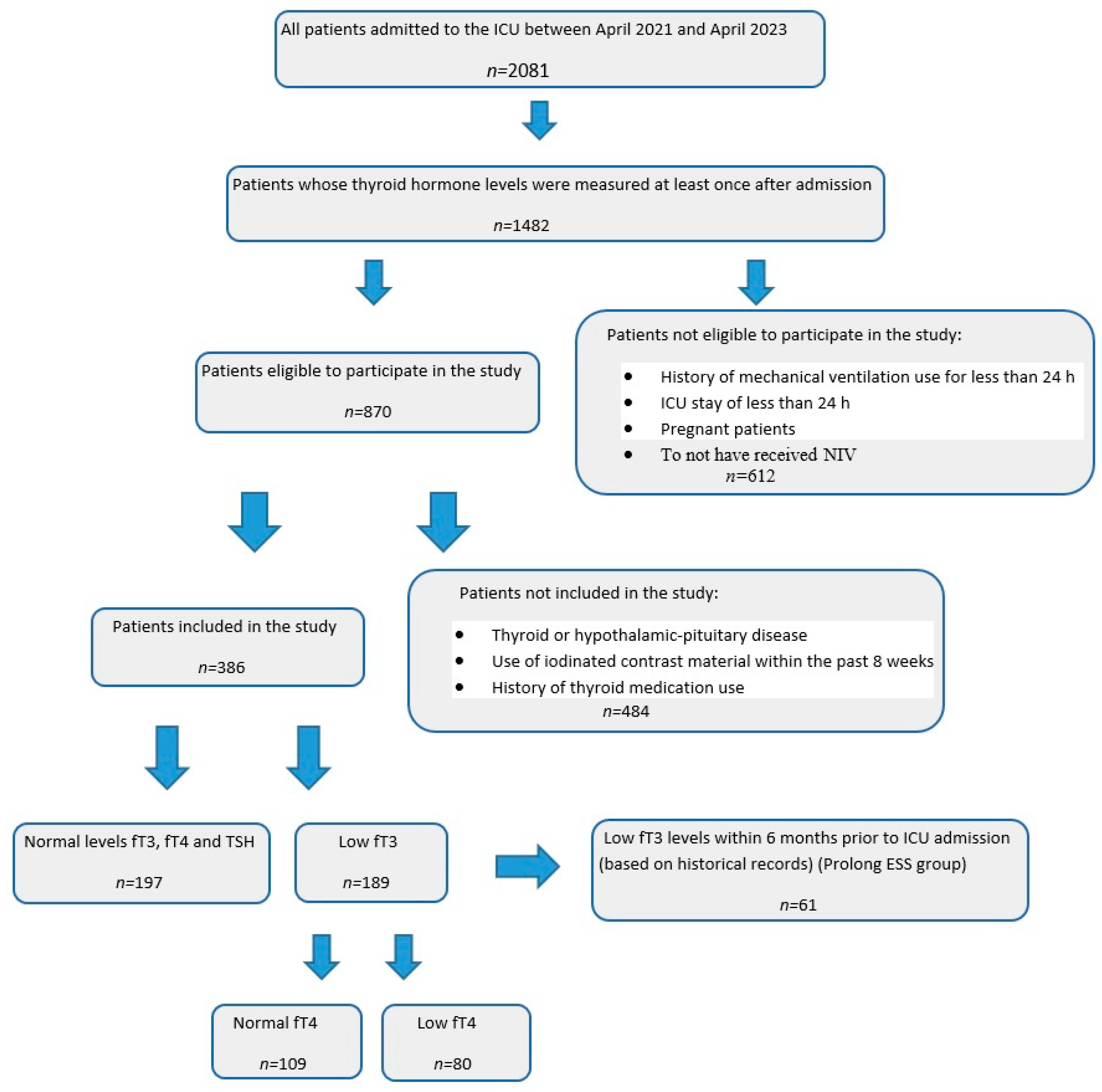
2. Materials and Methods
2.1. Setting and Study Design
2.2. Data Collection
2.3. Primary Secondary Outcomes
2.4. Statistical Analyses
3. Results
3.1. Patient Demographics and Clinical Characteristics
3.2. Clinical Scores and Laboratory Findings
3.3. Mortality and NIV Failure
3.4. Length of ICU Stay
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Data Availability Statement
Conflicts of Interest
References
- De Groot, L.J. Non-thyroidal illness syndrome is a manifestation of hypothalamic-pituitary dysfunction, and in view of current evidence, should be treated with appropriate replacement therapies. Crit. Care Clin. 2006, 22, 57–86. [Google Scholar] [CrossRef] [PubMed]
- Williams Textbook of Endocrinology-13th Edition. Available online: https://www.elsevier.com/books/williams-textbook-of-endocrinology/melmed/978-0-323-29738-7 (accessed on 17 June 2020).
- Téblick, A.; Langouche, L.; Van den Berghe, G. Anterior pituitary function in critical illness. Endocr. Connect. 2019, 8, R131–R143. [Google Scholar] [CrossRef] [PubMed]
- Wartofsky, L.; Burman, K.D. Alterations in thyroid function in patients with systemic illness: The “euthyroid sick syndrome”. Endocr. Rev. 1982, 3, 164–217. [Google Scholar] [CrossRef]
- Castro, I.; Quisenberry, L.; Calvo, R.-M.; Obregon, M.-J.; Lado-Abeal, J. Septic shock non-thyroidal illness syndrome causes hypothyroidism and conditions for reduced sensitivity to thyroid hormone. J. Mol. Endocrinol. 2013, 50, 255–266. [Google Scholar] [CrossRef]
- De Luca, R.; Davis, P.J.; Lin, H.-Y.; Gionfra, F.; Percario, Z.A.; Affabris, E.; Pedersen, J.Z.; Marchese, C.; Trivedi, P.; Anastasiadou, E.; et al. Thyroid Hormones Interaction with Immune Response, Inflammation and Non-thyroidal Illness Syndrome. Front. Cell Dev. Biol. 2021, 8, 614030. [Google Scholar] [CrossRef]
- Gheorghiţă, V.; Barbu, A.E.; Gheorghiu, M.L.; Căruntu, F.A. Endocrine dysfunction in sepsis: A beneficial or deleterious host response? GERMS 2015, 5, 17–25. [Google Scholar] [CrossRef]
- Siafakas, N.M.; Salesiotou, V.; Filaditaki, V.; Tzanakis, N.; Thalassinos, N.; Bouros, D. Respiratory muscle strength in hypothyroidism. Chest 1992, 102, 189–194. [Google Scholar] [CrossRef]
- Dulchavsky, S.A.; Kennedy, P.R.; Geller, E.R.; Maitra, S.R.; Foster, W.M.; Langenbeck, E.G. T3 preserves respiratory function in sepsis. J. Trauma 1991, 31, 753–758. [Google Scholar] [CrossRef]
- Khaleeli, A.A.; Griffith, D.G.; Edwards, R.H. The clinical presentation of hypothyroid myopathy and its relationship to abnormalities in structure and function of skeletal muscle. Clin. Endocrinol. 1983, 19, 365–376. [Google Scholar] [CrossRef] [PubMed]
- Arem, R.; Wiener, G.J.; Kaplan, S.G.; Kim, H.S.; Reichlin, S.; Kaplan, M.M. Reduced tissue thyroid hormone levels in fatal illness. Metabolism 1993, 42, 1102–1108. [Google Scholar] [CrossRef] [PubMed]
- Bello, G.; Pennisi, M.A.; Montini, L.; Silva, S.; Maviglia, R.; Cavallaro, F.; Bianchi, A.; De Marinis, L.; Antonelli, M. Nonthyroidal illness syndrome and prolonged mechanical ventilation in patients admitted to the ICU. Chest 2009, 135, 1448–1454. [Google Scholar] [CrossRef]
- Schönhofer, B. Starting and stopping acute NİV: When and why? In ERS Practical Handbook of Noninvasive Ventilation; Simonds, A.K., Ed.; Latimer Trend: Sheffield, UK, 2015; pp. 102–110. [Google Scholar]
- Rothberger, G.D.; Valestra, P.K.; Knight, K.; Desai, A.K.; Calixte, R.; Shapiro, L.E. Low Free T3 Is Associated with Worse Outcomes in Patients in the ICU Requiring Invasive Mechanical Ventilation. J. Intensiv. Care Med. 2021, 36, 313–318. [Google Scholar] [CrossRef]
- Evans, T.W. International Consensus Conferences in Intensive Care Medicine: Noninvasive positive pressure ventilation in acute Respiratory failure: Organized jointly by the American Thoracic Society, the European Respiratory Society, the European Society of Intensive Care Medicine, and the Société de Réanimation de Langue Française, and approved by ATS Board of Directors, December 2000. Am. J. Respir. Crit. Care Med. 2001, 163, 283–291. [Google Scholar] [CrossRef]
- Gao, W.; Guo, W.; Guo, Y.; Shi, M.; Dong, G.; Wang, G.; Ge, Q.; Zhu, J.; Zhou, X. Thyroid hormone concentrations in severely or critically ill patients with COVID-19. J. Endocrinol. Investig. 2021, 44, 1031–1040. [Google Scholar] [CrossRef]
- Zou, R.; Wu, C.; Zhang, S.; Wang, G.; Zhang, Q.; Yu, B.; Wu, Y.; Dong, H.; Wu, G.; Wu, S.; et al. Euthyroid Sick Syndrome in Patients with COVID-19. Front. Endocrinol. 2020, 11, 566439. [Google Scholar] [CrossRef]
- Su, W.; Zhao, X.Q.; Wang, M.; Chen, H.; Li, H.W. Low T3 syndrome improves risk prediction of in-hospital cardiovascular death in patients with acute myocardial infarction. J. Cardiol. 2018, 72, 215–219. [Google Scholar] [CrossRef]
- Wang, B.; Liu, S.; Li, L.; Yao, Q.; Song, R.; Shao, X.; Li, Q.; Shi, X.; Zhang, J.A. Non-thyroidal illness syndrome in patients with cardiovascular diseases: A systematic review and meta-analysis. Int. J. Cardiol. 2017, 226, 1–10. [Google Scholar] [CrossRef]
- Lamba, N.; Liu, C.; Zaidi, H.; Broekman, M.L.D.; Simjian, T.; Shi, C.; Doucette, J.; Ren, S.; Smith, T.R.; Mekary, R.A.; et al. A prognostic role for low triiodothyronine syndrome in acute stroke patients: A systematic review and meta-analysis. Clin. Neurol. Neurosurg. 2018, 169, 55–63. [Google Scholar] [CrossRef]
- Schultheiss, U.T.; Steinbrenner, I.; Nauck, M.; Schneider, M.P.; Kotsis, F.; Baid-Agrawal, S.; Schaeffner, E.; Eckardt, K.-U.; Köttgen, A.; Sekula, P.; et al. Thyroid function, renal events and mortality in chronic kidney disease patients: The German Chronic Kidney Disease study. Clin. Kidney J. 2021, 14, 959–968. [Google Scholar] [CrossRef]
- Vaughan, G.M.; Mason, A.D., Jr.; McManus, W.F.; Pruitt, B.A., Jr. Alterations of mental status and thyroid hormones after thermal injury. J. Clin. Endocrinol. Metab. 1985, 60, 1221–1225. [Google Scholar] [CrossRef]
- Wang, F.; Pan, W.; Wang, H.; Wang, S.; Pan, S.; Ge, J. Relationship between thyroid function and ICU mortality: A prospective observation study. Crit. Care 2012, 16, R11. [Google Scholar] [CrossRef] [PubMed]
- Guo, J.; Hong, Y.; Wang, Z.; Li, Y. Analysis of the Incidence of Euthyroid Sick Syndrome in Comprehensive Intensive Care Units and Related Risk Factors. Front. Endocrinol. 2021, 12, 656641. [Google Scholar] [CrossRef] [PubMed]
- Świstek, M.; Broncel, M.; Gorzelak-Pabiś, P.; Morawski, P.; Fabiś, M.; Woźniak, E. Euthyroid Sick Syndrome as a Prognostic Indicator of COVID-19 Pulmonary Involvement, Associated with Poorer Disease Prognosis and Increased Mortality. Endocr. Pract. 2022, 28, 494–501. [Google Scholar] [CrossRef]
- Asai, K.; Shirakabe, A.; Kiuchi, K.; Kobayashi, N.; Okazaki, H.; Matsushita, M.; Shibata, Y.; Goda, H.; Shigihara, S.; Asano, K.; et al. Relation of Low Triiodothyronine Syndrome Associated with Aging and Malnutrition to Adverse Outcome in Patients with Acute Heart Failure. Am. Cardiol. 2020, 125, 427–435. [Google Scholar] [CrossRef]
- Fastiggi, M.; Meneghel, A.; Gutierrez de Rubalcava Doblas, J.; Vittadello, F.; Tirelli, F.; Zulian, F.; Martini, G. Prognostic role of euthyroid sick syndrome in MIS-C: Results from a single-center observational study. Front. Pediatr. 2023, 11, 1217151. [Google Scholar] [CrossRef]
- Krug, N.; Bercker, S.; Busch, T.; Friese, S.; Jahn, N.; Voelker, N.T. Non-thyroidal Illness Syndrome (NTIS) is no independent predictor for mortality in ICU patients. BMC Anesthesiol. 2023, 23, 103. [Google Scholar] [CrossRef]
- Spencer, C.; Eigen, A.; Shen, D.; Duda, M.; Qualls, S.; Weiss, S.; Nicoloff, J. Specificity of sensitive assays of thyrotropin (TSH) used to screen for thyroid disease in hospitalized patients. Clin. Chem. 1987, 33, 1391–1396. [Google Scholar] [CrossRef]
- Ning, N.; Li, J.; Sun, W.; Ma, C.; Li, J.; Sheng, H.; Chen, Y.; Zhao, B.; Zhang, J.; Zhu, J.; et al. Different subtypes of nonthyroidal illness syndrome on the prognosis of septic patients: A two-centered retrospective cohort study. Front. Endocrinol. 2023, 14, 1227530. [Google Scholar] [CrossRef]
- Shi, C.; Bao, Y.; Chen, X.; Tian, L. The Effectiveness of Thyroid Hormone Replacement Therapy on Heart Failure and Low-Triiodothyronine Syndrome: An Updated Systematic Review and Meta-analysis of Randomized Controlled Trials. Endocr. Pract. 2022, 28, 1178–1186. [Google Scholar] [CrossRef]
- Kovacevic, M.; Adam, V.N.; Causevic, S. Triiodothyronine hormone supplementation therapy in septic shock patients with euthyroid sick syndrome: Two pilot, placebo-controlled, randomized trials. Anaesth. Crit. Care Pain Med. 2024, 43, 101336. [Google Scholar] [CrossRef]

| Parameters | Total Patients n = 386 | Survived n = 332 | Deceased n = 54 | p-Value |
|---|---|---|---|---|
| Age, years | 65 (36-89) | 65 (43-89) | 66 (36-79) | 0.212 |
| Gender, male | 205 (53.1) | 152 (45.8) | 29 (53.7) | 0.279 |
| Patient’s groups | 0.005 | |||
| 197 (51.0) | 179 (53.9) | 18 (33.3) | |
| 189 (49.0) | 153 (46.1) | 36 (66.7) | |
| Low fT3 (total n = 189) | <0.001 | |||
| 128 (67.7) | 113 (73.9) | 15 (41.7) | |
| 61 (32.3) | 40 (26.1) | 21 (58.3) | |
| ESS subgroups (total n = 189) | <0.001 | |||
| 109 (57.7) | 98 (64.1) | 11 (30.6) | |
| 80 (42.3) | 55 (35.9) | 25 (69.4) | |
| Reasons for ICU admission | ||||
| 112 (29.0) | 100 (30.1) | 12 (22.2) | 0.236 |
| 122 (31.6) | 99 (29.8) | 23 (42.6) | 0.061 |
| 120 (31.1) | 106 (31.9) | 14 (25.9) | 0.377 |
| 20 (5.2) | 18 (5.4) | 2 (3.7) | 1.000 |
| 8 (2.1) | 7 (2.1) | 1 (1.9) | 1.000 |
| 4 (1.0) | 4 (1.2) | 2 (3.7) | 0.199 |
| Comorbidities | ||||
| 218 (56.5) | 194 (58.4) | 24 (44.4) | 0.054 |
| 185 (47.9) | 162 (48.8) | 23 (42.6) | 0.397 |
| 174 (45.1) | 151 (45.5) | 23 (42.6) | 0.692 |
| 28 (7.3) | 25 (7.5) | 3 (5.6) | 0.781 |
| Other clinical variables | ||||
| 58 (15.0) | 44 (13.3) | 14 (25.9) | 0.016 |
| 103 (26.7) | 86 (25.9) | 17 (31.5) | 0.390 |
| 136 (35.2) | 87 (26.2) | 49 (90.7) | <0.001 |
| 175 (45.1) | 156 (47.0) | 19 (35.2) | 0.106 |
| 9 (0–17) | 8 (0–17) | 12 (3–15) | <0.001 |
| 18 (15–29) | 18 (15–29) | 24.5 (15–29) | <0.001 |
| 15 (12–15) | 15 (12–15) | 15 (13–15) | 0.920 |
| 5 (2–14) | 5 (2–13) | 7 (4–14) | <0.001 |
| 7 (3-18) | 7 (3–18) | 11 (6–18) | <0.001 |
| Laboratory findings | ||||
| 7.19 (7.05–7.33) | 7.19 (7.05–7.33) | 7.21 (7.05–7.33) | 0.373 |
| 60 (47–75) | 60 (48–75) | 58.5 (47–73) | 0.162 |
| 33 (26–43) | 33 (26–43) | 31.5 (27–43) | 0.090 |
| 74 (53–88) | 74 (53–88) | 72 (61–88) | 0.254 |
| 1.8 (1–3.2) | 1.7 (1–2.7) | 2.3 (1–3.2) | <0.001 |
| 1.69 (0.18–4.2) | 1.7 (0.21–4.2) | 1.64 (0.18–4.12) | 0.670 |
| 2.02 (0.1–4.4) | 2.11 (0.1–4.4) | 1.3 (0.19–4.4) | 0.002 |
| 12.41 (9.2–17) | 12.38 (9.2–17) | 13.32 (9.3–17) | 0.011 |
| 103.63 (1.1–198.83) | 99.11 (1.1–198.83) | 123.86 (18.6–193.97) | 0.002 |
| Parameters | Non-ESS Group n = 197 | ESS Group n = 189 | p-Value |
|---|---|---|---|
| Gender, male | 110 (55.8) | 95 (50.3) | 0.273 |
| Age, years | 65 (43–89) | 65 (36-86) | 0.780 |
| Reasons for ICU admission | |||
| 58 (29.4) | 54 (28.6) | 0.851 |
| 60 (30.5) | 62 (32.8) | 0.620 |
| 61 (31.0) | 59 (31.2) | 0.957 |
| 9 (4.6) | 11 (5.8) | 0.579 |
| 6 (3.0) | 2 (1.1) | 0.285 |
| 3 (1.5) | 3 (1.6) | 1.000 |
| Comorbidities | |||
| 115 (58.4) | 103 (54.5) | 0.442 |
| 99 (50.3) | 86 (45.5) | 0.350 |
| 91 (46.2) | 83 (43.9) | 0.653 |
| 17 (8.6) | 11 (5.8) | 0.287 |
| Other clinical variables | |||
| 33 (16.8) | 25 (13.2) | 0.333 |
| 58 (29.4) | 45 (23.8) | 0.211 |
| 18 (9.1) | 36 (19.0) | 0.005 |
| 52 (26.4) | 84 (44.4) | <0.001 |
| 90 (45.7) | 85 (45.0) | 0.888 |
| 8 (1–17) | 10 (0–17) | 0.089 |
| 17 (15–29) | 18 (15–29) | <0.001 |
| 15 (12–15) | 15 (12–15) | 0.257 |
| 4 (2–8) | 6 (3–14) | <0.001 |
| 6 (3–15) | 8 (4–18) | <0.001 |
| Laboratory findings | |||
| 7.19 (7.05–7.33) | 7.19 (7.05–7.33) | 0.927 |
| 60 (48–73) | 60 (47–75) | 0.717 |
| 32 (26–43) | 34 (26–43) | 0.003 |
| 74 (53–88) | 74 (53–88) | 0.718 |
| 1.7 (1–2.8) | 1.8 (1–3.2) | 0.200 |
| 1.54 (0.27–4.2) | 1.85 (0.18–4.12) | 0.058 |
| 2.87 (2–4.4) | 1.2 (0.1–1.93) | <0.001 |
| 12.4 (9.3–17) | 12.49 (9.2–17) | 0.429 |
| 99.7 (1.5–198.83) | 105.81 (1.1–198.26) | 0.106 |
| Parameters | Patients Without NIV Failure n = 250 | Patients With NIV Failure n = 136 | p-Value |
|---|---|---|---|
| Gender, male | 131 (52.4) | 7 (54.4) | 0.705 |
| Age, years | 65 (45–89) | 65 (36–86) | 0.814 |
| Patient’s groups | <0.001 | ||
| 145 (58.0) | 52 (38.2) | |
| 105 (42.0) | 84 (61.8) | |
| Low fT3 (total n = 189) | 0.002 | ||
| 81 (77.1) | 47 (56.0) | |
| 24 (22.9) | 37 (44.0) | |
| ESS subgroups (total n = 189) | 0.107 | ||
| 66 (62.9) | 43 (51.2) | |
| 39 (37.1) | 41 (48.8) | |
| Reasons for ICU admission | |||
| 79 (31.6) | 33 (24.3) | 0.129 |
| 78 (31.2) | 44 (32.4) | 0.816 |
| 73 (29.2) | 47 (34.6) | 0.277 |
| 13 (5.2) | 7 (5.1) | 0.982 |
| 5 (2.0) | 3 (2.2) | 0.892 |
| 3 (1.2) | 3 (2.2) | 0.445 |
| Comorbidities | |||
| 149 (59.6) | 69 (50.7) | 0.093 |
| 123 (49.2) | 62 (45.6) | 0.497 |
| 123 (49.2) | 51 (37.5) | 0.027 |
| 19 (7.6) | 9 (6.6) | 0.722 |
| Other clinical variables | |||
| 38 (15.2) | 20 (14.7) | 0.897 |
| 67 (26.8) | 36 (26.5) | 0.944 |
| 5 (2.0) | 49 (36.0) | <0.001 |
| 127 (50.8) | 48 (35.3) | 0.003 |
| 6 (0–17) | 12 (4–17) | <0.001 |
| 17 (15–28) | 22 (15–29) | <0.001 |
| 15 (12–15) | 15 (13–15) | 0.781 |
| 4 (2-9) | 7 (3–14) | <0.001 |
| 6 (3–15) | 10 (4–18) | <0.001 |
| Laboratory findings | |||
| 7.2 (7.05–7.33) | 7.19 (7.05–7.33) | 0.096 |
| 59 (48–73) | 61 (47–75) | 0.163 |
| 33 (26–42) | 34 (27–43) | 0.269 |
| 74 (53–88) | 73 (53–88) | 0.059 |
| 1.6 (1–2.7) | 2.1 (1–3.2) | <0.001 |
| 1.67 (0.21–4.2) | 1.71 (0.18–4.12) | 0.705 |
| 2.21 (0.1–4.4) | 1.44 (0.19–4.4) | <0.001 |
| 12.36 (9.2–17) | 12.72 (9.28–17) | 0.561 |
| 84.43 (1.1–198.83) | 120.45 (7.46–194.13) | <0.001 |
| Parameters | Patients Without Low fT3 Levels Before ICU Admission n = 128 | Patients with Low fT3 Levels Before ICU Admission (Prolonged ESS Groups) n = 61 | p-Value |
|---|---|---|---|
| Gender, male | 69 (53.9) | 26 (42.6) | 0.147 |
| Age, years | 65 (43-86) | 65 (36–79) | 0.622 |
| ESS subgroups (total n = 189) | <0.001 | ||
| 92 (71.9) | 17 (27.9) | |
| 36 (28.1) | 44 (72.1) | |
| Reasons for ICU admission | |||
| 41 (32.0) | 13 (21.3) | 0.127 |
| 38 (29.7) | 24 (39.3) | 0.186 |
| 40 (31.3) | 19 (31.1) | 0.989 |
| 7 (5.5) | 4 (6.6) | 0.749 |
| 2 (1.6) | 0 (0.0) | 1.000 |
| 2 (1.6) | 1 (1.6) | 1.000 |
| Comorbidities | |||
| 81 (63.3) | 22 (36.1) | <0.001 |
| 60 (46.9) | 26 (42.6) | 0.583 |
| 62 (48.4) | 21 (34.4) | 0.070 |
| 10 (7.8) | 1 (1.6) | 0.090 |
| Other clinical variables | |||
| 16 (12.5) | 9 (14.8) | 0.669 |
| 28 (21.9) | 17 (27.9) | 0.366 |
| 15 (11.7) | 21 (34.4) | <0.001 |
| 47 (36.7) | 37 (60.7) | 0.002 |
| 66 (51.6) | 19 (31.1) | 0.008 |
| 8.5 (0–17) | 11 (3–15) | <0.001 |
| 18 (15–29) | 19 (15–28) | 0.057 |
| 15 (12–15) | 15 (12–15) | 0.818 |
| 6 (3–13) | 7 (3–14) | Table 7 |
| 7.5 (4–18) | 10 (4–18) | <0.001 |
| Laboratory findings | |||
| 7.19 (7.05–7.33) | 7.19 (7.07–7.33) | 0.870 |
| 59.5 (47–73) | 61 (47–75) | 0.759 |
| 35 (27–43) | 33 (26–42) | 0.080 |
| 74 (53–88) | 74 (58–88) | 0.537 |
| 1.7 (1–2.6) | 1.9 (1–3.2) | 0.002 |
| 1.78 (0.18–4.11) | 1.92 (0.21–4.12) | 0.287 |
| 1.26 (0.1–1.93) | 1.09 (0.34–1.84) | 0.188 |
| 12.4 (9.2–17) | 13.2 (9.28–17) | 0.132 |
| 106.9 (1.1–198.26) | 103.61 (2.6–186.6) | 0.994 |
| Parameters | Patients with Normal fT4 n = 109 | Patients with Low fT4 n = 80 | p-Value |
|---|---|---|---|
| Gender, male | 57 (52.3) | 42 (52.5) | 0.515 |
| Low fT3 (total n = 189) | <0.001 | ||
| 92 (84.4) | 36 (45.0) | |
| 17 (15.6) | 44 (55.0) | |
| Reasons for ICU admission | |||
| 35 (32.1) | 19 (23.8) | 0.209 |
| 32 (29.4) | 30 (37.5) | 0.239 |
| 36 (33.0) | 23 (28.7) | 0.531 |
| 5 (4.6) | 6 (7.5) | 0.532 |
| 1 (0.9) | 1 (1.3) | 1.000 |
| 1 (0.9) | 2 (2.5) | 0.575 |
| Comorbidities | |||
| 65 (59.6) | 38 (47.5) | 0.098 |
| 53 (48.6) | 33 (41.3) | 0.315 |
| 49 (45.0) | 34 (42.5) | 0.737 |
| 6 (5.5) | 5 (6.3) | 1.000 |
| Other clinical variables | |||
| 12 (11.0) | 13 (16.3) | 0.293 |
| 23 (21.1) | 22 (27.5) | 0.307 |
| 11 (10.1) | 25 (31.3) | <0.001 |
| 43 (39.4) | 41 (51.2) | 0.107 |
| 65 (36–86) | 65 (45–79) | 0.986 |
| 53 (48.6) | 32 (40.0) | 0.239 |
| 8 (0–14) | 10.5 (3–17) | <0.001 |
| 18 (15–29) | 19 (15-28) | 0.089 |
| 15 (12–15) | 15 (13–15) | 0.756 |
| 5 (3-9) | 7.5 (3–14) | <0.001 |
| 7 (4–12) | 10 (4–18) | <0.001 |
| Laboratory findings | |||
| 7.19 (7.05–7.33) | 7.19 (7.05–7.33) | 0.975 |
| 59 (47–72) | 61 (47–75) | 0.411 |
| 35 (27–43) | 34 (26–42) | 0.347 |
| 74 (53–88) | 74 (60–88) | 0.379 |
| 1.7 (1–2.7) | 1.9 (1–3.2) | <0.001 |
| 1.78 (0.18–4.12) | 1.89 (0.21–3.9) | 0.936 |
| 1.1 (0.1–1.91) | 1.25 (0.28–1.93) | 0.604 |
| 12.4 (9.2–17) | 12.78 (9.35–17) | 0.507 |
| 90.09 (1.1–195.8) | 120.18 (2.6–198.26) | 0.126 |
| Parameters | HR | 95% CI | p-Value | |
|---|---|---|---|---|
| Lower Limit | Upper Limit | |||
| For the ICU mortality 1 | ||||
| 3.470 | 1.046 | 11.512 | 0.042 |
| 1.117 | 0.996 | 1.251 | 0.058 |
| 22.465 | 5.248 | 96.169 | <0.001 |
| 1.214 | 1.043 | 1.413 | 0.012 |
| For the NIV failure 2 | ||||
| 0.443 | 0.198 | 0.991 | 0.047 |
| 1.715 | 1.462 | 2.011 | <0.001 |
| 1.384 | 1.209 | 1.585 | <0.001 |
| 19.442 | 4.397 | 85.970 | <0.001 |
| 1.008 | 1.000 | 1.016 | 0.056 |
| 1.360 | 1.114 | 1.660 | 0.003 |
| Parameters | AUC | Cut-off | p-Value | Sens. % | Spec. % | PPV % | NPV % |
|---|---|---|---|---|---|---|---|
| For the ICU mortality | |||||||
| 0.631 | ≤1.33 | 0.002 | 53.7 | 71.1 | 23.2 | 90.4 |
| 0.608 | >11.49 | 0.009 | 81.5 | 36.7 | 17.3 | 92.4 |
| 0.518 | ≤2.78 | 0.655 | 90.7 | 20.8 | 15.7 | 93.2 |
| For the NIV failure | |||||||
| 0.630 | <1.77 | <0.001 | 59.6 | 62.0 | 46.0 | 73.8 |
| 0.518 | >12.37 | 0.558 | 57.4 | 50.4 | 38.6 | 68.5 |
| 0.512 | ≤3.13 | 0.701 | 90.4 | 16.8 | 37.2 | 76.4 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Published by MDPI on behalf of the Lithuanian University of Health Sciences. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Elmas, D.; Kizilarslanoglu, M.C. Non-Thyroidal Illness Syndrome: A Predictor of Non-Invasive Ventilation Failure and Mortality in Critically Ill Patients. Medicina 2025, 61, 927. https://doi.org/10.3390/medicina61050927
Elmas D, Kizilarslanoglu MC. Non-Thyroidal Illness Syndrome: A Predictor of Non-Invasive Ventilation Failure and Mortality in Critically Ill Patients. Medicina. 2025; 61(5):927. https://doi.org/10.3390/medicina61050927
Chicago/Turabian StyleElmas, Dursun, and Muhammet Cemal Kizilarslanoglu. 2025. "Non-Thyroidal Illness Syndrome: A Predictor of Non-Invasive Ventilation Failure and Mortality in Critically Ill Patients" Medicina 61, no. 5: 927. https://doi.org/10.3390/medicina61050927
APA StyleElmas, D., & Kizilarslanoglu, M. C. (2025). Non-Thyroidal Illness Syndrome: A Predictor of Non-Invasive Ventilation Failure and Mortality in Critically Ill Patients. Medicina, 61(5), 927. https://doi.org/10.3390/medicina61050927






