The Global Burden of Maxillofacial Trauma in Critical Care: A Narrative Review of Epidemiology, Prevention, Economics, and Outcomes
Abstract
1. Introduction
2. Methods
2.1. Search Strategy
2.2. Selection Criteria
2.3. Data Extraction and Analysis
- Epidemiological patterns (incidence, prevalence, demographic characteristics);
- Etiology and mechanisms of injury;
- Prevention strategies and their effectiveness;
- Economic impact (direct healthcare costs, productivity losses, and rehabilitation expenses);
- Management approaches in critical care settings;
- Short-term and long-term outcomes;
- Complications specific to maxillofacial trauma in critical care.
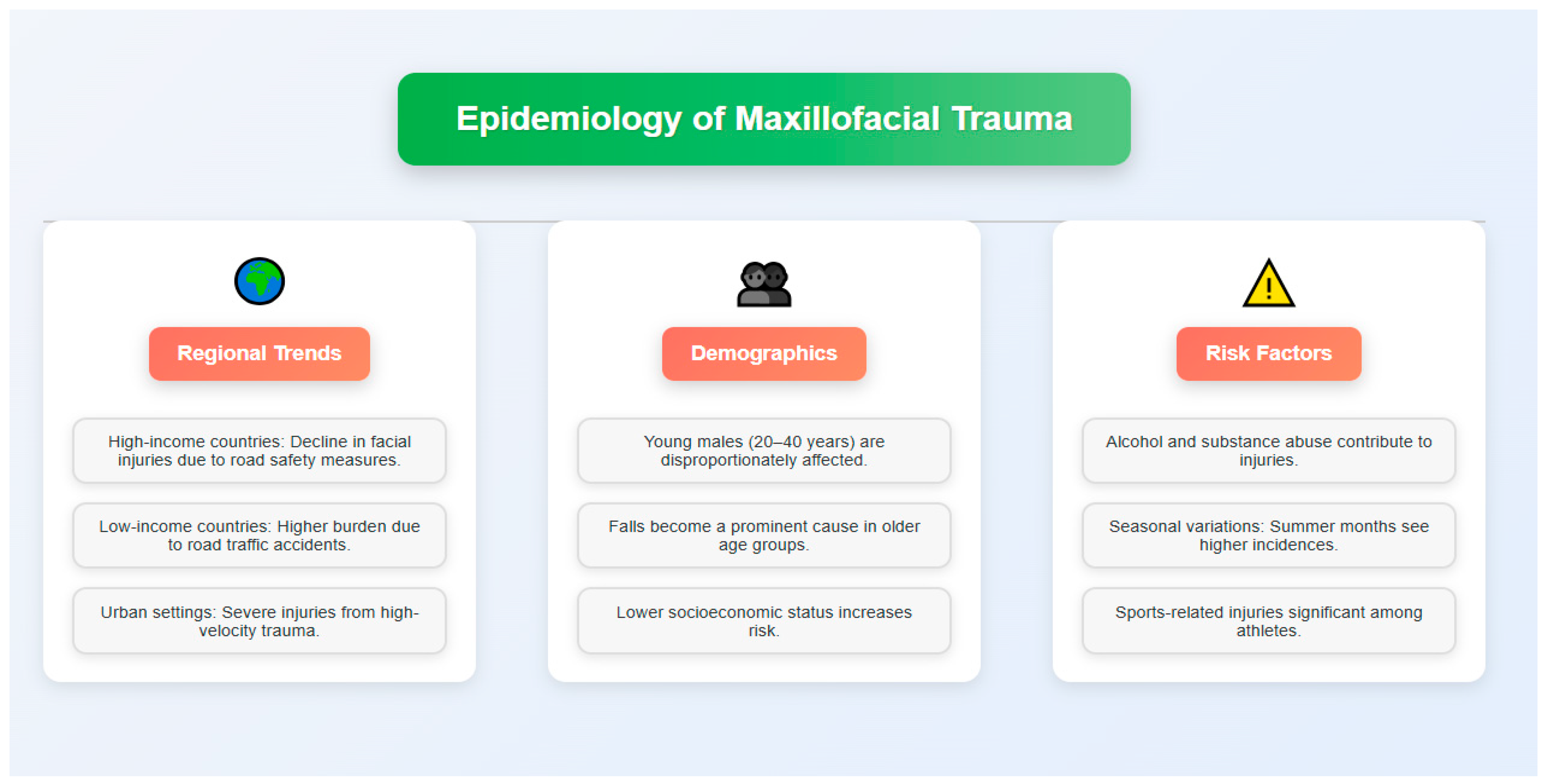
3. Epidemiology
4. Etiology
5. Common Maxillofacial Injuries
5.1. Soft Tissue Injuries
5.2. Facial Bone Fractures
5.3. Dental and Alveolar Injuries
5.4. Associated Injuries
6. Economic Impact
6.1. Healthcare Costs
6.2. Loss of Productivity
6.3. Rehabilitation Expenses
7. Prevention Strategies
7.1. Road Safety Measures
7.2. Violence Prevention Programs
7.3. Occupational Safety Regulations
7.4. Awareness Raising Campaigns
8. Surgical Management
8.1. Timing of Interventions
8.2. Surgical Approaches
8.3. Reconstruction Techniques
9. Complications and Long-Term Outcomes
9.1. Immediate Complications
9.2. Long-Term Functional Disability
9.3. Psychological Impact
10. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Park, H.; Oh, S.; Ra, Y.-S. Worldwide epidemiology of maxillofacial fractures: A systematic review and meta-analysis. J. Craniomaxillofac Surg. 2022, 50, 895–905. [Google Scholar]
- Patil, S.G.; Patil, B.S.; Joshi, U. The Contemporary Management of Maxillofacial Trauma: A Review. J. Maxillofac. Oral. Surg. 2022, 21, 909–925. [Google Scholar]
- Boffano, P.; Roccia, F.; Zavattero, E.; Dediol, E.; Uglešić, V.; Kovačič, Ž.; Vesnaver, A.; Konstantinović, V.S.; Petrović, M.; Stephens, J.; et al. European Maxillofacial Trauma (EURMAT) project: A multicentre and prospective study. J. Craniomaxillofac Surg. 2015, 43, 62–70. [Google Scholar] [CrossRef]
- Singaram, M.; Udhayakumar, R.K. Prevalence, pattern, etiology, and management of maxillofacial trauma in a developing country: A retrospective study. J. Korean Assoc. Oral Maxillofac. Surg. 2016, 42, 174–181. [Google Scholar] [CrossRef]
- Alkhabuli, J.; Alnaqbi, H.; Aisha, A. Etiology and pattern of maxillofacial fractures: A 10-year retrospective analysis of cases in Ras Al-Khaimah, United Arab Emirates. Oral. Health Dent. Manag. 2020, 19, 1–6. [Google Scholar]
- Zargar, M.R.; Khaji, A.; Karbakhsh, M.; Reza Zarei, M. Epidemiology study of facial injuries during a 13 month of trauma registry in Tehran. Indian. J. Med. Sci. 2016, 58, 109–114. [Google Scholar]
- Katsaros, T.; Balasubramanian, S.; Basyuni, S. The epidemiology of facial trauma in major trauma patients. Surgeon 2021, 19, e406–e410. [Google Scholar]
- Tuckett, J.; Lynham, A.; Lee, G.; Perry, M.; Harrington, U. Maxillofacial trauma in the emergency department: A review. Surgeon 2018, 12, 106–114. [Google Scholar] [CrossRef] [PubMed]
- Choi, S.H.; Cha, J.Y.; Kang, D.Y. Precision and accuracy of automated 3D cephalometric landmark identification with CNN-based segmentation method. Sci. Rep. 2021, 11, 17509. [Google Scholar]
- Murphy, C.; Oguz, I.; Shetye, P.R. Machine learning-based prediction of post-trauma facial growth in children with facial fractures. Laryngoscope 2021, 131, E2778–E2785. [Google Scholar]
- Girotto, J.A.; MacKenzie, E.; Fowler, C.; Redett, R.; Robertson, B.; Manson, P.N. Long-term physical impairment and functional outcomes after complex facial fractures. Plast. Reconstr. Surg. 2001, 108, 312–327. [Google Scholar] [CrossRef] [PubMed]
- Kaura, A.; Leitner, L.; Grant, C. Psychological impact of facial trauma: A systematic review. Br. J. Oral. Maxillofac. Surg. 2020, 58, 627–638. [Google Scholar]
- Zaid, M.; Shetty, V.; Glynn, S. Psychosocial factors in trauma recovery: A systematic review. Dent. Traumatol. 2021, 37, 275–290. [Google Scholar]
- Van Boven, G.; Dijkema, T.; Raghoebar, G.M. Global inequality in access to oral and maxillofacial surgical care. Lancet Glob. Health 2023, 11, e693–e700. [Google Scholar]
- World Health Organization. Global Status Report on Road Safety 2023; World Health Organization: Geneva, Switzerland, 2023. [Google Scholar]
- World Health Organization. World Report on Violence and Trauma Prevention; World Health Organization: Geneva, Switzerland, 2019. [Google Scholar]
- Shumrick, K.A.; Campbell, A.C.; Timashpolsky, A. Advances in radiographic evaluation of facial trauma. J. Craniofac Surg. 2018, 29, 2127–2129. [Google Scholar]
- Metzler, P.; Geiger, E.J.; Alcon, A. Three-dimensional virtual surgical planning for patient-specific oromandibular reconstruction using a segmented fibula. J. Craniofac Surg. 2020, 25, 1296–1302. [Google Scholar]
- Ahn, Y.S.; Kim, S.G.; Baik, S.M.; Kim, B.O.; Kim, H.K.; Moon, S.Y. Comparative study between resorbable and nonresorbable plates in orthognathic surgery. J. Oral. Maxillofac. Surg. 2018, 76, 2167–2176. [Google Scholar] [CrossRef]
- Meara, J.G.; Leather, A.J.; Hagander, L.; Alkire, B.C.; Alonso, N.; Ameh, E.A.; Bickler, S.W.; Conteh, L.; Dare, A.J.; Davies, J. Global Surgery 2030: Evidence and solutions for achieving health, welfare, and economic development. Lancet 2015, 386, 569–624. [Google Scholar] [CrossRef]
- Alkire, B.C.; Raykar, N.P.; Shrime, M.G. Global access to surgical care: A modelling study. Lancet Glob. Health 2023, 11, e512–e520. [Google Scholar] [CrossRef]
- Chauhan, V.; Khan, M.A.; Raval, C.B. Telemedicine for maxillofacial trauma triage during the COVID-19 pandemic and beyond: A systematic review. J. Stomatol. Oral. Maxillofac. Surg. 2022, 123, 296–301. [Google Scholar]
- Olsson, P.; Svensson, S.; Johansen, K. A systematic review of the etiology and pattern of maxillofacial fractures in elderly patients. Int. J. Oral. Maxillofac. Surg. 2022, 51, 570–577. [Google Scholar]
- Chrcanovic, B.R. Factors influencing the incidence of maxillofacial fractures. Oral. Maxillofac. Surg. 2012, 16, 3–17. [Google Scholar] [CrossRef]
- Gassner, R.; Tuli, T.; Hächl, O.; Rudisch, A.; Ulmer, H. Cranio-maxillofacial trauma: A 10 year review of 9,543 cases with 21,067 injuries. J. Craniomaxillofac Surg. 2003, 31, 51–61. [Google Scholar] [CrossRef] [PubMed]
- Tamimi, I.; Alabdullah, K.; Alshaalan, H. Interpersonal violence-related facial injuries in Saudi Arabia: A nationwide analysis. J. Craniomaxillofac Surg. 2022, 50, 516–522. [Google Scholar]
- Naddumba, E.K. A cross sectional retrospective study of boda boda injuries at Mulago Hospital in Kampala, Uganda. East. Cent. Afr. J. Surg. 2004, 9, 44–47. [Google Scholar]
- Schnitzer, M.G.; Evangelista, F.C.; dos Santos, B.C. Mandibular fractures: A 10-year retrospective epidemiological study in Brazil. J. Oral. Maxillofac. Surg. Med. Pathol. 2023, 35, 93–97. [Google Scholar]
- Iida, S.; Kogo, M.; Sugiura, T.; Mima, T.; Matsuya, T. Retrospective analysis of 1502 patients with facial fractures. Int. J. Oral. Maxillofac. Surg. 2001, 30, 286–290. [Google Scholar] [CrossRef]
- Lee, K.H. Interpersonal violence and facial fractures. J. Oral. Maxillofac. Surg. 2009, 67, 1878–1883. [Google Scholar] [CrossRef]
- Sane, V.D.; Rathi, S.S.; Kondekar, A. Changing patterns of maxillofacial trauma in India during COVID-19 pandemic: A comparative retrospective study. J. Maxillofac. Oral. Surg. 2022, 21, 263–270. [Google Scholar]
- Erdmann, D.; Follmar, K.E.; Debruijn, M.; Bruno, A.D.; Jung, S.H.; Edelman, D.; Mukundan, S.; Marcus, J.R. A retrospective analysis of facial fracture etiologies. Ann. Plast. Surg. 2008, 60, 398–403. [Google Scholar] [CrossRef]
- Mourouzis, C.; Koumoura, F. Sports-related maxillofacial fractures: A retrospective study of 125 patients. Int. J. Oral. Maxillofac. Surg. 2005, 34, 635–638. [Google Scholar] [CrossRef] [PubMed]
- Ramli, R.; Rahman, N.A.; Rahman, R.A.; Hussaini, H.M.; Hamid, A.L.A. A retrospective study of oral and maxillofacial injuries in Seremban Hospital, Malaysia. Dent. Traumatol. 2011, 27, 122–126. [Google Scholar] [CrossRef] [PubMed]
- Breeze, J.; Gibbons, A.J.; Hunt, N.C.; Monaghan, A.M.; Gibb, I.; Hepper, A. Mandibular fractures in British military personnel secondary to blast trauma sustained in Iraq and Afghanistan. Br. J. Oral. Maxillofac. Surg. 2011, 49, 607–611. [Google Scholar] [CrossRef] [PubMed]
- Salzano, G.; Dell’Aversana Orabona, G.; Audino, G.; Vaira, L.A.; Trevisiol, L.; D’Agostino, A. Have there been any changes in the epidemiology and etiology of maxillofacial trauma during the Italian lockdown for the COVID-19 epidemic? An analysis of 712 injuries received during the pandemic. J. Craniomaxillofac Surg. 2021, 49, 164–170. [Google Scholar]
- Boffano, P.; Kommers, S.C.; Karagozoglu, K.H.; Forouzanfar, T. Aetiology of maxillofacial fractures: A review of published studies during the last 30 years. Br. J. Oral. Maxillofac. Surg. 2014, 52, 901–906. [Google Scholar] [CrossRef]
- Lee, K. Global trends in maxillofacial fractures. Craniomaxillofac Trauma. Reconstr. 2012, 5, 213–222. [Google Scholar] [CrossRef]
- Wong, J.Y.; Choi, A.W.; Fong, D.Y.; Wong, J.K.; Lau, C.L.; Kam, C.W. Patterns, aetiology and risk factors of intimate partner violence-related injuries to head, neck and face in Chinese women. BMC Womens Health 2014, 14, 6. [Google Scholar] [CrossRef]
- Yamamoto, K.; Kuraki, M.; Kurihara, M.; Matsusue, Y.; Murakami, K.; Horita, S.; Sugiura, T.; Kirita, T. Maxillofacial fractures resulting from falls. J. Oral. Maxillofac. Surg. 2010, 68, 1602–1607. [Google Scholar] [CrossRef]
- Lee, K.S.; Lee, J.H.; Kim, S.M. Management of maxillofacial trauma in pediatric patients: A nationwide multicenter study in South Korea. J. Craniofac Surg. 2020, 31, 1412–1415. [Google Scholar]
- Vieira, R.C.A.; de Melo, G.P.; Antunes, A.A.; Dourado, E.; de Barros Silva, P.G. The influence of extreme sports in the prevalence of maxillofacial fractures: A retrospective study of 72 cases. Oral. Maxillofac. Surg. 2014, 18, 397–402. [Google Scholar]
- Roccia, F.; Bianchi, F.; Zavattero, E.; Tanteri, G.; Ramieri, G. Characteristics of maxillofacial trauma in females: A retrospective analysis of 367 patients. J. Craniomaxillofac Surg. 2010, 38, 314–319. [Google Scholar] [CrossRef] [PubMed]
- Breeze, J.; Gibbons, A.J.; Shieff, C.; Banfield, G.; Bryant, D.G.; Midwinter, M.J. Combat-related craniofacial and cervical injuries: A 5-year review from the British military. J. Trauma. Acute Care Surg. 2011, 71, 108–113. [Google Scholar] [CrossRef]
- Ugboko, V.I.; Olasoji, H.O.; Ajike, S.O.; Amole, A.O.D.; Ogundipe, O.T. Facial injuries caused by animals in northern Nigeria. Br. J. Oral. Maxillofac. Surg. 2002, 40, 433–437. [Google Scholar] [CrossRef]
- O’Meara, C.; Witherspoon, R.; Hapangama, N.; Hyam, D.M. Alcohol and interpersonal violence may increase the severity of facial fracture. Br. J. Oral. Maxillofac. Surg. 2012, 50, 36–40. [Google Scholar] [CrossRef] [PubMed]
- Namiri, N.K.; Lui, H.; Tangney, T.; Allen, I.E.; Cohen, A.J.; Breyer, B.N. Electric scooter injuries and hospital admissions in the United States, 2014–2018. JAMA Surg. 2020, 155, 357–359. [Google Scholar] [CrossRef]
- Perry, M.; Holmes, S. Atlas of Operative Maxillofacial Trauma Surgery: Primary Repair of Facial Injuries; Springer: Berlin/Heidelberg, Germany, 2014. [Google Scholar]
- Hollier, L.H.; Sharabi, S.E.; Koshy, J.C.; Stal, S. Facial trauma: General principles of management. J. Craniofac Surg. 2010, 21, 1051–1053. [Google Scholar] [CrossRef] [PubMed]
- Alvi, A.; Doherty, T.; Lewen, G. Facial fractures and concomitant injuries in trauma patients. Laryngoscope 2003, 113, 102–106. [Google Scholar] [CrossRef]
- Biçakci, A.A.; Büyüksoylu, O.; Yilmaz, Y. Current trends in treatment of mandibular condyle fractures: A systematic review and meta-analysis. J. Stomatol. Oral. Maxillofac. Surg. 2022, 123, e348–e357. [Google Scholar]
- Abdelghani, M.; Durand, P.; Nasser, M. Reduction and fixation sequences in panfacial fractures: A systematic review and meta-analysis. J. Craniomaxillofac Surg. 2021, 49, 218–223. [Google Scholar]
- Hwang, K.; You, S.H.; Kim, S.G. Analysis of nasal bone fractures; a six-year study of 503 patients. J. Craniofac Surg. 2007, 18, 87–91. [Google Scholar] [CrossRef]
- Metzinger, S.E.; Guerra, A.B.; Garcia, R.E. Frontal sinus fractures: Management guidelines. Facial Plast. Surg. 2005, 21, 199–206. [Google Scholar] [CrossRef] [PubMed]
- Andreasen, J.O.; Andreasen, F.M.; Andersson, L. Textbook and Color Atlas of Traumatic Injuries to the Teeth; John Wiley & Sons: Hoboken, NJ, USA, 2018. [Google Scholar]
- Andersson, L.; Andreasen, J.O.; Day, P.; Heithersay, G.; Trope, M.; DiAngelis, A.J.; Kenny, D.J.; Sigurdsson, A.; Bourguignon, C.; Flores, M.T.; et al. International Association of Dental Traumatology guidelines for the management of traumatic dental injuries: 2. Avulsion of permanent teeth. Dent. Traumatol. 2012, 28, 88–96. [Google Scholar] [CrossRef]
- Rajandram, R.K.; Syed Omar, S.N.; Rashdi, M.F.N.; Abdul Jabar, M.N. Maxillofacial injuries and traumatic brain injury—A pilot study. Dent. Traumatol. 2014, 30, 128–132. [Google Scholar] [CrossRef] [PubMed]
- Mulligan, R.P.; Friedman, J.A.; Mahabir, R.C. A nationwide review of the associations among cervical spine injuries, head injuries, and facial fractures. J. Trauma. Acute Care Surg. 2010, 68, 587–592. [Google Scholar] [CrossRef] [PubMed]
- Al-Qurainy, I.A.; Stassen, L.F.; Dutton, G.N.; Moos, K.F.; El-Attar, A. The characteristics of midfacial fractures and the association with ocular injury: A prospective study. Br. J. Oral. Maxillofac. Surg. 1991, 29, 291–301. [Google Scholar] [CrossRef]
- Perry, M.; Morris, C. Advanced trauma life support (ATLS) and facial trauma: Can one size fit all? Part 2: ATLS, maxillofacial injuries and airway management dilemmas. Int. J. Oral. Maxillofac. Surg. 2008, 37, 309–320. [Google Scholar] [CrossRef]
- Krug, E.G.; Sharma, G.K.; Lozano, R. The global burden of injuries. Am. J. Public. Health 2000, 90, 523–526. [Google Scholar] [CrossRef]
- Glynn, S.M.; Shetty, V.; Elliot-Brown, K.; Leathers, R.; Belin, T.R.; Wang, J. Chronic posttraumatic stress disorder after facial injury: A 1-year prospective cohort study. J. Trauma. Acute Care Surg. 2007, 62, 410–418. [Google Scholar] [CrossRef]
- Potter, J.K.; Asteriadis, S.; Likavec, M.J. Middle and upper facial fractures: A retrospective review of 234 patients. J. Oral. Maxillofac. Surg. 2005, 63, 790–794. [Google Scholar]
- Levine, E.; Degutis, L.; Pruzinsky, T.; Shin, J.; Persing, J.A. Quality of life and facial trauma: Psychological and body image effects. Ann. Plast. Surg. 2005, 54, 502–510. [Google Scholar] [CrossRef]
- Fonseca, R.J.; Walker, R.V.; Betts, N.J.; Barber, H.D.; Powers, M.P. Oral and Maxillofacial Trauma; Elsevier Health Sciences: Amsterdam, The Netherlands, 2013. [Google Scholar]
- Scherer, M.; Sullivan, W.G.; Smith, D.J.; Phillips, L.G.; Robson, M.C. An analysis of 1423 facial fractures in 788 patients at an urban trauma center. J. Trauma. Acute Care Surg. 1989, 29, 388–390. [Google Scholar] [CrossRef] [PubMed]
- Islam, S.; Ahmed, M.; Walton, G.M.; Dinan, T.G.; Hoffman, G.R. The association between depression and anxiety disorders following facial trauma--a comparative study. Injury 2010, 41, 92–96. [Google Scholar] [CrossRef] [PubMed]
- Brennan, P.A.; Schliephake, H.; Ghali, G.E.; Cascarini, L. Maxillofacial Surgery; Churchill Livingstone: London, UK, 2017. [Google Scholar]
- Peled, M.; Leiser, Y.; Emodi, O.; Krausz, A. Treatment protocol for high velocity/high energy gunshot injuries to the face. Craniomaxillofac Trauma. Reconstr. 2012, 5, 31–40. [Google Scholar] [CrossRef]
- Singleton, M.; Qin, H.; Luan, J. Factors associated with higher levels of injury severity in occupants of motor vehicles that were severely damaged in traffic crashes in Kentucky, 2000–2001. Traffic Inj. Prev. 2004, 5, 144–150. [Google Scholar] [CrossRef]
- Zhu, W.; Zhou, Y.; Jiang, F. The effectiveness of helmet use on reducing motorcycle-related maxillofacial injuries: An updated meta-analysis. Int. J. Environ. Res. Public Health 2021, 18, 5778. [Google Scholar]
- Feng, S.; Li, Z.; Du, Y. Urban traffic engineering interventions to reduce road traffic injuries: A systematic review and meta-analysis. Lancet Planet. Health 2022, 6, e688–e698. [Google Scholar]
- Allareddy, V.; Allareddy, V.; Nalliah, R.P. Epidemiology of facial fracture injuries. J. Oral Maxillofac. Surg. 2011, 69, 2613–2618. [Google Scholar] [CrossRef]
- Deng, H.; Yang, Z.; Li, J. Applications of 3D printing technology in the COVID-19 response: A literature review. Front. Med. 2021, 8, 648771. [Google Scholar]
- Florence, C.; Shepherd, J.; Brennan, I.; Simon, T. Effectiveness of anonymised information sharing and use in health service, police, and local government partnership for preventing violence related injury: Experimental study and time series analysis. BMJ 2011, 342, d3313. [Google Scholar] [CrossRef]
- Krug, E.G.; Mercy, J.A.; Dahlberg, L.L.; Zwi, A.B. The world report on violence and health. Lancet 2002, 360, 1083–1088. [Google Scholar] [CrossRef]
- Campbell, J.C. Health consequences of intimate partner violence. Lancet 2002, 359, 1331–1336. [Google Scholar] [CrossRef] [PubMed]
- Lipscomb, H.J. Effectiveness of interventions to prevent work-related eye injuries. Am. J. Prev. Med. 2000, 18, 27–32. [Google Scholar] [CrossRef] [PubMed]
- Lombardi, D.A.; Verma, S.K.; Brennan, M.J.; Perry, M.J. Factors influencing worker use of personal protective eyewear. Accid. Anal. Prev. 2009, 41, 755–762. [Google Scholar] [CrossRef]
- Newsome, P.R.; Tran, D.C.; Cooke, M.S. The role of the mouthguard in the prevention of sports-related dental injuries: A review. Int. J. Paediatr. Dent. 2001, 11, 396–404. [Google Scholar] [CrossRef]
- Wakefield, M.A.; Loken, B.; Hornik, R.C. Use of mass media campaigns to change health behaviour. Lancet 2010, 376, 1261–1271. [Google Scholar] [CrossRef]
- Finch, C.F.; Donaldson, A. A sports setting matrix for understanding the implementation context for community sport. Br. J. Sports Med. 2010, 44, 973–978. [Google Scholar] [CrossRef]
- Durbin, D.R.; Chen, I.; Smith, R.; Elliott, M.R.; Winston, F.K. Effects of seating position and appropriate restraint use on the risk of injury to children in motor vehicle crashes. Pediatrics 2005, 115, e305–e309. [Google Scholar] [CrossRef] [PubMed]
- Ellis, E. Timing of definitive management of facial fractures. J. Oral Maxillofac. Surg. 2019, 77, 1153–1162. [Google Scholar]
- Manson, P.N.; Clark, N.; Robertson, B.; Slezak, S.; Wheatly, M.; Vander Kolk, C.; Ilif, N. Subunit principles in midface fractures: The importance of sagittal buttresses, soft-tissue reductions, and sequencing treatment of segmental fractures. Plast. Reconstr. Surg. 1999, 103, 1287–1306. [Google Scholar] [CrossRef]
- Chrcanovic, B.R. Open versus closed reduction: Comminuted mandibular fractures. Oral Maxillofac. Surg. 2012, 16, 153–162. [Google Scholar] [CrossRef]
- Wei, H.; Liu, Y.; Gao, Y. Management of mandibular condylar fractures using intraoral approach: A retrospective analysis of 356 cases. Int. J. Oral Maxillofac. Surg. 2020, 49, 1533–1539. [Google Scholar]
- Tan, Y.; Chen, X.; Hu, J. Endoscopic-assisted management of mandibular condylar fractures: A 10-year review of surgical outcomes. J. Craniomaxillofac Surg. 2021, 49, 726–732. [Google Scholar]
- Salgarelli, A.C.; Bellini, P.; Landini, B.; Multinu, A.; Consolo, U. A comparative study of different approaches in the treatment of orbital trauma: An experience based on 274 cases. Oral. Maxillofac. Surg. 2010, 14, 23–27. [Google Scholar] [CrossRef]
- Khadembaschi, D.; Smeets, R.; Jung, S. Biodegradable versus titanium osteosynthesis materials for internal fixation of maxillofacial fractures: A systematic review. Int. J. Oral Maxillofac. Surg. 2023, 52, 520–528. [Google Scholar]
- Gander, T.; Essig, H.; Metzler, P.; Lindhorst, D.; Dubois, L.; Rücker, M.; Schumann, P. Patient specific implants (PSI) in reconstruction of orbital floor and wall fractures. J. Craniomaxillofac Surg. 2015, 43, 126–130. [Google Scholar] [CrossRef] [PubMed]
- García-Mato, D.; Ochandiano, S.; García-Sevilla, M. Advances in intraoperative navigation and real-time validation in craniomaxillofacial surgery: A systematic review. J. Clin. Med. 2021, 10, 1315. [Google Scholar]
- Pu, L.L.Q.; Coleman, S.R.; Cui, X. Autologous fat grafting in the face: Technical considerations and management of complications. J. Craniofac Surg. 2022, 33, 76–84. [Google Scholar]
- Coleman, S.R. Structural fat grafting: More than a permanent filler. Plast. Reconstr. Surg. 2006, 118, 108S–120S. [Google Scholar] [CrossRef]
- Markowitz, B.L.; Manson, P.N. Panfacial fractures: Organization of treatment. Clin. Plast. Surg. 1989, 16, 105–114. [Google Scholar] [CrossRef]
- Sosin, M.; Ceradini, D.J.; Levine, J.P.; Hazen, A.; Staffenberg, D.A.; Saadeh, P.; Flores, R.; Sweeney, N.; Bernstein, G.; Leslie, M. Total face, eyelids, ears, scalp, and skeletal subunit transplant: A reconstructive solution for the full face and total scalp burn. Plast. Reconstr. Surg. 2016, 138, 205–219. [Google Scholar] [CrossRef]
- Mendez, B.M.; Chiodo, M.V.; Patel, P.A. Customized “in-office” three-dimensional printing for virtual surgical planning in craniofacial surgery. J. Craniofac. Surg. 2015, 26, 1584–1586. [Google Scholar] [CrossRef]
- Ma, J.; Both, S.K.; Yang, F.; Cui, F.-Z.; Pan, J.; Meijer, G.J.; Jansen, J.A.; van den Beucken, J.J.J.P. Concise review: Cell-based strategies in bone tissue engineering and regenerative medicine. Stem Cells Transl. Med. 2014, 3, 98–107. [Google Scholar] [CrossRef]
- Andreasen, J.O.; Jensen, S.S.; Schwartz, O.; Hillerup, Y. A systematic review of prophylactic antibiotics in the surgical treatment of maxillofacial fractures. J. Oral. Maxillofac. Surg. 2006, 64, 1664–1668. [Google Scholar] [CrossRef]
- Cogbill, T.H.; Cothren, C.C.; Ahearn, M.K.; Cullinane, D.C.; Kaups, K.L.; Scalea, T.M.; Maggio, L.; Brasel, K.J.; Harrison, P.B.; Patel, N.Y. Management of maxillofacial injuries with severe oronasal hemorrhage: A multicenter perspective. J. Trauma. Acute Care Surg. 2008, 65, 994–999. [Google Scholar] [CrossRef] [PubMed]
- Bouloux, G.F.; Perciaccante, V.J. Massive hemorrhage during oral and maxillofacial surgery: Ligation of the external carotid artery or embolization? J. Oral. Maxillofac. Surg. 2004, 62, 1199–1200. [Google Scholar] [CrossRef]
- Ulug, T.; Ulubil, S.A. Management of facial paralysis in temporal bone fractures: A prospective study analyzing 11 operated fractures. Am. J. Otolaryngol. 2005, 26, 230–238. [Google Scholar] [CrossRef]
- Christensen, J.; Sawatari, Y.; Peleg, M. High-energy traumatic maxillofacial injury. J. Craniofac. Surg. 2015, 26, 1487–1491. [Google Scholar] [CrossRef]
- Al-Moraissi, E.A.; Ellis, E. What method for management of unilateral mandibular angle fractures has the lowest rate of postoperative complications? A systematic review and meta-analysis. J. Oral Maxillofac. Surg. 2014, 72, 2197–2211. [Google Scholar] [CrossRef]
- Kunz, C.; Sigron, G.R.; Jaquiéry, C. Functional outcome after non-surgical management of orbital fractures--the bias of decision-making according to size of defect: Critical review of 48 patients. Br. J. Oral Maxillofac. Surg. 2013, 51, 486–492. [Google Scholar] [CrossRef]
- Mondin, V.; Rinaldo, A.; Ferlito, A. Management of nasal bone fractures. Am. J. Otolaryngol. 2005, 26, 181–185. [Google Scholar] [CrossRef]
- Conforte, J.J.; Alves, C.P.; Sánchez, M.D.P.; Ponzoni, D. Impact of trauma and surgical treatment on quality of life of patients with facial fractures. Int. J. Oral Maxillofac. Surg. 2016, 25, 254–257. [Google Scholar] [CrossRef] [PubMed]
- Vishwanath, K.; Prasad, R.; Thakur, D. Psychological impact of facial trauma: A multicenter cross-sectional study. Craniomaxillofac Trauma. Reconstr. 2020, 13, 310–317. [Google Scholar]
- De Sousa, A. Psychological issues in acquired facial trauma. Indian. J. Plast. Surg. 2008, 41, 183–193. [Google Scholar] [CrossRef] [PubMed]

| Economic Factor | Description | Key Findings | Implementation Challenges | Affected Groups | References |
|---|---|---|---|---|---|
| Direct Healthcare Costs | Immediate medical expenses for treatment of facial injuries | Mean hospital charges of USD 55,385 per admission; annual cost of USD 1.06 billion in the US | High variability in costs across regions and facilities | Patients, hospitals, insurance providers | [45] |
| Surgical Intervention Costs | Costs for surgical procedures, including reconstruction and fixation | Severe cases may cost up to USD 200,000 per patient | Limited access to advanced surgical facilities in low-income regions | Patients with severe injuries | [61,62,63,64] |
| Imaging and Diagnostic Costs | Expenses for CT, MRI, and other imaging required for diagnosis and surgical planning | Imaging is essential but significantly contributes to overall costs | Limited availability of CT/MRI in resource-poor settings | Trauma patients, healthcare facilities | [63] |
| Long-term Follow-up Costs | Expenses for follow-up visits and secondary procedures | Recovery often requires multiple follow-ups, adding to cumulative healthcare expenditure | Compliance with follow-up care can be challenging | Patients requiring ongoing care | [64] |
| Loss of Productivity | Time away from work or school due to hospitalization and recovery | An average of 11.8 days lost per incident; substantial economic loss in affected regions | Long recovery periods or permanent disability | Workers, employers, families | [65] |
| Long-term Employment Impact | Effects on career progression and earning capacity | Up to 30% of severely injured patients face long-term unemployment or underemployment | Limited opportunities for rehabilitation and retraining | Low-income workers, severely injured | [66] |
| Rehabilitation Expenses | Costs for therapies (physical, speech, psychological), prosthetics, and long-term care | Patients require an average of 22 therapy sessions over six months, costing ~USD 3800 per patient | Access to therapy facilities and affordability issues | Trauma patients, rehab centers | [67,68] |
| Dental Rehabilitation Costs | Costs for dental implants, prosthetics, and restorations | Average cost of USD 18,000 per patient; complex cases can exceed USD 50,000 | Insurance may not cover dental implants; affordability for patients | Patients with dental injuries | [69] |
| Psychological Treatment Costs | Mental health care costs for PTSD, depression, and anxiety associated with disfigurement | Often underestimated but essential for long-term recovery | Stigma around mental health; availability of specialized care | Patients, mental health providers | [70,71] |
| Impact on Uninsured Patients | Financial burden on individuals without insurance coverage | 22.4% of patients with facial fractures are uninsured, leading to increased out-of-pocket expenses | Limited access to affordable care options | Uninsured and underinsured populations | [72] |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Published by MDPI on behalf of the Lithuanian University of Health Sciences. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Maniaci, A.; Lentini, M.; Vaira, L.; Lavalle, S.; Ronsivalle, S.; Rubulotta, F.M.; Lentini, L.; Paternò, D.S.; Galletti, C.; Sorbello, M.; et al. The Global Burden of Maxillofacial Trauma in Critical Care: A Narrative Review of Epidemiology, Prevention, Economics, and Outcomes. Medicina 2025, 61, 915. https://doi.org/10.3390/medicina61050915
Maniaci A, Lentini M, Vaira L, Lavalle S, Ronsivalle S, Rubulotta FM, Lentini L, Paternò DS, Galletti C, Sorbello M, et al. The Global Burden of Maxillofacial Trauma in Critical Care: A Narrative Review of Epidemiology, Prevention, Economics, and Outcomes. Medicina. 2025; 61(5):915. https://doi.org/10.3390/medicina61050915
Chicago/Turabian StyleManiaci, Antonino, Mario Lentini, Luigi Vaira, Salvatore Lavalle, Salvatore Ronsivalle, Francesca Maria Rubulotta, Lepanto Lentini, Daniele Salvatore Paternò, Cosimo Galletti, Massimiliano Sorbello, and et al. 2025. "The Global Burden of Maxillofacial Trauma in Critical Care: A Narrative Review of Epidemiology, Prevention, Economics, and Outcomes" Medicina 61, no. 5: 915. https://doi.org/10.3390/medicina61050915
APA StyleManiaci, A., Lentini, M., Vaira, L., Lavalle, S., Ronsivalle, S., Rubulotta, F. M., Lentini, L., Paternò, D. S., Galletti, C., Sorbello, M., Lechien, J. R., & La Via, L. (2025). The Global Burden of Maxillofacial Trauma in Critical Care: A Narrative Review of Epidemiology, Prevention, Economics, and Outcomes. Medicina, 61(5), 915. https://doi.org/10.3390/medicina61050915














