Abstract
Background and Objectives: Central sensitization (CS) has been identified as a significant factor influencing persistent pain and dissatisfaction following total knee arthroplasty (TKA). However, its effect on unicompartmental knee arthroplasty (UKA) remains largely unexplored. Unlike TKA, UKA preserves most native knee structures, with less bone cut, leading to different postoperative pain mechanisms. Nevertheless, the revision rate for unexplained pain following UKA is higher than after TKA. This study investigates the influence of preoperative CS on pain and dissatisfaction after UKA. Materials and Methods: This retrospective cohort study included 121 patients who underwent primary UKA for medial compartment osteoarthritis of the knee. Patients were screened for CS preoperatively using the Central Sensitization Inventory (CSI) and categorized into a CS group (CSI ≥ 40; n = 26) and a non-CS group (CSI < 40; n = 95). Clinical outcomes, including the Western Ontario and McMaster Universities Osteoarthritis Index (WOMAC), Forgotten Joint Score (FJS), and patient satisfaction, were assessed at the 2-year postoperative follow-up visit. A multivariate regression analysis was used to determine the risk factors for postoperative dissatisfaction. Results: The CS group reported significantly worse postoperative WOMAC pain, function, and total scores than the non-CS group (all p < 0.05). FJS was also significantly worse in the CS group than in the non-CS group (64.4 vs. 72.7, respectively, p = 0.005). Patient satisfaction was significantly lower in the CS group than in the non-CS group (65.4% vs. 95.8%, respectively, p < 0.001). The multivariate logistic regression analysis demonstrated that patients with a CSI score ≥ 40 had an 11.349-fold increased likelihood of dissatisfaction after UKA (95% CI: 2.315–55.626, p = 0.003). Conclusions: This study underscores the importance of recognizing CS as a critical determinant of postoperative pain and functional recovery following UKA. Patients with high CSI scores experience greater pain, increased joint awareness, and overall poorer satisfaction despite technically successful surgeries.
1. Introduction
Unicompartmental knee arthroplasty (UKA) is a well-established surgical procedure for treating unicompartmental osteoarthritis (OA), offering a less invasive alternative to total knee arthroplasty (TKA) with generally favorable outcomes [1,2,3,4]. However, a certain proportion of UKA patients experience persistent postoperative pain and discomfort, even in the absence of clear radiographic abnormalities or mechanical complications [5,6,7]. Among all revision cases, the proportion of revisions performed due to unexplained pain was higher after UKA (23%) than TKA (9%), raising concerns about factors influencing postoperative pain perception [5].
Persistent postoperative pain after knee arthroplasty has traditionally been attributed to peripheral mechanisms such as residual inflammation, tissue damage, or prosthetic malalignment, which activate peripheral nociceptors and lead to peripheral sensitization [8,9]. However, recent evidence suggests that in many chronic pain cases, particularly without clear anatomical abnormalities, central sensitization (CS) may play a key role. CS is a maladaptive response of the central nervous system marked by heightened pain sensitivity, reduced inhibitory control, and glial activation, often leading to allodynia and hyperalgesia [9,10]. This central amplification of pain signals—also referred to as “centralized pain,” “central augmentation,” or “pain hypersensitivity”—can persist long after the initial surgical insult has resolved [9,10]. In such cases, the brain and spinal cord essentially ‘turn up the volume’ of pain processing, independent of ongoing peripheral input [9,10]. This phenomenon helps explain why some patients report severe pain after knee arthroplasty despite good surgical outcomes and the absence of detectable complications [9,10].
Recent research has explored the role of CS in persistent pain following joint arthroplasty [8,9,10]. CS is a condition characterized by an exaggerated pain response due to alterations in central nervous system processing [8,9,10]. It is mediated by neurotransmitters such as serotonin and norepinephrine and leads to increased sensitivity to pain stimuli, lowered pain thresholds, and prolonged pain perception even after the initial source of pain has been resolved [8,9,10]. Patients with CS often report widespread pain, hyperalgesia, and allodynia, which can significantly affect their recovery following orthopedic procedures [8,9,10].
Previous studies have established a link between CS and poor outcomes following TKA [11,12,13,14,15,16]. Patients with high preoperative pain levels and low pain thresholds are more likely than others to experience severe postoperative pain and dissatisfaction, despite successful surgical intervention [11,12,13,14,15,16]. However, the role of CS in UKA remains relatively underexplored. Given that UKA is a less invasive procedure that preserves the surrounding soft tissues, it might be assumed that patients would experience less postoperative pain than TKA patients [3]. Persistent pain in a subset of UKA patients suggests that factors beyond structural abnormalities could be contributing to suboptimal outcomes [7].
Understanding the association between CS and postoperative pain in UKA patients is crucial for improving patient outcomes. Identifying patients with preoperative CS could allow for the implementation of targeted perioperative strategies to mitigate its effects. The purpose of this study was to investigate whether preoperative CS is associated with worse postoperative outcomes, including pain, function, and satisfaction, in patients undergoing UKA. We hypothesized that patients with preoperative CS would report inferior clinical outcomes and lower satisfaction following UKA compared to those without CS.
2. Materials and Methods
2.1. Study Design
This study used a retrospective cohort design to evaluate the effects of CS on postoperative outcomes following UKA. The study was conducted at a single tertiary medical center, and all procedures were performed by a single experienced orthopedic surgeon to minimize variability in surgical technique. Ethical approval for this study was obtained from the institutional review board, and informed consent was obtained from all patients prior to participation.
2.2. Patient Selection
Data from 131 patients who underwent unilateral UKA between 2014 and 2022 were initially included in the study. The inclusion criteria were as follows: (1) isolated medial compartment OA with an intact anterior cruciate ligament, (2) correctable varus deformity (less than 10 degrees), (3) minimum two-year follow-up period, and (4) no history of prior knee surgery on the affected side. Patients were excluded if they had: inflammatory arthritis (e.g., rheumatoid arthritis), osteonecrosis affecting the knee joint (1 patient), post-traumatic OA (1 patient), a history of knee infection, a documented history of CS-related conditions such as irritable bowel syndrome (1 patient) and chronic low back pain (2 patients), prior use of centrally acting agents or patients with diagnosed psychiatric conditions known to affect CS, such as anxiety or depressive disorders (2 patients), incomplete clinical outcome data (2 patients), or a subsequent operation on either knee during the follow-up period (1 patient). All patients were clinically screened for signs of peripheral neuropathy, including diabetic neuropathy, through neurologic examination and medical history review. Patients with confirmed or suspected peripheral neuropathy were excluded from the study. Notably, none of the enrolled participants exhibited clinical evidence of peripheral neuropathy. Following the application of those criteria, 10 patients were excluded from the study, resulting in a final cohort of 121 patients (Figure 1). All analyses were limited to patients who met the criteria for medial UKA, stratified by CS status. Patient demographics and baseline characteristics, including body mass index (BMI), comorbidities, and preoperative functional status, were collected through medical records and patient-reported questionnaires.
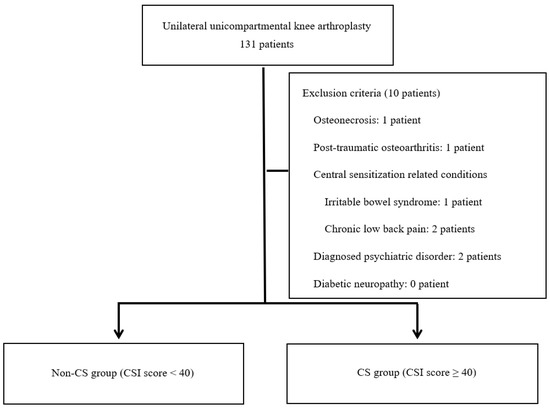
Figure 1.
Participant flow diagram. CS: Central Sensitization, CSI: Central Sensitization Inventory.
CS is influenced by both non-modifiable factors, such as female sex [17] and genetic predisposition [18], and modifiable factors, including poor sleep, psychological distress, and CS-related conditions like restless leg syndrome or chronic fatigue syndrome [19,20]. To minimize confounding, we excluded patients with major psychiatric disorders, pain catastrophizing tendencies, or clinical features of CS-related diseases through thorough medical record reviews and preoperative interviews. This approach aimed to enhance the specificity of our findings on the impact of CS [19,20].
2.3. Assessment of Central Sensitization
The Central Sensitization Inventory (CSI) is commonly used to assess CS and offers significant practical benefits in clinical settings [17,18]. The CSI is a validated self-reported questionnaire designed to evaluate symptoms associated with CS. Unlike quantitative sensory testing (QST), which objectively measures sensory responses to external stimuli, the CSI focuses on subjective symptom assessment [17,18].
The CSI questionnaire consists of 25 items that capture a broad spectrum of somatic and emotional symptoms frequently observed in individuals with CS [17,18]. These include headaches, fatigue, sleep disturbances, cognitive difficulties, and psychological distress, as well as heightened pain sensitivity that can interfere with daily life. The CSI specifically evaluates the presence of unrefreshing sleep, muscle stiffness and pain, anxiety attacks, bruxism, gastrointestinal disturbances (diarrhea/constipation), difficulty daily activities, light sensitivity, physical fatigue, widespread pain, urinary discomfort, poor sleep quality, concentration issues, skin problems, stress-related physical symptoms, depression, low energy, muscle tension in the neck and shoulders, jaw pain, dizziness or nausea triggered by certain smells, frequent urination, restless legs, memory impairment, childhood trauma, and pelvic pain [17,18].
Each item is rated on a 5-point Likert scale ranging from 0 (never) to 4 (always), with a total possible score of 0 to 100. According to Neblett et al. [18], a score of 40 or higher suggests the presence of CS. The CSI is easy to administer, takes less than 10 min to complete, and does not require specialized equipment. Additionally, because it incorporates non-painful and hypothetical scenarios, it avoids ethical concerns associated with other assessment methods. These advantages make the CSI a highly useful tool for evaluating the severity of CS-related symptoms. It is widely recognized as a reliable and validated measure for quantifying CS symptom severity [17,18] (Supplementary Figure S1).
2.4. Surgical Procedure and Postoperative Management
All UKA procedures were performed by a single surgeon using a standardized minimally invasive approach. The same cemented, mobile-bearing (MB) UKA system (Microplasty Oxford MB UKA, Zimmer Biomet, Warsaw, IN, USA) was used in all cases to ensure consistency across patients. All operations were performed under general anesthesia through the mini-medial parapatellar approach. A pneumatic tourniquet that inflated to 300 mmHg was applied. The medial meniscus was resected, and the osteophytes of the medial femoral condyle and tibial plateau were carefully removed. With the Microplasty Oxford MB UKA system, the femoral gap-sizing spoons and G-clamp were used to assess the femoral component size, tibial cutting depth, and orientation. After determining the size of the medial femoral condyle and evaluating the gap between the femur and tibia using a series of femoral sizing spoons, the most suitable spoon was selected and positioned on the MFC. After securing the gap-sizing spoon to the tibial resection guide with the G-clamp, the guide was aligned parallel to the long axis of the tibia in both the coronal and sagittal planes. The tibia was then resected, and an intramedullary rod with a distal linking feature was inserted into the femoral canal until fully seated. With the IM link engaged, the femoral drill guide was positioned on the tibial cut surface to determine the femoral component position. A posterior femoral condylar cut was performed along the femoral cutting guide. Subsequently, distal femoral milling was carefully performed to balance the flexion and extension gaps without ligament release. Cement fixation was used for all femoral and tibial components. A compressive bandage was applied postoperatively. Patients were allowed full weight-bearing on postoperative day 1 with the assistance of a walker, and a structured physical therapy program was initiated to optimize range of motion and quadriceps strengthening. The same preemptive multimodal analgesic regimen was applied to all patients. Postoperatively, intravenous patient-controlled analgesia, programmed to deliver 1 mL of a 100-mL solution containing 2000 μg of fentanyl, was used. Once the patients restarted oral intake, they received 10 mg of oxycodone every 12 h for one week, along with 200 mg of celecoxib, 37.5 mg of tramadol, and 650 mg of acetaminophen every 12 h for six weeks. Subsequent visits were scheduled at two weeks, six weeks, three months, six months, and one year, with yearly visits thereafter.
2.5. Outcome Measures
Postoperative outcomes were assessed at baseline and two years using validated patient-reported outcome measures (PROMs). Pain, stiffness, and function were evaluated using the Western Ontario and McMaster Universities Osteoarthritis Index (WOMAC), a well-established tool for assessing clinically relevant outcomes in patients undergoing treatment for OA of the hip or knee [19]. Additionally, joint awareness during daily activities was measured using the Forgotten Joint Score (FJS), which has been validated as a key indicator of successful joint arthroplasty [20]. To assess patient satisfaction, the new Knee Society Satisfaction (KSS) score, a five-item questionnaire designed to evaluate satisfaction with daily activities, was used. Patients were categorized as satisfied (total score 21–40) or dissatisfied (0–20), following the scoring system developed by Noble et al. [21] In addition to PROMs, postoperative complications—infection, implant loosening, and the need for revision surgery—were systematically recorded to provide a comprehensive evaluation of surgical outcomes.
3. Statistical Analysis
All data are presented as the mean and standard deviation. Data were compared between the non-CS group (preoperative CSI score < 40) and the CS group (preoperative CSI score ≥ 40). Continuous variables were analyzed using independent t-tests, and categorical variables were compared using chi-square tests. Patient demographics and surgical characteristics were collected as dependent variables to identify risk factors for patient dissatisfaction. A multivariable logistic regression analysis was conducted to evaluate associated factors, using a backward elimination approach to retain significant predictors of postoperative dissatisfaction following UKA. Odds ratios were calculated with 95% confidence intervals (CIs). Statistical analysis was performed using SPSS® for Windows v21.0, with p < 0.05 indicating statistical significance.
4. Results
The final cohort comprised 121 patients who underwent UKA and met the inclusion criteria. Participants included individuals aged 42 to 82 years who met the inclusion criteria for UKA. Patients were stratified into two groups based on their preoperative CSI scores: 95 patients (78.5%) had CSI scores below 40 (non-CS group), and 26 patients (21.5%) had CSI scores of 40 or higher (CS group). The two groups did not differ significantly in demographic characteristics or surgical factors, except for CSI scores (Table 1).

Table 1.
Comparison of demographic characteristics and surgical factors in the central sensitization and non–central sensitization groups.
Preoperative WOMAC subscores differed significantly between the groups (p < 0.05). Before surgery, WOMAC pain, function, and total scores were significantly worse in the CS group than in the non-CS group, indicating worse baseline symptoms (all p < 0.05).
In both groups, all WOMAC subscores (pain, function, and total scores) showed significant improvements postoperatively, compared with the preoperative values (all p < 0.05) (Table 2). However, the mean postoperative WOMAC pain score was still higher in the CS group than the non-CS group (7.8 vs. 1.8, respectively, p < 0.001) 2 years postoperatively. Similarly, the postoperative total WOMAC score was significantly higher in the CS group than in the non-CS group (30.5 vs. 12.8, respectively, p < 0.001). The improvement in preoperative to postoperative WOMAC subscores (pain, function, and total) was significantly greater in the non-CS group than in the CS group (all p < 0.05) (Table 2).

Table 2.
Preoperative and postoperative patient-reported outcomes.
The FJS, which evaluates joint awareness during daily activities, was significantly lower in the CS group than in the non-CS group (64.4 vs. 72.7, respectively, p = 0.005). This finding suggests that patients with CS were more likely than those without CS to be aware of their knee joint postoperatively (Table 3).

Table 3.
Postoperative Forgotten Joint Score (FJS) results.
The new KSS score was 33.1 in the non-CS group and 25.5 in the CS group (p < 0.001). Among non-CS group patients, 91 (95.8%) were satisfied with their UKAs, whereas only 17 (65.4%) patients in the CS group reported satisfaction with the surgery (p < 0.001). Satisfaction in the CS group was, thus, significantly lower than in the non-CS group, not only for light daily activities such as sitting, lying in bed, and getting out of bed, but also for physically demanding tasks such as household chores and recreational or leisure activities (all p < 0.05) (Table 4).

Table 4.
Comparison of satisfaction scores and proportions.
The multivariate logistic regression analysis demonstrated that patients with a CSI score ≥ 40 had a 6.526-fold increased likelihood of dissatisfaction after UKA (95% CI: 2.298–18.531, p < 0.001), compared with patients with a CSI score < 40. The associations remained statistically significant after adjusting for age, gender, BMI, American Society of Anesthesiologists grade, preoperative flexion contracture and further flexion, preoperative hip/knee/ankle angle, and preoperative WOMAC total scores (Table 5). No patient in either group experienced complications requiring additional surgery or revision during the follow-up period.

Table 5.
Results of multivariate analysis of risk factors predicting dissatisfaction.
To assess whether the sample size was sufficient to detect the observed difference in satisfaction between the groups, we conducted a post-hoc power analysis using the observed satisfaction rates (95.8% in the non-CS group vs. 65.4% in the CS group). Based on a two-sided α of 0.05 and group sizes of 92 and 26, the power to detect a statistically significant difference was calculated to be 95.7% using a two-proportion z-test. This suggests that despite the unequal group sizes, the study was adequately powered to detect the observed effect.
5. Discussion
The findings of this study highlight the significant role that CS plays in postoperative pain and dissatisfaction following UKA. Patients with preoperative CS, identified as a CSI score of 40 or higher, demonstrated significantly worse postoperative pain scores, increased joint awareness, and inferior functional outcomes compared with those without CS. These results provide valuable insights into the influence of preoperative pain processing mechanisms on surgical recovery and patient satisfaction.
Several tools are available to assess CS, including QST and advanced imaging modalities such as functional magnetic resonance imaging (fMRI). QST objectively measures pain and sensory thresholds to external stimuli at local or remote sites, and has been widely used to detect abnormal pain processing suggestive of CS [21,22]. fMRI has also provided insights into altered brain structure and neurochemical activity in CS, such as decreased cortical thickness and elevated glutamate levels [23,24]. In this study, we chose to use the CSI, a validated self-reported questionnaire specifically designed to identify symptoms associated with CS [13,19,20,25,26]. While CSI is a self-reported measure and inherently subject to potential response bias, it offers several advantages that help mitigate these concerns. First, the CSI has been shown to have high internal consistency and reliability, and a cutoff score of 40 has been validated to identify patients with clinically significant central sensitization [19,20,25]. It is composed of items that assess not only pain but also other non-painful characteristic symptoms of CS, such as fatigue, poor sleep, and concentration difficulties, reducing the likelihood of misclassification due to isolated pain complaints [13,19,20,25,26]. Second, to minimize confounding factors, we excluded patients with known CS-related conditions (e.g., fibromyalgia, irritable bowel syndrome) and psychiatric disorders, both of which are known to influence CSI scores [19,20,25]. This allowed for a more specific assessment of CS-related symptoms within the context of knee OA [19,20,25]. Finally, although objective methods such as QST can provide valuable information about the sensory nervous system and local/distant hyperalgesia, they require specialized equipment and training, and are not always feasible in a retrospective design [19,20,25]. The CSI, in contrast, is efficient (<10 min), easy to administer, and ethically unproblematic, making it an appropriate tool for screening CS in clinical populations when used with appropriate exclusion criteria [13,19,20,25,26]. Given these benefits and considering the retrospective nature of our study, CSI provided an efficient and robust tool to stratify patients based on their CS status [19,20,25].
Patients with preoperative CS experienced significantly worse postoperative pain and functional outcomes than those without CS, despite the theoretical advantages of UKA over TKA, such as a smaller incision, preservation of most soft tissues, and less bone resection [3]. Our findings reveal that the CS group reported notably higher pain scores two years postoperatively. No previous studies investigated the effects of preoperative CS on UKA outcomes. However, numerous studies have examined the relationship between preoperative CS and clinical outcomes following TKA [11,12,13,14,15,16,27,28], and the evidence suggests that patients with preoperative CS are at greater risk than those without CS for chronic postoperative pain [11,12,13,14,15,16,27,28]. Martinez et al. [28] found that TKA patients with heat hyperalgesia reported greater pain both before and after surgery and required higher doses of postoperative morphine. Similarly, Lundblad et al. [27] followed 69 patients for 18 months after TKA and noted that persistent pain was more prevalent among those with high preoperative pain levels and a lower pain threshold—both indicative of CS-related mechanisms. In another study, Kim et al. [13] reported that patients with a high CSI score (≥40) experienced more intense postoperative pain and required greater analgesic use during the first three months postoperatively. Their study also demonstrated that higher CSI scores were associated with more severe preoperative pain, persistent postoperative pain, and lower satisfaction with pain relief three months after surgery. Interestingly, although UKA is designed to preserve native ligaments and provide more natural knee kinematics, patients with CS did not appear to benefit from those advantages [3]. Instead, they continued to experience significant pain and functional limitations. This suggests that in CS patients, abnormalities in pain processing play a more important role in postoperative recovery than the specific surgical technique used. These findings further support the hypothesis that postoperative pain perception is not solely dictated by structural changes but is also influenced by alterations in central nervous system pain processing.
Preoperative CS not only contributes to persistent pain following surgery but also significantly affects functional outcomes and overall patient satisfaction. In our study, the CS group exhibited poorer WOMAC function and total scores than the non-CS group at the two-year follow-up visit. Additionally, the FJS scores were notably lower in the CS group, indicating a greater level of functional impairment. These findings align with previous studies of TKA [12,14]. Kim et al. [12] reported that the CS group showed significantly inferior preoperative and postoperative WOMAC function and total scores than the non-CS group. Similarly, Koh et al. [14] found that the CS group experienced worse quality of life and greater functional disability than the non-CS group after TKA. In addition, one of the most striking findings of our study is the significant effect of CS on patient satisfaction following UKA. Whereas 88% of patients in the non-CS group reported being satisfied with their surgical outcomes, only 62% of those in the CS group expressed satisfaction (p < 0.01). Sasaki et al. [16] demonstrated that preoperative CS was also negatively associated with postoperative EQ-5D scores in TKA patients. Moreover, Koh et al. [14], using the same new KSS score as in our study, showed that patients in the CS group were significantly more dissatisfied than those in the non-CS group. Further supporting this, our multivariate regression analysis identified CS as a significant predictor of dissatisfaction. The preoperative CSI score (adjust odds ratio = 11.349, p = 0.003) was independently associated with lower satisfaction rates. These findings underscore the importance of preoperative CS assessment, which may help screen high-risk patients and enable tailored interventions, including education and preemptive medication, to improve postoperative satisfaction.
CS is strongly associated with poor clinical outcomes following UKA for several reasons. First, patients with CS often have higher preoperative expectations than those without CS. Specifically, they anticipate greater pain relief and psychological well-being after surgery [29]. Although high expectations can sometimes contribute to favorable postoperative outcomes [30], excessively high expectations are closely linked to dissatisfaction and poor clinical results [31]. Second, the heightened pain sensitivity of CS patients negatively affects their postoperative outcomes [29]. Individuals with CS experience increased pain perception, often presenting with hyperalgesia and allodynia as characteristic symptoms [9]. This heightened sensitivity can play a crucial role in difficulties with post-surgical pain and recovery, further contributing to suboptimal clinical results [29]. Third, CS patients tend to have higher minimal clinically important difference (MCID) thresholds than non-CS patients. As a result, their overall postoperative outcomes tend to be worse, and the likelihood of achieving the MCID is significantly lower [12]. For those reasons, patients with CS are more prone than those without CS to experience persistent pain and inferior outcomes following UKA.
Effective management of CS, particularly in patients undergoing knee arthroplasty, requires a multidimensional approach that extends beyond conventional surgical intervention [14,32,33,34]. First, preoperative education and expectation setting play a crucial role. Numerous studies have demonstrated that preoperative expectations are closely linked to postoperative satisfaction and clinical outcomes [33,34]. For patients with CS, it is especially important to provide detailed explanations about the potential impact of CS on pain perception and recovery trajectory [33,34]. By aligning patient expectations with realistic outcomes, clinicians can mitigate dissatisfaction and enhance shared decision-making [33,34]. Furthermore, specific education on the nature of CS and its role in persistent postoperative pain should be incorporated into preoperative counseling sessions for patients with knee OA scheduled for UKA [33,34]. Second, pharmacologic treatment targeting central pain mechanisms can be an effective adjunct. Among the available agents, the serotonin-norepinephrine reuptake inhibitor (SNRI) duloxetine has shown particular promise in CS-associated pain [32]. In a randomized controlled trial by Koh et al., patients with CS undergoing TKA who received duloxetine experienced not only significant pain reduction starting two weeks postoperatively, but also notable improvements in mood, mental health, sleep quality, and social functioning [14]. These findings suggest that targeting descending pain modulation pathways may alleviate both sensory and affective components of CS-related pain [14]. Taken together, these strategies—preoperative patient-centered education and targeted pharmacotherapy—represent critical components in the perioperative management of patients with CS to improve both subjective and objective surgical outcomes [14,32,33,34]. Although UKA is widely regarded as a minimally invasive and function-preserving procedure, patients with CS may not fully experience its expected clinical benefits due to persistent central pain mechanisms [14,32,33,34]. This does not imply that UKA is counterproductive in CS patients, but rather highlights the need for realistic expectation-setting, individualized pain management, and possibly multimodal interventions to support postoperative recovery in this subgroup.
This study has several strengths, including a well-defined patient cohort, a standardized surgical technique performed by a single surgeon, and the use of validated outcome measures such as the WOMAC and FJS. These factors minimize variability and enhance the reliability of our findings. However, there are also limitations to consider. First, most of the patients who underwent UKAs were female (108 of 131, 89%). Although this demographic trend is well-documented in the Korean population, the underlying reasons remain unclear [35,36,37,38,39,40,41]. Second, although the data were collected prospectively, this study was conducted as a retrospective review using a single-institution database. As a result, inherent limitations such as selection bias might have influenced the findings. Third, various tools exist for assessing patient satisfaction after surgery [42]. In this study, we used the new KSS system, a validated tool designed to minimize the evaluation burden [43]. Although the KSS is widely accepted, incorporating additional assessment methods could provide a more comprehensive evaluation of patient satisfaction. Fourth, the follow-up period was limited to two years, and patient satisfaction was assessed only at the two-year postoperative mark. Longer-term studies are needed to better understand how postoperative satisfaction and its relationship with CS evolve over time. Fifth, the study might be underpowered, increasing the risk of type II errors and potentially limiting the ability to detect all relevant associations. Larger prospective studies with a broader and more diverse patient population are needed to strengthen these findings. Sixth, we used the CSI as the primary tool for assessing CS. Although the CSI is a validated and widely used screening measure [19,20], it is based on self-reported data and might not fully capture the neurophysiological aspects of CS. Future studies incorporating QST or functional neuroimaging could provide a more comprehensive understanding of CS in patients undergoing UKA [44]. Seventh, all surgeries were performed at a single institution by a single surgeon, which might limit the generalizability of the findings to other surgical settings. A multicenter study would help validate these results across different patient populations. Eighth, although we aimed to isolate the impact of CS on UKA outcomes by excluding patients with major psychiatric disorders and CS-related conditions through predefined exclusion criteria [19,20], it is important to acknowledge that completely eliminating all potential CS-associated factors is inherently challenging. Subclinical symptoms or undiagnosed comorbidities, such as mild sleep disturbances or psychological stress, may have persisted and influenced outcomes, representing a limitation of this study. Additionally, although patients with peripheral neuropathy were excluded based on clinical screening, we did not conduct formal neurologic or electrophysiological evaluations. Future studies may benefit from incorporating objective neuropathy assessments and stratifying patients by metabolic comorbidities to better isolate the effects of CS [45]. Lastly, anxiety and depression were excluded based on preoperative evaluation; we did not assess subclinical levels of anxiety or depressive symptoms postoperatively. Considering the established relationship between CS and mood disturbances, this remains a relevant limitation that may have influenced subjective outcome measures [14]. Despite those limitations, this study provides valuable insights into the relationship between CS and both pain and dissatisfaction following UKA.
6. Conclusions
This study underscores the importance of recognizing CS as a critical determinant of postoperative pain and dissatisfaction following UKA. Patients with high CSI scores experience greater pain, increased joint awareness, and overall poorer outcomes despite technically successful surgeries. Patients with CS should be closely monitored postoperatively and provided with appropriate pain management strategies to optimize their surgical outcomes. Future research should focus on refining these strategies and exploring innovative approaches to pain modulation in this patient population.
Supplementary Materials
The following supporting information can be downloaded at: https://www.mdpi.com/article/10.3390/medicina61050912/s1, Figure S1: Central Sensitization Inventory.
Author Contributions
Y.I. had full access to all the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis. Concept and design: M.-S.K. and Y.I.; Acquisition, analysis, or interpretation of data: M.-S.K. and K.-Y.C.; Drafting of the manuscript: M.-S.K. and Y.I.; Critical revision of the manuscript for important intellectual content: All authors; Administrative, technical, or material support: M.-S.K. and K.-Y.C.; Supervision: Y.I. All authors have read and agreed to the published version of the manuscript.
Funding
This work was supported by the National Research Foundation of Korea (NRF) grant funded by the Korean Government (MSIT) (RS-2023-00215891) and Research Fund of Seoul St. Mary’s Hospital, The Catholic University of Korea (ZC25CISI0102).
Institutional Review Board Statement
The study was conducted in accordance with the Declaration of Helsinki, and approved by the Institutional Review Board of Seoul St. Mary’s Hospital (KC22RISI0506).
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study.
Data Availability Statement
The data published in this research are available on request from the corresponding author (Y.I.).
Conflicts of Interest
The authors declare no conflict of interest.
Abbreviations
| CS | Central Sensitization |
| UKA | Unicompartmental Knee Arthroplasty |
| TKA | Total Knee Arthroplasty |
| CSI | Central Sensitization Inventory |
| WOMAC | Western Ontario and McMaster Universities Osteoarthritis Index |
| FJS | Forgotten Joint Score |
| OA | Osteoarthritis |
| CNS | Central Nervous System |
| QST | Quantitative Sensory Testing |
| MB | Mobile-Bearing |
| PROMs | Patient-Reported Outcome Measures |
| KSS | Knee Society Satisfaction |
References
- Digennaro, V.; Ferri, R.; Panciera, A.; Bordini, B.; Cecchin, D.; Benvenuti, L.; Traina, F.; Faldini, C. Coronal plane alignment of the knee (CPAK) classification and its impact on medial unicompartmental knee arthroplasty: Exposing a unexpected external shift of limb mechanical axis in case of prearthritic constitutional valgus alignment: A retrospective radiographic study. Knee Surg. Relat. Res. 2024, 36, 14. [Google Scholar] [CrossRef] [PubMed]
- Koshino, T.; Sato, K.; Umemoto, Y.; Akamatsu, Y.; Kumagai, K.; Saito, T. Clinical results of unicompartmental arthroplasty for knee osteoarthritis using a tibial component with screw fixation. Int. Orthop. 2015, 39, 1085–1091. [Google Scholar] [CrossRef] [PubMed]
- Vasso, M.; Antoniadis, A.; Helmy, N. Update on unicompartmental knee arthroplasty: Current indications and failure modes. EFORT Open Rev. 2018, 3, 442–448. [Google Scholar] [CrossRef]
- Vasso, M.; Del Regno, C.; Perisano, C.; D′Amelio, A.; Corona, K.; Schiavone Panni, A. Unicompartmental knee arthroplasty is effective: Ten year results. Int. Orthop. 2015, 39, 2341–2346. [Google Scholar] [CrossRef]
- Baker, P.N.; Petheram, T.; Avery, P.J.; Gregg, P.J.; Deehan, D.J. Revision for unexplained pain following unicompartmental and total knee replacement. J. Bone Jt. Surg. Am. 2012, 94, e126. [Google Scholar] [CrossRef]
- Calkins, T.E.; Hannon, C.P.; Fillingham, Y.A.; Culvern, C.C.; Berger, R.A.; Della Valle, C.J. Fixed-Bearing Medial Unicompartmental Knee Arthroplasty in Patients Younger Than 55 Years of Age at 4–19 Years of Follow-Up: A Concise Follow-Up of a Previous Report. J. Arthroplasty 2021, 36, 917–921. [Google Scholar] [CrossRef]
- Walsh, J.M.; Burnett, R.A.; Serino, J.; Gerlinger, T.L. Painful Unicompartmental Knee Arthroplasty: Etiology, Diagnosis and Management. Arch. Bone Jt. Surg. 2024, 12, 546–557. [Google Scholar] [CrossRef]
- Clauw, D.J.; Hassett, A.L. The role of centralised pain in osteoarthritis. Clin. Exp. Rheumatol. 2017, 107, 79–84. [Google Scholar]
- Woolf, C.J. Central sensitization: Implications for the diagnosis and treatment of pain. Pain 2011, 152, S2–S15. [Google Scholar] [CrossRef]
- Nijs, J.; Leysen, L.; Vanlauwe, J.; Logghe, T.; Ickmans, K.; Polli, A.; Malfliet, A.; Coppieters, I.; Huysmans, E. Treatment of central sensitization in patients with chronic pain: Time for change? Expert Opin. Pharmacother. 2019, 20, 1961–1970. [Google Scholar] [CrossRef]
- Dave, A.J.; Selzer, F.; Losina, E.; Usiskin, I.; Collins, J.E.; Lee, Y.C.; Band, P.; Dalury, D.F.; Iorio, R.; Kindsfater, K.; et al. The association of pre-operative body pain diagram scores with pain outcomes following total knee arthroplasty. Osteoarthr. Cartil. 2017, 25, 667–675. [Google Scholar] [CrossRef] [PubMed]
- Kim, M.S.; Koh, I.J.; Choi, K.Y.; Seo, J.Y.; In, Y. Minimal Clinically Important Differences for Patient-Reported Outcomes After TKA Depend on Central Sensitization. J. Bone Jt. Surg. Am. 2021, 103, 1374–1382. [Google Scholar] [CrossRef] [PubMed]
- Kim, S.H.; Yoon, K.B.; Yoon, D.M.; Yoo, J.H.; Ahn, K.R. Influence of Centrally Mediated Symptoms on Postoperative Pain in Osteoarthritis Patients Undergoing Total Knee Arthroplasty: A Prospective Observational Evaluation. Pain Pract. 2015, 15, E46–E53. [Google Scholar] [CrossRef]
- Koh, I.J.; Kang, B.M.; Kim, M.S.; Choi, K.Y.; Sohn, S.; In, Y. How Does Preoperative Central Sensitization Affect Quality of Life Following Total Knee Arthroplasty? J. Arthroplasty 2020, 35, 2044–2049. [Google Scholar] [CrossRef]
- Lape, E.C.; Selzer, F.; Collins, J.E.; Losina, E.; Katz, J.N. Stability of Measures of Pain Catastrophizing and Widespread Pain Following Total Knee Replacement. Arthritis Care Res. 2020, 72, 1096–1103. [Google Scholar] [CrossRef]
- Sasaki, E.; Kasai, T.; Araki, R.; Sasaki, T.; Wakai, Y.; Akaishi, K.; Chiba, D.; Kimura, Y.; Yamamoto, Y.; Tsuda, E.; et al. Central Sensitization and Postoperative Improvement of Quality of Life in Total Knee and Total Hip Arthroplasty: A Prospective Observational Study. Prog. Rehabil. Med. 2022, 7, 20220009. [Google Scholar] [CrossRef] [PubMed]
- Iio, R.; Manaka, T.; Nakazawa, K.; Hirakawa, Y.; Ito, Y.; Ogura, A.; Nakamura, H. Assessment of Prevalence and Risk Factors for Central Sensitization Related to Shoulder Osteoarthritis and Rotator Cuff Tears Using the Central Sensitization Inventory: A Cross-Sectional Study in Shoulder Surgery Patients. J. Clin. Med. 2023, 12, 5633. [Google Scholar] [CrossRef]
- Buskila, D. Genetics of chronic pain states. Best Pract. Res. Clin. Rheumatol. 2007, 21, 535–547. [Google Scholar] [CrossRef]
- Mayer, T.G.; Neblett, R.; Cohen, H.; Howard, K.J.; Choi, Y.H.; Williams, M.J.; Perez, Y.; Gatchel, R.J. The development and psychometric validation of the central sensitization inventory. Pain Pract. 2012, 12, 276–285. [Google Scholar] [CrossRef]
- Neblett, R.; Cohen, H.; Choi, Y.; Hartzell, M.M.; Williams, M.; Mayer, T.G.; Gatchel, R.J. The Central Sensitization Inventory (CSI): Establishing clinically significant values for identifying central sensitivity syndromes in an outpatient chronic pain sample. J. Pain 2013, 14, 438–445. [Google Scholar] [CrossRef]
- Lluch, E.; Torres, R.; Nijs, J.; Van Oosterwijck, J. Evidence for central sensitization in patients with osteoarthritis pain: A systematic literature review. Eur. J. Pain 2014, 18, 1367–1375. [Google Scholar] [CrossRef] [PubMed]
- Staud, R.; Robinson, M.E.; Price, D.D. Temporal summation of second pain and its maintenance are useful for characterizing widespread central sensitization of fibromyalgia patients. J. Pain 2007, 8, 893–901. [Google Scholar] [CrossRef] [PubMed]
- Jensen, K.B.; Srinivasan, P.; Spaeth, R.; Tan, Y.; Kosek, E.; Petzke, F.; Carville, S.; Fransson, P.; Marcus, H.; Williams, S.C.; et al. Overlapping structural and functional brain changes in patients with long-term exposure to fibromyalgia pain. Arthritis Rheum. 2013, 65, 3293–3303. [Google Scholar] [CrossRef]
- Napadow, V.; Kim, J.; Clauw, D.J.; Harris, R.E. Decreased intrinsic brain connectivity is associated with reduced clinical pain in fibromyalgia. Arthritis Rheum. 2012, 64, 2398–2403. [Google Scholar] [CrossRef]
- Akinci, A.; Al Shaker, M.; Chang, M.H.; Cheung, C.W.; Danilov, A.; José Dueñas, H.; Kim, Y.C.; Guillen, R.; Tassanawipas, W.; Treuer, T.; et al. Predictive factors and clinical biomarkers for treatment in patients with chronic pain caused by osteoarthritis with a central sensitisation component. Int. J. Clin. Pract. 2016, 70, 31–44. [Google Scholar] [CrossRef]
- Kim, M.S.; Koh, I.J.; Kim, C.K.; Choi, K.Y.; Kim, C.Y.; In, Y. Cross-cultural adaptation and validation of the Korean version of the Central Sensitization Inventory in patients undergoing total knee arthroplasty for knee osteoarthritis. PLoS ONE 2020, 15, e0242912. [Google Scholar] [CrossRef]
- Lundblad, H.; Kreicbergs, A.; Jansson, K.A. Prediction of persistent pain after total knee replacement for osteoarthritis. J. Bone Jt. Surg. Br. 2008, 90, 166–171. [Google Scholar] [CrossRef]
- Martinez, V.; Fletcher, D.; Bouhassira, D.; Sessler, D.I.; Chauvin, M. The evolution of primary hyperalgesia in orthopedic surgery: Quantitative sensory testing and clinical evaluation before and after total knee arthroplasty. Anesth. Analg. 2007, 105, 815–821. [Google Scholar] [CrossRef]
- Kim, M.S.; Koh, I.J.; Sung, Y.G.; Park, D.C.; Yoon, E.J.; In, Y. Influence of increased pain sensitivity on patient-reported outcomes following total knee arthroplasty. Knee Surg. Sports Traumatol. Arthrosc. 2022, 30, 782–790. [Google Scholar] [CrossRef]
- Flood, A.B.; Lorence, D.P.; Ding, J.; McPherson, K.; Black, N.A. The role of expectations in patients’ reports of post-operative outcomes and improvement following therapy. Med. Care 1993, 31, 1043–1056. [Google Scholar] [CrossRef]
- Mancuso, C.A.; Reid, M.C.; Duculan, R.; Girardi, F.P. Improvement in Pain After Lumbar Spine Surgery: The Role of Preoperative Expectations of Pain Relief. Clin. J. Pain 2017, 33, 93–98. [Google Scholar] [CrossRef] [PubMed]
- Itoh, N.; Tsuji, T.; Ishida, M.; Ochiai, T.; Konno, S.; Uchio, Y. Efficacy of duloxetine for multisite pain in patients with knee pain due to osteoarthritis: An exploratory post hoc analysis of a Japanese phase 3 randomized study. J. Orthop. Sci. 2021, 26, 141–148. [Google Scholar] [CrossRef] [PubMed]
- Louw, A.; Diener, I.; Butler, D.S.; Puentedura, E.J. The effect of neuroscience education on pain, disability, anxiety, and stress in chronic musculoskeletal pain. Arch. Phys. Med. Rehabil. 2011, 92, 2041–2056. [Google Scholar] [CrossRef] [PubMed]
- Watson, J.A.; Ryan, C.G.; Cooper, L.; Ellington, D.; Whittle, R.; Lavender, M.; Dixon, J.; Atkinson, G.; Cooper, K.; Martin, D.J. Pain Neuroscience Education for Adults with Chronic Musculoskeletal Pain: A Mixed-Methods Systematic Review and Meta-Analysis. J. Pain 2019, 20, 1140.e1–1140.e22. [Google Scholar] [CrossRef]
- Kim, D.H.; Jeong, S.Y.; Yang, J.H.; Choi, C.H. Evaluation of Appropriateness of the Reimbursement Criteria of Korean Health Insurance Review and Assessment Service for Total Knee Arthroplasty. Clin. Orthop. Surg. 2023, 15, 241–248. [Google Scholar] [CrossRef]
- Kim, K.I.; Kim, J.H.; Min, K. Does the clinical and radiologic outcomes following total knee arthroplasty using a new design cobalt-chrome tibial plate or predecessor different? Knee Surg. Relat. Res. 2024, 36, 34. [Google Scholar] [CrossRef]
- Kim, S.E.; Ro, D.H.; Lee, M.C.; Han, H.S. Can individual functional improvements be predicted in osteoarthritic patients after total knee arthroplasty? Knee Surg. Relat. Res. 2024, 36, 31. [Google Scholar] [CrossRef]
- Ko, K.; Kim, K.H.; Ko, S.; Jo, C.; Han, H.S.; Lee, M.C.; Ro, D.H. Total Knee Arthroplasty: Is It Safe? A Single-Center Study of 4124 Patients in South Korea. Clin. Orthop. Surg. 2023, 15, 935–941. [Google Scholar] [CrossRef]
- Lee, Y.M.; Kim, G.W.; Lee, C.Y.; Song, E.K.; Seon, J.K. No Difference in Clinical Outcomes and Survivorship for Robotic, Navigational, and Conventional Primary Total Knee Arthroplasty with a Minimum Follow-up of 10 Years. Clin. Orthop. Surg. 2023, 15, 82–91. [Google Scholar] [CrossRef]
- Nagata, N.; Hiranaka, T.; Okamoto, K.; Fujishiro, T.; Tanaka, T.; Kensuke, A.; Kitazawa, D.; Kotoura, K. Is simultaneous bilateral unicompartmental knee arthroplasty and total knee arthroplasty better than simultaneous bilateral total knee arthroplasty? Knee Surg. Relat. Res. 2023, 35, 12. [Google Scholar] [CrossRef]
- Park, J.; Chang, M.J.; Kim, T.W.; D′Lima, D.D.; Kim, H.; Han, H.S. Serial changes in patient-reported outcome measures and satisfaction rate during long-term follow-up after total knee arthroplasty: A systematic review and meta-analysis. Knee Surg. Relat. Res. 2024, 36, 43. [Google Scholar] [CrossRef]
- Webster, K.E.; Feller, J.A. Comparison of the short form-12 (SF-12) health status questionnaire with the SF-36 in patients with knee osteoarthritis who have replacement surgery. Knee Surg. Sports Traumatol. Arthrosc. 2016, 24, 2620–2626. [Google Scholar] [CrossRef] [PubMed]
- Noble, P.C.; Scuderi, G.R.; Brekke, A.C.; Sikorskii, A.; Benjamin, J.B.; Lonner, J.H.; Chadha, P.; Daylamani, D.A.; Scott, W.N.; Bourne, R.B. Development of a new Knee Society scoring system. Clin. Orthop. Relat. Res. 2012, 470, 20–32. [Google Scholar] [CrossRef]
- Wylde, V.; Palmer, S.; Learmonth, I.D.; Dieppe, P. The association between pre-operative pain sensitisation and chronic pain after knee replacement: An exploratory study. Osteoarthr. Cartil. 2013, 21, 1253–1256. [Google Scholar] [CrossRef]
- Currado, D.; Berardicurti, O.; Saracino, F.; Trunfio, F.; Kun, L.; Marino, A.; Corberi, E.; Lamberti, L.; Ruscitti, P.; Liakouli, V.; et al. The Relationship Between Metabolic Syndrome and Pain Catastrophizing in Psoriatic Arthritis. Rheumatol. Ther. 2025, 12, 581–592. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Published by MDPI on behalf of the Lithuanian University of Health Sciences. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).