Impacts of an Oral Appliance on Snoring in Adults with Varying Degrees of Snoring Severity: A Preliminary Study
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design
2.2. Study Population
2.3. Interventions
2.4. Outcome Measures
2.5. Statistical Analysis
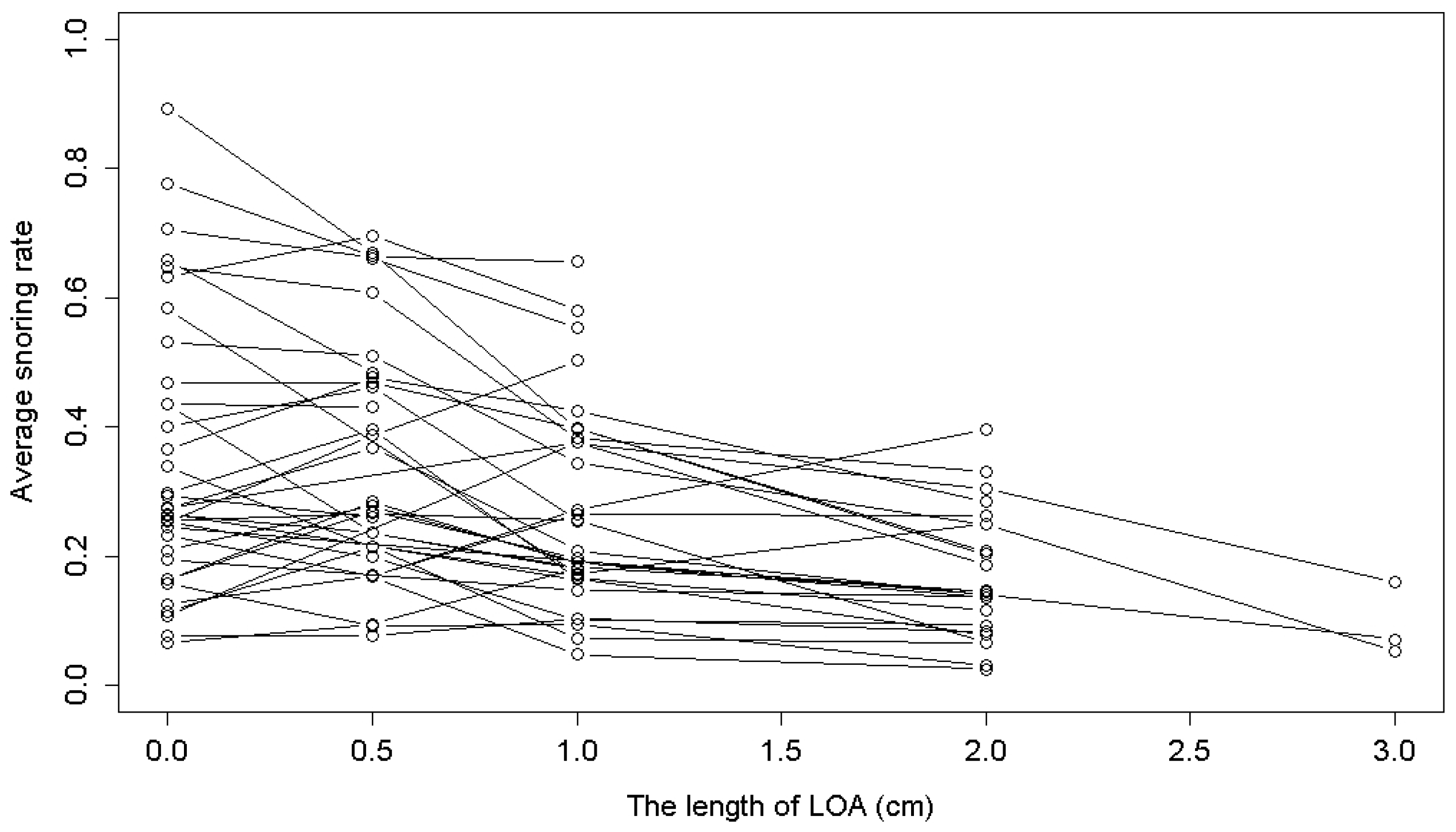
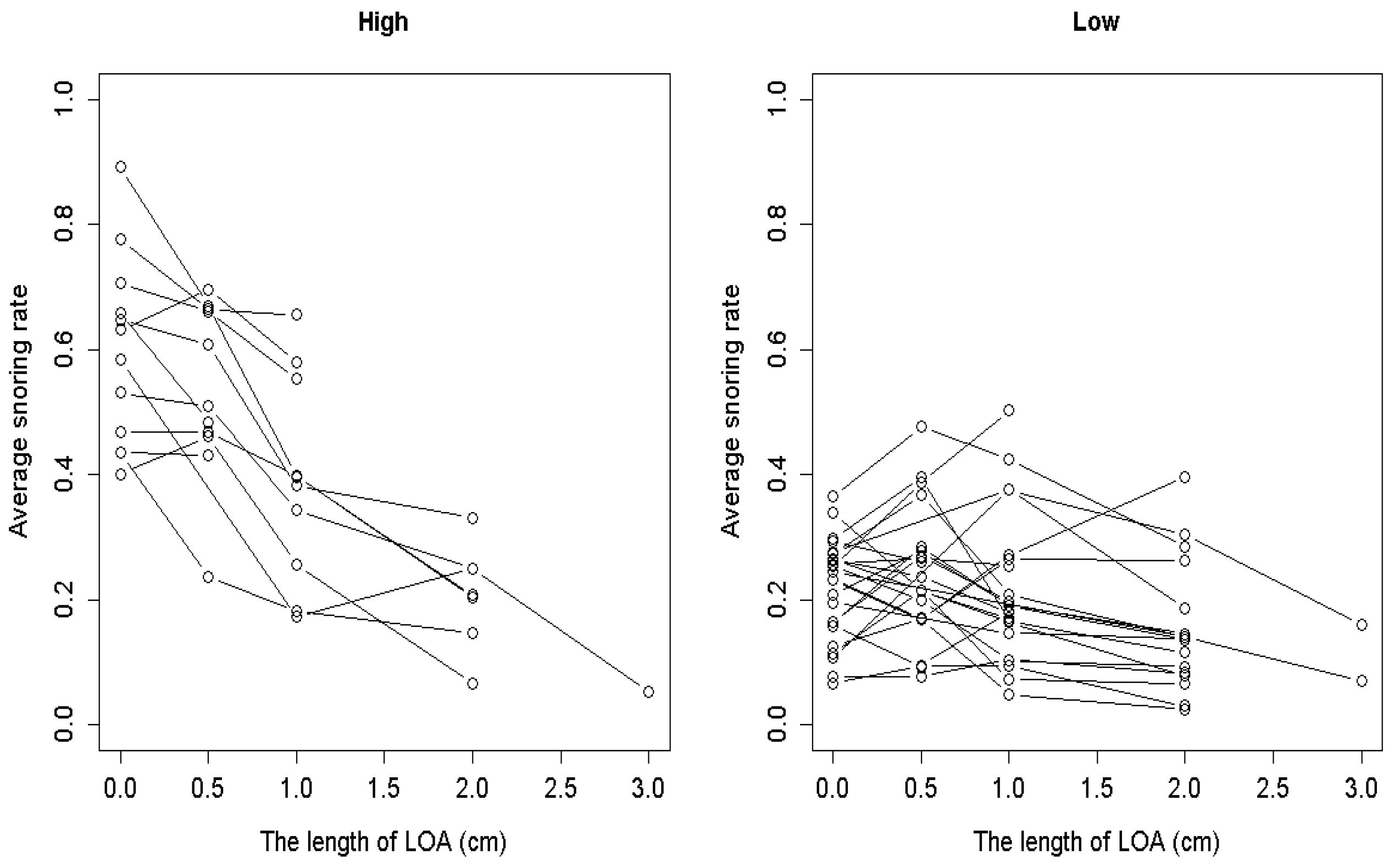
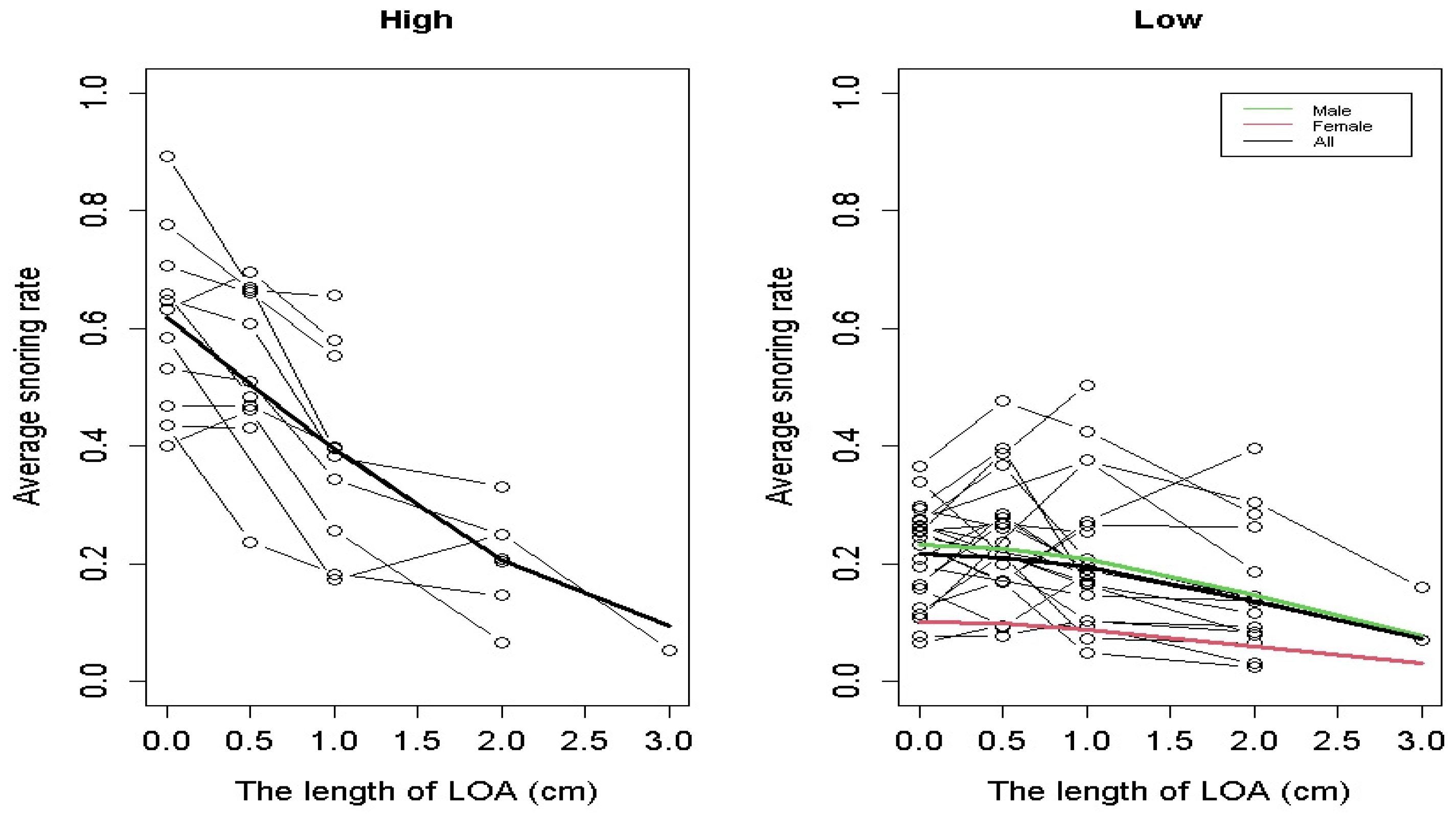
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Appendix A
| L Group | Model | Intercept | Coefficient |
|---|---|---|---|
| Squared LOA length | Pooled | −1.312 (<0.001) | −0.128 (0.002) |
| Random effect | −1.282 (<0.001) | −0.142 (<0.001) | |
| Male | Pooled | −2.371 (<0.001) | 0.981 (<0.001) |
| Random effect | −1.364 (<0.001) | −0.003 (0.007) |
References
- Pevernagie, D.; Aarts, R.M.; De Meyer, M. The acoustics of snoring. Sleep Med. Rev. 2010, 14, 131–144. [Google Scholar] [CrossRef] [PubMed]
- Yunus, F.M.; Khan, S.; Mitra, D.K.; Mistry, S.K.; Afsana, K.; Rahman, M. Relationship of sleep pattern and snoring with chronic disease: Findings from a nationwide population-based survey. Sleep Health 2018, 4, 40–48. [Google Scholar] [CrossRef] [PubMed]
- Chuang, L.P.; Hsu, S.C.; Lin, S.W.; Ko, W.S.; Chen, N.H.; Tsai, Y.H. Prevalence of snoring and witnessed apnea in Taiwanese adults. Chang Gung Med. J. 2008, 31, 175–181. [Google Scholar] [PubMed]
- Sekizuka, H.; Miyake, H. Relationship between Snoring and Lifestyle-related Diseases among a Japanese Occupational Population. Intern. Med. 2020, 59, 2221–2228. [Google Scholar] [CrossRef]
- Patel, M.; Tran, D.; Chakrabarti, A.; Vasquez, A.; Gilbert, P.; Davidson, T. Prevalence of snoring in college students. J. Am. Coll. Health 2008, 57, 45–52. [Google Scholar] [CrossRef]
- Kara, C.O.; Zencir, M.; Topuz, B.; Ardic, N.; Kocagozoglu, B. The prevalence of snoring in adult population. Kulak Burun Bogaz Ihtis. Derg. 2005, 14, 18–24. [Google Scholar]
- Park, C.G.; Shin, C. Prevalence and association of snoring, anthropometry and hypertension in Korea. Blood Press. 2005, 14, 210–216. [Google Scholar] [CrossRef]
- Lam, B.; Ip, M.S.; Tench, E.; Ryan, C.F. Craniofacial profile in Asian and white subjects with obstructive sleep apnoea. Thorax 2005, 60, 504–510. [Google Scholar] [CrossRef]
- Chan, C.H.; Wong, B.M.; Tang, J.L.; Ng, D.K. Gender difference in snoring and how it changes with age: Systematic review and meta-regression. Sleep Breath. 2012, 16, 977–986. [Google Scholar] [CrossRef]
- Knuiman, M.; James, A.; Divitini, M.; Bartholomew, H. Longitudinal study of risk factors for habitual snoring in a general adult population: The Busselton Health Study. Chest 2006, 130, 1779–1783. [Google Scholar] [CrossRef]
- Young, T.; Finn, L.; Hla, K.M.; Morgan, B.; Palta, M. Snoring as part of a dose-response relationship between sleep-disordered breathing and blood pressure. Sleep 1996, 19, S202–S205. [Google Scholar] [CrossRef] [PubMed]
- Bixler, E.O.; Vgontzas, A.N.; Lin, H.M.; Ten Have, T.; Leiby, B.E.; Vela-Bueno, A.; Kales, A. Association of hypertension and sleep-disordered breathing. Arch. Intern. Med. 2000, 160, 2289–2295. [Google Scholar] [CrossRef] [PubMed]
- Silverberg, D.S.; Oksenberg, A. Are sleep-related breathing disorders important contributing factors to the production of essential hypertension? Curr. Hypertens. Rep. 2001, 3, 209–215. [Google Scholar] [CrossRef] [PubMed]
- Bednarek, M.; Polakowska, M.; Kurjata, P.; Kupsc, W.; Plywaczewski, R.; Zgierska, A.; Zielinski, J. Snoring and excessive daytime somnolence and risk of cardiovascular diseases. Pol. Arch. Med. Wewn. 2001, 105, 11–17. [Google Scholar]
- Wada, H.; Furuya, S.; Maruyama, K.; Ikeda, A.; Kondo, K.; Tanigawa, T. Japan Gerontological Evaluation Study Group Prevalence and clinical impact of snoring in older community-dwelling adults. Geriatr. Gerontol. Int. 2019, 19, 1165–1171. [Google Scholar] [CrossRef]
- Guilleminault, C.; Stoohs, R.; Shiomi, T.; Kushida, C.; Schnittger, I. Upper airway resistance syndrome, nocturnal blood pressure monitoring, and borderline hypertension. Chest 1996, 109, 901–908. [Google Scholar] [CrossRef]
- Maimon, N.; Hanly, P.J. Does snoring intensity correlate with the severity of obstructive sleep apnea? J. Clin. Sleep Med. 2010, 6, 475–478. [Google Scholar] [CrossRef]
- Deeb, R.; Smeds, M.R.; Bath, J.; Peterson, E.; Roberts, M.; Beckman, N.; Lin, J.C.; Yaremchuk, K. Snoring and carotid artery disease: A new risk factor emerges. Laryngoscope 2019, 129, 265–268. [Google Scholar] [CrossRef]
- Kohler, M.; Stradling, J.R. Mechanisms of vascular damage in obstructive sleep apnea. Nat. Rev. Cardiol. 2010, 7, 677–685. [Google Scholar] [CrossRef]
- Calabrese, P.; Perrault, H.; Dinh, T.P.; Eberhard, A.; Benchetrit, G. Cardiorespiratory interactions during resistive load breathing. Am. J. Physiol. Regul. Integr. Comp. Physiol. 2000, 279, R2208–R2213. [Google Scholar] [CrossRef]
- Henke, K.G.; Sullivan, C.E. Effects of high-frequency oscillating pressures on upper airway muscles in humans. J. Appl. Physiol. 1993, 75, 856–862. [Google Scholar] [CrossRef] [PubMed]
- Stoohs, R.; Guilleminault, C. Snoring during NREM sleep: Respiratory timing, esophageal pressure and EEG arousal. Respir. Physiol. 1991, 85, 151–167. [Google Scholar] [CrossRef] [PubMed]
- Trotter, M.I.; Morgan, D.W. Snoring: Referral, investigation and treatment. Br. J. Hosp. Med. 2007, 68, 95–99. [Google Scholar] [CrossRef] [PubMed]
- Ramar, K.; Dort, L.C.; Katz, S.G.; Lettieri, C.J.; Harrod, C.G.; Thomas, S.M.; Chervin, R.D. Clinical Practice Guideline for the Treatment of Obstructive Sleep Apnea and Snoring with Oral Appliance Therapy: An Update for 2015. J. Clin. Sleep Med. 2015, 11, 773–827. [Google Scholar] [CrossRef]
- Sutherland, K.; Chan, A.S.; Cistulli, P.A. Three-dimensional assessment of anatomical balance and oral appliance treatment outcome in obstructive sleep apnoea. Sleep Breath. 2016, 20, 903–910. [Google Scholar] [CrossRef]
- Sutherland, K.; Vanderveken, O.M.; Tsuda, H.; Marklund, M.; Gagnadoux, F.; Kushida, C.A.; Cistulli, P.A. Oral appliance treatment for obstructive sleep apnea: An update. J. Clin. Sleep Med. 2014, 10, 215–227. [Google Scholar] [CrossRef]
- Scherr, S.C.; Dort, L.C.; Almeida, F.; Bennett, K.; Blumenstock, N.T.; Demko, B.G.; Essick, G.K.; Katz, S.; McLornan, P.M.; Phillips, K.S.; et al. Definition of an effective oral appliance for the treatment of obstructive sleep apnea and snoring: A report of the American Academy of Dental Sleep Medicine. J. Dent. Sleep Med. 2014, 1, 39–50. [Google Scholar] [CrossRef]
- Van Haesendonck, G.; Dieltjens, M.; Hamans, E.; Braem, M.J.; Vanderveken, O.M. Treatment efficacy of a titratable oral appliance in obstructive sleep apnea patients: A prospective clinical trial. B-ENT 2016, 12, 1–8. [Google Scholar]
- Kao, H.H.; Lin, Y.C.; Chiang, J.K.; Ho, M.; Yu, H.C.; Hsu, C.Y.; Lu, C.M.; Kao, Y.H. Effects of a novel oral appliance on snoring in adults: A pilot study. J. Dent. Sci. 2022, 17, 521–527. [Google Scholar] [CrossRef]
- Nature Dental Clinic. Available online: https://alliswell.tw/?lang=en (accessed on 10 January 2025).
- Adstrum, S.; Hedley, G.; Schleip, R.; Stecco, C.; Yucesoy, C.A. Defining the fascial system. J. Bodyw. Mov. Ther. 2017, 21, 173–177. [Google Scholar] [CrossRef]
- Chiang, J.K.; Lin, Y.C.; Lin, C.W.; Ting, C.S.; Chiang, Y.Y.; Kao, Y.H. Validation of snoring detection using a smartphone app. Sleep Breath. 2022, 26, 81–87. [Google Scholar] [CrossRef] [PubMed]
- Chiang, J.K.; Lin, Y.C.; Lu, C.M.; Kao, Y.H. Correlation between snoring sounds and obstructive sleep apnea in adults: A meta-regression analysis. Sleep Sci. 2022, 15, 463–470. [Google Scholar] [CrossRef] [PubMed]
- Khoo, S.M.; Tan, W.C.; Ng, T.P.; Ho, C.H. Risk factors associated with habitual snoring and sleep-disordered breathing in a multi-ethnic Asian population: A population-based study. Respir. Med. 2004, 98, 557–566. [Google Scholar] [CrossRef] [PubMed]
- Nagayoshi, M.; Yamagishi, K.; Tanigawa, T.; Sakurai, S.; Kitamura, A.; Kiyama, M.; Imano, H.; Ohira, T.; Sato, S.; Sankai, T.; et al. Risk factors for snoring among Japanese men and women: A community-based cross-sectional study. Sleep Breath. 2011, 15, 63–69. [Google Scholar] [CrossRef]
- Hoffstein, V. Review of oral appliances for treatment of sleep-disordered breathing. Sleep Breath. 2007, 11, 1–22. [Google Scholar] [CrossRef]
- Marklund, M.; Carlberg, B.; Forsgren, L.; Olsson, T.; Stenlund, H.; Franklin, K.A. Oral Appliance Therapy in Patients With Daytime Sleepiness and Snoring or Mild to Moderate Sleep Apnea: A Randomized Clinical Trial. JAMA Intern. Med. 2015, 175, 1278–1285. [Google Scholar] [CrossRef]
- Partinen, M.; Gislason, T. Basic Nordic Sleep Questionnaire (BNSQ): A quantitated measure of subjective sleep complaints. J. Sleep Res. 1995, 4, 150–155. [Google Scholar] [CrossRef]

| Variables | All | H Group | L Group | p-Value |
|---|---|---|---|---|
| Participants | 36 | 12 | 24 | |
| Number of records | 4052 | 1201 | 2851 | |
| Female/male | 6/30 | 4/8 | 2/22 | 0.155 |
| Age, years | 44.91 ± 9.96 | 42.83 ± 10.96 | 46.15 ± 9.38 | 0.393 |
| BMI, kg/m2 | 26.18 ± 3.50 | 26.01 ± 3.38 | 26.27 ± 3.65 | 0.859 |
| Recording time, min | 398.27 ± 77.56 | 391.77 ± 68.96 | 401.01 ± 80.77 | <0.001 |
| Snoring rate, % [n *] | ||||
| LOA-0 | 29.48 ± 22.43 [532] | 56.53 ± 15.71 [144] | 19.44 ± 15.02 [388] | <0.001 |
| LOA-0.5 cm | 31.76 ± 21.41 [430] | 54.97 ± 18.37 [117] | 23.08 ± 15.07 [313] | <0.001 |
| LOA-1 cm | 25.87 ± 18.07 [1227] | 33.21 ± 18.67 [574] | 19.41 ± 14.79 [653] | <0.001 |
| LOA-2 cm | 15.22 ± 12.73 [1499] | 21.75 ± 13.20 [356] | 13.19 ± 11.88 [1143] | <0.001 |
| LOA-3 cm | 9.03 ± 8.82 [364] | 5.38 ± 5.92 [10] | 9.13 ± 8.87 [354] | 0.080 |
| Version (cm) | All | H Group | L Group | p-Value a |
|---|---|---|---|---|
| 0 to 0.5 | −0.83 (0.314 b) | −6.27 (0.032 b) | 2.16 (0.235 c) | 0.0274 |
| 0.5 to 1 | −7.20 (<0.001 b) | −13.62 (<0.001 b) | −4.15 (0.036 b) | 0.0182 |
| 1 to 2 | −6.06 (<0.001 b) | −9.69 (0.024 b) | −4.47 (0.010 b) | 0.2520 |
| 2 to 3 | −13.70 | −19.65 | −10.72 | - |
| Group | Model | LOA Length | Squared LOA Length | Male vs. Female | Intercept | p-Value |
|---|---|---|---|---|---|---|
| H group | <0.001 | |||||
| Pooled | −1.009 (<0.001) | 0.536 (<0.001) | ||||
| Random effect | −0.916 (<0.001) | 0.483 (0.006) | ||||
| L group (Model 1) | <0.001 | |||||
| Pooled | −0.129 (<0.001) | 0.983 (<0.001) | −2.202 (<0.001) | |||
| Random effect | −0.141 (<0.001) | 0.986 (0.004) | −2.186 (<0.001) | |||
| L group (Model 2) | <0.001 | |||||
| Pooled | −0.128 (0.002) | - | −1.312 (<0.001) | |||
| Random effect | −0.142 (<0.001) | - | −1.282 (<0.001) | |||
| LOA-0 | LOA-0.5 | LOA-1 | LOA-2 | LOA-3 | |
|---|---|---|---|---|---|
| H group | 61.9 | 50.6 | 39.3 | 20.6 | 9.4 |
| L group (model 2) | 21.7 | 21.1 | 19.4 | 13.6 | 7.2 |
| L group (model 1, male) | 23.2 | 22.5 | 20.7 | 14.7 | 7.8 |
| L group (model 1, female) | 10.1 | 9.8 | 8.9 | 6.0 | 3.1 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Published by MDPI on behalf of the Lithuanian University of Health Sciences. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Cheng, Y.-H.; Chiang, J.-K.; Lin, Y.-C.; Kao, H.-H.; Kao, Y.-H. Impacts of an Oral Appliance on Snoring in Adults with Varying Degrees of Snoring Severity: A Preliminary Study. Medicina 2025, 61, 893. https://doi.org/10.3390/medicina61050893
Cheng Y-H, Chiang J-K, Lin Y-C, Kao H-H, Kao Y-H. Impacts of an Oral Appliance on Snoring in Adults with Varying Degrees of Snoring Severity: A Preliminary Study. Medicina. 2025; 61(5):893. https://doi.org/10.3390/medicina61050893
Chicago/Turabian StyleCheng, Yu-Hsiang, Jui-Kun Chiang, Yen-Chang Lin, Hsueh-Hsin Kao, and Yee-Hsin Kao. 2025. "Impacts of an Oral Appliance on Snoring in Adults with Varying Degrees of Snoring Severity: A Preliminary Study" Medicina 61, no. 5: 893. https://doi.org/10.3390/medicina61050893
APA StyleCheng, Y.-H., Chiang, J.-K., Lin, Y.-C., Kao, H.-H., & Kao, Y.-H. (2025). Impacts of an Oral Appliance on Snoring in Adults with Varying Degrees of Snoring Severity: A Preliminary Study. Medicina, 61(5), 893. https://doi.org/10.3390/medicina61050893





