Observational Study on Progressive Muscle Relaxation and Breathing Control for Reducing Dental Anxiety in Children
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design
- Group A (Breathing Control) practiced guided diaphragmatic breathing before dental treatment.
- Group B (JPMR) received a brief structured muscle relaxation session before treatment.
- The Control Group received standard dental care with no relaxation intervention.
2.2. Participants
- Children and adolescents aged 8–17 years;
- Scheduled for non-invasive prophylactic dental procedures;
- Fluent in Romanian or able to follow instructions with minimal support;
- Provided informed consent by parent/guardian and assent by the child.
- Diagnosed cognitive or developmental disorders;
- Current psychiatric treatment, anxiolytic medication use;
- Acute dental pain or emergency treatment needs.
2.3. Ethical Considerations
2.4. Sample Size Calculation and Group Allocation
- Group A (Breathing Control): n = 63;
- Group B (JPMR): n = 63;
- Control Group: n = 63.
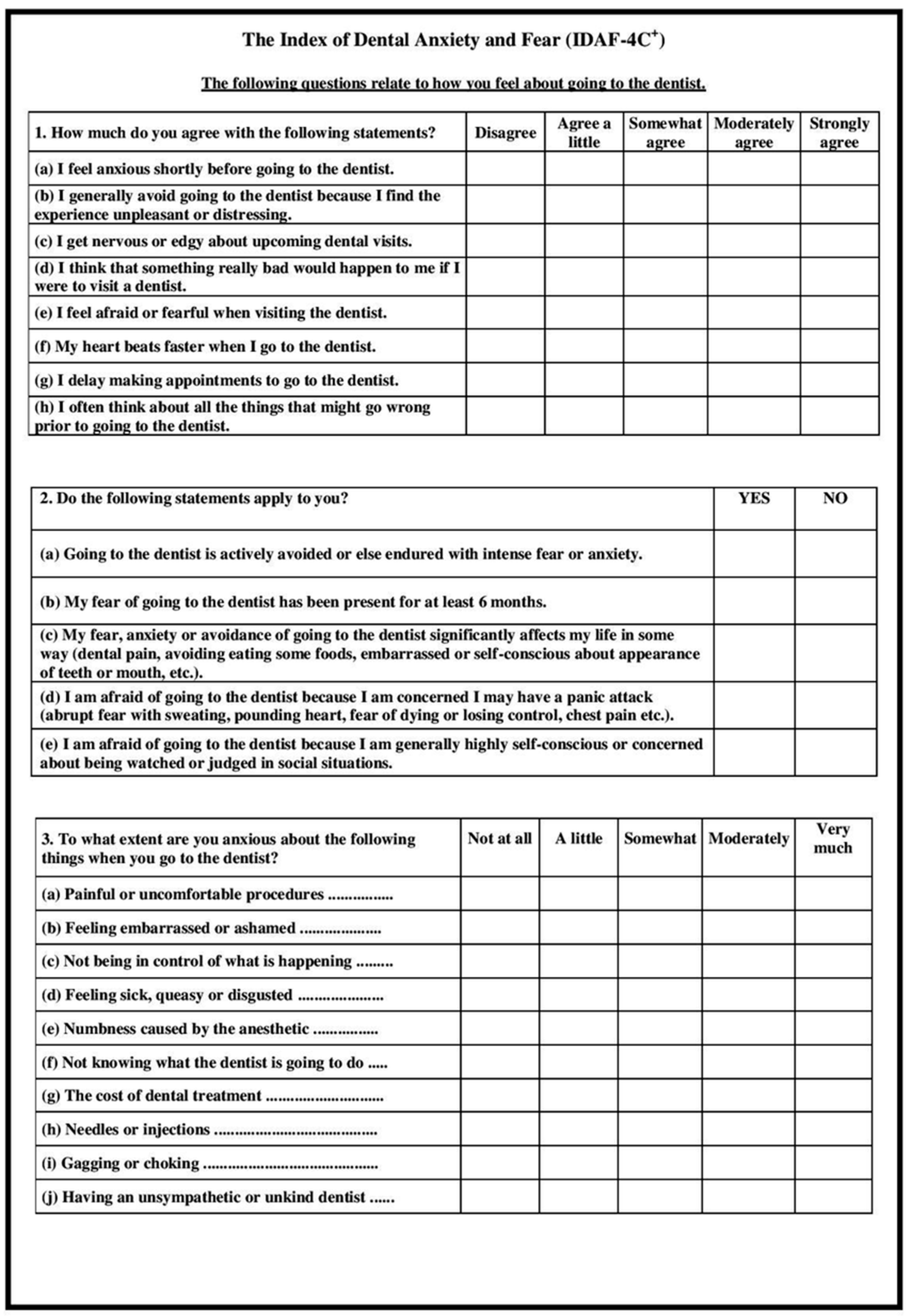
2.5. Psychological Measures
- Core module (8 items) that evaluates emotional, behavioral, cognitive, and physiological anxiety dimensions using a 5-point Likert scale.
- Interpretation: A mean score ≥ 3 indicates clinically significant dental anxiety.
2.6. Physiological Measures
- Baseline: Measured before intervention or procedure;
- Post-intervention: Measured immediately after the dental treatment.
2.7. Intervention Protocols
- Group A (BC): A 5 min diaphragmatic breathing session guided by trained personnel; participants were instructed to inhale deeply through the nose and exhale slowly through the mouth, with hand-on-abdomen for tactile feedback.
- Group B (JPMR): A 10 min JPMR session guided by audio and an assistant, focused on sequential tensing and relaxing muscle groups (hands, arms, shoulders, face, legs), emphasizing the contrast between tension and relaxation.
- The Control Group received routine dental care without any relaxation techniques.
2.8. Procedure Overview
2.9. Data Analysis
3. Results
3.1. Demographic Characteristics and Baseline Anxiety
3.2. Within-Group Comparisons
3.3. Between-Group Comparisons
3.4. Cluster Analysis: Individual Response Patterns
- Cluster 1 represented the most reactive group and primarily benefited from JPMR.
- Cluster 2 showed moderate improvement across interventions.
- Cluster 3 had the lowest baseline anxiety and minimal measurable benefit.
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Appendix A
Appendix A.1. Jacobson’s Progressive Muscle Relaxation (JPMR) Technique in the Dental Setting [3]
- Begin with a few slow, gentle breaths. Ask the patient to inhale softly, pause, and then exhale slowly.
- Feet and legs: The child pulls the toes upward slightly toward the knees, just enough to feel the muscles engage, then holds for a moment, and releases. Then, the child presses the heels down onto the footrest, holds briefly, and relaxes.
- Legs and hips: Ask the child to press their knees gently together, hold briefly, and allow them to drift apart slightly. Then, have them squeeze the gluteal muscles together, hold, and relax.
- Abdomen: Guide the child to draw their tummy slightly toward their spine, hold, and then release. Emphasize noticing how their body feels when relaxed.
- Shoulders and arms: Ask the child to slowly lift their shoulders toward their ears, just enough to notice tension, hold, and let them drop. Then, have them gently press their elbows into their sides, hold, and relax.
- Hands: Instruct them to softly clench their fists, hold for a few seconds, then open their hands, and let them rest.
- Neck and face: Tilt the head forward, make a break, and let it return to a natural, balanced position. Ask them to clench their teeth slightly, hold, and then relax the jaw. Press lips together gently, hold, and then let them loosen naturally. Instruct the child to press their tongue against the roof of their palate, hold it, and let it fall into a relaxed position.
- Eyes and forehead: Ask the child to squint the eyes gently and then release them. Finally, have them furrow their brow slightly, hold, and then allow the forehead to soften.
Appendix B
Appendix B.1. Romanian Index of Dental Anxiety and Fear (IDAF-4C+) [26]
References
- Stein Duker, L.I.; Grager, M.; Giffin, W.; Hikita, N.; Polido, J.C. The Relationship between Dental Fear and Anxiety, General Anxiety/Fear, Sensory Over-Responsivity, and Oral Health Behaviors and Outcomes: A Conceptual Model. Int. J. Environ. Res. Public Health 2022, 19, 2380. [Google Scholar] [CrossRef] [PubMed]
- Slabšinskienė, E.; Kavaliauskienė, A.; Žemaitienė, M.; Vasiliauskienė, I.; Zaborskis, A. Dental Fear and Associated Factors among Children and Adolescents: A School-Based Study in Lithuania. Int. J. Environ. Res. Public Health 2021, 18, 8883. [Google Scholar] [CrossRef]
- Avramova, N.T. Dental Fear, Anxiety, and Phobia—Behavioral Management and Implications for Dentists. J. Mind Med. Sci. 2023, 10, 42–50. [Google Scholar] [CrossRef]
- Grisolia, B.M.; Dos Santos, A.P.P.; Dhyppolito, I.M.; Buchanan, H.; Hill, K.; Oliveira, B.H. Prevalence of dental anxiety in children and adolescents globally: A systematic review with meta-analyses. Int. J. Paediatr. Dent. 2021, 31, 168–183. [Google Scholar] [CrossRef]
- Sun, I.G.; Chu, C.H.; Lo, E.C.M.; Duangthip, D. Global prevalence of early childhood dental fear and anxiety: A systematic review and meta-analysis. J. Dent. 2024, 142, 104841. [Google Scholar] [CrossRef]
- Alamoudi, R.A.; Bamashmous, N.; Albeladi, N.H.; Sabbagh, H.J. Risk Factors Associated with Children’s Behavior in Dental Clinics: A Cross-Sectional Study. Children 2024, 11, 677. [Google Scholar] [CrossRef] [PubMed]
- Klingberg, G.; Broberg, A.G. Dental fear/anxiety and dental behaviour management problems in children and adolescents: A review of prevalence and concomitant psychological factors. Int. J. Paediatr. Dent. 2007, 17, 391–406. [Google Scholar] [CrossRef]
- Skversky-Blocq, Y.; Haaker, J.; Shechner, T. Watch and Learn: Vicarious Threat Learning across Human Development. Brain Sci. 2021, 11, 1345. [Google Scholar] [CrossRef]
- Gautam, S.; Jain, A.; Chaudhary, J.; Gautam, M.; Gaur, M.; Grover, S. Concept of mental health and mental well-being, its determinants and coping strategies. Indian J. Psychiatry 2024, 66, S231–S244. [Google Scholar] [CrossRef]
- Duică, L.; Antonescu, E.; Totan, M.; Antonescu, O.R.; Boța, G.; Maniu, I.; Pirlog, M.C.; Silișteanu, S.C. Perceived Stress, Resilience and Emotional Intelligence in Romanian Healthcare Professionals. Healthcare 2024, 12, 2336. [Google Scholar] [CrossRef]
- Okuro, R.T.; Freire, R.C.; Zin, W.A.; Quagliato, L.A.; Nardi, A.E. Panic disorder respiratory subtype: Psychopathology and challenge tests—An update. Braz. J. Psychiatry 2020, 42, 420–430. [Google Scholar] [CrossRef]
- Banushi, B.; Brendle, M.; Ragnhildstveit, A.; Murphy, T.; Moore, C.; Egberts, J.; Robison, R. Breathwork interventions for adults with clinically diagnosed anxiety disorders: A scoping review. Brain Sci. 2023, 13, 256. [Google Scholar] [CrossRef] [PubMed]
- Pippalapalli, J.; Lumb, A.B. The respiratory system and acid-base disorders. BJA Educ. 2023, 23, 221–228. [Google Scholar] [CrossRef]
- Zhang, D.; Li, S.; Zhang, R. Effects of dental anxiety and anesthesia on vital signs during tooth extraction. BMC Oral Health 2024, 24, 632. [Google Scholar] [CrossRef] [PubMed]
- Hamdani, S.U.; Zafar, S.W.; Suleman, N.; Waqas, A.; Rahman, A.A. Effectiveness of relaxation techniques ‘as an active ingredient of psychological interventions’ to reduce distress, anxiety and depression in adolescents: A systematic review and meta-analysis. Int. J. Ment. Health Syst. 2022, 16, 31. [Google Scholar] [CrossRef]
- Kliegman, R.M.; St. Geme, J.W.; Blum, N.J.; Shah, S.S.; Tasker, R.C.; Wilson, K.M. Nelson Textbook of Pediatrics, 21st ed.; Elsevier: Philadelphia, PA, USA, 2020. [Google Scholar]
- Balon, R.; Starcevic, V. Role of benzodiazepines in anxiety disorders. Adv. Exp. Med. Biol. 2020, 1191, 367–388. [Google Scholar] [CrossRef]
- Toussaint, L.; Nguyen, Q.A.; Roettger, C.; Dixon, K.; Offenbächer, M.; Kohls, N.; Hirsch, J.; Sirois, F. Effectiveness of progressive muscle relaxation, deep breathing, and guided imagery in promoting psychological and physiological states of relaxation. Evid. Based Complement. Alternat. Med. 2021, 2021, 5924040. [Google Scholar] [CrossRef]
- Aalami, M.; Jafarnejad, F.; ModarresGharavi, M. The effects of progressive muscular relaxation and breathing control technique on blood pressure during pregnancy. Iran J. Nurs. Midwifery Res. 2016, 21, 331–336. [Google Scholar] [CrossRef] [PubMed]
- Bentley, T.G.K.; D’Andrea-Penna, G.; Rakic, M.; Arce, N.; LaFaille, M.; Berman, R.; Cooley, K.; Sprimont, P. Breathing practices for stress and anxiety reduction: Conceptual framework of implementation guidelines based on a systematic review of the published literature. Brain Sci. 2023, 13, 1612. [Google Scholar] [CrossRef]
- Griffin, J.B. Psychological disturbances of vegetative function. In Clinical Methods: The History, Physical, and Laboratory Examinations, 3rd ed.; Walker, H.K., Hall, W.D., Hurst, J.W., Eds.; Butterworths: Boston, MA, USA, 1990; Chapter 205. Available online: https://www.ncbi.nlm.nih.gov/books/NBK318/ (accessed on 24 March 2024).
- Peretz, B.; Gluck, G.M. Assessing an Active Distracting Technique for Local Anesthetic Injection in Pediatric Dental Patients: Repeated Deep Breathing and Blowing Out Air. J. Clin. Pediatr. Dent. 1999, 24, 5–8. Available online: https://pubmed.ncbi.nlm.nih.gov/10709535/ (accessed on 24 March 2024). [PubMed]
- Levi, M.; Bossù, M.; Luzzi, V.; Semprini, F.; Salaris, A.; Ottaviani, C.; Violani, C.; Polimeni, A. Breathing out dental fear: A feasibility crossover study on the effectiveness of diaphragmatic breathing in children sitting on the dentist’s chair. Int. J. Paediatr. Dent. 2022, 32, 801–811. [Google Scholar] [CrossRef] [PubMed]
- Svensson, L.; Hakeberg, M.; Wide, U. Evaluating the Validity of the Index of Dental Anxiety and Fear (IDAF-4C+) in Adults with Severe Dental Anxiety. Eur. J. Oral Sci. 2020, 128, 423–428. [Google Scholar] [CrossRef] [PubMed]
- Armencia, A.O.; Bamboi, I.; Toader, B.; Rapis, A.; Nicolau, A.; Balcos, C.; Edlibi Al Hage, W.; Panaite, T. A Cross-Sectional Study on the Impact of Dental Fear and Anxiety on the Quality of Life of Romanian Dental Students. Medicina 2025, 61, 688. [Google Scholar] [CrossRef]
- Done, A.E.; Preoteasa, E.; Preoteasa, C.T. Psychometric Assessment of the Romanian Version of the Index of Dental Anxiety and Fear (IDAF-4C+). Healthcare 2023, 11, 2129. [Google Scholar] [CrossRef]
- Tavakol, M.; Dennick, R. Making Sense of Cronbach’s Alpha. Int. J. Med. Educ. 2011, 2, 53–55. [Google Scholar] [CrossRef] [PubMed]
- Faul, F.; Erdfelder, E.; Buchner, A.; Lang, A.G. Statistical power analyses using G*Power 3.1: Tests for correlation and regression analyses. Behav. Res. Methods. 2009, 41, 1149–1160. [Google Scholar] [CrossRef]
- Yeung, A.W.K. A Bibliometric Analysis on the Early Works of Dental Anxiety. Dent. J. 2023, 11, 36. [Google Scholar] [CrossRef]
- Eric, J.; Davidovic, B.; Mladenovic, R.; Milosavljevic, M.; Miljevic, I.D.; Bjelovic, L.; Jankovic, S.; Dolic, O.; Davidovic, B. Prevalence of Dental Fear and Its Association with Oral Health Status Among School Children in Bosnia and Herzegovina: A Cross-Sectional Study. Medicina 2025, 61, 55. [Google Scholar] [CrossRef] [PubMed]
- Sabherwal, P.; Kalra, N.; Tyagi, R.; Khatri, A.; Srivastava, S. Hypnosis and progressive muscle relaxation for anxiolysis and pain control during extraction procedure in 8–12-year-old children: A randomized control trial. Eur. Arch. Paediatr. Dent. 2021, 22, 823–832. [Google Scholar] [CrossRef]
- Mustafa, M.S.; Shafique, M.A.; Zaidi, S.D.E.Z.; Qamber, A.; Rangwala, B.S.; Ahmed, A.; Zaidi, S.M.F.; Rangwala, H.S.; Uddin, M.M.N.; Ali, M.; et al. Preoperative anxiety management in pediatric patients: A systemic review and meta-analysis of randomized controlled trials on the efficacy of distraction techniques. Front. Pediatr. 2024, 12, 1353508. [Google Scholar] [CrossRef]
- Chen, J.; Deng, K.; Yu, D.; Fan, C.; Liu, L.; Gu, H.; Huang, F.; Huo, Y. Recent Developments in the Non-Pharmacological Management of Children’s Behavior Based on Distraction Techniques: A Concise Review. Healthcare 2024, 12, 1940. [Google Scholar] [CrossRef] [PubMed]
- AlAzmah, A.; Sharanesha, R.B.; Abushanan, A.; Khojah, A.B.; Dhaafi, A.A.; Almakenzi, A.A.; Alqarni, A.S.; Alagla, M.; Al Ghwainem, A.; Alghamdi, S. Comparison of parental and children’s dental anxiety levels using the Modified Dental Anxiety Scale and Modified Short State-Trait Anxiety Inventory (EMOJI) Scale. Children 2024, 11, 1532. [Google Scholar] [CrossRef]
- Alsakr, A.; Gufran, K.; Alqahtani, A.S.; Alkharaan, H.; Abushanan, A.; Alnufaiy, B.; Alkhaldi, A.; Alshammari, T.; Alanazi, M. Pre-Treatment and Post-Treatment Dental Anxiety in Patients Visiting Intern Dental Clinic. Medicina 2023, 59, 1284. [Google Scholar] [CrossRef] [PubMed]
- Bucur, S.-M.; Moraru, A.; Adamovits, B.; Bud, E.S.; Olteanu, C.D.; Vaida, L.L. Psychometric Properties of Scared-C Scale in a Romanian Community Sample and Its Future Utility for Dental Practice. Children 2022, 9, 34. [Google Scholar] [CrossRef]
- Rath, S.; Das, D.; Sahoo, S.K.; Raj, A.; Guddala, N.R.; Rathee, G. Childhood dental fear in children aged 7–11 years old by using the Children’s Fear Survey Schedule-Dental Subscale. J. Med. Life 2021, 14, 45–49. [Google Scholar] [CrossRef]
- Winkler, C.H.; Bjelopavlovic, M.; Lehmann, K.M.; Petrowski, K.; Irmscher, L.; Berth, H. Impact of Dental Anxiety on Dental Care Routine and Oral-Health-Related Quality of Life in a German Adult Population—A Cross-Sectional Study. J. Clin. Med. 2023, 12, 5291. [Google Scholar] [CrossRef] [PubMed]
- Santos-Puerta, N.; Peñacoba-Puente, C. The role of dental fear, pain anticipation and self-efficacy in endodontic therapy. Community Dent. Health 2023, 40, 85–91. [Google Scholar] [CrossRef]
- Taheri, A.A.; Parvizifard, A.A.; Reisi, S.; Jafari, M.; Mohammadian, Y.; Heshmati, K.; Foroughi, A.; Eivazi, M.; Ghasemi, M. Associations between the Perception of Dental Pain and Pain Anxiety, Mental Pain, and Dental Anxiety in Iranian Sample. Int. J. Psychiatry Med. 2024, 59, 34–49. [Google Scholar] [CrossRef]
- Mehrabkhani, M.; Khanmohammdi, R.; Nematollahi, H.; Rajabi, N.; Gheidari, A. Influence of Temperament on Children’s Cooperation during Dental Treatment. Dent. Res. J. 2024, 21, 45. [Google Scholar] [CrossRef] [PubMed]
- Janeshin, A.; Habibi, M. The Relationship between Temperament and Behavior in 3–7-Year-Old Children during Dental Treatment. Dent. Res. J. 2021, 18, 12. [Google Scholar] [CrossRef] [PubMed]
- Ho, J.C.-Y.; Chai, H.H.; Lo, E.C.-M.; Huang, M.-Z.; Chu, C.-H. Strategies for effective dentist–patient communication: A literature review. Patient Prefer. Adherence 2024, 18, 1385–1394. [Google Scholar] [CrossRef] [PubMed]
- Al Homoud, R.A.; Alshellatie, A.K.; Alzumaie, A.S.; Al-Bayati, S.A. Behavior and anxiety levels in pediatric patients: The behavioral changes and anxiety of pediatric patients in dental clinics. Clin. Exp. Dent. Res. 2023, 9, 1223–1231. [Google Scholar] [CrossRef] [PubMed]
- Kvesić, A.J.; Hrelja, M.; Lovrić, Ž.; Šimunović, L.; Špiljak, B.; Supina, N.; Vranić, L.; Vranić, D.N. Possible risk factors for dental fear and anxiety in children who suffered traumatic dental injury. Dent. J. 2023, 11, 190. [Google Scholar] [CrossRef]
- Esian, D.; Bica, C.; Vlasa, A.; Bud, E.; Stepco, E.; Bud, A.; Beresescu, L. Retrospective Study Regarding the Correlation between Dental Anxiety and Color Preferences in Children with Severe Early Childhood Caries. Dent. J. 2024, 12, 155. [Google Scholar] [CrossRef]
- Bayón, G.; Stiernhufvud, F.; Ribas-Pérez, D.; Biedma Perea, M.; Mendoza Mendoza, A. Parental Anxiety Disorders and Their Impact on Dental Treatment in Children Aged 4 to 13 Years: A Cross-Sectional Observational Study. J. Clin. Med. 2025, 14, 1869. [Google Scholar] [CrossRef] [PubMed]
- Fux-Noy, A.; Zohar, M.; Herzog, K.; Shmueli, A.; Halperson, E.; Moskovitz, M.; Ram, D. The effect of the waiting room’s environment on the level of anxiety experienced by children prior to dental treatment: A case-control study. BMC Oral Health 2019, 19, 294. [Google Scholar] [CrossRef]
- Kohli, N.; Hugar, S.M.; Soneta, S.P.; Saxena, N.; Kadam, K.S.; Gokhale, N. Psychological behavior management techniques to alleviate dental fear and anxiety in 4–14-year-old children in pediatric dentistry: A systematic review and meta-analysis. Dent. Res. J. 2022, 19, 47. [Google Scholar]
- Cristea, R.A.; Ganea, M.; Potra Cicalău, G.I.; Ciavoi, G. Dentophobia and the Interaction Between Child Patients and Dentists: Anxiety Triggers in the Dental Office. Healthcare 2025, 13, 1021. [Google Scholar] [CrossRef]
- Ehizele, A.O.; Ayamolowo, L.B.; Ishola, A.; Foláyan, M.O. Culture and Behaviour Management of Children in the Dental Clinic: A Scoping Review. Dent. J. 2025, 13, 186. [Google Scholar] [CrossRef]
- Bani-Hani, T.; Al-Fodeh, R.; Tabnjh, A.; Leith, R. The use of local anesthesia in pediatric dentistry: A survey of specialists’ current practices in children and attitudes in relation to articaine. Int. J. Dent. 2024, 2024, 2468502. [Google Scholar] [CrossRef]
- Caleza-Jiménez, C.; López-de Francisco, M.D.M.; Mendoza-Mendoza, A.; Ribas-Pérez, D. Relationship between children’s lifestyle and fear during dental visits: A cross-sectional study. Children 2022, 10, 26. [Google Scholar] [CrossRef] [PubMed]

| Age | Systolic BP (mm Hg) | Diastolic BP (mm Hg) | Status |
|---|---|---|---|
| 10 years | 102 ± 11 | 64 ± 10 | Normal |
| 13 years | 108 ± 13 | 66 ± 11 | Normal |
| 16 years | 115 ± 12 | 67 ± 11 | Normal |
| Age (Years) | Sex | Mean HR (Beats/Min) | Normal Range (Beats/Min) |
|---|---|---|---|
| 10 | Girls and Boys | 90 | 70–110 |
| 12 | Girls | 90 | 70–110 |
| 12 | Boys | 85 | 65–105 |
| 14 | Girls | 85 | 65–105 |
| 14 | Boys | 80 | 60–100 |
| 16 | Girls | 80 | 60–100 |
| 16 | Boys | 75 | 55–95 |
| 18 | Girls | 75 | 55–95 |
| 18 | Boys | 70 | 50–90 |
| Variable | Group A (BC) | Group B (JPMR) | Control | p-Value |
|---|---|---|---|---|
| Age (years, mean ± SD) | 12.4 ± 2.5 | 12.6 ± 2.4 | 12.5 ± 2.6 | 0.88 |
| Gender (M/F) | 34/29 | 32/31 | 33/30 | 0.94 |
| Baseline IDAF-4C+ | 3.32 ± 0.41 | 3.33 ± 0.44 | 3.31 ± 0.40 | 0.92 |
| Measure | Time | Group A (BC) | Group B (JPMR) | Control | p-Value (Within Group) |
|---|---|---|---|---|---|
| IDAF-4C+ | Pre | 3.32 ± 0.41 | 3.33 ± 0.44 | 3.31 ± 0.40 | — |
| Post | 3.02 ± 0.43 1 | 2.64 ± 0.39 2 | 3.28 ± 0.38 | <0.001 | |
| Systolic BP (mmHg) | Pre | 108.9 ± 7.8 | 109.1 ± 7.5 | 108.4 ± 8.0 | — |
| Post | 105.7 ± 7.2 1 | 102.2 ± 6.9 2 | 107.6 ± 7.9 | 0.038 | |
| Heart Rate (bpm) | Pre | 91.0 ± 9.3 | 91.5 ± 8.8 | 90.7 ± 9.1 | — |
| Post | 87.6 ± 8.6 1 | 83.1 ± 8.1 2 | 90.2 ± 9.3 | 0.041 |
| Outcome | ANOVA p-Value | Significant Post Hoc Differences | Cohen’s d (Effect Size) |
|---|---|---|---|
| IDAF-4C+ Score | <0.001 | JPMR < BC < Control | JPMR vs. Control = 1.12 |
| JPMR vs. BC = 0.70 | |||
| Systolic BP | 0.041 | JPMR < Control | JPMR vs. Control = 0.62 |
| Heart Rate | 0.053 (trend) | No significant differences | — |
| Cluster | Key Traits | n | Predominant Group |
|---|---|---|---|
| Cluster 1 | High anxiety, strong reduction with JPMR, younger, more females | 58 | JPMR |
| Cluster 2 | Moderate anxiety, partial responders | 74 | Mixed |
| Cluster 3 | Low anxiety, minimal response | 57 | Control and BC |
| y | Baseline IDAF | Post IDAF | Δ Systolic BP | Δ HR | Age Range | Gender Trend |
|---|---|---|---|---|---|---|
| Cluster 1 | 3.91 | 2.38 | –9.4 mmHg | –6.5 bpm | 8–12 years | More females |
| Cluster 2 | 2.91 | 2.54 | –3.2 mmHg | –2.4 bpm | 10–14 years | Balanced |
| Cluster 3 | 2.34 | 2.30 | –0.8 mmHg | –0.5 bpm | 13–17 years | Balanced |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Published by MDPI on behalf of the Lithuanian University of Health Sciences. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Bucur, S.M.; Crișan, I.M.; Cocoș, D.I.; Bud, E.S.; Galea, C. Observational Study on Progressive Muscle Relaxation and Breathing Control for Reducing Dental Anxiety in Children. Medicina 2025, 61, 876. https://doi.org/10.3390/medicina61050876
Bucur SM, Crișan IM, Cocoș DI, Bud ES, Galea C. Observational Study on Progressive Muscle Relaxation and Breathing Control for Reducing Dental Anxiety in Children. Medicina. 2025; 61(5):876. https://doi.org/10.3390/medicina61050876
Chicago/Turabian StyleBucur, Sorana Maria, Ioana Maria Crișan, Dorin Ioan Cocoș, Eugen Silviu Bud, and Carmen Galea. 2025. "Observational Study on Progressive Muscle Relaxation and Breathing Control for Reducing Dental Anxiety in Children" Medicina 61, no. 5: 876. https://doi.org/10.3390/medicina61050876
APA StyleBucur, S. M., Crișan, I. M., Cocoș, D. I., Bud, E. S., & Galea, C. (2025). Observational Study on Progressive Muscle Relaxation and Breathing Control for Reducing Dental Anxiety in Children. Medicina, 61(5), 876. https://doi.org/10.3390/medicina61050876






