Abstract
Background and Objectives: Total knee arthroplasty (TKA) is one of the most common medical procedures worldwide. However, 10 to 20% of patients are still dissatisfied despite implants and surgical technique advancements. Recently, several medial-stabilized TKAs have been developed in attempts to replicate the native kinematics of the knee. The aim of this scoping review on medial-stabilized TKA inserts—medial congruent (MC) and medial pivot (MP)—is to focus on their clinical outcomes and the role of the posterior cruciate ligament (PCL), aiming to systematically map the existing research and highlight current knowledge gaps. Materials and Methods: A search of the PubMed, Embase and Cochrane databases was performed to identify relevant studies on the kinematics and outcomes of medial pivot (MP) or medial congruent (MC) inserts. The following Mesh terms were used in combination with the Boolean operators “AND” and “OR”: “total knee arthroplasty”, “total knee replacement”, “medial pivot”, “medial congruence”, “outcomes” and “kinematic”. Original studies reporting on clinical outcomes assessed with validated patient-reported scales, surgical techniques and reoperation rates for any reason with a minimum follow-up of 18 months were included. Results: A total of 39 articles met the inclusion criteria, accounting for 6143 total knee replacements. The overall reoperation-free survivorship rate was 98.4% (6047 out of 6143 knees) at a weighted average follow-up of 6.3 years (range 1.5–15.2 years, SD 0.7). Both MP and MC inserts demonstrated good outcomes, with no differences between groups. Few studies evaluated the role of the PCL in MP and MC inserts, with no differences in terms of clinical outcomes between retaining and sacrificing the PCL. Conclusions: MS-TKA demonstrated good outcomes in the literature independently of the specific design (medial pivot or medial congruent). Different possible biases may be present when evaluating the outcomes of these inserts, including different types of alignment and soft tissue balancing philosophies.
1. Introduction
Total knee arthroplasty (TKA) is a widely performed procedure for treating end-stage knee osteoarthritis [1]. However, up to 20% of patients are dissatisfied due to persistent pain, instability or unnatural knee motion [2]. Different factors may be related to this dissatisfaction rate, including the surgical technique, the type of implant and the post-operative protocol. To improve the rate of satisfied patients, surgeons may “personalize” TKA either through the surgical technique, by choosing new alignment philosophies, or the implant, by choosing new bearings. Different studies have confirmed that normal knee kinematics follow a “medial pivot” concept, with the medial compartment being relatively “fixed” and the lateral compartment performing a physiological combination of rolling back and translational movements during flexion [3,4]. For this reason, medially conforming inserts have recently been introduced with the goal of recreating “medial pivot” kinematics [5]. Particularly, two bearings with slightly different kinematics can be distinguished. In the so-called “medial pivot” design (MP), the insert has a peculiar shape which includes a concave medial compartment providing a large contact surface, and a flatter lateral surface facilitating the femoral rollback. MP bearing is usually associated with a single-radius femoral component (SR) that closely reproduces a true ball-and-socket mechanism [6,7]. Conversely, the “medial congruent” insert (MC) is highly congruent on the medial side with a more posterior dwell point, resulting in a good reproduction of the knee kinematics. This type of insert is associated with a J-curve or multi-radius femoral condyle (MR). Both MP and MC inserts have demonstrated similar biomechanical properties, even though they have slightly different designs. Particularly, in MP inserts, tibial rotation close to the native knee has been demonstrated, in association with good AP stability and more natural joint kinematics [8,9]. Furthermore, medial-stabilized implants, in comparison to the UC design, demonstrated similar total tibio-femoral contact forces over the whole knee flexion movement but with a more favorable relative contact pressure distribution and lower peak contact pressures in the MP design, which may suggest a lower rate of wear and potentially enhances implant’s longevity [9]. Similarly, the MC design demonstrated good tibial external rotation in maximum extension, confirming the restoration of the screw-home mechanism with good anteroposterior stability and the avoidance of mid-flexion instability [10]. Figure 1 summarizes the different insert characteristics.
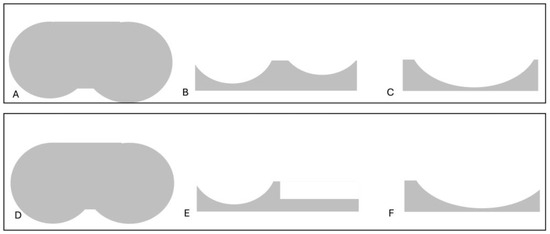
Figure 1.
In the upper part of the figure, an MC insert is shown: (A) Axial view demonstrating the anatomic asymmetric shape of the tibial plateau with a larger medial surface. (B) AP view demonstrating a more concave medial surface for a more constrained medial compartment compared to the lateral one. (C) Lateral view showing the deep anterior and posterior lips to achieve AP stability. In the lower part of the figure, an MP insert is shown. (D) Axial view demonstrating the symmetric shape of the tibial plateau. (E) AP view demonstrating a more concave medial surface and a flat lateral one, reproducing the “medial pivot” kinematics of the knee. (F) Lateral view showing the deep anterior lip to achieve AP stability.
Good survivorship has been demonstrated in both MP and MC implants [11,12], with similar or better clinical outcomes and patient satisfaction compared to posterior stabilized TKA at short-term follow-up [13,14,15,16,17]. Furthermore, both an MP and an MC insert can be implanted while sacrificing or respecting the posterior cruciate ligament (PCL), with conflicting results reported in the literature [18,19,20,21,22,23].
The aim of this scoping review is to summarize the available literature on these two closely related MS-TKA inserts, highlighting their differences in terms of outcomes. Furthermore, an analysis of the differences between respecting or sacrificing the PCL with these inserts will also be performed.
2. Materials and Methods
2.1. Literature Search
Extensive research in PubMed, Embase and Cochrane databases was performed to identify relevant studies on kinematics and outcomes of medial pivot (MP) or medial congruent (MC) inserts. The articles in this study included all English-written papers published up to December 2024. The following Mesh terms have been used in combination with Boolean operators “AND” and “OR”: “total knee arthroplasty”, “total knee replacement”, “medial pivot”, “medial congruence”, “outcomes” and “kinematic”. The search yielded 369 results. The papers that met inclusion criteria were original studies, describing outcomes of medial-stabilized (MS) implants (either MP or MC) in primary total knee arthroplasty (TKA), in which there was a description of the surgical technique and re-operation rate for any reason, with a minimum follow-up of 18 months. Case reports, review articles, expert opinions, letters to editors, biomechanical studies, investigations involving animals, cadaver studies, in vitro research, book chapters as well as studies published in a language other than English were excluded. Titles and abstracts were screened by two authors (F.R. and F.R. blinded for review) to identify the included studies [6,7,14,15,16,17,18,19,20,21,22,23,24,25,26,27,28,29,30,31,32,33,34,35,36,37,38,39,40,41,42,43,44,45,46,47,48,49,50]. Disagreements on study selection were resolved by discussion with a third reviewer (F.P.) when necessary.
Different data were collected for every article, including the year of publication, level of evidence of the study, number of patients, length of follow-up, number of patients dead or lost to follow-up, diagnosis, age, Body Mass Index (BMI), sex, implant system and features, surgical technique (posterior cruciate ligament resected or preserved, patella resurfaced or not, alignment), re-operation for any reason and patient-reported outcomes. Data from each eligible article was independently collected by two reviewers (F.R. and F.R., blinded for review). Any disagreements were addressed by consultation with a third reviewer (F.P.). All study data were collected using Microsoft Excel (Microsoft Corp., Redmond, WA, USA). Table 1 summarizes the evaluated studies.

Table 1.
Summary of the studies.
After an initial overall analysis of MS-TKA outcomes, a detailed evaluation of MP or MC outcomes was performed, as well as a subgroup analysis evaluating the differences between PCL-retained and PCL-scarified implants.
2.2. Statistical Analysis
Categorical variables are presented as percentages. Continuous variables are presented as means, weighted by sample size, with the range between minimum and maximum values and the standard deviation.
3. Results
3.1. Study Selection
The selection process is illustrated in Figure 2. The literature search yielded a total of 369 references. After removing duplicate papers and applying inclusion and exclusion criteria, 72 articles were assessed for eligibility. After full-text evaluation, 39 studies were included in this scoping review [6,7,14,15,16,17,18,19,20,21,22,23,24,25,26,27,28,29,30,31,32,33,34,35,36,37,38,39,40,41,42,43,44,45,46,47,48,49,50].
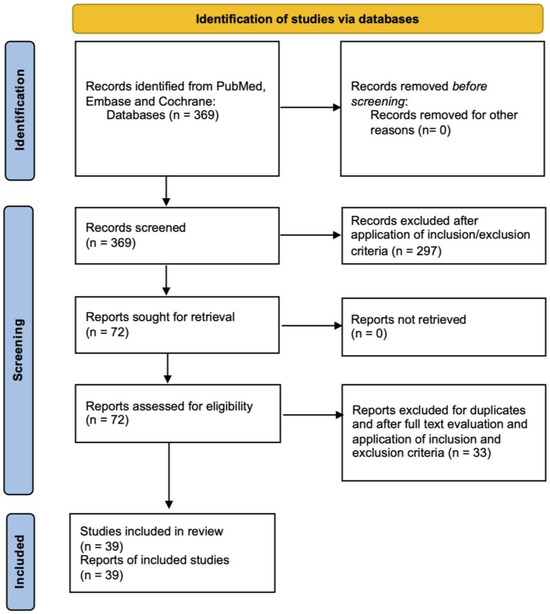
Figure 2.
PRISMA diagram.
3.2. Demographic Data
A total of 697 total knee replacements in 5887 patients were performed in the 39 evaluated studies. Accounting for patients lost to follow-up, the final analysis included 6143 medial stabilized total knee arthroplasties (MS-TKAs). The weighted average age was 69.9 years (range 55–78 years, SD 3.3) and the weighted average BMI was 28 kg/m2 (range 23.4–34.6, SD 1.2), with 66.1% of female patients. Indication for TKA was knee osteoarthritis in 94.6% of patients, rheumatoid arthritis in 4.6% and 0.8% were indicated for other reasons, such as osteonecrosis. The average follow-up was 6.3 years (range 1.5–15.2 years, SD 0.7). There were 80.2% of medial pivot implants (n = 4965) and 19.2% of medial congruent implants (n = 1178). The different types of implants utilized are summarized in Table 2.

Table 2.
Implants used in the different studies.
In twenty-three studies, TKA was implanted with a mechanical alignment, either with gap balancing or measured resection techniques [6,7,15,16,17,19,20,21,22,24,25,27,28,31,32,34,37,39,41,43,44,48,50]. In three studies, kinematic alignment philosophy was used [14,23,49]. One randomized controlled trial specifically compared the clinical outcomes of mechanically versus kinematically aligned MP- TKA [47]. One prospective observational study described a functional alignment with a “ligament-driven” technique [18]. Different alignments are summarized in Table 3.

Table 3.
Summary of alignments.
3.3. General Outcomes
Thirty-three studies [6,7,14,15,16,17,19,20,21,22,23,24,25,26,27,28,30,32,33,34,35,36,38,39,40,41,42,43,44,45,46,48,50] reported on the range of motion of 5447 TKAs, with a weighted average of 115.2° (range 104°–132.1°, SD 5.8). In thirty-two studies (5202 TKAs) [6,7,14,17,19,21,22,23,24,25,26,27,29,30,32,33,34,35,36,37,38,40,41,42,43,44,45,46,47,48,49,50] the Knee Society Knee Score was used to evaluate the clinical outcomes, in twenty-six studies (4305 TKAs) [6,7,17,19,21,23,24,26,30,32,33,34,35,36,37,38,41,42,43,44,45,46,47,48,49,50] the functional Knee Society Score was used, in eleven studies (1601 TKAs) [6,7,15,17,18,20,24,38,45,47,50] the Oxford Knee Score and in fourteen studies (3102 TKAs) [21,24,28,31,32,36,37,38,42,43,45,47,48,49] the Western Ontario and McMaster University (WOMAC) score were used. The post-operative Forgotten Joint Score was used only in sixteen studies for 3322 TKAs [7,14,16,18,20,21,22,23,24,27,36,39,41,46,47,48]. A significant improvement from pre-operative to post-operative scores was demonstrated in all studies. Average scores are reported in Table 4 and Table 5.

Table 4.
Clinical outcome average scores. Comparison between medial pivot and medial congruent.

Table 5.
Clinical outcome average scores. Comparison between alignment options.
3.4. Reoperation
The overall reoperation-free survivorship rate was 98.4% (6047 out of 6143 knees) at a weighted average follow-up of 6.3 years (range 1.5–15.2 years, SD 0.7), excluding patients who were deceased for reasons unrelated to surgery or lost to follow-up. The overall reintervention rate was 1.6%, mainly due to periprosthetic fractures (0.4%), aseptic loosening (0.2%) and infections (0.7%). The average reintervention rate was 1.3% (range 0–5.8%, SD 1.5).
3.5. Medial Pivot
A medial pivot implant was evaluated in thirty studies [6,7,14,15,16,17,19,21,29,30,31,32,33,34,35,36,37,38,39,40,41,42,43,44,45,46,47,48,49,50], for a total of 4965 MP-TKAs, representing 80.8% of the total sample. The average follow-up was 6.8 years (range 2–15.2, SD 0.7). Table 6 summarizes these studies.

Table 6.
Summary of medial pivot studies.
The medial pivot TKA was designed to replicate the kinematics of the natural knee joint, trying to enhance patient comfort and satisfaction while providing a more “natural” knee kinematics [5,8,9]. A key aspect of the MP implant is the asymmetry between its medial and lateral compartments. The medial compartment features high congruence and a large contact surface, contributing to stability and pivoting kinematics. In contrast, the lateral compartment has a flat surface allowing a sliding motion of the lateral femoral condyle while enabling tibial internal rotation and femoral external rotation during knee flexion. Anteroposterior stability is provided by the anterior and posterior lips, which act as replacements for the anterior and posterior cruciate ligaments, respectively, justifying the term “medially stabilized implants.” This type of insert is usually associated with a single-radius femoral component, creating the so-called “ball-in-socket” mechanism. This association between MP insert and single radius femoral component effectively prevents anterior femoral sliding, known as paradoxical movement, which is often observed in conventional multi-radius implants based on the four-bar link theory [8,9]. Figure 3 shows a medial pivot implant.
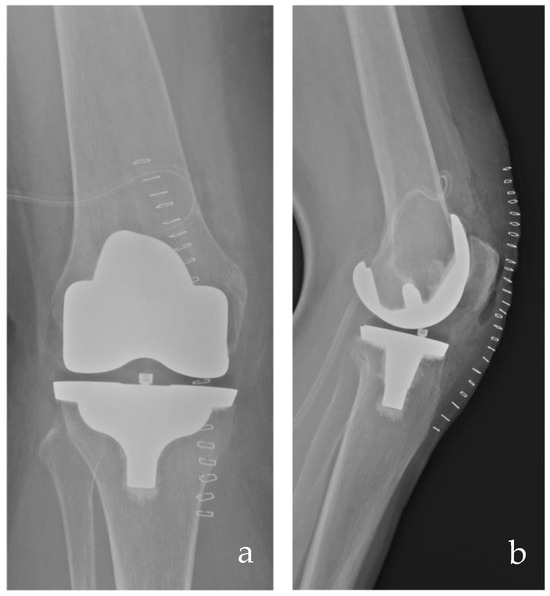
Figure 3.
Post-operative anteroposterior (a) and lateral (b) radiographs of a medial pivot TKA from the senior author’s case series.
General outcomes of medial pivot TKA have been evaluated in nineteen retrospective studies [6,7,19,21,31,32,33,35,36,38,39,40,41,42,44,46,48,49,50], with a total of 3736 TKAs. These studies described good outcomes at a weighted average follow-up of 6.3 years (range 2–13.4, SD 0.6) (Table 5). Xiang et al. evaluated more than 1100 patients, the largest case series published, with good to excellent clinical outcomes and a mid-term cumulative survival rate of 99.2% (95% CI, 99.6–98.4%). Karachalios et al. have reported the longest follow-up among retrospective observational studies, with a success rate of 97.3% (95% CI 96.7 to 97.9) at 15 years with revision for any reason as the end point. One study specifically investigates the results of the medial pivot TKA in patients affected by rheumatoid arthritis [50], with satisfactory clinical outcomes at a minimum follow-up of three years. In two studies, a medial pivot implant was compared with a rotating-platform mobile-bearing implant [32,48] with no differences in clinical outcomes, even though the findings of Shakya et al. described better FJS and functional KSS for medial pivot implants at a 7.1-year average follow-up.
Outcomes of medial pivot implants compared to other types of inserts were evaluated in six randomized controlled trials. Particularly, four studies compared an MP-TKA with a posterior stabilized TKA (PS-TKA) [14,15,16,17], one study compared the results of medial pivot implants implanted with mechanical or a kinematic alignment [47] and one study evaluated the outcomes of medial pivot compared to a cruciate-retaining (CR) rotating platform [43]. Batra et al. reported increased KSS-Satisfaction and Expectation scores at the four-year follow-up for MP-TKAs compared to PS-TKAs. In the study by Chang et al., no significant differences in outcomes were observed at the two-year follow-up between MP or PS implants in association with a single radius femoral component. Furthermore, Kulshrestha et al. demonstrated significantly better performance at the Direct Observation of Procedural Skills (DOPSs) in patients with an MP insert compared to those with PS implants. Ettinger et al. reported that MP-TKA associated with kinematic alignment had a superior joint awareness score (Forgotten Joint Score) as well as higher expectation and satisfaction at 1-year and 2-year follow-up compared to those implanted with a mechanical philosophy, especially in cases of varus morphotype. Conversely, Kim et al. reported superior clinical results with a CR mobile bearing implant compared to an MP-TKA with a minimum 11-year follow-up.
Five prospective observational studies described the clinical outcomes of medial pivot TKA [29,30,34,37,45]. Macheras et al. reported on the longest follow available in the literature (15.2-years average follow-up, range 15–17 years) with a cumulative survivorship of 98.8% (95% confidence interval: 97.6–100%) at 17 years. During the follow-up period, four cases (1%) required revision: three for persisting anterior knee pain (requiring patella resurfacing) and one case for a periprosthetic tibial fracture.
Two studies focused on the comparison between medial pivot TKA with a medial congruent TKA [6,7], with no statistically significant differences in short-term clinical outcomes at the two-year follow-up. However, the authors demonstrated that J-curved implants had a greater post-operative range of motion (ROM). Additionally, Vecchini et al. described a higher Forgotten Joint Score in patients with medial pivot (MP) implants compared to medial congruent (MC) ones.
3.6. Medial Congruent
A medial congruent bearing was evaluated in eleven studies [6,7,18,20,22,23,24,25,26,27,28] with 1178 MC-TKAs (19.2% of the total sample) at a weighted average follow-up of 3.8 years (range 1.5–6, SD 0.3).
Medial congruent inserts have been recently introduced with a design mainly based on the kinematics of ultracongruent (UC) implants. They are usually characterized by a highly congruent medial side, with a more posterior dwell point, allowing the femoral roll back, and an anterior and posterior lip for anteroposterior stability. These inserts are usually associated with the cruciate-retaining J-curved femoral component, and they were initially designed for both retaining or sacrificing the posterior cruciate ligament. Figure 4 shows an X-ray of an MC-TKA.
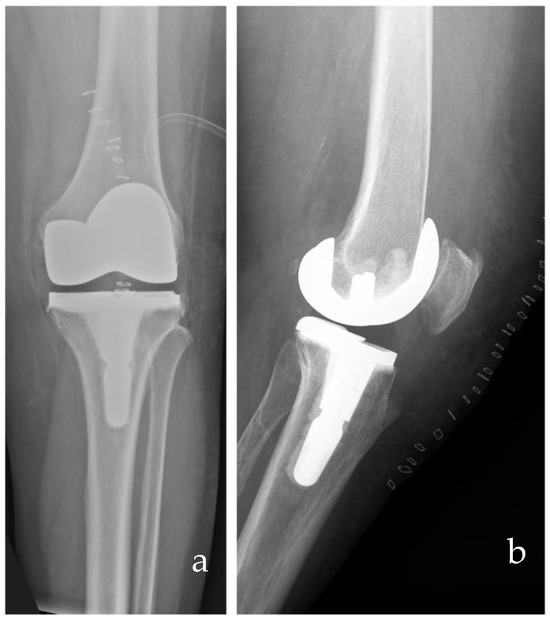
Figure 4.
Post-operative anteroposterior (a) and lateral (b) radiographs of a medial congruent TKA from the senior author’s case series.
Faschingbauer et al., in their cadaveric study on one of these implants (Persona® Zimmer Biomet, Warsaw, IN, USA), compared the kinematics of ultracongruent (UC), cruciate-retaining (CR) and medial congruent (MC) inserts. In this study, the MC insert demonstrated the least degree of femoral rollback, tibio-femoral rotation and single bony rotations, exhibiting a pronounced paradoxical roll forward, but still showing a greater degree of constraint than the UC and CR inserts [53].
Two randomized clinical trials have been conducted with MC-TKA [20,26]. Nishitani et al. have evaluated the same J-curved implant with two different inserts, one asymmetrical (MC) and one symmetrical, and reported no significant differences in clinical outcomes or post-operative ROM at the two-year follow-up.
Furthermore, seven retrospective studies have investigated the overall outcomes of MC-TKAs [6,7,23,24,25,27,28]. Among these studies, two studies previously mentioned [6,7] compared the outcomes of MP and MC bearings while two studies have analyzed the clinical outcomes of MC-TKAs in valgus knee osteoarthritis (OA) [27,28], with favorable results at short-term follow-up. Only one retrospective observational study evaluated the clinical outcomes of an MC-TKA implanted with a kinematic alignment philosophy, with good results [23]. Table 7 summarizes the outcomes of these studies.

Table 7.
Summary of medial congruent studies.
3.7. The Role of Posterior Cruciate Ligament
Even if the MS-TKA has been designed to overcome the stabilizing role of the PCL, surgeons can decide to either preserve or sacrifice the posterior cruciate ligament. However, the literature lacks standardized guidelines supporting an evidence-based decision. In the evaluated papers, three retrospective studies compare MP-TKA with or without the PCL [19,21,23], with no differences in clinical outcomes between the two groups. In the RCT by Budhiparama et al. [20], the MC-TKA with or without PCL preservation was compared in simultaneous bilateral TKA, with no significant differences in range of motion or clinical outcomes at two-year follow-up. The clinical outcomes and survival rates of a medial congruent TKA with or without PCL were compared in two prospective observational studies [18,22]. Rossi et al. analyzed the outcomes of 165 TKRs divided into two groups: PCL-preserved and PCL-sacrificed implants. Each group underwent the same surgical technique, performed by a single surgeon, with a slight reduction in the tibial slope in the PCL-sacrificing group in order to balance the flexion gap. The results showed no significant differences in clinical outcomes at mid-term follow-up. Instead, Rajgopal et al. compared 60 simultaneous bilateral MC-TKA with or without the PCL, reproducing in all knees the native tibial slope. Their findings indicated that the PCL-sacrificed group had a greater post-operative ROM, while the PCL-preserved group had a higher Knee Society Score (KSS) at an 18-month follow-up.
In medial stabilized implants, preservation of the PCL may result in more physiological knee kinematics [18,19,20,21,22,23]. However, the excision of the PCL, with a consequent increase in flexion gap may be correlated with a greater range of motion, as evidenced by Rajgopal et al. While the effects of PCL on the flexion gap are more straightforward and can be assessed intraoperatively with tests such as the anterior lift-off, determining the influence of PCL on knee biomechanics is difficult. Nedopil et al. suggested that the PCL plays a critical role in driving tibial internal rotation: its tension facilitates internal rotation of the tibia during knee flexion, which subsequently reduces the Q-angle optimizing the extensor mechanism [54]. On the other hand, Moewis et al. [55] showed that the retention of PCL alone is insufficient to reduce the anterior translation of the femur in the early knee flexion and to reproduce the lateral femoral roll-back. Howell et al. [56] have underlined that a PCL-retaining technique combined with kinematic alignment should be utilized even in cases of valgus deformity, where the PCL is tight compared to neutral or varus-aligned knees. However, Indelli et al. [27] reported good clinical outcomes in valgus knee OA treated with an MC-TKA performing a posterior capsular release in 72% of the cases, without recording any case of post-operative instability.
4. Discussion
Medial stabilized implants are designed to mimic native knee kinematics while preventing the paradoxical anterior sliding of the femoral condyles in TKA, following the findings by Freeman and Pinskerova [3,4] that first described the pivot mechanism in non-arthritic knees. Various manufacturers have developed their own implants based on this philosophy to ideally enhance patient satisfaction, eliminate residual pain and fulfill patients’ pre-operative expectations. Consequently, research about medial stabilized total knee arthroplasty is expanding, with different papers being published in recent years. However, there is some confusion between the different types of insert (medial congruent or medial pivot) and the different types of femoral components (ball-in-socket or J-curve). The primary aim of this scoping review was to comprehensively analyze different studies, focusing on the differences between medial pivot and medial congruent inserts, including clinical outcomes and also considering other variables related to surgical technique, such as alignment and soft tissue balancing philosophies.
A total of 39 primary studies were included in this scoping review. There are numerous studies supporting good clinical results of medial pivot TKA. On the other hand, the literature on medial congruent TKA is less extensive, but it similarly shows good results. There are few studies confirming the long-term survivorship of medial pivot implants [33,37,38,43,45,46], while only mid-term studies have been conducted on medial congruent TKA’s [18,24] and further research is needed to assess long-term outcomes and survival rates. Medial congruent implants have been developed more recently, which may contribute to the limited number of studies available. Few studies directly compare MP and MC inserts, reporting no significant differences in clinical outcomes [6,7]. However, in most studies, not only different inserts but also different alignment philosophies are described (Table 1 and Table 3), with possible biases. Surgeons should be aware that MP and MC inserts have different biomechanical characteristics, which may yield similar kinematics and consequently, similar outcomes, even if different alignment philosophies are adopted. A limited number of studies analyzed the outcomes of kinematic alignment in association with medial stabilized TKA [14,23,47,49], highlighting another lack of evidence in the literature. The randomized trial conducted by Ettinger et al. concluded that patients undergoing MP TKA with restricted kinematic alignment may report improved joint awareness (FJS) and higher satisfaction levels (KSS satisfaction and expectation scores) compared to MP TKA associated with mechanical alignment at short-term follow-up. The authors suggested that integrating the two aforementioned techniques, developed in order to reproduce the native knee kinematics—rKA, which emphasizes the preservation of soft tissues, and the MP implant that ideally maintains pivot kinematics—may lead to better clinical outcomes.
The choice between MP and MC bearings cannot be evidence-based due to a lack of strong clinical evidence, but it is still up to the surgeon’s preference, similar to the opportunity to sacrifice or retain the PCL with the same bearing surfaces. The role of the posterior cruciate ligament in MP or MC inserts remains debated. Current studies agree that retaining the PCL is unnecessary with a medial-stabilized design, given the anterior–posterior stability achieved by the insert itself, suggesting that both preserving or sacrificing the PCL can be effective and, again, a surgeon’s preference [18,19,20,21,22,23]. However, if the PCL is sacrificed, tibial slope correction should be performed to balance the flexion gap. Only Rajgopal et al. reported significant differences between the PCL-retained and PCL-sacrificed groups, demonstrating higher KSS-2011 and FJS-12 and a gait pattern closer to normal at short-term follow-up in the retained group. Similarly, Budhiparama et al. concluded that retaining the PCL favors the tibia’s internal rotation during flexion, which optimizes patellofemoral tracking, though this results in a tighter flexion gap. Hu et al. concluded that preserving the PCL can be beneficial in cases where the extension and flexion gaps are balanced, as this can enhance patient proprioception; additionally, the authors suggested preferring a slight varus alignment to sustain medial tension and ensure knee stability.
This scoping review has some limitations. First, it only focuses on studies evaluating clinical outcomes, excluding biomechanical studies, which may offer crucial insights into the kinematics of total knee arthroplasty (TKA). Furthermore, it was not possible to directly compare the outcomes between MP and MC designs due to the different numerosity of the studies. However, MC designs have been introduced more recently than MP implants, and further studies are needed in order to reach long-term outcomes and significant clinical evidence.
5. Conclusions
Both MP and MC are effective in reproducing knee kinematics, with good outcomes. However, there is no available evidence to guide the decision-making process in sacrificing or retaining the PCL in these implants. High-quality studies (i.e., randomized trials) with long follow-ups may be necessary to better understand the role of the PCL and tibial slope in this type of insert and to evaluate their long-term survivorship.
Author Contributions
Conceptualization, F.R. (Federica Rosso) and R.R.; validation, U.C. and M.B.; formal analysis, F.R. (Francesco Romano); investigation, F.P.; resources, F.R. (Francesco Romano) and F.P.; data curation, U.C.; writing—original draft preparation, F.R. (Francesco Romano); writing—review and editing, F.R. (Federica Rosso); visualization, U.C. and M.B.; supervision, U.C. and M.B.; project administration, F.R. (Federica Rosso). All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Conflicts of Interest
F Romano: no disclosure; R Rossi: Angelini Farmaceutica—paid presenter or speaker; Arthrex, Inc—paid presenter or speaker; DePuy A Johnson & Johnson Company—paid presenter or speaker; Lima corporate—IP royalties; Zimmer—paid consultant, paid presenter or speaker and Commitee Member of Siagascot, European Knee Society, American Knee Society, AAHKS international member; U Cottino: teaching consultant Zimmer Biomet; M Bruzzone teaching consultant Depuy; F Pirato: no disclosure; F Rosso: research grant from Medacta and Commitee member of Siagascot, European Knee Society.
Abbreviations
The following abbreviations are used in this manuscript:
| TKA | total knee arthroplasty |
| MP | medial pivot |
| MC | medial congruent |
| MS | medial stabilized |
| ROM | range of motion |
| SR | single radius |
| MR | multi-radius |
| PCL | posterior cruciate ligament |
| kKSS | Knee Society Score |
| fKKS | Function Knee Society Score |
| OKS | Oxford Knee Score |
| WOMAC | Western Ontario and McMaster University score |
| FJS | Forgotten Joint Score |
| SD | standard deviation |
References
- Evans, J.T.; Walker, R.W.; Evans, J.P.; Blom, A.W.; Sayers, A.; Whitehouse, M.R. How Long Does a Knee Replacement Last? A Systematic Review and Meta-Analysis of Case Series and National Registry Reports with More than 15 Years of Follow-Up. Lancet 2019, 393, 655–663. [Google Scholar] [CrossRef] [PubMed]
- Flierl, M.A.; Sobh, A.H.; Culp, B.M.; Baker, E.A.; Sporer, S.M. Evaluation of the Painful Total Knee Arthroplasty. J. Am. Acad. Orthop. Surg. 2019, 27, 743–751. [Google Scholar] [CrossRef]
- Freeman, M.A.R.; Pinskerova, V. The Movement of the Normal Tibio-Femoral Joint. J. Biomech. 2005, 38, 197–208. [Google Scholar] [CrossRef] [PubMed]
- Freeman, M.A.R.; Pinskerova, V. The Movement of the Knee Studied by Magnetic Resonance Imaging. Clin. Orthop. Relat. Res. 2003, 410, 35–43. [Google Scholar] [CrossRef]
- Alesi, D.; Marcheggiani Muccioli, G.M.; Roberti di Sarsina, T.; Bontempi, M.; Pizza, N.; Zinno, R.; Di Paolo, S.; Zaffagnini, S.; Bragonzoni, L. In Vivo Femorotibial Kinematics of Medial-Stabilized Total Knee Arthroplasty Correlates to Post-Operative Clinical Outcomes. Knee Surg. Sports Traumatol. Arthrosc. 2021, 29, 491–497. [Google Scholar] [CrossRef] [PubMed]
- Indelli, P.F.; Morello, F.; Ghirardelli, S.; Fidanza, A.; Iannotti, F.; Ferrini, A. No Clinical Differences at the 2-Year Follow-up between Single Radius and J-Curve Medial Pivot Total Knee Arthroplasty in the Treatment of Neutral or Varus Knees. Knee Surg. Sports Traumatol. Arthrosc. 2020, 28, 3949–3954. [Google Scholar] [CrossRef]
- Vecchini, E.; Ramazzini, L.; Lunardelli, E.; Zancanaro, F.; Amarossi, A.; Anselmi, A.; De Cristan, D.; Maluta, T.; Magnan, B.; Ricci, M. Short-Term Clinical and Radiological Comparisons between Two Medial Pivot Total Knee Arthroplasty Implants with Different Geometries. Acta Biomed. 2023, 94, e2023087–e2023094. [Google Scholar] [CrossRef]
- Elorza, S.P.; O’Donnell, E.; Nedopil, A.J.; Howell, S.M.; Hull, M.L. A New Tibial Insert Design with Ball-in-Socket Medial Conformity and Posterior Cruciate Ligament Retention Closely Restores Native Knee Tibial Rotation after Unrestricted Kinematic Alignment. J. Exp. Orthop. 2023, 10, 115. [Google Scholar] [CrossRef] [PubMed]
- Putame, G.; Terzini, M.; Rivera, F.; Kebbach, M.; Bader, R.; Bignardi, C. Kinematics and Kinetics Comparison of Ultra-Congruent versus Medial-Pivot Designs for Total Knee Arthroplasty by Multibody Analysis. Sci. Rep. 2022, 12, 3052. [Google Scholar] [CrossRef]
- Tsubosaka, M.; Ishida, K.; Kodato, K.; Shibanuma, N.; Hayashi, S.; Kurosaka, M.; Kuroda, R.; Matsumoto, T. Mid-Flexion Stability in the Anteroposterior Plane Is Achieved with a Medial Congruent Insert in Cruciate-Retaining Total Knee Arthroplasty for Varus Osteoarthritis. Knee Surg. Sports Traumatol. Arthrosc. 2021, 29, 467–473. [Google Scholar] [CrossRef]
- Cassar-Gheiti, A.J.; Jamieson, P.S.; Radi, M.; Wolfstadt, J.I.; Backstein, D.J. Evaluation of the Medial Stabilized Knee Design Using Data from National Joint Registries and Current Literature. J. Arthroplast. 2020, 35, 1950–1955. [Google Scholar] [CrossRef] [PubMed]
- Alessio-Mazzola, M.; Clemente, A.; Russo, A.; Mertens, P.; Burastero, G.; Formica, M.; Felli, L. Clinical Radiographic Outcomes and Survivorship of Medial Pivot Design Total Knee Arthroplasty: A Systematic Review of the Literature. Arch. Orthop. Trauma Surg. 2022, 142, 3437–3448. [Google Scholar] [CrossRef]
- Tso, R.; Smith, J.; Doma, K.; Grant, A.; McEwen, P. Clinical and Patient-Reported Outcomes of Medial Stabilized Versus Non–Medial Stabilized Prostheses in Total Knee Arthroplasty: A Systematic Review and Meta-Analysis. J. Arthroplast. 2021, 36, 767–776. [Google Scholar] [CrossRef]
- Scott, D.F.; Gray, C.G. Outcomes Are Better with a Medial-Stabilized vs a Posterior-Stabilized Total Knee Implanted with Kinematic Alignment. J. Arthroplast. 2022, 37, 852–858. [Google Scholar] [CrossRef]
- Batra, S.; Malhotra, R.; Kumar, V.; Srivastava, D.N.; Backstein, D.; Pandit, H. Superior Patient Satisfaction in Medial Pivot as Compared to Posterior Stabilized Total Knee Arthroplasty: A Prospective Randomized Study. Knee Surg. Sports Traumatol. Arthrosc. 2021, 29, 3633–3640. [Google Scholar] [CrossRef]
- Kulshrestha, V.; Sood, M.; Kanade, S.; Kumar, S.; Datta, B.; Mittal, G. Early Outcomes of Medial Pivot Total Knee Arthroplasty Compared to Posterior-Stabilized Design: A Randomized Controlled Trial. CiOS Clin. Orthop. Surg. 2020, 12, 178–186. [Google Scholar] [CrossRef]
- Chang, J.S.; Kayani, B.; Moriarty, P.D.; Tahmassebi, J.E.; Haddad, F.S. A Prospective Randomized Controlled Trial Comparing Medial-Pivot versus Posterior-Stabilized Total Knee Arthroplasty. J. Arthroplast. 2021, 36, 1584–1589. [Google Scholar] [CrossRef] [PubMed]
- Rossi, S.M.P.; Sangaletti, R.; Jannelli, E.; Bova, D.; Montagna, A.; Benazzo, F. PCL Preservation or Sacrifice Does Not Influence Clinical Outcomes and Survivorship at Mid-Term Follow-up of a J-Curve CR Total Knee Replacement with a Medial Congruent Liner and a Functional Coronal Alignment. Arch. Orthop. Trauma Surg. 2024, 144, 307–313. [Google Scholar] [CrossRef] [PubMed]
- Bae, D.K.; Song, S.J.; Cho, S.D. Clinical Outcome of Total Knee Arthroplasty with Medial Pivot Prosthesis. A Comparative Study Between the Cruciate Retaining and Sacrificing. J. Arthroplast. 2011, 26, 693–698. [Google Scholar] [CrossRef]
- Budhiparama, N.C.; Lumban-Gaol, I.; Novito, K.; Hidayat, H.; De Meo, F.; Cacciola, G.; Cavaliere, P. PCL Retained Is Safe in Medial Pivot TKA—A Prospective Randomized Trial. Knee Surg. Sports Traumatol. Arthrosc. 2023, 31, 5856–5863. [Google Scholar] [CrossRef]
- Hu, M.; Xiang, S.; Xu, H.; Wang, Y.; Lv, C.; Zhang, H. Equivalence of Clinical and Radiological Outcomes in Cruciate-Retaining and Cruciate-Substituting Total Knee Arthroplasty with Medial Pivot Knee: A Comparative Study. Heliyon 2023, 9, e22741. [Google Scholar] [CrossRef]
- Rajgopal, A.; Kumar, S.; Singh, M.K.; Aggarwal, K. PCL Retention Demonstrates Better Functional Scores and Gait Patterns in Total Knee Arthroplasty Using a Medial Congruent Insert—A Prospective Study. Knee Surg. Sports Traumatol. Arthrosc. 2023, 31, 4741–4746. [Google Scholar] [CrossRef] [PubMed]
- Giustra, F.; Bosco, F.; Cacciola, G.; Risitano, S.; Capella, M.; Bistolfi, A.; Massè, A.; Sabatini, L. No Significant Differences in Clinical and Radiographic Outcomes between PCL Retained or Sacrificed Kinematic Aligned Medial Pivot Total Knee Arthroplasty in Varus Knee. J. Clin. Med. 2022, 11, 6569. [Google Scholar] [CrossRef]
- Cacciola, G.; De Martino, I.; De Meo, F. Does the Medial Pivot Knee Improve the Clinical and Radiographic Outcome of Total Knee Arthroplasty? A Single Centre Study on Two Hundred and Ninety Seven Patients. Int. Orthop. 2020, 44, 291–299. [Google Scholar] [CrossRef]
- Nakamura, J.; Inoue, T.; Suguro, T.; Suzuki, M.; Sasho, T.; Hagiwara, S.; Akagi, R.; Orita, S.; Inage, K.; Akazawa, T.; et al. A Comparative Study of Flat Surface Design and Medial Pivot Design in Posterior Cruciate-Retaining Total Knee Arthroplasty: A Matched Pair Cohort Study of Two Years. BMC Musculoskelet. Disord. 2018, 19, 234. [Google Scholar] [CrossRef] [PubMed]
- Nishitani, K.; Furu, M.; Nakamura, S.; Kuriyama, S.; Ishikawa, M.; Ito, H.; Matsuda, S. No Differences in Patient-Reported Outcomes between Medial Pivot Insert and Symmetrical Insert in Total Knee Arthroplasty: A Randomized Analysis. Knee 2018, 25, 1254–1261. [Google Scholar] [CrossRef]
- Indelli, P.F.; Spinello, P.; Zepeda, K.; Campi, S.; Rossi, S.M.P.; Engl, M.; Papalia, R.; Benazzo, F. Medially Congruent Total Knee Arthroplasty in Valgus Knee Deformities Yields Satisfactory Outcomes: A Multicenter, International Study. Knee Surg. Sports Traumatol. Arthrosc. 2023, 31, 407–412. [Google Scholar] [CrossRef] [PubMed]
- Iwakiri, K.; Ohta, Y.; Ohyama, Y.; Minoda, Y.; Kobayashi, A.; Nakamura, H. Is Medial Pivot Total Knee Arthroplasty Suitable for Patients with Valgus Knee Osteoarthritis? Eur. J. Orthop. Surg. Traumatol. 2022, 32, 551–557. [Google Scholar] [CrossRef]
- Anderson, M.J.; Kruse, R.L.; Leslie, C.; Levy, L.J.; Pritchett, J.W.; Hodge, J. Medium-Term Results of Total Knee Arthroplasty Using a Medially Pivoting Implant: A Multicenter Study. J. Surg. Orthop. Adv. 2010, 19, 191–195. [Google Scholar]
- Mannan, K.; Scott, G. The Medial Rotation Total Knee Replacement a Clinical and Radiological Review at a Mean Follow-Up of Six Years. J. Bone Jt. Surg. Br. Vol. 2009, 91, 750–756. [Google Scholar] [CrossRef]
- Katchky, A.M.; Jones, C.W.; Walter, W.L.; Shimmin, A.J. Medial Ball and Socket Total Knee Arthroplasty: Five-Year Clinical Results. Bone Jt. J. 2019, 101-B, 59–65. [Google Scholar] [CrossRef]
- Choi, N.Y.; In, Y.; Bae, J.H.; Do, J.H.; Chung, S.J.; Koh, I.J. Are Midterm Patient-Reported Outcome Measures Between Rotating-Platform Mobile-Bearing Prosthesis and Medial-Pivot Prosthesis Different? A Minimum of 5-Year Follow-Up Study. J. Arthroplast. 2017, 32, 824–829. [Google Scholar] [CrossRef] [PubMed]
- Dehl, M.; Bulaïd, Y.; Chelli, M.; Belhaouane, R.; Gabrion, A.; Havet, E.; Mertl, P. Total Knee Arthroplasty with the Medial-Pivot Knee System: Clinical and Radiological Outcomes at 9.5 Years’ Mean Follow-Up. Orthop. Traumatol. Surg. Res. 2018, 104, 185–191. [Google Scholar] [CrossRef]
- Fan, C.Y.; Hsieh, J.T.S.; Hsieh, M.S.; Shih, Y.C.; Lee, C.H. Primitive Results after Medial-Pivot Knee Arthroplasties. A Minimum 5-Year Follow-up Study. J. Arthroplast. 2010, 25, 492–496. [Google Scholar] [CrossRef] [PubMed]
- Vecchini, E.; Christodoulidis, A.; Magnan, B.; Ricci, M.; Regis, D.; Bartolozzi, P. Clinical and Radiologic Outcomes of Total Knee Arthroplasty Using the Advance Medial Pivot Prosthesis. A Mean 7years Follow-Up. Knee 2012, 19, 851–855. [Google Scholar] [CrossRef]
- Xiang, S.; Wang, Y.; Lv, C.; Wang, C.; Zhang, H. Mid-Term Clinical Outcomes and Survivorship of Medial-Pivot Total Knee Arthroplasty-a Mean Five Year Follow-up Based on One Thousand, One Hundred and Twenty Eight Cases. Int. Orthop. 2021, 45, 2877–2883. [Google Scholar] [CrossRef] [PubMed]
- Brinkman, J.M.; Bubra, P.S.; Walker, P.; Walsh, W.R.; Bruce, W.J.M. Midterm Results Using a Medial Pivot Total Knee Replacement Compared with the Australian National Joint Replacement Registry Data. ANZ J. Surg. 2014, 84, 172–176. [Google Scholar] [CrossRef]
- Karachalios, T.; Varitimidis, S.; Bargiotas, K.; Hantes, M.; Roidis, N.; Malizos, K.N. An 11-to 15-Year Clinical Outcome Study of the Advance Medial Pivot Total Knee Arthroplasty Pivot Knee Arthroplasty. Bone Jt. J. 2016, 98-B, 1050–1055. [Google Scholar] [CrossRef]
- Shi, W.; Jiang, Y.; Wang, C.; Zhang, H.; Wang, Y.; Li, T. Comparative Study on Mid- and Long-Term Clinical Effects of Medial Pivot Prosthesis and Posterior-Stabilized Prosthesis after Total Knee Arthroplasty. J. Orthop. Surg. Res. 2020, 15, 421. [Google Scholar] [CrossRef]
- Schmidt, R.; Ogden, S.; Blaha, J.D.; Alexander, A.; Fitch, D.A.; Barnes, C.L. Midterm Clinical and Radiographic Results of the Medial Pivot Total Knee System. Int. Orthop. 2014, 38, 2495–2498. [Google Scholar] [CrossRef]
- Ueyama, H.; Kanemoto, N.; Minoda, Y.; Yamamoto, N.; Taniguchi, Y.; Nakamura, H. Comparison of Postoperative Knee Flexion and Patient Satisfaction between Newly and Conventionally Designed Medial Pivot Total Knee Arthroplasty: A 5-Year Follow-up Matched Cohort Study. Arch. Orthop. Trauma Surg. 2022, 142, 2057–2064. [Google Scholar] [CrossRef] [PubMed]
- Youm, Y.S.; Cho, S.D.; Lee, S.H.; Cho, H.Y. Total Knee Arthroplasty Using a Posterior Cruciate Ligament Sacrificing Medial Pivot Knee: Minimum 5-Year Follow-up Results. Knee Surg. Relat. Res. 2014, 26, 135–140. [Google Scholar] [CrossRef] [PubMed]
- Kim, Y.H.; Park, J.W.; Kim, J.S. Clinical Outcome of Medial Pivot Compared with Press-Fit Condylar Sigma Cruciate-Retaining Mobile-Bearing Total Knee Arthroplasty. J. Arthroplast. 2017, 32, 3016–3023. [Google Scholar] [CrossRef] [PubMed]
- Chinzei, N.; Ishida, K.; Tsumura, N.; Matsumoto, T.; Kitagawa, A.; Iguchi, T.; Nishida, K.; Akisue, T.; Kuroda, R.; Kurosaka, M. Satisfactory Results at 8years Mean Follow-up after ADVANCE® Medial-Pivot Total Knee Arthroplasty. Knee 2014, 21, 387–390. [Google Scholar] [CrossRef]
- Macheras, G.A.; Galanakos, S.P.; Lepetsos, P.; Anastasopoulos, P.P.; Papadakis, S.A. A Long Term Clinical Outcome of the Medial Pivot Knee Arthroplasty System. Knee 2017, 24, 447–453. [Google Scholar] [CrossRef]
- Ueyama, H.; Kanemoto, N.; Minoda, Y.; Yamamoto, N.; Taniguchi, Y.; Nakamura, H. Long-Term Clinical Outcomes of Medial Pivot Total Knee Arthroplasty for Asian Patients: A Mean 10-Year Follow-up Study. Knee 2020, 27, 1778–1786. [Google Scholar] [CrossRef]
- Ettinger, M.; Tuecking, L.R.; Savov, P.; Windhagen, H. Higher Satisfaction and Function Scores in Restricted Kinematic Alignment versus Mechanical Alignment with Medial Pivot Design Total Knee Arthroplasty: A Prospective Randomised Controlled Trial. Knee Surg. Sports Traumatol. Arthrosc. 2024, 32, 1275–1286. [Google Scholar] [CrossRef]
- Shakya, A.; Singh, V.; Agrawal, R.A.; Sharma, A.; Mangale, N.; Wadgave, V.; Jaiswal, A. A Mid-Term Comparison of the Functional Outcomes of Medial Pivot and Rotating Platform Mobile-Bearing Total Knee Arthroplasty in the Indian Population. Indian J. Orthop. 2022, 56, 271–279. [Google Scholar] [CrossRef]
- Sosio, C.; Rossi, N.; Sirtori, P.; Ciliberto, R.; Lombardo, M.D.M.; Peretti, G.M.; Mangiavini, L. Clinical and Functional Outcomes of Kinematic Aligned Total Knee Arthroplasty with a Medial Pivot Design: Two-Year Follow-Up. J. Clin. Med. 2023, 12, 7258. [Google Scholar] [CrossRef]
- Malhotra, R.; Janardhanan, R.; Batra, S. Total Knee Arthroplasty in Rheumatoid Arthritis Patients with a Medial Stabilized Prosthesis—A Retrospective Analysis. J. Clin. Orthop. Trauma 2021, 21, 101566. [Google Scholar] [CrossRef]
- Howell, S.M. Calipered Kinematically Aligned Total Knee Arthroplasty: An Accurate Technique That Improves Patient Outcomes and Implant Survival. Orthopedics 2019, 42, 126–135. [Google Scholar] [CrossRef] [PubMed]
- Rossi, S.M.P.; Benazzo, F. Individualized Alignment and Ligament Balancing Technique with the ROSA® Robotic System for Total Knee Arthroplasty. Int. Orthop. 2023, 47, 755–762. [Google Scholar] [CrossRef] [PubMed]
- Faschingbauer, M.; Hambrecht, J.; Schwer, J.; Martin, J.R.; Reichel, H.; Seitz, A. Tibial Insert Design Significantly Alters Knee Kinematics Using a Single Cruciate-Retaining Total Knee Implant an in Vitro Study. Bone Jt. Open 2024, 5, 592–600. [Google Scholar] [CrossRef]
- Nedopil, A.J.; Howell, S.M.; Hull, M.L. More Passive Internal Tibial Rotation with Posterior Cruciate Ligament Retention than with Excision in a Medial Pivot TKA Implanted with Unrestricted Caliper Verified Kinematic Alignment. Knee Surg. Sports Traumatol. Arthrosc. 2023, 31, 852–860. [Google Scholar] [CrossRef] [PubMed]
- Moewis, P.; Duda, G.N.; Trepczynski, A.; Krahl, L.; Boese, C.K.; Hommel, H. Retention of Posterior Cruciate Ligament Alone May Not Achieve Physiological Knee Joint Kinematics After Total Knee Arthroplasty. J. Bone Jt. Surg. 2021, 103, 146–154. [Google Scholar] [CrossRef]
- Howell, S.M.; Shelton, T.J.; Gill, M.; Hull, M.L. A Cruciate-Retaining Implant Can Treat Both Knees of Most Windswept Deformities When Performed with Calipered Kinematically Aligned TKA. Knee Surg. Sports Traumatol. Arthrosc. 2021, 29, 437–445. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Published by MDPI on behalf of the Lithuanian University of Health Sciences. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).