A Comparison of the Results of Two Different Double-Row Repair Techniques in Arthroscopic Repair of Rotator Cuff Tears
Abstract
1. Introduction
2. Materials and Methods
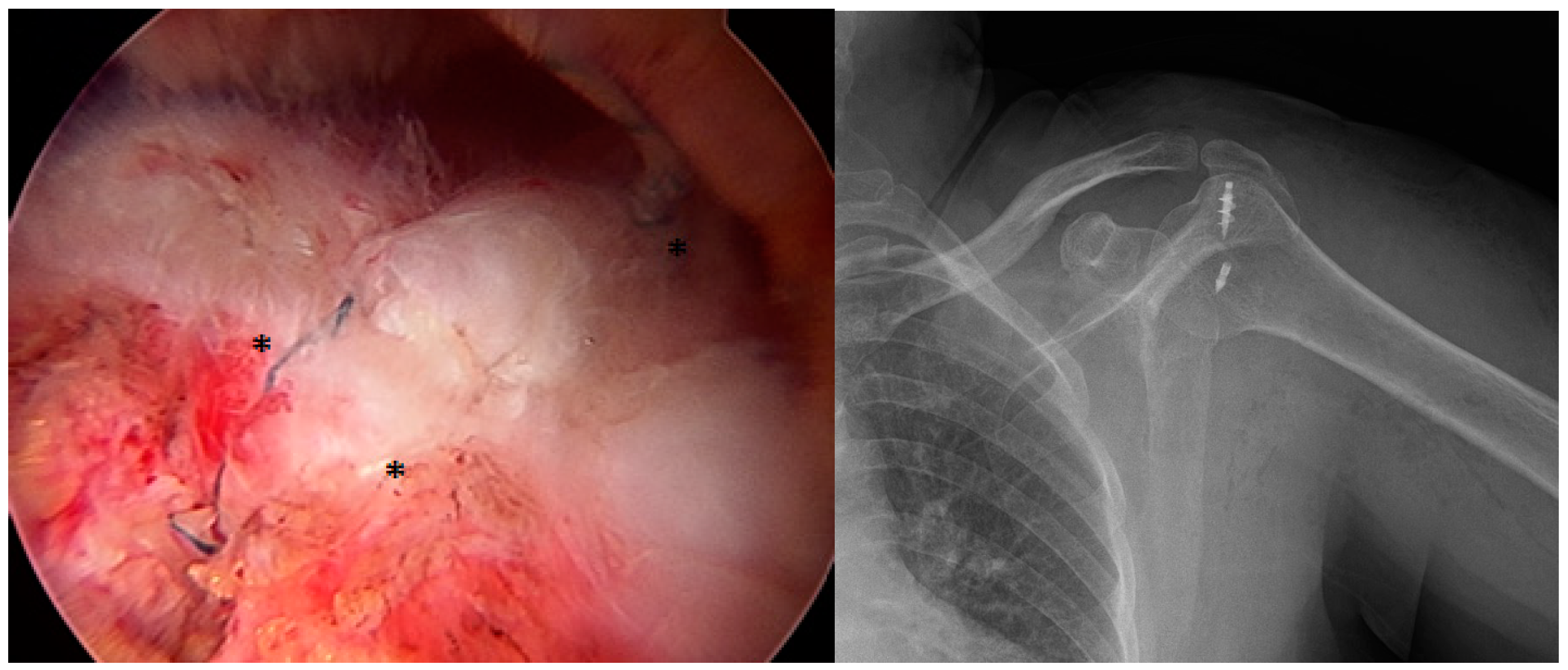
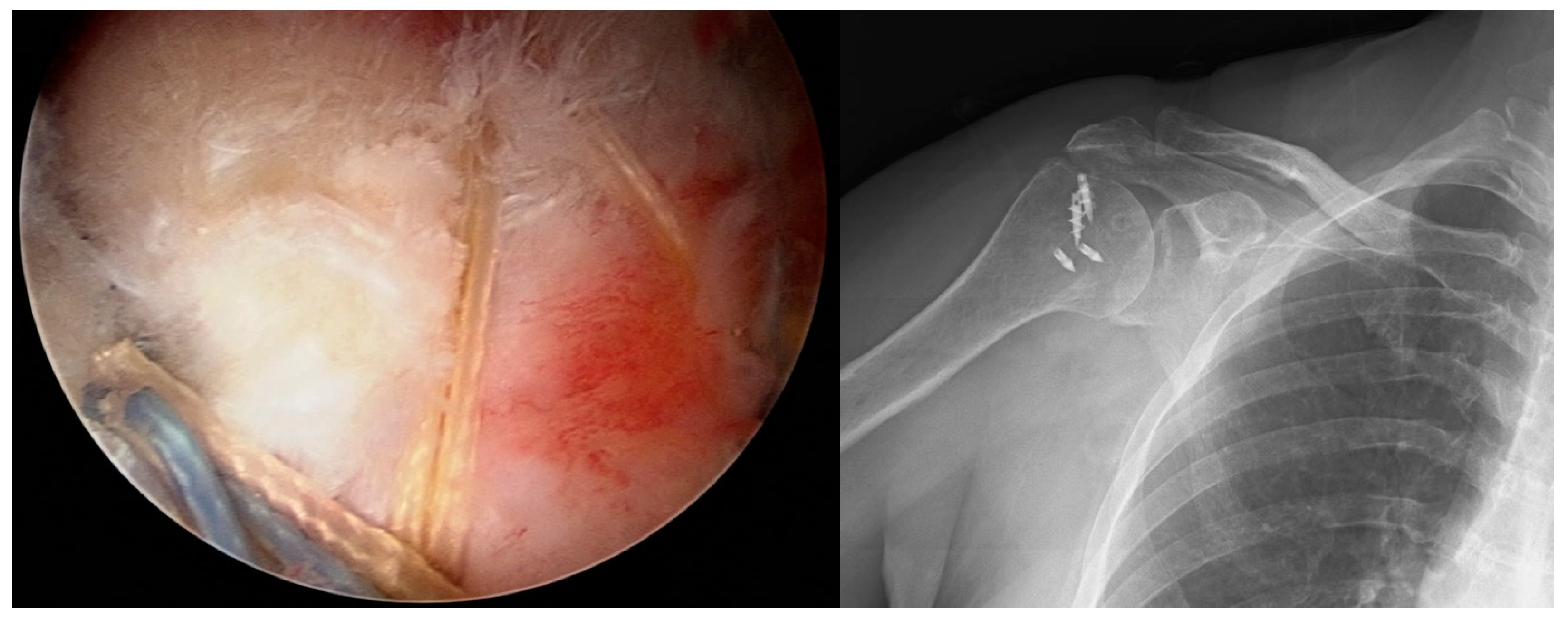
2.1. Surgical Procedure
2.2. Clinical Evaluation
2.3. Rehabilitation Protocol
2.4. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Tempelhof, S.; Rupp, S.; Seil, R. Age-related prevalence of rotator cuff tears in asymptomatic shoulders. J. Shoulder Elb. Surg. 1999, 8, 296–299. [Google Scholar] [CrossRef] [PubMed]
- Moulton, S.G.; Greenspoon, J.A.; Millett, P.J.; Petri, M. Suppl 1: M3: Risk factors, pathobiomechanics and physical examination of rotator cuff tears. Open Orthop. J. 2016, 10, 277. [Google Scholar] [CrossRef] [PubMed]
- Petri, M.; Ettinger, M.; Brand, S.; Stuebig, T.; Krettek, C.; Omar, M. Suppl 1: M11: Non-Operative Management of Rotator Cuff Tears. Open Orthop. J. 2016, 10, 349. [Google Scholar] [CrossRef] [PubMed]
- Hawi, N.; Schmiddem, U.; Omar, M.; Stuebig, T.; Krettek, C.; Petri, M.; Meller, R. Suppl 1: M8: Arthroscopic Debridement for Irreparable Rotator Cuff Tears. Open Orthop. J. 2016, 10, 324. [Google Scholar] [CrossRef][Green Version]
- Millett, P.J.; Warth, R.J.; Dornan, G.J.; Lee, J.T.; Spiegl, U.J. Clinical and structural outcomes after arthroscopic single-row versus double-row rotator cuff repair: A systematic review and meta-analysis of level I randomized clinical trials. J. Shoulder Elb. Surg. 2014, 23, 586–597. [Google Scholar] [CrossRef]
- Mook, W.R.; Greenspoon, J.A.; Millett, P.J. Suppl 1: M4: Arthroscopic double-row transosseous equivalent rotator cuff repair with a knotless self-reinforcing technique. Open Orthop. J. 2016, 10, 286. [Google Scholar] [CrossRef]
- Paolucci, T.; Agostini, F.; Conti, M.; Cazzolla, S.; Mussomeli, E.; Santilli, G.; Poso, F.; Bernetti, A.; Paoloni, M.; Mangone, M. Comparison of Early versus Traditional Rehabilitation Protocol after Rotator Cuff Repair: An Umbrella-Review. J. Clin. Med. 2023, 12, 6743. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Baums, M.H.; Spahn, G.; Steckel, H.; Fischer, A.; Schultz, W.; Klinger, H.-M. Comparative evaluation of the tendon-bone interface contact pressure in different single-versus double-row suture anchor repair techniques. Knee Surg. Sports Traumatol. Arthrosc. 2009, 17, 1466–1472. [Google Scholar] [CrossRef]
- Kim, D.H.; ElAttrache, N.S.; Tibone, J.E.; Jun, B.-J.; DeLaMora, S.N.; Kvitne, R.S.; Lee, T.Q. Biomechanical comparison of a single-row versus double-row suture anchor technique for rotator cuff repair. Am. J. Sports Med. 2006, 34, 407–414. [Google Scholar] [CrossRef]
- Gu, Z.; Wu, S.; Yang, Y.; Ren, T.; Zhang, K.-W. Comparison of arthroscopic single-row and double-row repair for rotator cuff injuries with different tear sizes: A systematic review and meta-analysis. Orthop. J. Sports Med. 2023, 11, 23259671231180854. [Google Scholar] [CrossRef]
- Lo, I.K.; Burkhart, S.S. Double-row arthroscopic rotator cuff repair: Re-establishing the footprint of the rotator cuff. Arthrosc. J. Arthrosc. Relat. Surg. 2003, 19, 1035–1042. [Google Scholar]
- Walch, G.; Edwards, T.B.; Boulahia, A.; Nové-Josserand, L.; Neyton, L.; Szabo, I. Arthroscopic tenotomy of the long head of the biceps in the treatment of rotator cuff tears: Clinical and radiographic results of 307 cases. J. Shoulder Elb. Surg. 2005, 14, 238–246. [Google Scholar] [CrossRef]
- Bishop, J.; Klepps, S.; Lo, I.K.; Bird, J.; Gladstone, J.N.; Flatow, E.L. Cuff integrity after arthroscopic versus open rotator cuff repair: A prospective study. J. Shoulder Elb. Surg. 2006, 15, 290–299. [Google Scholar]
- Lee, E.; Bishop, J.Y.; Braman, J.P.; Langford, J.; Gelber, J.; Flatow, E.L. Outcomes after arthroscopic rotator cuff repairs. J. Shoulder Elb. Surg. 2007, 16, 1–5. [Google Scholar]
- Boileau, P.; Brassart, N.; Watkinson, D.J.; Carles, M.; Hatzidakis, A.M.; Krishnan, S.G. Arthroscopic repair of full-thickness tears of the supraspinatus: Does the tendon really heal? J. Bone Jt. Surg. 2005, 87, 1229–1240. [Google Scholar]
- Galatz, L.M.; Ball, C.M.; Teefey, S.A.; Middleton, W.D.; Yamaguchi, K. The outcome and repair integrity of completely arthroscopically repaired large and massive rotator cuff tears. J. Bone Jt. Surg. 2004, 86, 219–224. [Google Scholar]
- Park, M.C.; ElAttrache, N.S.; Tibone, J.E.; Ahmad, C.S.; Jun, B.-J.; Lee, T.Q. Part I: Footprint contact characteristics for a transosseous-equivalent rotator cuff repair technique compared with a double-row repair technique. J. Shoulder Elb. Surg. 2007, 16, 461–468. [Google Scholar] [CrossRef]
- Park, M.C.; Tibone, J.E.; ElAttrache, N.S.; Ahmad, C.S.; Jun, B.-J.; Lee, T.Q. Part II: Biomechanical assessment for a footprint-restoring transosseous-equivalent rotator cuff repair technique compared with a double-row repair technique. J. Shoulder Elb. Surg. 2007, 16, 469–476. [Google Scholar]
- Fealy, S.; Adler, R.S.; Drakos, M.C.; Kelly, A.M.; Allen, A.A.; Cordasco, F.A.; Warren, R.F.; O’Brien, S.J. Patterns of vascular and anatomical response after rotator cuff repair. Am. J. Sports Med. 2006, 34, 120–127. [Google Scholar] [CrossRef]
- Gamradt, S.C.; Gallo, R.A.; Adler, R.S.; Maderazo, A.; Altchek, D.W.; Warren, R.F.; Fealy, S. Vascularity of the supraspinatus tendon three months after repair: Characterization using contrast-enhanced ultrasound. J. Shoulder Elb. Surg. 2010, 19, 73–80. [Google Scholar]
- Nicholas, S.J.; Lee, S.J.; Mullaney, M.J.; Tyler, T.F.; Fukunaga, T.; Johnson, C.D.; McHugh, M.P. Functional outcomes after double-row versus single-row rotator cuff repair: A prospective randomized trial. Orthop. J. Sports Med. 2016, 4, 2325967116667398. [Google Scholar] [CrossRef] [PubMed]
- Wang, E.; Wang, L.; Gao, P.; Li, Z.; Zhou, X.; Wang, S. Single-versus double-row arthroscopic rotator cuff repair in massive tears. Med. Sci. Monit. Int. Med. J. Exp. Clin. Res. 2015, 21, 1556. [Google Scholar] [CrossRef]
- Choi, C.-H.; Kim, S.-K.; Cho, M.-R.; Baek, S.-H.; Lee, J.-K.; Kim, S.-S.; Park, C.-M. Functional outcomes and structural integrity after double-pulley suture bridge rotator cuff repair using serial ultrasonographic examination. J. Shoulder Elb. Surg. 2012, 21, 1753–1763. [Google Scholar] [CrossRef] [PubMed]
- Yoo, J.C.; Ahn, J.H.; Koh, K.H.; Lim, K.S. Rotator cuff integrity after arthroscopic repair for large tears with less-than-optimal footprint coverage. Arthrosc. J. Arthrosc. Relat. Surg. 2009, 25, 1093–1100. [Google Scholar] [CrossRef]
- Cho, N.S.; Lee, B.G.; Rhee, Y.G. Arthroscopic rotator cuff repair using a suture bridge technique: Is the repair integrity actually maintained? Am. J. Sports Med. 2011, 39, 2108–2116. [Google Scholar] [CrossRef] [PubMed]
- Mihata, T.; Watanabe, C.; Fukunishi, K.; Ohue, M.; Tsujimura, T.; Fujiwara, K.; Kinoshita, M. Functional and structural outcomes of single-row versus double-row versus combined double-row and suture-bridge repair for rotator cuff tears. Am. J. Sports Med. 2011, 39, 2091–2098. [Google Scholar] [CrossRef]
- Yang Jr, J.; Robbins, M.; Reilly, J.; Maerz, T.; Anderson, K. The clinical effect of a rotator cuff retear: A meta-analysis of arthroscopic single-row and double-row repairs. Am. J. Sports Med. 2017, 45, 733–741. [Google Scholar]
- Yamamoto, A.; Takagishi, K.; Osawa, T.; Yanagawa, T.; Nakajima, D.; Shitara, H.; Kobayashi, T. Prevalence and risk factors of a rotator cuff tear in the general population. J. Shoulder Elb. Surg. 2010, 19, 116–120. [Google Scholar] [CrossRef]
- Björnsson, H.; Norlin, R.; Knutsson, A.; Adolfsson, L. Fewer rotator cuff tears fifteen years after arthroscopic subacromial decompression. J. Shoulder Elb. Surg. 2010, 19, 111–115. [Google Scholar] [CrossRef]
- Bölükbaşı, S.; Kanatlı, U. Rotator manşet hastalıklarında tanı ve tedavi algoritması. TOTBİD 2003, 2, 1–16. [Google Scholar]
- Milano, G.; Grasso, A.; Salvatore, M.; Zarelli, D.; Deriu, L.; Fabbriciani, C. Arthroscopic rotator cuff repair with and without subacromial decompression: A prospective randomized study. Arthrosc. J. Arthrosc. Relat. Surg. 2007, 23, 81–88. [Google Scholar] [CrossRef] [PubMed]
- Klintberg, I.H.; Karlsson, J.; Svantesson, U. Health-related quality of life, patient satisfaction, and physical activity 8–11 years after arthroscopic subacromial decompression. J. Shoulder Elb. Surg. 2011, 20, 598–608. [Google Scholar] [CrossRef] [PubMed]
- Norlin, R.; Adolfsson, L. Small full-thickness tears do well ten to thirteen years after arthroscopic subacromial decompression. J. Shoulder Elb. Surg. 2008, 17, S12–S16. [Google Scholar] [CrossRef] [PubMed]
- Voloshin, I.; Gelinas, J.; Maloney, M.D.; O’Keefe, R.J.; Bigliani, L.U.; Blaine, T.A. Proinflammatory cytokines and metalloproteases are expressed in the subacromial bursa in patients with rotator cuff disease. Arthrosc. J. Arthrosc. Relat. Surg. 2005, 21, 1076.e1–1076.e9. [Google Scholar] [CrossRef]
- Randelli, P.; Margheritini, F.; Cabitza, P.; Dogliotti, G.; Corsi, M.M. Release of growth factors after arthroscopic acromioplasty. Knee Surg. Sports Traumatol. Arthrosc. 2009, 17, 98–101. [Google Scholar] [CrossRef]
- Zhang, Z.; Ke, C.; Zhang, Z.; Chen, Y.; Weng, H.; Dong, J.; Hao, M.; Liu, B.; Zheng, M.; Li, J.; et al. Re-tear after arthroscopic rotator cuff repair can be predicted using deep learning algorithm. Front. Artif. Intell. 2024, 7, 1331853. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Santilli, G.; Mangone, M.; Agostini, F.; Paoloni, M.; Bernetti, A.; Diko, A.; Tognolo, L.; Coraci, D.; Vigevano, F.; Vetrano, M.; et al. Evaluation of Rehabilitation Outcomes in Patients with Chronic Neurological Health Conditions Using a Machine Learning Approach. J. Funct. Morphol. Kinesiol. 2024, 9, 176. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
| Group 1 | Group 2 | |
|---|---|---|
| Number of Patients | 26 | 27 |
| Female (n, %) | 18 (69.2%) | 22 (81.4%) |
| Male (n, %) | 8 (30.8%) | 5 (18.6%) |
| Mean Age (years) | 59.07 | 62 |
| Dominant Side Affected (n) | 19 | 17 |
| Bankart Repair (n) | 2 | 2 |
| SLAP Repair (n) | 2 | 1 |
| Biceps Tenodesis (n) | - | 1 |
| Biceps Tenotomy (n) | - | 1 |
| Subscapularis Repair (n) | - | 1 |
| Acromioplasty (n) | 26 | 27 |
| Preoperative Shoulder Abduction Degree | Group 1 | Group 2 | Total | |
| 0–30 | n % | 1 3.8% | 0 0% | 1 1.9% |
| 31–60 | n % | 6 23.1% | 2 7.4% | 8 15.1% |
| 61–90 | n % | 10 38.5% | 8 29.6% | 18 34% |
| 91–120 | n % | 5 19.2% | 9 33.3% | 14 26.4% |
| 121–150 | n % | 1 3.8% | 6 22.2% | 7 13.2% |
| 151–180 | n % | 3 11.5% | 2 7.4% | 5 9.4% |
| Total | n % | 26 100% | 27 100% | 53 100% |
| Postoperative Shoulder Abduction Degree | Group 1 | Group 2 | Total | |
| 61–90 | n % | 2 7.7% | 1 3.7% | 3 5.7% |
| 91–120 | n % | 3 11.5% | 4 14.8% | 7 13.2% |
| 121–150 | n % | 6 23.1% | 3 11.1% | 9 17% |
| 151–180 | n % | 15 57.7% | 19 70.4% | 34 64.2% |
| Total | n % | 26 100% | 27 100% | 53 100% |
| Group | Preop Constant | Postop Constant | |
|---|---|---|---|
| 1 | Mean | 41.73 | 84.1 |
| Median | 42 | 88.5 | |
| N | 26 | 26 | |
| Std. Deviation | 10.05 | 15.8 | |
| Minimum | 24 | 41 | |
| Maximum | 68 | 100 | |
| 2 | Mean | 42.85 | 84 |
| Median | 44 | 88 | |
| N | 27 | 27 | |
| Std. Deviation | 9.5 | 15.45 | |
| Minimum | 27 | 39 | |
| Maximum | 68 | 100 | |
| Total | Mean | 42.3 | 84.04 |
| Median | 42 | 88 | |
| N | 53 | 53 | |
| Std. Deviation | 9.71 | 15.5 | |
| Minimum | 24 | 39 | |
| Maximum | 68 | 100 | |
| Postoperative Constant Score | Group 1 | Group 2 | Total | |
|---|---|---|---|---|
| Poor | n % | 6 23.1% | 5 18.5% | 11 20.8% |
| Moderate | n % | 1 3.8% | 1 3.7% | 2 3.8% |
| Good | n % | 6 23.1% | 10 37% | 16 30.2% |
| Excellent | n % | 13 50% | 11 40.7% | 24 45.3% |
| Total | n % | 26 100% | 27 100% | 53 100% |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Published by MDPI on behalf of the Lithuanian University of Health Sciences. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ünlü, G.; Çatma, M.F.; Satılmış, A.B.; Cengiz, T.; Ünlü, S.; Erdem, M.; Ersan, Ö. A Comparison of the Results of Two Different Double-Row Repair Techniques in Arthroscopic Repair of Rotator Cuff Tears. Medicina 2025, 61, 674. https://doi.org/10.3390/medicina61040674
Ünlü G, Çatma MF, Satılmış AB, Cengiz T, Ünlü S, Erdem M, Ersan Ö. A Comparison of the Results of Two Different Double-Row Repair Techniques in Arthroscopic Repair of Rotator Cuff Tears. Medicina. 2025; 61(4):674. https://doi.org/10.3390/medicina61040674
Chicago/Turabian StyleÜnlü, Gökhan, Mehmet Faruk Çatma, Ahmet Burak Satılmış, Tolgahan Cengiz, Serhan Ünlü, Mustafa Erdem, and Önder Ersan. 2025. "A Comparison of the Results of Two Different Double-Row Repair Techniques in Arthroscopic Repair of Rotator Cuff Tears" Medicina 61, no. 4: 674. https://doi.org/10.3390/medicina61040674
APA StyleÜnlü, G., Çatma, M. F., Satılmış, A. B., Cengiz, T., Ünlü, S., Erdem, M., & Ersan, Ö. (2025). A Comparison of the Results of Two Different Double-Row Repair Techniques in Arthroscopic Repair of Rotator Cuff Tears. Medicina, 61(4), 674. https://doi.org/10.3390/medicina61040674






