Outcomes of Staphylococcal Prosthetic Joint Infection After Hip Hemiarthroplasty: Single Center Retrospective Study
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Protocol
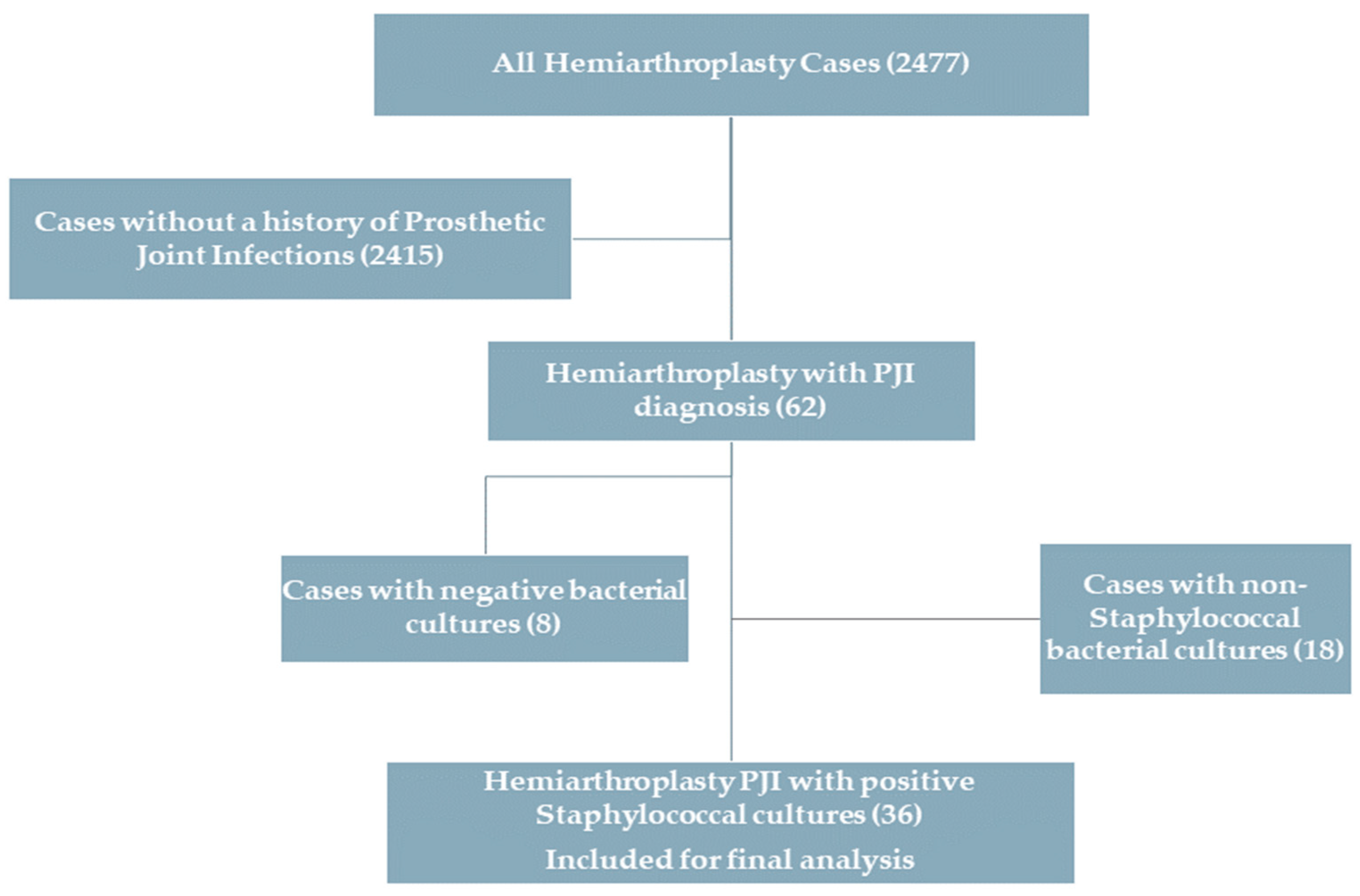
2.2. Inclusion Criteria
- Patients who underwent hemiarthroplasty for a hip fracture, either primarily after trauma or for the management of femoral neck fracture nonunion.
- Patients diagnosed with postoperative hematoma or postoperative prosthetic joint infection.
2.3. Exclusion Criteria
- Patients with bacterial culture results indicating non-staphylococcal colonization.
- Patients who had negative bacterial culture results.
2.4. Statistical Analysis
3. Results
3.1. Patients
3.2. Clinical Outcomes
3.3. DAIR Surgery Outcomes (Twenty-Nine Cases)
3.4. Primary Implant Removal Surgery Outcomes (6 Cases)
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Bhandari, M.; Devereaux, P.J.; Tornetta, P., III; Swiontkowski, M.F.; Berry, D.J.; Haidukewych, G.; Schemitsch, E.H.; Hanson, B.P.; Koval, K.; Dirschl, D.; et al. Operative management of displaced femoral neck fractures in elderly patients: An international survey. JBJS 2005, 87, 2122–2130. [Google Scholar]
- Maffulli, N.; Aicale, R. Proximal Femoral Fractures in the Elderly: A Few Things to Know, and Some to Forget. Medicina 2022, 58, 1314. [Google Scholar] [CrossRef]
- Theil, C.; Bockholt, S.; Gosheger, G.; Dieckmann, R.; Schwarze, J.; Schulze, M.; Puetzler, J.; Moellenbeck, B. Surgical Management of Periprosthetic Joint Infections in Hip and Knee Megaprostheses. Medicina 2024, 60, 583. [Google Scholar] [CrossRef]
- Onorato, F.; Masoni, V.; Gagliardi, L.; Comba, L.C.; Rivera, F. What to Know about Antimicrobial Coatings in Arthroplasty: A Narrative Review. Medicina 2024, 60, 574. [Google Scholar] [CrossRef] [PubMed]
- Benito, N.; Franco, M.; Ribera, A.; Soriano, A.; Rodriguez-Pardo, D.; Sorlí, L.; Fresco, G.; Fernández-Sampedro, M.; Del Toro, M.D.; Guío, L.; et al. Time trends in the aetiology of prosthetic joint infections: A multicentre cohort study. Clin. Microbiol. Infect. 2016, 22, 732-e1. [Google Scholar]
- Aboltins, C.A.; Page, M.A.; Buising, K.L.; Jenney, A.W.J.; Daffy, J.R.; Choong, P.F.M.; Stanley, P.A. Treatment of staphylococcal prosthetic joint infections with debridement, prosthesis retention and oral rifampicin and fusidic acid. Clin. Microbiol. Infect. 2007, 13, 586–591. [Google Scholar]
- Brandt, C.M.; Sistrunk, W.W.; Duffy, M.C.; Hanssen, A.D.; Steckelberg, J.M.; Ilstrup, D.M.; Osmon, D.R. Staphylococcus aureus prosthetic joint infection treated with debridement and prosthesis retention. Clin. Infect. Dis. 1997, 24, 914–919. [Google Scholar] [PubMed]
- Byren, I.; Bejon, P.; Atkins, B.L.; Angus, B.; Masters, S.; McLardy-Smith, P.; Gundle, R.; Berendt, A. One hundred and twelve infected arthroplasties treated with ‘DAIR’ (debridement, antibiotics and implant retention): Antibiotic duration and outcome. J. Antimicrob. Chemother. 2009, 63, 1264–1271. [Google Scholar]
- Lora-Tamayo, J.; Murillo, O.; Iribarren, J.A.; Soriano, A.; Sánchez-Somolinos, M.; Baraia-Etxaburu, J.M.; Rico, A.; Palomino, J.; Rodríguez-Pardo, D.; Horcajada, J.P.; et al. A large multicenter study of methicillin-susceptible and methicillin-resistant Staphylococcus aureus prosthetic joint infections managed with implant retention. Clin. Infect. Dis. 2013, 56, 182–194. [Google Scholar]
- Marculescu, C.E.; Berbari, E.F.; Hanssen, A.D.; Steckelberg, J.M.; Harmsen, S.W.; Mandrekar, J.N.; Osmon, D.R. Outcome of prosthetic joint infections treated with debridement and retention of components. Clin. Infect. Dis. 2006, 42, 471–478. [Google Scholar]
- Brandt, C.M.; Duffy, M.C.; Berbari, E.F.; Hanssen, A.D.; Steckelberg, J.M.; Osmon, D.R. Staphylococcus aureus prosthetic joint infection treated with prosthesis removal and delayed reimplantation arthroplasty. Mayo Clin. Proc. 1999, 74, 553–558. [Google Scholar] [CrossRef] [PubMed]
- Senneville, E.; Joulie, D.; Legout, L.; Valette, M.; Dezeque, H.; Beltrand, E.; Roselé, B.; d’Escrivan, T.; Loïez, C.; Caillaux, M.; et al. Outcome and predictors of treatment failure in total hip/knee prosthetic joint infections due to Staphylococcus aureus. Clin. Infect. Dis. 2011, 53, 334–340. [Google Scholar] [CrossRef]
- Gómez-Junyent, J.; Lora-Tamayo, J.; Baraia-Etxaburu, J.; Sánchez-Somolinos, M.; Iribarren, J.A.; Rodriguez-Pardo, D.; Praena-Segovia, J.; Sorlí, L.; Bahamonde, A.; Riera, M.; et al. Implant removal in the management of prosthetic joint infection by Staphylococcus aureus: Outcome and predictors of failure in a large retrospective multicenter study. Antibiotics 2021, 10, 118. [Google Scholar] [CrossRef] [PubMed]
- Masters, J.; Metcalfe, D.; Ha, J.S.; Judge, A.; Costa, M.L. Surgical site infection after hip fracture surgery: A systematic review and meta-analysis of studies published in the UK. Bone Jt. Res. 2020, 9, 554–562. [Google Scholar] [CrossRef]
- De Jong, L.; Klem, T.M.A.L.; Kuijper, T.M.; Roukema, G.R. Factors affecting the rate of surgical site infection in patients after hemiarthroplasty of the hip following a fracture of the neck of the femur. Bone Jt. J. 2017, 99, 1088–1094. [Google Scholar] [CrossRef] [PubMed]
- Zimmerli, W.; Trampuz, A.; Ochsner, P.E. Prosthetic-joint infections. N. Eng. J. Med. 2004, 351, 1645–1654. [Google Scholar] [CrossRef]
- Fernandes Queiroga Moraes, G.; Cordeiro, L.V.; de Andrade Júnior, F.P. Main laboratory methods used for the isolation and identification of Staphylococcus spp. Rev. Colomb. Cienc. Químico-Farm. 2021, 50, 5–28. [Google Scholar] [CrossRef]
- Kherabi, Y.; Zeller, V.; Kerroumi, Y.; Meyssonnier, V.; Heym, B.; Lidove, O.; Marmor, S. Streptococcal and Staphylococcus aureus prosthetic joint infections: Are they really different? BMC Infect. Dis. 2022, 22, 555. [Google Scholar] [CrossRef]
- Lum, Z.C.; Holland, C.T.; Meehan, J.P. Systematic review of single stage revision for prosthetic joint infection. World J. Orthop. 2020, 11, 559. [Google Scholar] [CrossRef]
- Wouthuyzen-Bakker, M.; Sebillotte, M.; Lomas, J.; Taylor, A.; Palomares, E.B.; Murillo, O.; Parvizi, J.; Shohat, N.; Reinoso, J.C.; Sánchez, R.E.; et al. Clinical outcome and risk factors for failure in late acute prosthetic joint infections treated with debridement and implant retention. J. Infect. 2019, 78, 40–47. [Google Scholar] [CrossRef]
- Bourget-Murray, J.; Horton, I.; Morris, J.; Bureau, A.; Garceau, S.; Abdelbary, H.; Grammatopoulos, G. Periprosthetic joint infection following hip hemiarthroplasty: Factors associated with infection and treatment outcome. Bone Jt. Open 2022, 3, 924–932. [Google Scholar] [PubMed]
- Tsang, S.J.; Ting, J.; Simpson, A.H.R.W.; Gaston, P. Outcomes following debridement, antibiotics and implant retention in the management of periprosthetic infections of the hip: A review of cohort studies. Bone Jt. J. 2017, 99, 1458–1466. [Google Scholar] [CrossRef] [PubMed]
- Van Houwelingen, A.P.; Garbuz, D.S.; Masri, B.A.; Duncan, C.P. Methicillin-resistant infection after hip and knee replacement: Reason to change practice? J. Orthop. Trauma Rehabil. 2012, 16, 9–12. [Google Scholar] [CrossRef]
- Kilgus, D.J.; Howe, D.J.; Strang, A. Results of periprosthetic hip and knee infections caused by resistant bacteria. Clin. Orthop. Relat. Res. 2002, 404, 116–124. [Google Scholar]
- Salgado, C.D.; Dash, S.; Cantey, J.R.; Marculescu, C.E. Higher risk of failure of methicillin-resistant Staphylococcus aureus prosthetic joint infections. Clin. Orthop. Relat. Res. 2007, 461, 48–53. [Google Scholar] [CrossRef]
- Hays, M.R.; Kildow, B.J.; Hartman, C.W.; Lyden, E.R.; Springer, B.D.; Fehring, T.K.; Garvin, K.L. Increased incidence of methicillin-resistant Staphylococcus aureus in knee and hip prosthetic joint infection. J. Arthroplast. 2023, 38, S326–S330. [Google Scholar]
- Fischbacher, A.; Borens, O. Prosthetic-joint infections: Mortality over the last 10 years. J. Bone Jt. Infect. 2019, 4, 198–202. [Google Scholar]
- Gundtoft, P.H.; Pedersen, A.B.; Varnum, C.; Overgaard, S. Increased mortality after prosthetic joint infection in primary THA. Clin. Orthop. Relat. Res. 2017, 475, 2623–2631. [Google Scholar]
- Zmistowski, B.; Karam, J.A.; Durinka, J.B.; Casper, D.S.; Parvizi, J. Periprosthetic joint infection increases the risk of one-year mortality. JBJS 2013, 95, 2177–2184. [Google Scholar]
- Aslan, A.; Atay, T.; Aydoğan, N.H. Risk factors for mortality and survival rates in elderly patients undergoing hemiarthroplasty for hip fracture. Acta Orthop. Traumatol. Turc. 2020, 54, 138–143. [Google Scholar] [CrossRef]
- Bekerom, M.P.V.D.; Sierevelt, I.N.; Bonke, H.; Raaymakers, E.L. The natural history of the hemiarthroplasty for displaced intracapsular femoral neck fractures: 302 patients followed until revision or death. Acta Orthop. 2013, 84, 555–560. [Google Scholar] [CrossRef] [PubMed]
- Mahmoud, A.N.; Suk, M.; Horwitz, D.S. Symptomatic Acetabular Erosion After Hip Hemiarthroplasty: Is It a Major Concern? A Retrospective Analysis of 2477 Hemiarthroplasty Cases. J. Clin. Med. 2024, 13, 6756. [Google Scholar] [CrossRef] [PubMed]
- Mahmoud, A.N.; El-Husseini, T.; Elabd, M.A.; Soliman, R.A.; Maziad, A.M.; Horwitz, D.S. Metastatic Hip Disease in the Elderly: Does Uncemented Hip Hemiarthroplasty have a Role? SciBase Oncol. 2024, 2, 1015. [Google Scholar] [CrossRef]
- Mahmoud, A.N.; Prodoehl, J.P.; Echeverry-Martinez, M.F.; Horwitz, D.S. Hemiarthroplasty for Hip Fracture in Down Syndrome: A Retrospective Series of Five Cases. Hip Pelvis. 2024, 36, 281–289. [Google Scholar] [CrossRef]
- Mahmoud, A.N.; Doyle, C.M.; Kline, C.M.; Brule, N.; Sams, K.B.; Nye, A.; Horwitz, D.S. Hip fracture in blind patients: Outcomes of hip hemiarthroplasty. Arch. Trauma Res. 2024, 13, 209–215. [Google Scholar]
- Autorino, C.M.; Battenberg, A.; Blom, A.; Catani, F.; ElGanzoury, I.; Farrell, A.; Giorgini, A.; Goswami, K.; Hernandez, V.; Karas, V.; et al. General Assembly, Prevention, Operating Room—Surgical Attire: Proceedings of International Consensus on Orthopedic Infections. J. Arthroplast. 2019, 34, S117–S125. [Google Scholar] [CrossRef]
- Ribau, A.I.; Collins, J.E.; Chen, A.F.; Sousa, R.J. Is preoperative Staphylococcus aureus screening and decolonization effective at reducing surgical site infection in patients undergoing orthopedic surgery? A systematic review and meta-analysis with a special focus on elective total joint arthroplasty. J. Arthroplast. 2021, 36, 752–766. [Google Scholar] [CrossRef] [PubMed]

| Early Infection (Presented Within 3 Months After HA Surgery) (n = 26) | Late Infection (Presented After 3 Months Post-HA Surgery) (n = 10) | Total Cases (36) | |
|---|---|---|---|
| Time of presentation (mean, range) weeks | 3.45 weeks (1–10) | 53.4 weeks (15.7–217.3) | 17.7 weeks (1–217.3) |
| Age | 79 (52.6–98.8) | 69.7 (53.5–100) | 76.5 years (52.6–100) |
| BMI | 27 (16.2–39) | 27 (16–40.4) | 27 (range, 16–40.4) |
| Causative organism | MRSA (11) Staphylococcus aureus (6) Coagulase-negative staphylococci (2) Staphylococcus hemolyticus (1) Staphylococcus epidermidis (1) Other staphylococci (5) | MRSA (4) Staphylococcus aureus (2) Other staphylococci (4) | MRSA (15) Non-MRSA (8) Other staphylococci (13) |
| Outcome |
|
|
|
| Successful DAIR | 8/24 (33.3%) | 1/5 (20%) |
| Successful DAIR | Unsuccessful DAIR | |
|---|---|---|
| Number | 9 (31%) | 20 (69%) |
| Age | 78.8 (59.7–100) | 76.3 (52.6–98.9) |
| Time from HA till presentation | 1 late acute hematogenous (11.1%), 8 early (88.9%) | 4 late (20%), 16 early (80%) |
| Time from presentation till DAIR surgery | 3.4 days ± 2.1 (range, 1–8 days) | 10.6 days ± 13.7 (range, 1–62) |
| p = 0.03 (Welch t-test) (statistically significant) | ||
| Type of implant | Cemented 8 Uncemented 1 | Cemented 14 Uncemented 6 |
| Number of DAIR trials | 1 (6 cases) 2 (3 cases) | 1 (5 cases) 2 (11 cases) 3 (4 cases) |
| Outcome | The mean infection-free follow-up was 44.6 months |
|
| Causative organism |
|
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Published by MDPI on behalf of the Lithuanian University of Health Sciences. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Mahmoud, A.N.; Brule, N.R.; Suk, M.; Horwitz, D.S. Outcomes of Staphylococcal Prosthetic Joint Infection After Hip Hemiarthroplasty: Single Center Retrospective Study. Medicina 2025, 61, 602. https://doi.org/10.3390/medicina61040602
Mahmoud AN, Brule NR, Suk M, Horwitz DS. Outcomes of Staphylococcal Prosthetic Joint Infection After Hip Hemiarthroplasty: Single Center Retrospective Study. Medicina. 2025; 61(4):602. https://doi.org/10.3390/medicina61040602
Chicago/Turabian StyleMahmoud, Ahmed Nageeb, Nicholas R. Brule, Michael Suk, and Daniel Scott Horwitz. 2025. "Outcomes of Staphylococcal Prosthetic Joint Infection After Hip Hemiarthroplasty: Single Center Retrospective Study" Medicina 61, no. 4: 602. https://doi.org/10.3390/medicina61040602
APA StyleMahmoud, A. N., Brule, N. R., Suk, M., & Horwitz, D. S. (2025). Outcomes of Staphylococcal Prosthetic Joint Infection After Hip Hemiarthroplasty: Single Center Retrospective Study. Medicina, 61(4), 602. https://doi.org/10.3390/medicina61040602






