Gastrostomy in Children: A 5-Year Single Tertiary Center Experience
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design and Population
2.2. Data Collection and Procedures
2.3. Primary and Secondary Endpoints
2.4. Ethics
2.5. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| ESPGHAN | European Society of Pediatric Gastroenterology Hepatology and Nutrition |
| PEG | Percutaneous endoscopic gastrostomy |
| GT | Gastrostomy tube |
References
- McSweeney, M.E.; Jiang, H.; Deutsch, A.J.; Atmadja, M.; Lightdale, J.R. Long-term outcomes of infants and children undergoing percutaneous endoscopy gastrostomy tube placement. J. Pediatr. Gastroenterol. Nutr. 2013, 57, 663–667. [Google Scholar] [CrossRef] [PubMed]
- Homan, M.; Hauser, B.; Romano, C.; Tzivinikos, C.; Torroni, F.; Gottrand, F.; Hojsak, I.; Dall’Oglio, L.; Thomson, M.; Bontems, P.; et al. Percutaneous Endoscopic Gastrostomy in Children: An Update to the ESPGHAN Position Paper. J. Pediatr. Gastroenterol. Nutr. 2021, 73, 415–426. [Google Scholar] [CrossRef] [PubMed]
- Craig, G.M.; Scambler, G.; Spitz, L. Why parents of children with neurodevelopmental disabilities requiring gastrostomy feeding need more support. Dev. Med. Child Neurol. 2003, 45, 183–188. [Google Scholar] [CrossRef] [PubMed]
- Nelson, K.E.; Lacombe-Duncan, A.; Cohen, E.; Nicholas, D.B.; Rosella, L.C.; Guttmann, A.; Mahant, S. Family experiences with feeding tubes in neurologic impairment: A systematic review. Pediatrics 2015, 136, e140–e151. [Google Scholar] [CrossRef]
- Glasson, E.J.; Forbes, D.; Ravikumara, M.; Nagarajan, L.; Wilson, A.; Jacoby, P.; Wong, K.; Leonard, H.; Downs, J. Gastrostomy and quality of life in children with intellectual disability: A qualitative study. Arch. Dis. Child. 2020, 105, 969–974. [Google Scholar] [CrossRef]
- Martínez-Costa, C.; Calderón, C.; Gómez-López, L.; Borraz, S.; Pedrón-Giner, C. Satisfaction with gastrostomy feeding in caregivers of children with home enteral nutrition; application of the SAGA-8 questionnaire and analysis of involved factors. Nutr. Hosp. 2013, 28, 1121–1128. [Google Scholar]
- Townsend, J.L.; Craig, G.; Lawson, M.; Reilly, S.; Spitz, L. Cost-effectiveness of gastrostomy placement for children with neurodevelopmental disability. Arch. Dis. Child. 2008, 93, 873–877. [Google Scholar] [CrossRef]
- Calderón, C.; Gómez-López, L.; Martínez-Costa, C.; Borraz, S.; Moreno-Villares, J.M.; Pedrón-Giner, C. Feeling of burden, psychological distress, and anxiety among primary caregivers of children with home enteral nutrition. J. Pediatr. Psychol. 2011, 36, 188–195. [Google Scholar] [CrossRef]
- Martínez-Costa, C.; Calderón, C.; Pedrón-Giner, C.; Borraz, S.; Gómez-López, L. Psychometric properties of the structured Satisfaction Questionnaire with Gastrostomy Feeding (SAGA-8) for caregivers of children with gastrostomy tube nutritional support. J. Hum. Nutr. Diet. 2013, 26, 191–197. [Google Scholar] [CrossRef]
- Noviello, C.; Romano, M.; Mariscoli, F.; De Benedictis, F.M.; Martino, A.; Cobellis, G. Esophageal multichannel intraluminal impedance and pH monitoring in children: Indications and limits. Minerva Pediatr. 2014, 66, 287–291. [Google Scholar]
- Ateş, U.; Gurbanov, A.; Göllü, G.; Taştekin, N.Y.; Sözduyar, S.; Ergün, E.; Yağmurlu, A.; Çakmak, M.; Aktuğ, T.; Dindar, H.; et al. Laparoscopic Gastrostomy in Children: 10 Years of Experience. Sisli Etfal Hast. Tip Bul. 2018, 52, 169–172. [Google Scholar]
- Braegger, C.; Decsi, T.; Dias, J.A.; Hartman, C.; Kolacek, S.; Koletzko, B.; Koletzko, S.; Mihatsch, W.; Moreno, L.; Puntis, J.; et al. ESPGHAN Committee on Nutrition: Practical approach to paediatric enteral nutrition: A comment by the ESPGHAN committee on nutrition. J. Pediatr. Gastroenterol. Nutr. 2010, 51, 110–122. [Google Scholar] [PubMed]
- Jeličić Kadić, A.; Radošević, T.; Žitko, V.; Despot, R.; Pogorelić, Z.; Llorente Muñoz, C.M.; Runjić, E.; Kovačević, T.; Ćatipović Ardalić, T.; Polić, B.; et al. Percutaneous Endoscopic Gastrostomy Tubes Can Be Considered Safe in Children: A Single-Center 11-Year Retrospective Analysis. Medicina 2021, 57, 1236. [Google Scholar] [CrossRef]
- Di Leo, G.; Pascolo, P.; Hamadeh, K.; Trombetta, A.; Ghirardo, S.; Schleef, J.; Barbi, E.; Codrich, D. Gastrostomy Placement and Management in Children: A Single-Center Experience. Nutrients 2019, 11, 1555. [Google Scholar] [CrossRef] [PubMed]
- Baker, L.; Beres, A.L.; Baird, R. A systematic review and meta-analysis of gastrostomy insertion techniques in children. J. Pediatr. Surg. 2015, 50, 718–725. [Google Scholar] [CrossRef]
- Sandberg, F.; Viktorsdottir, M.B.; Salo, M.; Stenstrom, P.; Arnbjornsson, E. Comparison of major complications in children after laparoscopy-assisted gastrostomy and percutaneous endoscopic gastrostomy placement: A meta-analysis. Pediatr. Surg. Int. 2018, 34, 1321–1327. [Google Scholar] [CrossRef]
- Suksamanapun, N.; Mauritz, F.A.; Franken, J.; van der Zee, D.C.; van Herwaarden-Lindeboom, M.Y. Laparoscopic versus percutaneous endoscopic gastrostomy placement in children: Results of a systematic review and meta-analysis. J. Minim. Access. Surg. 2017, 13, 81–88. [Google Scholar]
- Salazar, J.H.; Spanbauer, C.; Sood, M.R.; Densmore, J.C.; Van Arendonk, K.J. Variability in the Method of Gastrostomy Placement in Children. Children 2020, 7, 53. [Google Scholar] [CrossRef]
- Koca, T.; Sivrice, A.C.; Dereci, S.; Duman, L.; Akcam, M. Percutaneous endoscopic gastrostomy in children: A single center experience. Turk. Pediatri. Ars. 2015, 50, 211–216. [Google Scholar] [CrossRef]
- Romano, C.; van Wynckel, M.; Hulst, J.; Broekaert, I.; Bronsky, J.; Dall’Oglio, L.; Mis, N.F.; Hojsak, I.; Orel, R.; Papadopoulou, A.; et al. European Society for Paediatric Gastroenterology, Hepatology and Nutrition Guidelines for the Evaluation and Treatment of Gastrointestinal and Nutritional Complications in Children with Neurological Impairment. J. Pediatr. Gastroenterol. Nutr. 2017, 65, 242–264. [Google Scholar] [CrossRef]
- Sima, A.; Smădeanu, R.E.; Simionescu, A.A.; Nedelea, F.; Vlad, A.M.; Becheanu, C. Menke-Hennekam Syndrome: A Literature Review and a New Case Report. Children 2022, 9, 759. [Google Scholar] [CrossRef] [PubMed]
- Van Biervliet, S.; Van Renterghem, K.; Vande Putte, D.; Vande Velde, S.; De Bruyne, R.; Van Winckel, M. Gastrostomy use in children: A 3-year single centre experience. Acta Gastroenterol. Belg. 2014, 77, 8–12. [Google Scholar] [PubMed]
- Vernon-Roberts, A.; Vernon-Roberts, A. Fundoplication versus postoperative medication for gastro-oesophageal reflux in children with neurological impairment undergoing gastrostomy. Cochrane Database Syst. Rev. 2013, 8, 006151. [Google Scholar] [CrossRef] [PubMed]
- Heuschkel, R.B.; Gottrand, F.; Devarajan, K.; Poole, H.; Callan, J.; Dias, J.A.; Karkelis, S.; Papadopoulou, A.; Husby, S.; Ruemmele, F.; et al. ESPGHAN position paper on management of percutaneus endoscopic gastrostomy in children and adolescents. J. Pediatr. Gastroenterol. Nutr. 2015, 60, 131–141. [Google Scholar] [CrossRef]
- Bawazir, O.A. Percutaneous endoscopic gastrostomy in children less than 10 kilograms: A comparative study. Saudi J. Gastroenterol. 2020, 26, 105–110. [Google Scholar] [CrossRef]
- Zenilman, A.; DeFazio, J.; Griggs, C.; Picoraro, J.; Fallon, E.M.; Middlesworth, W. Retained gastrostomy bumper resulting in esophageal fistula and spinal osteomyelitis. J. Pediatr. Surg. Case Rep. 2020, 61, 101527. [Google Scholar] [CrossRef]
- Constantinescu, G.; Sandru, V.; Ilie, M.; Nedelcu, C.; Tincu, R.; Popa, B. Treatment of Malignant Esophageal Fistulas: Fluoroscopic Placement of Esophageal SEMS, Endoscopically-assisted through Surgical Gastrostomy. A Case Report. J. Gastrointest. Liver Dis. 2016, 25, 249–252. [Google Scholar] [CrossRef]
- Major, C.; Hall, N.J. The Insertion and Management of Gastrostomies in Children in the United Kingdom—A Survey of Practice. J. Pediatr. Surg. 2024, 59, 1531–1537. [Google Scholar] [CrossRef]
- Tincu, R.C.; Cobilinschi, C.; Tincu, I.F.; Macovei, R.A. Efficacy of Noble Metal–alloy Endotracheal Tubes in Ventilator-associated Pneumonia Prevention: A Randomized Clinical Trial. Balk. Med. J. 2022, 39, 167–171. [Google Scholar] [CrossRef]
- McCormack, S.; Patel, K.; Smith, C. Blended diet for enteral tube feeding in young people: A systematic review of the benefits and complications. J. Hum. Nutr. Diet. 2023, 36, 1390–1405. [Google Scholar] [CrossRef]
- Franken, J.; Stellato, R.K.; Tytgat, S.H.A.J.; van der Zee, D.C.; Mauritz, F.A.; Lindeboom, M.Y.A. Health-related quality of life in children after laparoscopic gastrostomy placement. Qual. Life Res. 2020, 29, 171–178. [Google Scholar] [CrossRef] [PubMed]
- Sumritsopak, R.; Treepongkaruna, S.; Butsriphum, N.; Tanpowpong, P. Percutaneous endoscopic gastrostomy in children: Caregivers’ perspectives. J. Pediatr. Nurs. 2015, 30, e3–e7. [Google Scholar] [CrossRef] [PubMed]
- Jennuvat, S.; Khanom, S.; Prachasitthisak, N.; Vithayasai, N. The Outcomes and Quality of Life in Children with Neurodevelopmental Disabilities with Percutaneous Endoscopic Gastrostomy at Queen Sirikit National Institute of Child Health. J. Med. Assoc. Thail. 2023, 106, 88–94. [Google Scholar]
| Group 1 (Reflux Surgery) | Group 2 (No Reflux Surgery) | p-Value | |
|---|---|---|---|
| No. of patients | 34 (47.88) | 37 (52.11) | 1.33 |
| Age (mean ± SD, years) | 4.86 ± 1.09 | 5.15 ± 1.11 | 0.89 |
| Sex (n, %) | |||
| Male | 14 (41.17) | 20 (54.05) | 0.78 |
| Female | 20 (58.82) | 17 (45.94) | 0.99 |
| Area | |||
| Urban | 18 (52.94) | 27 (72.97) | 0.05 |
| Rural | 16 (47.05) | 10 (27.02) | 0.05 |
| Indication (n, %) | |||
| GERD | 34 (100) | 2 (5.40) | 0.05 |
| Malnutrition | 3 (8.82) | 6 (16.21) | 0.05 |
| Aspiration | 2 (5.88) | 5 (13.51) | 0.05 |
| Multiple | 25 (50) | 14 (37.83) | 0.05 |
| Genetic syndrome (n, %) | 10 (29.41) | 12 (43.43) | 0.05 |
| Aspiration pneumonia (n, %) | 24 (70.58) | 9 (24.32) | 0.05 |
| Z Weight (mean ± SD) | −2.33 ± 0.44 | −2.76 ± 0.89 | 0.67 |
| Z Height (mean ± SD) | −1.78 ± 0.56 | −1.89 ± 0.97 | 1.32 |
| Z score BMI | −3.11 ± 1.01 | −3.23 ± 1.12 | 1.44 |
| Previous feeding procedure | |||
| Oral Naso-gastric tubes Mixed | 5 (14.7) 20 (58.82) 9 (26.47) | 9 (24.32) 26 (70.27) 3 (8.10) | 0.79 |
| Types of food used before GT | |||
| Standard formula Enteral formula Normal diet Mixt | 7 (20.58) 5 (14.7) 5 (14.7) 17 (50) | 9 (24.32) 8 (21.62) 7 (18.91) 13 (35.13) | 0.68 |
| Meal duration in minutes (mean ± SD) | 45 ± 12.33 | 45.72 ± 13.45 | 0.78 |
| Partial oral nutrition Y/N (n, %) | 5 (14.7) | 11 (29.72) | 0.05 |
| Types of food used after GT | |||
| Milk formula Home blenderized diet Modular diet | 7 (20.58) 9 (26.47) 18 (52.94) | 11 (29.72) 18 (48.64) 8 (21.62) | 0.99 |
| Time for the first feeding | 8.10 ± 2.54 | 8.14 ± 2.11 | 0.88 |
| Night continuous nutrition | 1 (2.94) | 0 (0) | NA |
| Group 1 (Reflux Surgery) | Group 2 (No Reflux Surgery) | p-Value | |
|---|---|---|---|
| Symptoms | |||
| Nausea (n, %) | 3 (8.82) | 5 (13.51) | 0.05 |
| Eructation (n, %) | 1 (2.94) | 3 (8.10) | 0.05 |
| Reflux (n, %) | 1 (2.94) | 1 (2.70) | 0.12 |
| Vomiting (n, %) | 1 (2.94) | 3 (8.10) | 0.05 |
| Flatulence (n, %) | 3 (8.82) | 5 (13.51) | 0.05 |
| abdominal pain (n, %) | 10 (29.41) | 9 (24.32) | 0.99 |
| Constipation (n, %) | 2 (5.88) | 2 (5.40) | 0.76 |
| Diarrhea (n, %) | 0 (0) | 0 (0) | NA |
| Mouth dryness (n, %) | 1 (2.94) | 0 (0) | NA |
| Complications | |||
| Suppuration (n, %) | 11 (32.35) | 8 (21.62) | 0.88 |
| Infection (n, %) | 2 (5.88) | 1 (2.70) | 0.67 |
| Disjunction (n, %) | 2 (5.88) | 2 (5.40) | 0.97 |
| Fistula (n, %) | 0 (0) | 0 (0) | NA |
| Bumper retraction (n, %) | 0 (0) | 0 (0) | NA |
| Hospitalization duration (mean ± SD, days) | 7.51 ± 3.56 | 4.22 ± 2.13 | <0.005 |
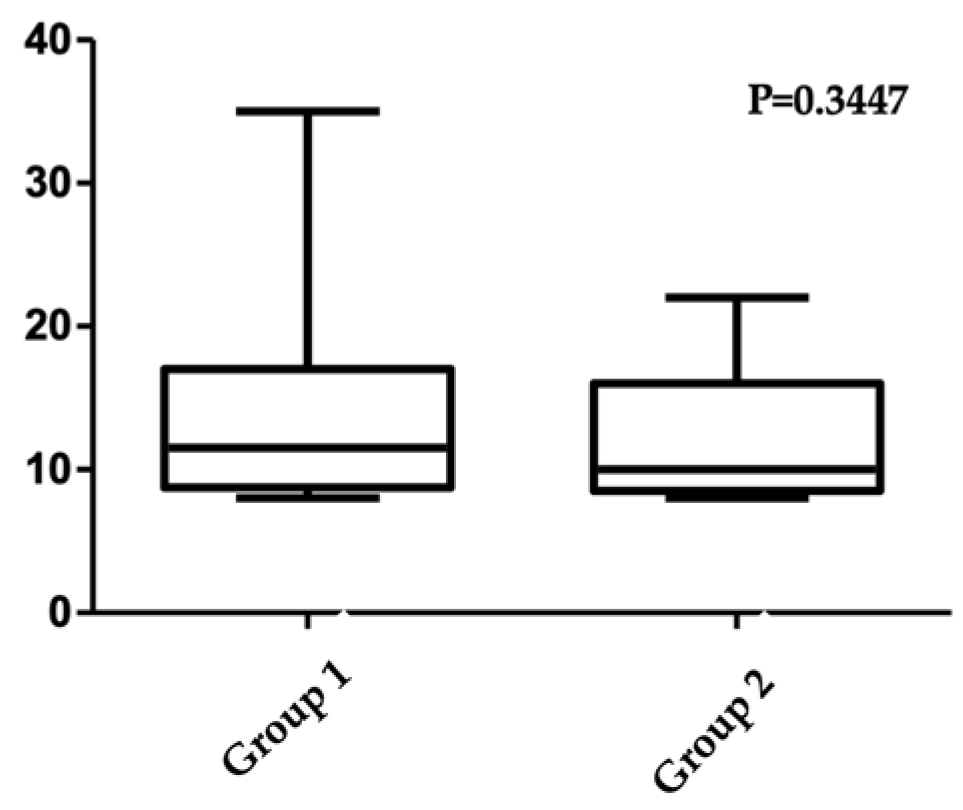
| SAGA-8 | |||
|---|---|---|---|
| Yes | No | p-Value | |
| Genetic syndrome | 11.9 | 11.5 | 0.88 |
| Aspiration pneumonia | 14.3 | 12.3 | 0.05 |
| Hospitalization > 5 days | 12.9 | 13.6 | 0.76 |
| Home blenderized diet | 15.39 | 12.04 | 0.75 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Published by MDPI on behalf of the Lithuanian University of Health Sciences. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ţincu, I.F.; Chenescu, B.T.; Drăgan, G.C.; Avram, A.I.; Pleșca, D.A. Gastrostomy in Children: A 5-Year Single Tertiary Center Experience. Medicina 2025, 61, 459. https://doi.org/10.3390/medicina61030459
Ţincu IF, Chenescu BT, Drăgan GC, Avram AI, Pleșca DA. Gastrostomy in Children: A 5-Year Single Tertiary Center Experience. Medicina. 2025; 61(3):459. https://doi.org/10.3390/medicina61030459
Chicago/Turabian StyleŢincu, Iulia Florentina, Bianca Teodora Chenescu, Gabriel Cristian Drăgan, Anca Ioana Avram, and Doina Anca Pleșca. 2025. "Gastrostomy in Children: A 5-Year Single Tertiary Center Experience" Medicina 61, no. 3: 459. https://doi.org/10.3390/medicina61030459
APA StyleŢincu, I. F., Chenescu, B. T., Drăgan, G. C., Avram, A. I., & Pleșca, D. A. (2025). Gastrostomy in Children: A 5-Year Single Tertiary Center Experience. Medicina, 61(3), 459. https://doi.org/10.3390/medicina61030459






