Impact of the Coronavirus Disease 2019 Pandemic on the Management and Outcomes of ST-Segment Elevation Myocardial Infarction Patients: A Retrospective Cohort Study
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design
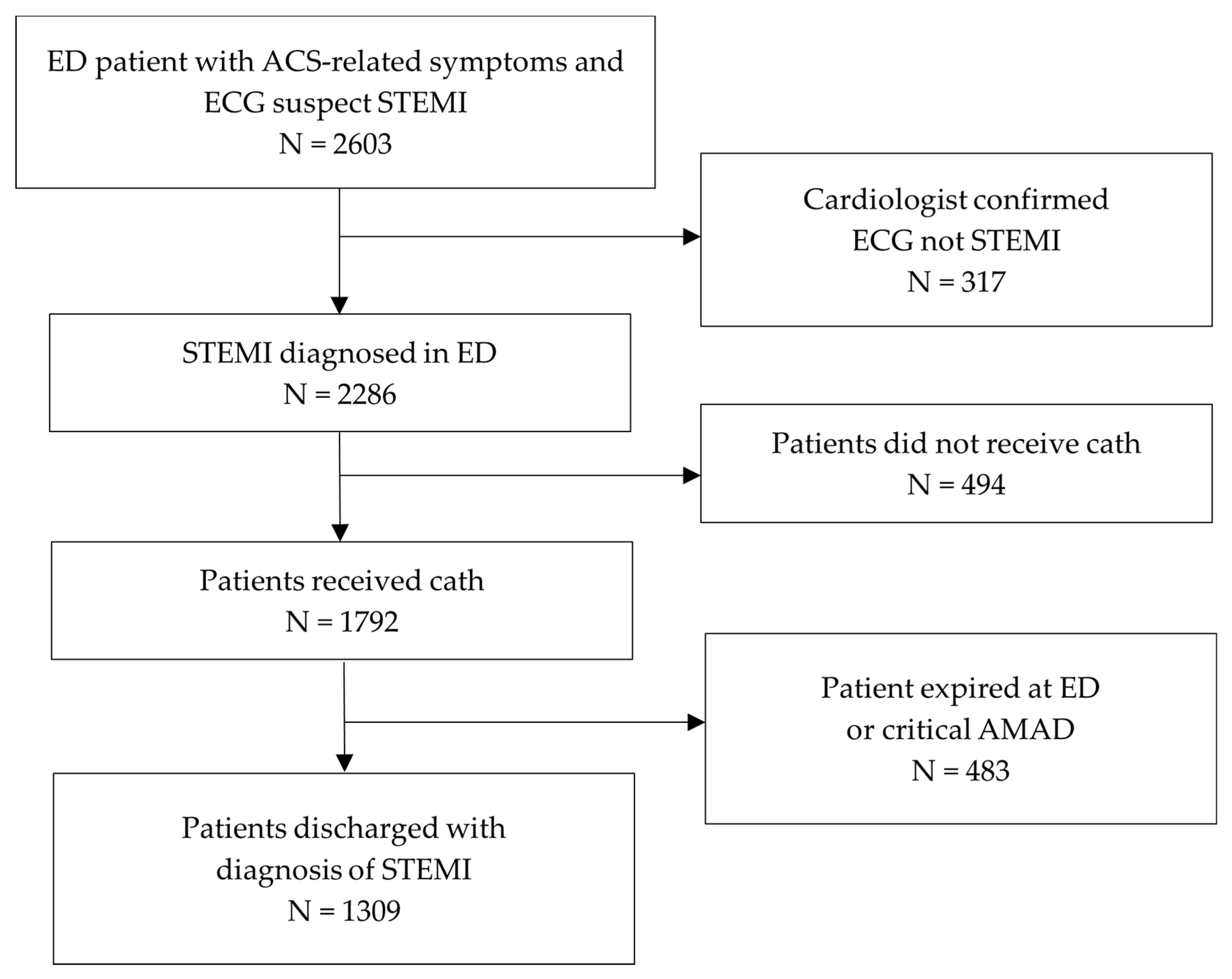
2.2. Patient Sampling
2.3. Data Collection and Outcome Measurement
2.4. Statistical Analysis
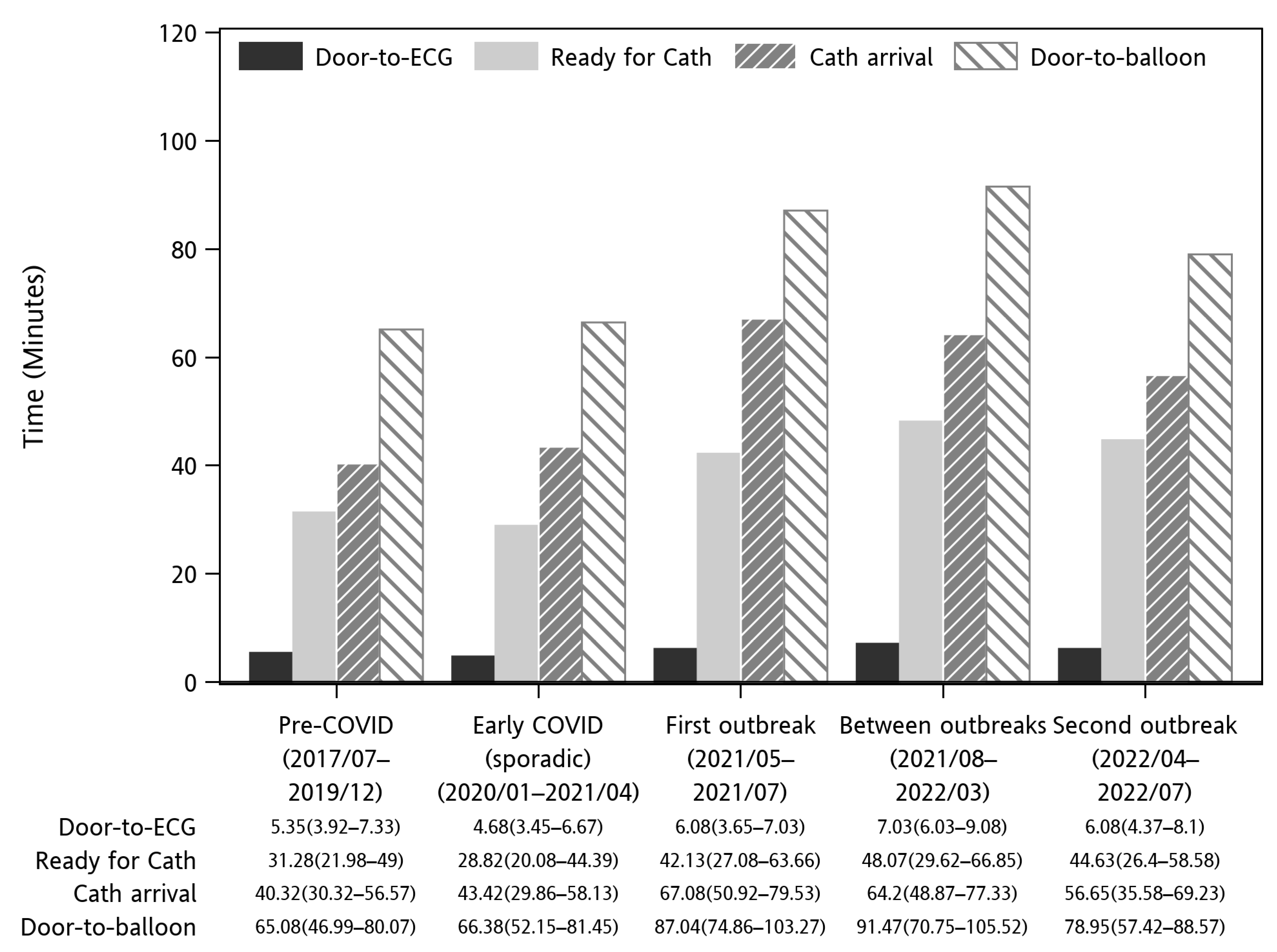
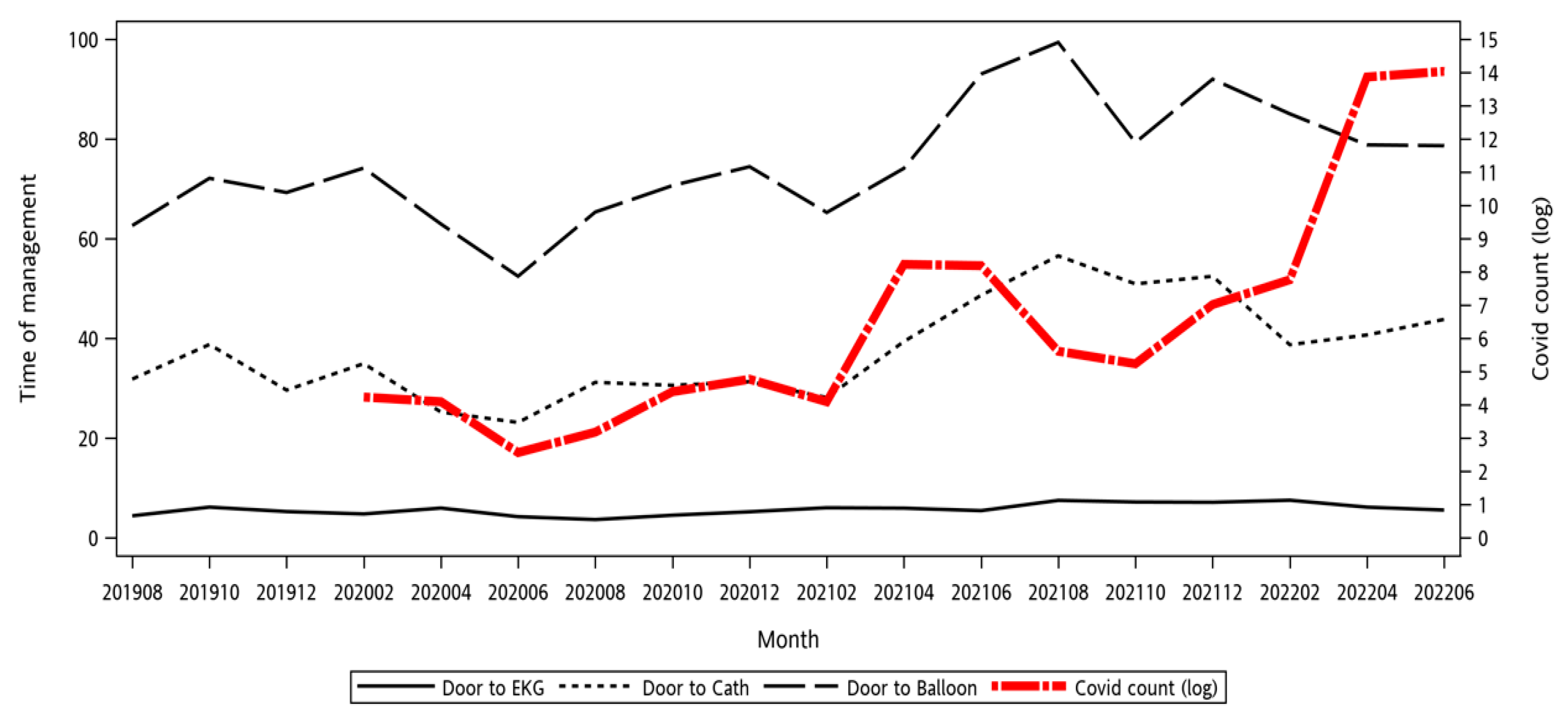
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| STEMI | ST-segment elevation myocardial infarction |
| IABP | Intra-aortic balloon pump |
| VA-ECMO | Veno-arterial extracorporeal membrane oxygenation |
| MV | Mechanical ventilation |
| ICU | Intensive care unit |
| COVID-19 | Coronavirus disease 2019 |
| SARS-CoV-2 | Severe acute respiratory syndrome CoV 2 |
| MI | Myocardial infarction |
| PPCI | Primary percutaneous coronary intervention |
| LCGMH | Chang Gung Memorial Hospital, Linkou Branch |
| ED | Emergency department |
| AMAD | Against medical advice |
| ACS | Acute coronary syndrome |
| ECG | Electrocardiogram |
| CGRD | Chang Gung Research Database |
| CDC | Centers for Disease Control |
| SD | Standard deviation |
| IQR | Interquartile range |
| SpO2 | Saturation of Peripheral Oxygen |
| OHCA | Out-of-Hospital Cardiac Arrest |
| CPK | Creatine Phosphokinase |
| MB | Creatine Kinase-MB |
| PCI | Percutaneous Coronary Intervention |
| CABG | Coronary Artery Bypass Grafting |
| Cath | Cathlab |
| ECG | Electrocardiogram |
| TOCC | Travel, Occupation, Contact, and Cluster |
References
- Taiwan Centers for Disease Control. Statistics Table of Area, Age, Sex of Death Cases—COVID-19 (by Month of Onset). 2024. Available online: https://data.cdc.gov.tw/dataset/death-statistics-cases-19cov?utm_source=chatgpt.com (accessed on 15 January 2025).
- Akhmetzhanov, A.R.; Cheng, H.-Y.; Linton, N.M.; Ponce, L.; Jian, S.-W.; Lin, H.-H. Transmission Dynamics and Effectiveness of Control Measures during COVID-19 Surge, Taiwan, April–August 2021. Emerg. Infect. Dis. 2022, 28, 2051–2059. [Google Scholar] [CrossRef]
- Chien, L.-C.; Beÿ, C.K.; Koenig, K.L. Taiwan’s Successful COVID-19 Mitigation and Containment Strategy: Achieving Quasi Population Immunity. Disaster Med. Public Health Prep. 2022, 16, 434–437. [Google Scholar] [CrossRef] [PubMed]
- Steinbrook, R. Lessons From the Success of COVID-19 Control in Taiwan. JAMA Intern. Med. 2021, 181, 922. [Google Scholar] [CrossRef] [PubMed]
- Haileamlak, A. The impact of COVID-19 on health and health systems. Ethiop. J. Health Sci. 2021, 31, 1073–1074. [Google Scholar] [PubMed]
- Ho, F.K.; Man, K.K.C.; Toshner, M.; Church, C.; Celis-Morales, C.; Wong, I.C.K.; Berry, C.; Sattar, N.; Pell, J.P. Thromboembolic Risk in Hospitalized and Nonhospitalized COVID-19 Patients: A Self-Controlled Case Series Analysis of a Nationwide Cohort. Mayo Clin. Proc. 2021, 96, 2587–2597. [Google Scholar] [CrossRef]
- Zahid, B.; Kamal, M.; Said, M.; Salem, M.; Elakabawi, K. Effect of COVID-19 pandemic on six-month mortality and clinical outcomes of patients with ST-elevation myocardial infarction. Adv. Interv. Cardiol. Postępy W Kardiol. Interwencyjnej 2022, 18, 228–236. [Google Scholar] [CrossRef]
- Garcia, S.; Albaghdadi, M.S.; Meraj, P.M.; Schmidt, C.; Garberich, R.; Jaffer, F.A.; Dixon, S.; Rade, J.J.; Tannenbaum, M.; Chambers, J.; et al. Reduction in ST-Segment Elevation Cardiac Catheterization Laboratory Activations in the United States During COVID-19 Pandemic. J. Am. Coll. Cardiol. 2020, 75, 2871–2872. [Google Scholar] [CrossRef]
- De Filippo, O.; D’Ascenzo, F.; Angelini, F.; Bocchino, P.P.; Conrotto, F.; Saglietto, A.; Secco, G.G.; Campo, G.; Gallone, G.; Verardi, R.; et al. Reduced Rate of Hospital Admissions for ACS during Covid-19 Outbreak in Northern Italy. N. Engl. J. Med. 2020, 383, 88–89. [Google Scholar] [CrossRef]
- Solomon, M.D.; McNulty, E.J.; Rana, J.S.; Leong, T.K.; Lee, C.; Sung, S.H.; Ambrosy, A.P.; Sidney, S.; Go, A.S. The Covid-19 Pandemic and the Incidence of Acute Myocardial Infarction. N. Engl. J. Med. 2020, 383, 691–693. [Google Scholar] [CrossRef]
- Mesnier, J.; Cottin, Y.; Coste, P.; Ferrari, E.; Schiele, F.; Lemesle, G.; Thuaire, C.; Angoulvant, D.; Cayla, G.; Bouleti, C.; et al. Hospital admissions for acute myocardial infarction before and after lockdown according to regional prevalence of COVID-19 and patient profile in France: A registry study. Lancet Public Health 2020, 5, e536–e542. [Google Scholar] [CrossRef]
- Watanabe, Y.; Miyachi, H.; Mozawa, K.; Yamada, K.; Oka, E.; Shiomura, R.; Sugizaki, Y.; Matsuda, J.; Nakata, J.; Tara, S.; et al. Impact of the COVID-19 Pandemic on ST-elevation Myocardial Infarction from a Single-center Experience in Tokyo. Intern. Med. 2021, 60, 3693–3700. [Google Scholar] [CrossRef] [PubMed]
- Meenakshisundaram, R.; Senthilkumaran, S.; Thirumalaikolundusubramanian, P.; Joy, M.; Jena, N.N.; Vadivelu, R.; Ayyasamy, S.; Chandrasekaran, V.P. Status of Acute Myocardial Infarction in Southern India During COVID-19 Lockdown: A Multicentric Study. Mayo Clin. Proc. Innov. Qual. Outcomes 2020, 4, 506–510. [Google Scholar] [CrossRef] [PubMed]
- Li, Y.H.; Huang, W.C.; Hwang, J.J. No Reduction of ST-segment Elevation Myocardial Infarction Admission in Taiwan During Coronavirus Pandemic. Am. J. Cardiol. 2020, 131, 133–134. [Google Scholar] [CrossRef] [PubMed]
- Butala, N.M.; Patel, N.K.; Chhatwal, J.; Vahdat, V.; Pomerantsev, E.V.; Albaghdadi, M.; Sakhuja, R.; Rosenzweig, A.; Elmariah, S. Patient and Provider Risk in Managing ST-Elevation Myocardial Infarction During the COVID-19 Pandemic: A Decision Analysis. Circ. Cardiovasc. Interv. 2020, 13, E010027. [Google Scholar] [CrossRef]
- Lee, C.Y.; Kuo, H.W.; Liu, Y.L.; Chuang, J.H.; Chou, J.H. Population-Based Evaluation of Vaccine Effectiveness against SARS-CoV-2 Infection, Severe Illness, and Death, Taiwan. Emerg. Infect. Dis. 2024, 30, 478–489. [Google Scholar] [CrossRef]
- St John Sutton, M.; Lee, D.; Rouleau, J.L.; Goldman, S.; Plappert, T.; Braunwald, E.; Pfeffer, M.A. Left ventricular remodeling and ventricular arrhythmias after myocardial infarction. Circulation 2003, 107, 2577–2582. [Google Scholar] [CrossRef]
- Mahmud, E.; Dauerman, H.L.; Welt, F.G.; Messenger, J.C.; Rao, S.V.; Grines, C.; Mattu, A.; Kirtane, A.J.; Jauhar, R.; Meraj, P.; et al. Management of acute myocardial infarction during the COVID-19 pandemic: A Consensus Statement from the Society for Cardiovascular Angiography and Interventions (SCAI), the American College of Cardiology (ACC), and the American College of Emergency Physicians (ACEP). Catheter. Cardiovasc. Interv. 2020, 96, 336–345. [Google Scholar] [CrossRef]
- Nallamothu, B.K.; Normand, S.L.; Wang, Y.; Hofer, T.P.; Brush, J.E., Jr.; Messenger, J.C.; Bradley, E.H.; Rumsfeld, J.S.; Krumholz, H.M. Relation between door-to-balloon times and mortality after primary percutaneous coronary intervention over time: A retrospective study. Lancet 2015, 385, 1114–1122. [Google Scholar] [CrossRef]
- De Luca, G.; Suryapranata, H.; Ottervanger, J.P.; Antman, E.M. Time delay to treatment and mortality in primary angioplasty for acute myocardial infarction: Every minute of delay counts. Circulation 2004, 109, 1223–1225. [Google Scholar] [CrossRef]
- De Luca, G.; van’t Hof, A.W.; de Boer, M.J.; Ottervanger, J.P.; Hoorntje, J.C.; Gosselink, A.T.; Dambrink, J.H.; Zijlstra, F.; Suryapranata, H. Time-to-treatment significantly affects the extent of ST-segment resolution and myocardial blush in patients with acute myocardial infarction treated by primary angioplasty. Eur. Heart J. 2004, 25, 1009–1013. [Google Scholar] [CrossRef]
- Terkelsen, C.J.; Sørensen, J.T.; Maeng, M.; Jensen, L.O.; Tilsted, H.H.; Trautner, S.; Vach, W.; Johnsen, S.P.; Thuesen, L.; Lassen, J.F. System delay and mortality among patients with STEMI treated with primary percutaneous coronary intervention. JAMA 2010, 304, 763–771. [Google Scholar] [CrossRef] [PubMed]
- De Rosa, S.; Spaccarotella, C.; Basso, C.; Calabrò, M.P.; Curcio, A.; Filardi, P.P.; Mancone, M.; Mercuro, G.; Muscoli, S.; Nodari, S.; et al. Reduction of hospitalizations for myocardial infarction in Italy in the COVID-19 era. Eur. Heart J. 2020, 41, 2083–2088. [Google Scholar] [CrossRef] [PubMed]
- Abdelaziz, H.K.; Patel, B.; Chalil, S.; Choudhury, T. COVID-19 Pandemic and Acute Myocardial Infarction: Management Protocol from a British Cardiac Centre. Crit. Pathw. Cardiol. 2020, 19, 55–57. [Google Scholar] [CrossRef]
- Chang Gung Medical Hospital Clinical Trial Center. Chang Gung Medical Hospital Clinical Trial Center—Linkou Branch. 2025. Available online: https://www1.cgmh.org.tw/intr/intr2/c3s400/profile-linkou.html (accessed on 13 February 2025).
- Lee, C.H.; Fang, C.C.; Tsai, L.M.; Gan, S.T.; Lin, S.H.; Li, Y.H. Patterns of Acute Myocardial Infarction in Taiwan from 2009 to 2015. Am. J. Cardiol. 2018, 122, 1996–2004. [Google Scholar] [CrossRef]
- Thompson, A.; Fleischmann, K.E.; Smilowitz, N.R.; de Las Fuentes, L.; Mukherjee, D.; Aggarwal, N.R.; Ahmad, F.S.; Allen, R.B.; Altin, S.E.; Auerbach, A.; et al. 2024 AHA/ACC/ACS/ASNC/HRS/SCA/SCCT/SCMR/SVM Guideline for Perioperative Cardiovascular Management for Noncardiac Surgery: A Report of the American College of Cardiology/American Heart Association Joint Committee on Clinical Practice Guidelines. J. Am. Coll. Cardiol. 2024, 84, 1869–1969. [Google Scholar] [CrossRef]
- Kwak, D.S.; Park, J. Analysis of the Prognosis Outcomes and Treatment Delay Among ST-Segment Elevation Myocardial Infarction Patients in Emergency Department Based on the Presence of Symptoms Suggestive of COVID-19. Int. J. Health Policy Manag. 2024, 13, 8207. [Google Scholar] [CrossRef]
- Sturkenboom, H.N.; van Hattem, V.A.E.; Nieuwland, W.; Paris, F.M.A.; Magro, M.; Anthonio, R.L.; Algin, A.; Lipsic, E.; Bruwiere, E.; Van den Branden, B.J.L.; et al. COVID-19-mediated patient delay caused increased total ischaemic time in ST-segment elevation myocardial infarction. Neth. Heart J. 2022, 30, 96–105. [Google Scholar] [CrossRef]
- McNamara, D.A.; VanOosterhout, S.; Klungle, D.; Busman, D.; Parker, J.L.; Kampfschulte, A.; Jovinge, S.; Wohns, D.; Madder, R.D. Pandemic-Associated Delays in Myocardial Infarction Presentation in Predominantly Rural Counties With Low COVID-19 Prevalence. Am. J. Cardiol. 2022, 169, 18–23. [Google Scholar] [CrossRef]
- Clodfelder, C.; Cooper, S.; Edwards, J.; Kraemer, J.; Ryznar, R.; LaPorta, A.; Meyers, M.; Shelton, R.; Chesnick, S. Delayed care in myocardial infarction and ischemic stroke patients during the COVID-19 pandemic. Am. J. Emerg. Med. 2022, 54, 326.e1–326.e4. [Google Scholar] [CrossRef]
- Choi, H.; Lee, J.H.; Park, H.K.; Lee, E.; Kim, M.S.; Kim, H.J.; Park, B.E.; Kim, H.N.; Kim, N.; Jang, S.Y.; et al. Impact of the COVID-19 Pandemic on Patient Delay and Clinical Outcomes for Patients With Acute Myocardial Infarction. J. Korean Med. Sci. 2022, 37, e167. [Google Scholar] [CrossRef]
- Pappagallo, S.; Tonizzo, M.; Colletta, M. Higher mortality in AMI during COVID 19 pandemia: Patient or system delay? Eur. Heart J. Suppl. 2021, 23 (Suppl. C), C75–C76. [Google Scholar] [CrossRef]
- McNamara, D.; Klungle, D.; Vanoosterhout, S.; Busman, D.; Parker, J.; Kampfschulte, A.R.; Wohns, D.; Jovinge, S.; Madder, R. Presentation delay among patients with ST-segment elevation myocardial infarction outside of a covid-19 hot zone. J. Am. Coll. Cardiol. 2021, 77, 3041. [Google Scholar] [CrossRef]
- Chen, C.C.; Tseng, C.Y.; Choi, W.M.; Lee, Y.C.; Su, T.H.; Hsieh, C.Y.; Chang, C.M.; Weng, S.L.; Liu, P.H.; Tai, Y.L.; et al. Taiwan Government-Guided Strategies Contributed to Combating and Controlling COVID-19 Pandemic. Front. Public. Health 2020, 8, 547423. [Google Scholar] [CrossRef] [PubMed]
- Oettinger, V.; Stachon, P.; Hilgendorf, I.; Heidenreich, A.; Zehender, M.; Westermann, D.; Kaier, K.; von Zur Muhlen, C. COVID-19 pandemic affects STEMI numbers and in-hospital mortality: Results of a nationwide analysis in Germany. Clin. Res. Cardiol. 2022, 112, 550–557. [Google Scholar] [CrossRef]
- Primessnig, U.; Pieske, B.M.; Sherif, M. Increased mortality and worse cardiac outcome of acute myocardial infarction during the early COVID-19 pandemic. ESC Heart Fail. 2021, 8, 333–343. [Google Scholar] [CrossRef]
- De Luca, G.; Algowhary, M.; Uguz, B.; Oliveira, D.C.; Ganyukov, V.; Zimbakov, Z.; Cercek, M.; Jensen, L.O.; Loh, P.H.; Calmac, L.; et al. COVID-19 pandemic, mechanical reperfusion and 30-day mortality in ST elevation myocardial infarction. Heart 2022, 108, 458–466. [Google Scholar] [CrossRef]
- Solano-López, J.; Zamorano, J.L.; Sanz, A.P.; Amat-Santos, I.; Sarnago, F.; Ibañes, E.G.; Sanchis, J.; Blas, J.R.R.; Gómez-Hospital, J.A.; Martínez, S.S.; et al. Risk factors for in-hospital mortality in patients with acute myocardial infarction during the COVID-19 outbreak. Rev. Esp. Cardiol. 2020, 73, 985–993. [Google Scholar] [CrossRef]
- Sarfraz, Z.; Sarfraz, A.; Sarfraz, M.; Zia, I.; Ali, M.Z.; Garimella, R.; Tebha, S.S.; Hussain, H.; Nadeem, Z.; Patel, G. Cardiovascular Disease, Intensive Care, and Mortality in Coronavirus Disease 2019 Patients: A Meta-Analysis. Turk. J. Anaesthesiol. Reanim. 2022, 50 (Suppl. 1), S15–S21. [Google Scholar] [CrossRef]
- Li, J.; Zhang, N.; Zhou, Z.; Huang, X.; Fang, W.; Yan, H.; Chen, J.; Wang, W.; Xiang, D.; Su, X.; et al. Twin peaks of in-hospital mortality among patients with STEMI across five phases of COVID-19 outbreak in China: A nation-wide study. Sci. China Life Sci. 2022, 65, 1855–1865. [Google Scholar] [CrossRef]
- Thyagaturu, H.; Sandhyavenu, H.; Titus, A.; Roma, N.; Gonuguntla, K.; Navinkumar Patel, N.; Hashem, A.; Dawn Abbott, J.; Balla, S.; Bhatt, D.L. Trends and Outcomes of Acute Myocardial Infarction During the Early COVID-19 Pandemic in the United States: A National Inpatient Sample Study. Korean Circ. J. 2024, 54, 710–723. [Google Scholar] [CrossRef]
- Zheng, W.; Reed, G.W.; Huded, C.; Kumar, A.; Kravitz, K.A.; Krishnaswamy, A.; Lincoff, A.M.; Meldon, S.; Kralovic, D.M.; Kapadia, S.R.; et al. Impact of COVID-19 pandemic on door-toballoon time and mortality within a high reliability STEMI system of care. Circulation 2021, 144 (Suppl. S1), A13721. [Google Scholar] [CrossRef]
- Shavelle, D.M.; Bosson, N.; French, W.J.; Thomas, J.L.; Niemann, J.T.; Gausche-Hill, M.; Rollman, J.E.; Rafique, A.M.; Klomhaus, A.M.; Kloner, R.A. Association of the COVID-19 Pandemic on Treatment Times for ST-Elevation Myocardial Infarction: Observations from the Los Angeles County Regional System. Am. J. Cardiol. 2024, 213, 93–98. [Google Scholar] [CrossRef]
- Kobayashi, S.; Sakakura, K.; Jinnouchi, H.; Taniguchi, Y.; Tsukui, T.; Watanabe, Y.; Yamamoto, K.; Seguchi, M.; Wada, H.; Fujita, H. Comparison of door-to-balloon time and in-hospital outcomes in patients with ST-elevation myocardial infarction between before versus after COVID-19 pandemic. Cardiovasc. Interv. Ther. 2022, 37, 641–650. [Google Scholar] [CrossRef] [PubMed]
- Range, G.; Hakim, R.; Beygui, F.; Angoulvant, D.; Marcollet, P.; Godin, M.; Deballon, R.; Bonnet, P.; Fichaux, O.; Barbey, C.; et al. Incidence, delays, and outcomes of STEMI during COVID-19 outbreak: Analysis from the France PCI registry. J. Am. Coll. Emerg. Physicians Open 2020, 1, 1168–1176. [Google Scholar] [CrossRef] [PubMed]
- Ministry of Health and Welfare. Taiwan National Infectious Disease Statistics System. 2023. Available online: https://nidss.cdc.gov.tw/en/Home/Index?op=6 (accessed on 31 December 2024).
| Variables | Total (N = 1309) | Group 1 2017–2019 (N = 598) | Group 2 2020–2022 (N = 711) | p-Value |
|---|---|---|---|---|
| Age ¥ | 62 (53–70) | 60 (52–69) | 63 (53–71) | 0.0008 * |
| Male sex, n (%) | 1068 (81.5) | 483 (80.7) | 585 (82.2) | 0.5285 |
| SpO2 (%) ¶ | 93.4 (16.4) | 94.2 (14.4) | 92.8 (18) | 0.1299 |
| Shock at triage, n (%) | 172 (13.5) | 93 (16.0) | 79 (11.4) | 0.0224 * |
| OHCA, n (%) | 33 (2.5) | 11 (1.8) | 22 (3.1) | 0.2041 |
| Chest pain, n (%) | 48 (3.6) | 27 (4.5) | 21 (2.9) | 0.1771 |
| Peak troponin (ng/mL) ¶ | 13.0 (23.8) | 10.3 (21.5) | 15.0 (25.2) | 0.0047 * |
| CPK (U/L) ¶ | 1394.9 (1842.9) | 1349.2 (1768.4) | 1433.3 (1903.9) | 0.4585 |
| MB (ng/mL) ¶ | 8.1 (7.6) | 9.0 (8.4) | 7.4 (6.7) | 0.0011 * |
| Past medical history | ||||
| Hypertension, n (%) | 822 (62.8) | 389 (65.0) | 433 (60.9) | 0.1362 |
| Diabetes mellitus, n (%) | 572 (43.7) | 267 (44.6) | 305 (42.9) | 0.5616 |
| Cigarette smoking, n (%) | 597 (45.6) | 282 (47.1) | 315 (44.3) | 0.3287 |
| Prior PCI, n (%) | 412 (31.4) | 244 (40.8) | 168 (23.6) | <0.0001 * |
| Prior CABG, n (%) | 19 (1.4) | 12 (2.0) | 7 (0.9) | 0.1908 |
| Prior stroke, n (%) | 178 (13.6) | 74 (12.3) | 104 (14.6) | 0.2698 |
| Outcomes | ||||
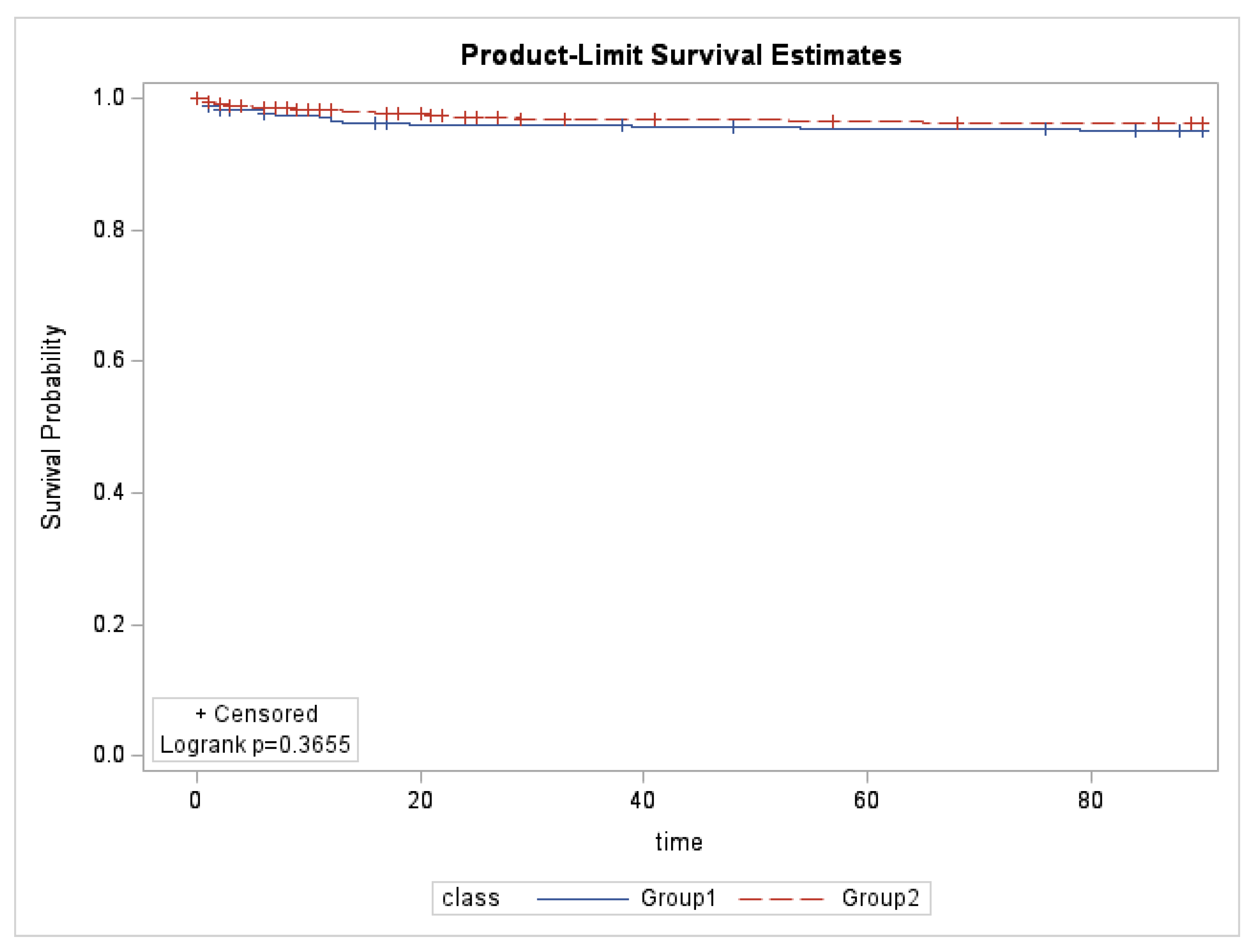
| In-hospital mortality, n (%) | 85 (6.4) | 35 (5.8) | 50 (7.0) | 0.4532 |
| 3-month mortality, n (%) | 114 (8.7) | 48 (8.0) | 66 (9.2) | 0.4812 |
| IABP, n (%) | 20 (1.5) | 6 (1) | 14 (1.9) | 0.2330 |
| VA-ECMO, n (%) | 19 (1.4) | 3 (0.5) | 16 (2.2) | 0.0163 * |
| MV, n (%) | 43 (3.2) | 18 (3.0) | 25 (3.5) | 0.7217 |
| Inotropic support, n (%) | 272 (20.7) | 118 (19.7) | 154 (21.6) | 0.4309 |
| Days of hospital stay ¶ | 8.1 (7.4) | 7.8 (6.5) | 8.4 (8.1) | 0.1300 |
| Days of ICU stay ¶ | 4.1 (4.2) | 3.9 (3.5) | 4.2 (4.8) | 0.1107 |
| Door-to-complete triage ¥ | 3.6 (2.1–6.5) | 3.5 (1.9–6.1) | 3.9 (2.2–6.7) | 0.0284 * |
| Door-to-EKG ¥ | 5.6 (3.9–7.6) | 5.3 (3.9–7.3) | 5.9 (3.9–7.8) | 0.0682 |
| Door-to-consultation ¥ | 8.1 (5.4–11.4) | 7.6 (4.9–10.5) | 8.8 (5.9–11.9) | <0.0001 * |
| Door-to-ready for cath ¥ | 33.1 (22.1–53.4) | 31.2 (21.9–49.0) | 35.3 (22.4–56.8) | 0.0163 * |
| Door-to-cath arrival ¥ | 51.6 (35.3–68.0) | 40.3 (30.3–56.5) | 53.2 (36.1–68.7) | 0.0335 * |
| Door-to-balloon ¥ | 74.4 (56.6–89.4) | 65.0 (46.9–80.0) | 74.9 (57.4–89.7) | 0.0143 * |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Published by MDPI on behalf of the Lithuanian University of Health Sciences. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Yang, C.-H.; Lin, Y.-J.; Gao, S.-Y.; Chen, W.-C.; Chaou, C.-H. Impact of the Coronavirus Disease 2019 Pandemic on the Management and Outcomes of ST-Segment Elevation Myocardial Infarction Patients: A Retrospective Cohort Study. Medicina 2025, 61, 422. https://doi.org/10.3390/medicina61030422
Yang C-H, Lin Y-J, Gao S-Y, Chen W-C, Chaou C-H. Impact of the Coronavirus Disease 2019 Pandemic on the Management and Outcomes of ST-Segment Elevation Myocardial Infarction Patients: A Retrospective Cohort Study. Medicina. 2025; 61(3):422. https://doi.org/10.3390/medicina61030422
Chicago/Turabian StyleYang, Cheng-Han, Yu-Jen Lin, Shi-Ying Gao, Wei-Chen Chen, and Chung-Hsien Chaou. 2025. "Impact of the Coronavirus Disease 2019 Pandemic on the Management and Outcomes of ST-Segment Elevation Myocardial Infarction Patients: A Retrospective Cohort Study" Medicina 61, no. 3: 422. https://doi.org/10.3390/medicina61030422
APA StyleYang, C.-H., Lin, Y.-J., Gao, S.-Y., Chen, W.-C., & Chaou, C.-H. (2025). Impact of the Coronavirus Disease 2019 Pandemic on the Management and Outcomes of ST-Segment Elevation Myocardial Infarction Patients: A Retrospective Cohort Study. Medicina, 61(3), 422. https://doi.org/10.3390/medicina61030422






