Kinetics of Serum-Free Light Chain Removal by High-Cutoff Hemodialysis in Patients with Multiple Myeloma and Acute Renal Failure
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design and Participants
2.2. Chemotherapy
2.3. HCO Treatment
2.4. Measurement of sFLCs and Their Clearance by HCO Dialysis
2.5. Statistical Analysis
3. Results
3.1. Patient Characteristics
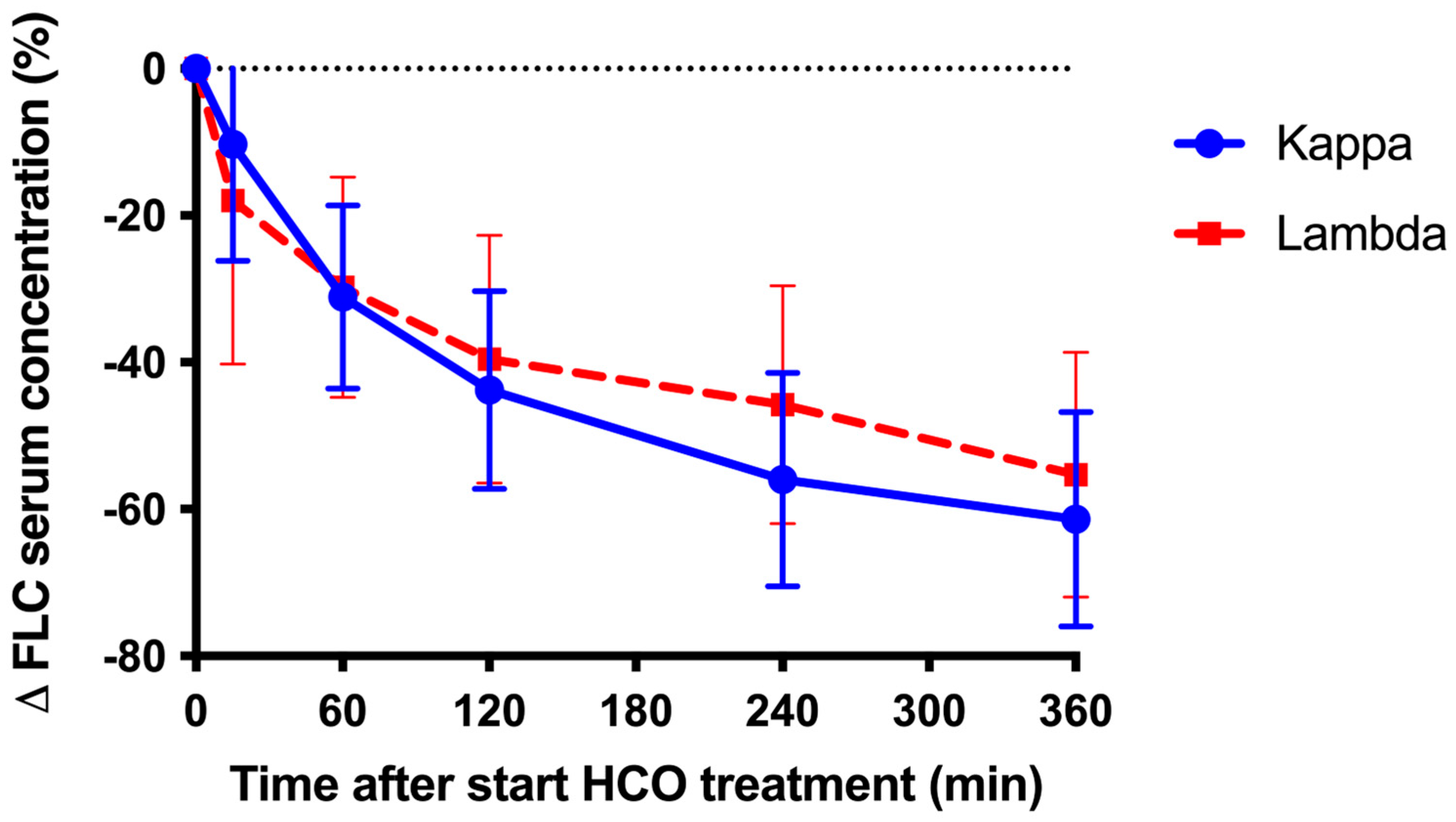
3.2. Effect of a Single HCO Dialysis on SFLCs
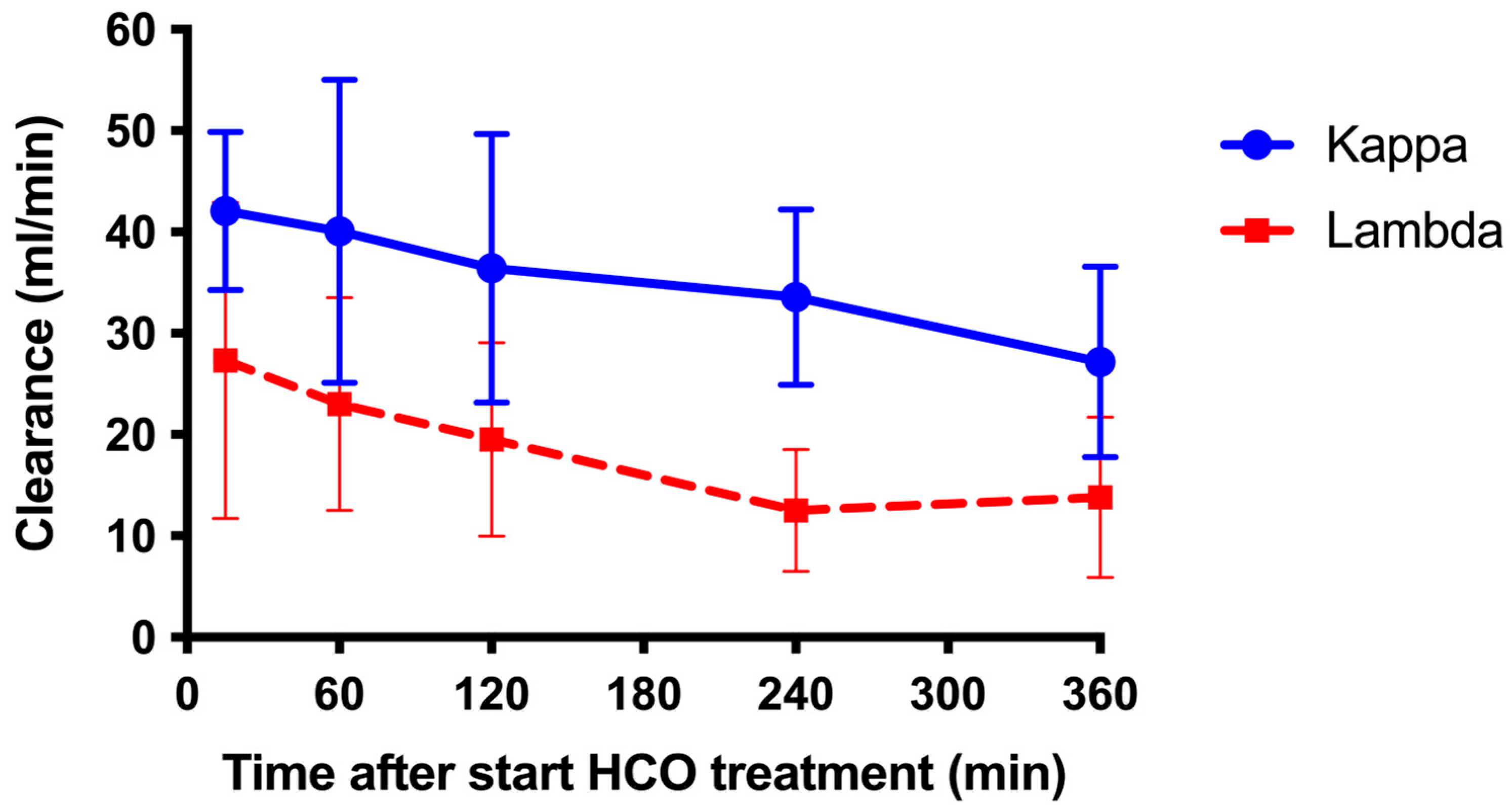
3.3. Clearance of sFLCs by HCO Dialysis
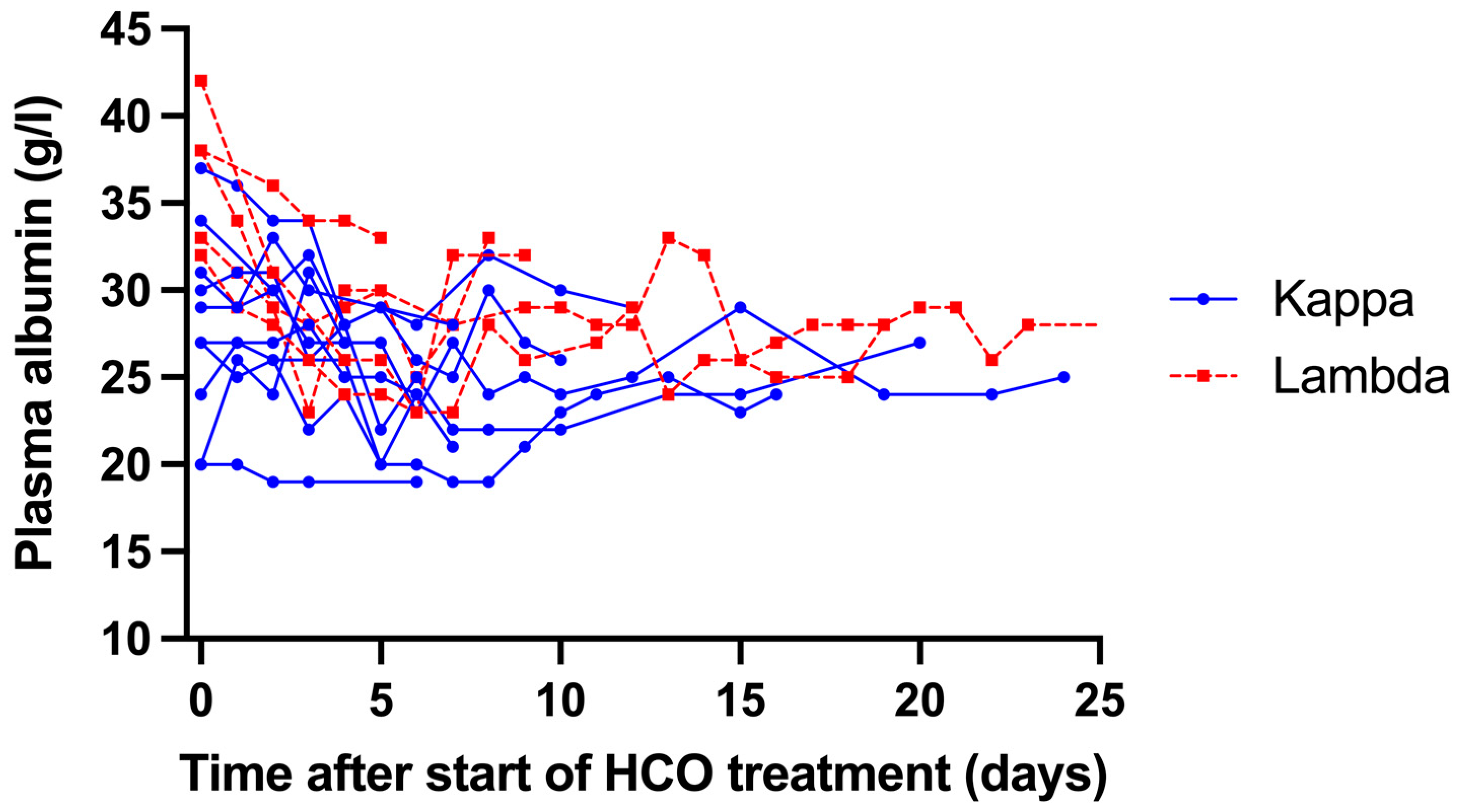
3.4. Adverse Effects
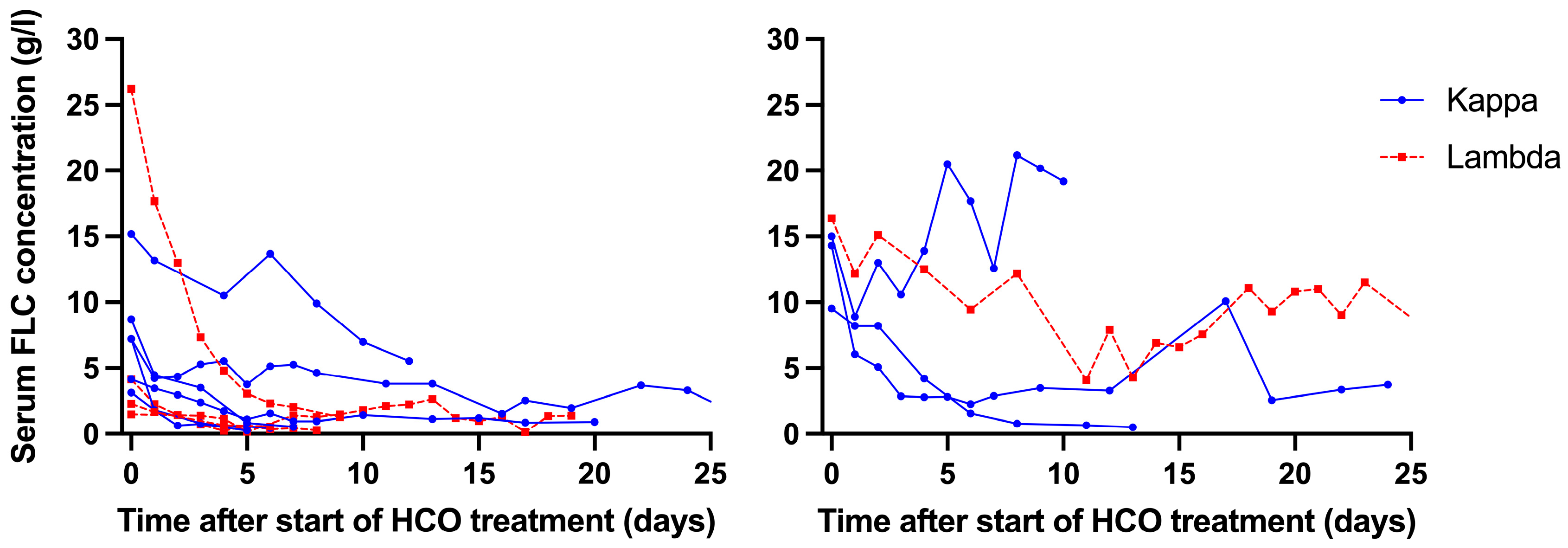
3.5. Long-Term Outcomes
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Bridoux, F.; Leung, N.; Belmouaz, M.; Royal, V.; Ronco, P.; Nasr, S.H.; Fermand, J.P. Management of acute kidney injury in symptomatic multiple myeloma. Kidney Int. 2021, 99, 570–580. [Google Scholar] [CrossRef] [PubMed]
- Leung, N.; Rajkumar, S.V. Multiple myeloma with acute light chain cast nephropathy. Blood Cancer J. 2023, 13, 46. [Google Scholar] [CrossRef] [PubMed]
- Hutchison, C.A.; Bradwell, A.R.; Cook, M.; Basnayake, K.; Basu, S.; Harding, S.; Hattersley, J.; Evans, N.D.; Chappel, M.J.; Sampson, P.; et al. Treatment of acute renal failure secondary to multiple myeloma with chemotherapy and extended high cut-off hemodialysis. Clin. J. Am. Soc. Nephrol. 2009, 4, 745–754. [Google Scholar] [CrossRef] [PubMed]
- Hutchison, C.A.; Cockwell, P.; Moroz, V.; Bradwell, A.R.; Fifer, L.; Gillmore, J.D.; Jesky, M.D.; Storr, M.; Wessels, J.; Winearls, C.G.; et al. High cutoff versus high-flux haemodialysis for myeloma cast nephropathy in patients receiving bortezomib-based chemotherapy (EuLITE) a phase 2 randomised controlled trial. Lancet Haematol. 2019, 6, e217–e228. [Google Scholar] [CrossRef] [PubMed]
- Kleber, M.; Ihorst, G.; Terhorst, M.; Koch, B.; Deschler, B.; Wäsch, R.; Engelhardt, M. Comorbidity as a prognostic variable in multiple myeloma: Comparative evaluation of common comorbidity scores and use of a novel MM–comorbidity score. Blood Cancer J. 2011, 16, e35. [Google Scholar] [CrossRef] [PubMed]
- Hutchison, C.A.; Cockwell, P.; Stringer, S.; Bradwell, A.; Cook, M.; Gertz, M.A.; Dispenzieri, A.; Winters, J.L.; Kumar, S.; Rajkumar, S.V.; et al. Early reduction in serum-free light chains associates with renal recovery in myeloma kidney. Clin. J. Am. Soc. Nephrol. 2011, 22, 1129–1136. [Google Scholar] [CrossRef] [PubMed]
- Hutchison, C.A.; Cockwell, P.; Reid, S.; Chandler, K.; Mead, G.P.; Harrison, J.; Hattersley, J.; Evans, N.D.; Chappell, M.J.; Cook, M.; et al. Efficient removal of immunoglobulin free light chains by hemodialysis for multiple myeloma: In vitro and In vivo studies. J. Am. Soc. Nephrol. 2007, 18, 886–895. [Google Scholar] [CrossRef] [PubMed]
- Hutchison, C.A.; Harding, S.; Mead, G.; Goehl, H.; Storr, M.; Bradwell, A.; Cockwell, P. Serum free-light chain removal by high cutoff hemodialysis: Optimizing removal and supportive care. Artif. Organs 2008, 32, 910–917. [Google Scholar] [CrossRef] [PubMed]
- Hutchison, C.A.; Heyne, N.; Airia, P.; Schindler, R.; Zickler, D.; Cook, M.; Cockwell, P.; Grima, D. Immunoglobulin free light chain levels and recovery from myeloma kidney on treatment with chemotherapy and high cut-off haemodialysis. Nephrol. Dial. Transplant. 2012, 27, 3823–3828. [Google Scholar] [CrossRef] [PubMed]
- Peters, N.O.; Laurain, E.; Cridlig, J.; Hulin, C.; Cao-Huu, T.; Frimat, L. Impact of free light chain hemodialysis in myeloma cast nephropathy: A case-control study. Hemodial. Int. 2011, 15, 538–545. [Google Scholar] [CrossRef] [PubMed]
- Zannetti, B.A.; Zamagni, E.; Santostefano, M.; De Sanctis, L.B.; Tacchetti, P.; Mancini, E.; Pantani, L.; Brioli, A.; Rizzo, R.; Mancuso, K.; et al. Bortezomib-based therapy combined with high cut-off hemodialysis is highly effective in newly diagnosed multiple myeloma patients with severe renal impairment. Am. J. Hematol. 2015, 90, 647–652. [Google Scholar] [CrossRef] [PubMed]
- Bridoux, F.; Carron, P.-L.; Pegourie, B.; Alamartine, E.; Augeul-Meunier, K.; Karras, A.; Joly, B.; Peraldi, M.-N.; Arnulf, B.; Vigneau, C.; et al. Effect of high-cutoff hemodialysis vs. conventional hemodialysis on hemodialysis independence among patients with myeloma cast nephropathy. JAMA 2017, 318, 2099–2110. [Google Scholar] [CrossRef] [PubMed]
- Steiner, N.; Hamid, A.A.; Kronbichler, A.; Neuwirt, H.; Myslivecek, M.; Kollar, M.; Lachmanova, J.; Rysava, R.; Hruskova, Z.; Spicka, I.; et al. Real world analysis of high-Cut-Off (Hco) hemodialysis with bortezomib based backbone therapy in patients with multiple myeloma and acute kidney injury. J. Nephrol. 2021, 34, 1263–1270. [Google Scholar] [CrossRef] [PubMed]
- van Gelder, M.K.; Abrahams, A.C.; Joles, J.A.; Kaysen, G.A.; Gerritsen, K.G.F. Albumin handling in different hemodialysis modalities. Nephrol. Dial. Transplant. 2018, 33, 906–913. [Google Scholar] [CrossRef] [PubMed]
- Hughes, M.S.; Balev, M.; Radhakrishnan, J.; Bhutani, D.; Mapara, M.; Lentzsch, S.; Chakraborty, R. Improved outcomes of myeloma cast nephropathy in newly diagnosed multiple myeloma with modern anti-myeloma therapies. Eur. J. Hematol. 2025, 114, 990–1000. [Google Scholar] [CrossRef] [PubMed]
| ID | M/F | Age (yr) | sFLC Type | New Diagnosis (N) or Relapse (R) | Chemotherapy | sFLC at Diagnosis (g/L) | Nr of HCO Treatments | Duration of HCO Treatment (days) | sFLC Reduction During First Treatment (%) | Mean sFLC Reduction During First 2 Treatments (%) | Patient Status at 1 yr After Start of HCO Treatment | Independence from Dialysis at Stop of HCO Treatment | Renal Function at Follow-Up (eGFR in mL/min/1.72 m2; Creatinine Clearance in mL/min) | ||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 3 Months After Start of HCO Treatment | 6 Months After Start of HCO Treatment | 12 Months After Start of HCO Treatment | |||||||||||||
| 1 | F | 66 | Kappa | F | Bortezomib, dexamethasone | 9.5 | 7 | 13 | 33.0 | 58.6 | Died (3 months after start HCO) | No | Dialysis- dependent | Dialysis- dependent | Dialysis- dependent |
| 2 | M | 70 | Lambda | F | Bortezomib, dexamethasone, doxorubicin | 16.4 | 39 | 75 | 50.2 | 46.6 | Alive | No | Dialysis-dependent | Dialysis-dependent | Dialysis- dependent |
| 3 | M | 63 | Kappa | F | Bortezomib, dexamethasone, doxorubicin | 8.7 | 5 | 7 | 73.0 | 76.9 | Alive | Yes | eGFR 29 CC 32 | eGFR 42 CC 55 | eGFR 37 CC 45 |
| 4 | M | 53 | Lambda | R | Bortezomib, dexamethasone | 2.3 | 4 | 6 | 59.4 | 62.6 | Alive | Yes | eGFR 51 CC 68 | eGFR 56 CC | NA Died |
| 5 | M | 62 | Kappa | R | Bortezomib, dexamethasone | 1.5 | 6 | 6 | 64.8 | 61.1 | Alive | Yes | eGFR 56 CC 16 | eGFR NA CC NA | eGFR: NA CC NA |
| 6 | F | 70 | Lambda | F | Bortezomib, dexamethasone | 26.2 | 10 | 10 | 29.0 | 29.3 | Died (5 months after start of HCO) | Yes | eGFR 98 CC 23 | NA Died | NA Died |
| 7 | M | 81 | Kappa | R | Bortezomib, prednisolone, melphalan | 4.2 | 12 | 20 | 74.2 | 70.7 | Alive | Yes | eGFR 25 CC 30 | eGFR NA CC NA | NA |
| 8 | M | 53 | Kappa | R | Bortezomib, dexamethasone, lenalidomide | 15.0 | 12 | 12 | 43.4 | 37.5 | Died (1 month after start of HCO) | No | NA Died | NA Died | NA Died |
| 9 | M | 64 | Kappa | F | Bortezomib, dexamethasone | 15.2 | 9 | 12 | 46.6 | 53.0 | Alive | Yes | eGFR 22 CC NA | eGFR 29 CC NA | eGFR 35 CC NA |
| 10 | M | 79 | Kappa | F | Bortezomib, dexamethasone | 7.2 | 5 | 5 | 85.4 | 66.1 | Alive | Yes | eGFR 9 CC 19 | eGFR 11 CC 15 | eGFR 12 CC 17 |
| 11 | M | 62 | Kappa | F | Bortezomib, dexamethasone | 7.2 | 16 | 36 | 81.8 | 63.5 | Alive | Yes | eGFR 46 CC 65 | eGFR 51 CC NA | eGFR 57 CC 72 |
| 12 | M | 84 | Kappa | F | Bortezomib, dexamethasone | 14.3 | 14 | 25 | 56.7 | 49.8 | Alive | No | Dialysis-dependent | Dialysis-dependent | Dialysis- dependent |
| 13 | M | 63 | Kappa | F | Bortezomib, dexamethasone, thalidomide | 3.1 | 5 | 6 | 63.7 | 56.3 | Alive | Yes | eGFR 31 CC 40 | eGFR 36 CC 86 | eGFR 32 CC 64 |
| 14 | F | 64 | Lambda | R | Bortezomib, dexamethasone, daratumumab | 4.1 | 9 | 9 | 71.4 | 68.5 | Alive | Yes | eGFR 23 CC 27 | eGFR 29 CC 26 | eGFR 27 CC 39 |
| 15 | M | 79 | Lambda | F | Bortezomib, dexamethasone, daratumumab | 1.5 | 17 | 19 | 66.3 | 59.1 | Died (1 month after start HCO) | Yes | NA Died | NA | NA |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Published by MDPI on behalf of the Lithuanian University of Health Sciences. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Veldman, W.A.; Weerman, D.J.; Molog, S.; Diepenbroek, A.; Roeloffzen, W.W.H.; Stegeman, C.A.; Franssen, C.F.M. Kinetics of Serum-Free Light Chain Removal by High-Cutoff Hemodialysis in Patients with Multiple Myeloma and Acute Renal Failure. Medicina 2025, 61, 1977. https://doi.org/10.3390/medicina61111977
Veldman WA, Weerman DJ, Molog S, Diepenbroek A, Roeloffzen WWH, Stegeman CA, Franssen CFM. Kinetics of Serum-Free Light Chain Removal by High-Cutoff Hemodialysis in Patients with Multiple Myeloma and Acute Renal Failure. Medicina. 2025; 61(11):1977. https://doi.org/10.3390/medicina61111977
Chicago/Turabian StyleVeldman, Wilma A., Debora J. Weerman, Saskia Molog, Adry Diepenbroek, Wilfried W. H. Roeloffzen, Coen A. Stegeman, and Casper F. M. Franssen. 2025. "Kinetics of Serum-Free Light Chain Removal by High-Cutoff Hemodialysis in Patients with Multiple Myeloma and Acute Renal Failure" Medicina 61, no. 11: 1977. https://doi.org/10.3390/medicina61111977
APA StyleVeldman, W. A., Weerman, D. J., Molog, S., Diepenbroek, A., Roeloffzen, W. W. H., Stegeman, C. A., & Franssen, C. F. M. (2025). Kinetics of Serum-Free Light Chain Removal by High-Cutoff Hemodialysis in Patients with Multiple Myeloma and Acute Renal Failure. Medicina, 61(11), 1977. https://doi.org/10.3390/medicina61111977







