Assessment of Sedation in Mechanically Ventilated Children with Severe Acute Bronchiolitis: Correlation Between COMFORT-B Scale and Bispectral Index During Continuous Infusion of Fentanyl and Midazolam
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design and Ethical Considerations
2.2. Study Population
2.3. Data Collection
2.4. Statistical Analysis
2.4.1. Descriptive Statistics
2.4.2. Correlation Analysis
2.4.3. Simple Moving Average Trend Analysis
2.4.4. Linear Mixed Effects
2.4.5. Random Forest
3. Results
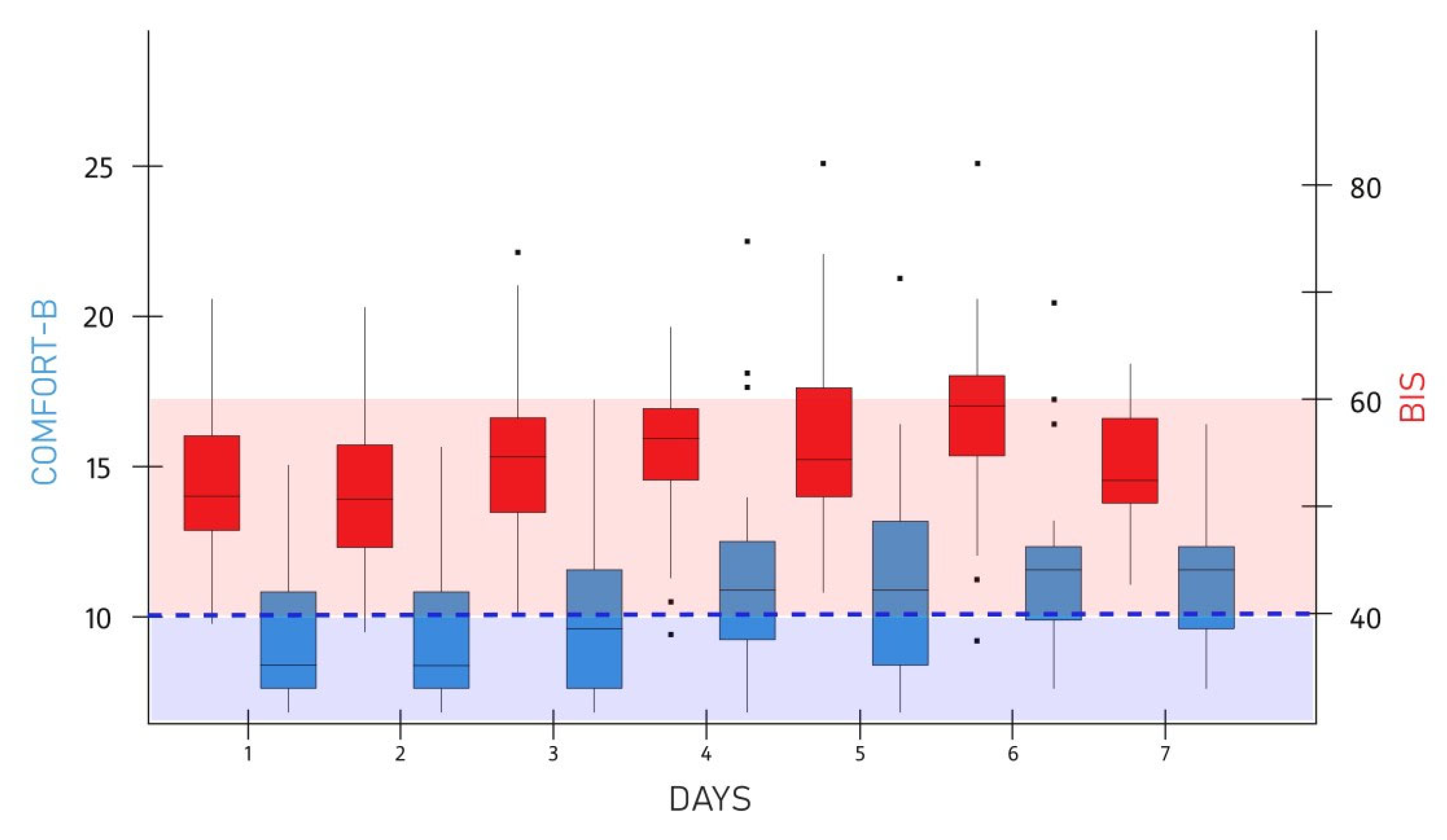
3.1. Statistical Analysis of the Entire Cohort
3.2. Statistical Analysis of the Subgroups of Patients
3.2.1. Age
3.2.2. Administration of Neuromuscular Blockers
3.2.3. Degree of Sedation
3.3. Linear Mixed Effects
3.4. Random Forest
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| BIS | Bispectral Index |
| CCF | Cross-correlation function |
| COMFORT-B | A behavioral unobtrusive method of measuring distress in unconscious and ventilated infants, children and adolescence |
| EEG | Electroencephalography |
| ICE | Individual conditional expectation |
| LOOCV | Leave-one-out cross-validation |
| NMB | Neuromuscular blocker |
| PICU | Pediatric intensive care unit |
| RMSE | Root mean square error |
| SD | Standard deviation |
References
- Malviya, S.; Voepel-Lewis, T.; Tait, A.R.; Merkel, S. Sedation/Analgesia for Diagnostic and Therapeutic Procedures in Children. J. Perianesth. Nurs. 2000, 15, 415–422. [Google Scholar] [CrossRef]
- Egelhoff, J.C.; Ball, W.S.; Koch, B.L.; Parks, T.D. Safety and Efficacy of Sedation in Children Using a Structured Sedation Program. Am. J. Roentgenol. 1997, 168, 1259–1262. [Google Scholar] [CrossRef]
- Brinker, D. Sedation and Comfort Issues in the Ventilated Infant and Child. Crit. Care Nurs. Clin. N. Am. 2004, 16, 365–377. [Google Scholar] [CrossRef]
- Playfor, S.D.; Thomas, D.A.; Choonara, I. Sedation and Neuromuscular Blockade in Paediatric Intensive Care: A Review of Current Practice in the UK. Pediatr. Anesth. 2003, 13, 147–151. [Google Scholar] [CrossRef] [PubMed]
- Desbiens, N.A.; Wu, A.W.; Broste, S.K.; Wenger, N.S.; Connors, A.F.; Lynn, J.; Yasui, Y.; Phillips, R.S.; Fulkerson, W. Pain and Satisfaction with Pain Control in Seriously Ill Hospitalized Adults: Findings from the Support Research Investigations. Crit. Care Med. 1996, 24, 1953–1961. [Google Scholar] [CrossRef] [PubMed]
- Martin, L.D.; Bratton, S.L.; Quint, P.; Mayock, D.E. Prospective Documentation of Sedative, Analgesic, and Neuromuscular Blocking Agent Use in Infants and Children in the Intensive Care Unit: A Multicenter Perspective. Pediatr. Crit. Care Med. 2001, 2, 205–210. [Google Scholar] [CrossRef] [PubMed]
- Ista, E.; van Dijk, M.; Tibboel, D.; de Hoog, M. Assessment of Sedation Levels in Pediatric Intensive Care Patients Can Be Improved by Using the Comfort “Behavior” Scale. Pediatr. Crit. Care Med. 2005, 6, 58–63. [Google Scholar] [CrossRef]
- Marx, C.M.; Smith, P.G.; Lowrie, L.H.; Hamlett, K.W.; Ambuel, B.; Yamashita, T.S.; Blumer, J.L. Optimal Sedation of Mechanically Ventilated Pediatric Critical Care Patients. Crit. Care Med. 1994, 22, 163–170. [Google Scholar] [CrossRef]
- Silva, C.D.C.; Alves, M.M.O.; El Halal, M.G.D.S.; Pinheiro, S.D.S.; Carvalho, P.R.A. A Comparison of Gradual Sedation Levels Using the Comfort-B Scale and Bispectral Index in Children on Mechanical Ventilation in the Pediatric Intensive Care Unit. Rev. Bras. Ter. Intensiv. 2013, 25, 306–311. [Google Scholar] [CrossRef]
- Sigl, J.C.; Chamoun, N.G. An Introduction to Bispectral Analysis for the Electroencephalogram. J. Clin. Monit. Comput. 1994, 10, 392–404. [Google Scholar] [CrossRef]
- Sebel, P.S.; Lang, E.; Rampil, I.J.; White, P.F.; Cork, R.; Jopling, M.; Smith, N.T.; Glass, P.S.; Manberg, P. A Multicenter Study of Bispectral Electroencephalogram Analysis for Monitoring Anesthetic Effect. Anesth. Analg. 1997, 84, 891–899. [Google Scholar] [CrossRef]
- McDermott, N.B.; VanSickle, T.; Motas, D.; Friesen, R.H. Validation of the Bispectral Index Monitor During Conscious and Deep Sedation in Children. Anesth. Analg. 2003, 97, 39–43. [Google Scholar] [CrossRef]
- Kussman, B.D.; Gruber, E.M.; Zurakowski, D.; Hansen, D.D.; Sullivan, L.J.; Laussen, P.C. Bispectral index monitoring during infant cardiac surgery: Relationship of BIS to the stress response and plasma fentanyl levels. Pediatr. Anesth. 2001, 11, 663–669. [Google Scholar] [CrossRef]
- Agrawal, D.; Feldman, H.A.; Krauss, B.; Waltzman, M.L. Bispectral index monitoring quantifies depth of sedation during emergency department procedural sedation and analgesia in children. Ann. Emerg. Med. 2004, 43, 247–255. [Google Scholar] [CrossRef]
- Haberland, C.M.; Baker, S.; Liu, H. Bispectral index monitoring of sedation depth in pediatric dental patients. Anesth. Prog. 2011, 58, 66–72. [Google Scholar] [CrossRef] [PubMed]
- Eisermann, M.; Kaminska, A.; Moutard, M.L.; Soufflet, C.; Plouin, P. Normal Eeg in Childhood: From Neonates to Adolescents. Neurophysiol. Clin. 2013, 43, 35–65. [Google Scholar] [CrossRef] [PubMed]
- Malviya, S.; Voepel-Lewis, T.; Tait, A.R.; Watcha, M.F.; Sadhasivam, S.; Friesen, R.H. Effect of Age and Sedative Agent on the Accuracy of Bispectral Index in Detecting Depth of Sedation in Children. Pediatrics 2007, 120, e461–e470. [Google Scholar] [CrossRef] [PubMed]
- Rampil, I.J. A Primer for EEG Signal Processing in Anesthesia. Anesthesiology 1998, 89, 980–1002. [Google Scholar] [CrossRef]
- Aneja, R.; Heard, A.M.B.; Fletcher, J.E.; Heard, C.M.B. Sedation Monitoring of Children by the Bispectral Index in the Pediatric Intensive Care Unit. Pediatr. Crit. Care Med. 2003, 4, 60–64. [Google Scholar] [CrossRef]
- Hayden, J.C.; Breatnach, C.; Doherty, D.R.; Healy, M.; Howlett, M.M.; Gallagher, P.J.; Cousins, G. Efficacy of A2-Agonists for Sedation in Pediatric Critical Care: A Systematic Review. Pediatr. Crit. Care Med. 2016, 17, e66–e75. [Google Scholar] [CrossRef]
- Heiberger, A.L.; Ngorsuraches, S.; Olgun, G.; Luze, L.; Leimbach, C.; Madison, H.; Lakhani, S.A. Safety and Utility of Continuous Ketamine Infusion for Sedation in Mechanically Ventilated Pediatric Patients. J. Pediatr. Pharmacol. Ther. 2018, 23, 447–454. [Google Scholar] [CrossRef]
- Kim, H.J.; Shin, W.J.; Park, S.; Ahn, H.S.; Oh, J.H. The Sedative Effects of the Intranasal Administration of Dexmedetomidine in Children Undergoing Surgeries Compared to Other Sedation Methods: A Systematic Review and Meta-Analysis. J. Clin. Anesth. 2017, 38, 33–39. [Google Scholar] [CrossRef] [PubMed]
- Pansini, V.; Curatola, A.; Gatto, A.; Lazzareschi, I.; Ruggiero, A.; Chiaretti, A. Intranasal Drugs for Analgesia and Sedation in Children Admitted to Pediatric Emergency Department: A Narrative Review. Ann. Transl. Med. 2021, 9, 189. [Google Scholar] [CrossRef] [PubMed]
- Amigoni, A.; Mozzo, E.; Brugnaro, L.; Gentilomo, C.; Stritoni, V.; Michelin, E.; Pettenazzo, A. Assessing Sedation in a Pediatric Intensive Care Unit Using Comfort Behavioural Scale and Bispectral Index: These Tools Are Different. Minerva Anestesiol. 2012, 78, 322–329. [Google Scholar] [PubMed]
- Courtman, S.P.; Wardurgh, A.; Petros, A.J. Comparison of the Bispectral Index Monitor with the Comfort Score in Assessing Level of Sedation of Critically Ill Children. Intensiv. Care Med. 2003, 29, 2239–2246. [Google Scholar] [CrossRef]
- Crain, N.; Slonim, A.; Pollack, M.M. Assessing Sedation in the Pediatric Intensive Care Unit by Using Bis and the Comfort Scale. Pediatr. Crit. Care Med. 2002, 3, 11–14. [Google Scholar] [CrossRef]
- Lamas, A.; López-Herce, J.; Sancho, L.; Mencía, S.; Carrillo, Á.; Santiago, M.J.; Martínez, V. Assessing Sedation in Critically Ill Children by Bispectral Index, Auditory-Evoked Potentials and Clinical Scales. Intensiv. Care Med. 2008, 34, 2092–2099. [Google Scholar] [CrossRef]
- Triltsch, A.E.; Nestmann, G.; Orawa, H.; Moshirzadeh, M.; Sander, M.; Grosse, J.; Genähr, A.; Konertz, W.; Spies, C.D. Bispectral Index Versus Comfort Score to Determine the Level of Sedation in Paediatric Intensive Care Unit Patients: A Prospective Study. Crit. Care 2005, 9, R9–R17. [Google Scholar] [CrossRef]
- Twite, M.D.; Zuk, J.; Gralla, J.; Friesen, R.H. Correlation of the Bispectral Index Monitor with the Comfort Scale in the Pediatric Intensive Care Unit. Pediatr. Crit. Care Med. 2005, 6, 648–653. [Google Scholar] [CrossRef]
- Kos, M.K.; Miksić, M.; Jovanović, M.; Roškar, R.; Grosek, Š.; Grabnar, I. Maturation of Midazolam Clearance in Critically Ill Children with Severe Bronchiolitis: A Population Pharmacokinetic Analysis. Eur. J. Pharm. Sci. 2020, 141, 105095. [Google Scholar] [CrossRef]
- R Core Team. R: A Language and Environment for Statistical Computing; R Foundation for Statistical Computing: Vienna, Austria, 2021. [Google Scholar]
- Bakdash, J.Z.; Marusich, L.R. rmcorr: Repeated Measures Correlation. R Package Version 0.7.0. 2024. Available online: https://CRAN.R-project.org/package=rmcorr (accessed on 2 June 2025).
- Ulrich, J. TTR: Technical Trading Rules. R Package Version 0.24.3. 2021. Available online: https://CRAN.R-project.org/package=TTR (accessed on 2 June 2025).
- Bates, D.; Mächler, M.; Bolker, B.; Walker, S. Fitting Linear Mixed-Effects Models Using Lme4. J. Stat. Softw. 2015, 67, 1–48. [Google Scholar] [CrossRef]
- Liaw, A.; Wiener, M. Classification and Regression by Randomforest. R News 2002, 2, 18–22. [Google Scholar]
- Tahmasebi, P.; Hezarkhani, A.; Sahimi, M. Multiple-Point Geostatistical Modeling Based on the Cross-Correlation Functions. Comput. Geosci. 2012, 16, 779–797. [Google Scholar] [CrossRef]
- Montgomery, D.C.; Jennings, C.L.; Kulahci, M. Introduction to Time Series Analysis and Forecasting. John Wiley & Sons: Hoboken, NJ, USA, 2015. [Google Scholar]
- Geroldinger, A.; Lusa, L.; Nold, M.; Heinze, G. Leave-one-out Cross-Validation, Penalization, and Differential Bias of Some Prediction Model Performance Measures—A Simulation Study. Diagn. Progn. Res. 2023, 7, 9. [Google Scholar] [CrossRef] [PubMed]
- Hu, J.; Szymczak, S. A Review on Longitudinal Data Analysis with Random Forest. Briefings Bioinform. 2023, 24, bbad002. [Google Scholar] [CrossRef] [PubMed]
- Sandri, M.; Zuccolotto, P. A Bias Correction Algorithm for the Gini Variable Importance Measure in Classification Trees. J. Comput. Graph. Stat. 2008, 17, 611–628. [Google Scholar] [CrossRef]
- Goldstein, A.; Kapelner, A.; Bleich, J.; Pitkin, E. Peeking Inside the Black Box: Visualizing Statistical Learning with Plots of Individual Conditional Expectation. J. Comput. Graph. Stat. 2015, 24, 44–65. [Google Scholar] [CrossRef]
| All Patients | NMB Co-Administration | Age Group | Degree of Sedation | |||||||
|---|---|---|---|---|---|---|---|---|---|---|
| n = 41 | Yes n = 22 | No n = 19 | p-Value | <26 Weeks n = 30 | ≥26 Weeks n = 11 | p-Value | Deep Sedation COMFORT-B (6–10) n = 21 | Moderate Sedation COMFORT-B > 10 n = 20 | p-Value | |
| Age (weeks) | 27.8 (37.3) | 35.5 (39.9) | 18.9 (32.8) | 0.014 | 8.1 (5.4) | 81.6 (33.9) | <0.0001 | 28.9 (37.9) | 31.7 (39.1) | 0.025 |
| Body weight (kg) | 6.1 (2.9) | 6.8 (3.0) | 5.4 (2.6) | 0.09 | 4.7 (1.2) | 10.2 (2.2) | <0.0001 | 6.2 (2.9) | 6.5 (2.9) | 0.004 |
| COMFORT-B | 10.1 (2.7) | 9.9 (2.3) | 10.1 (3.1) | 0.98 | 9.4 (2.6) | 11.6 (2.5) | 0.017 | 7.7 (1.1) | 14.0 (2.3) | <0.001 |
| BIS | 51.5 (7.1) | 51.0 (6.6) | 51.9 (7.9) | 0.77 | 50.1 (6.8) | 54.8 (7.4) | 0.053 | 50.7 (8.7) | 55.5 (9.3) | 0.026 |
| Time Slice * | n | Spearman Rho (p-Value) |
|---|---|---|
| 1 2 3 4 5 6 7 8 9 10 11 12 13 14 15 | 37 37 39 37 35 34 35 35 30 25 23 22 14 10 9 | 0.41 (0.006) −0.11 (0.678) 0.18 (0.170) 0.10 (0.363) 0.17 (0.511) 0.37 (0.029) 0.39 (0.021) 0.06 (0.712) −0.10 (0.606) 0.07 (0.735) 0.48 (0.021) 0.33 (0.136) −0.09 (0.754) 0.67 (0.035) 0.21 (0.587) |
| Metric (by Subject) | All Patients | NMB Co-Administration | Age | Degree of Sedation | |||
|---|---|---|---|---|---|---|---|
n = 41 | Yes n = 22 | No n = 19 | <26 Weeks n = 30 | ≥26 Weeks n = 11 | Deep COMFORT-B (6–10) n = 21 | Moderate COMFORT-B > 10 n = 20 | |
| Mean | 0.42 (0.007) | 0.21 (0.34) | 0.61 (0.0063) | 0.45 (0.01) | 0.29 (0.23) | 0.55 (0.01) | 0.083 (0.73) |
| Time weighted average | 0.36 (0.022) | 0.36 (0.022) | 0.36 (0.022) | 0.36 (0.022) | 0.36 (0.022) | 0.36 (0.022) | 0.36 (0.022) |
| Median | 0.31 (0.045) | 0.12 (0.58) | 0.47 (0.043) | 0.33 (0.075) | 0.27 (0.27) | 0.37 (0.10) | 0.13 (0.58) |
| Minimum | 0.15 (0.34) | 0.10 (0.66) | 0.21 (0.40) | 0.26 (0.16) | 0.05 (0.85) | 0.075 (0.75) | 0.18 (0.45) |
| Maximum | 0.40 (0.008) | 0.29 (0.19) | 0.51 (0.025) | 0.35 (0.061) | 0.21 (0.40) | 0.34 (0.13) | 0.24 (0.31) |
| Parameter | Estimate | 95% Confidence Interval |
|---|---|---|
| Intercept | 43.1 | (38.4, 47.9) |
| Slope | 0.799 | (0.383, 1.215) |
| Between-subject variability (variance) | ||
| Intercept | 25.8 | (12.7, 38.8) |
| Residual variability | ||
| Proportional error (%) | 21.2 | (19.1, 23.3) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Published by MDPI on behalf of the Lithuanian University of Health Sciences. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Jožef, M.; Kerec Kos, M.; Grosek, Š.; Hajdinjak, M.; Dolinar, G.; Grabnar, I. Assessment of Sedation in Mechanically Ventilated Children with Severe Acute Bronchiolitis: Correlation Between COMFORT-B Scale and Bispectral Index During Continuous Infusion of Fentanyl and Midazolam. Medicina 2025, 61, 1953. https://doi.org/10.3390/medicina61111953
Jožef M, Kerec Kos M, Grosek Š, Hajdinjak M, Dolinar G, Grabnar I. Assessment of Sedation in Mechanically Ventilated Children with Severe Acute Bronchiolitis: Correlation Between COMFORT-B Scale and Bispectral Index During Continuous Infusion of Fentanyl and Midazolam. Medicina. 2025; 61(11):1953. https://doi.org/10.3390/medicina61111953
Chicago/Turabian StyleJožef, Maj, Mojca Kerec Kos, Štefan Grosek, Melita Hajdinjak, Gregor Dolinar, and Iztok Grabnar. 2025. "Assessment of Sedation in Mechanically Ventilated Children with Severe Acute Bronchiolitis: Correlation Between COMFORT-B Scale and Bispectral Index During Continuous Infusion of Fentanyl and Midazolam" Medicina 61, no. 11: 1953. https://doi.org/10.3390/medicina61111953
APA StyleJožef, M., Kerec Kos, M., Grosek, Š., Hajdinjak, M., Dolinar, G., & Grabnar, I. (2025). Assessment of Sedation in Mechanically Ventilated Children with Severe Acute Bronchiolitis: Correlation Between COMFORT-B Scale and Bispectral Index During Continuous Infusion of Fentanyl and Midazolam. Medicina, 61(11), 1953. https://doi.org/10.3390/medicina61111953







