Locking Plate with Cerclage Wiring Versus Hook Plate Fixation for Unstable Distal Clavicle Fractures: Is There Still a Role for Hook Plates?
Abstract
1. Introduction
2. Materials and Methods
2.1. Patient Enrollment
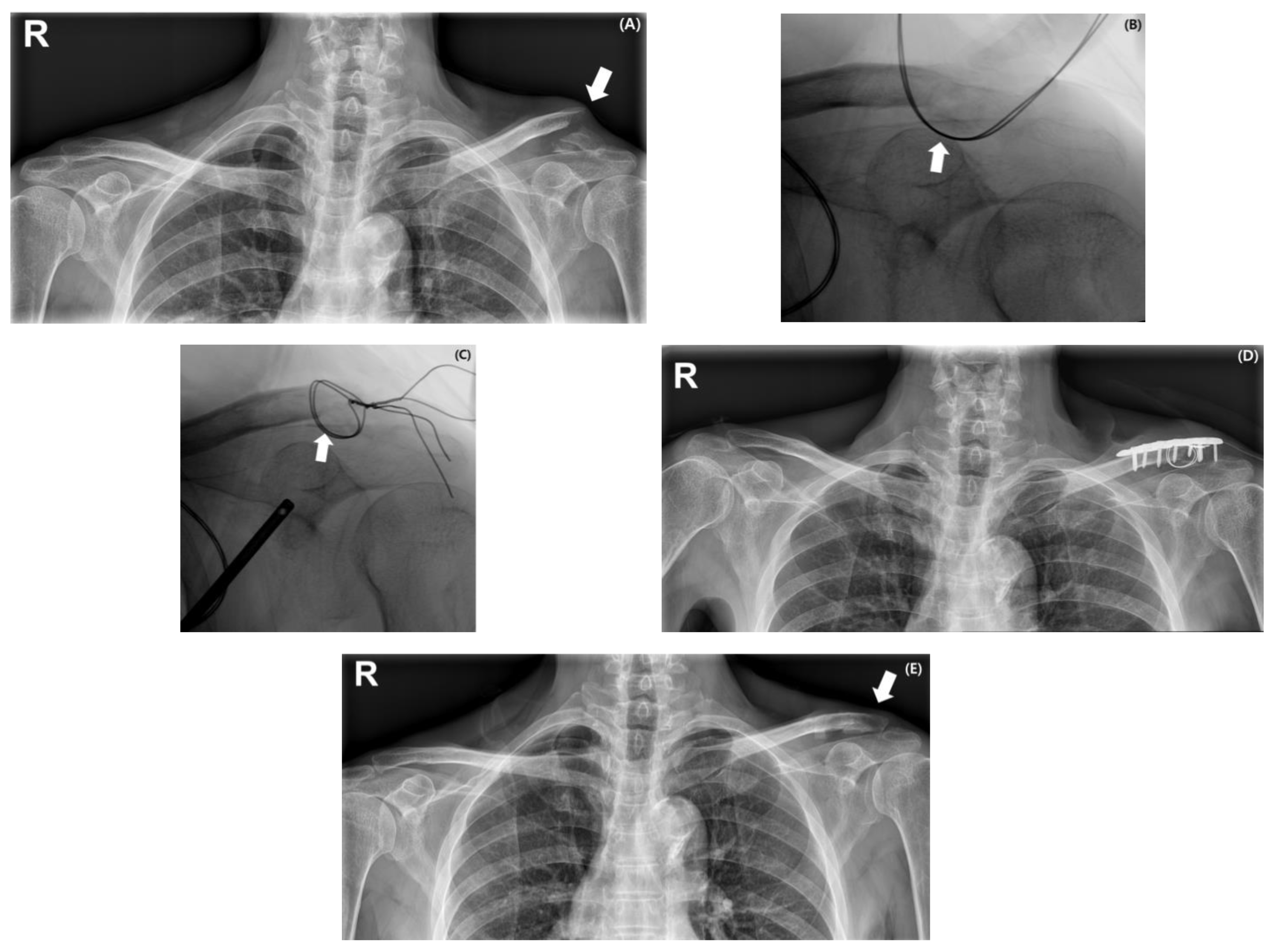
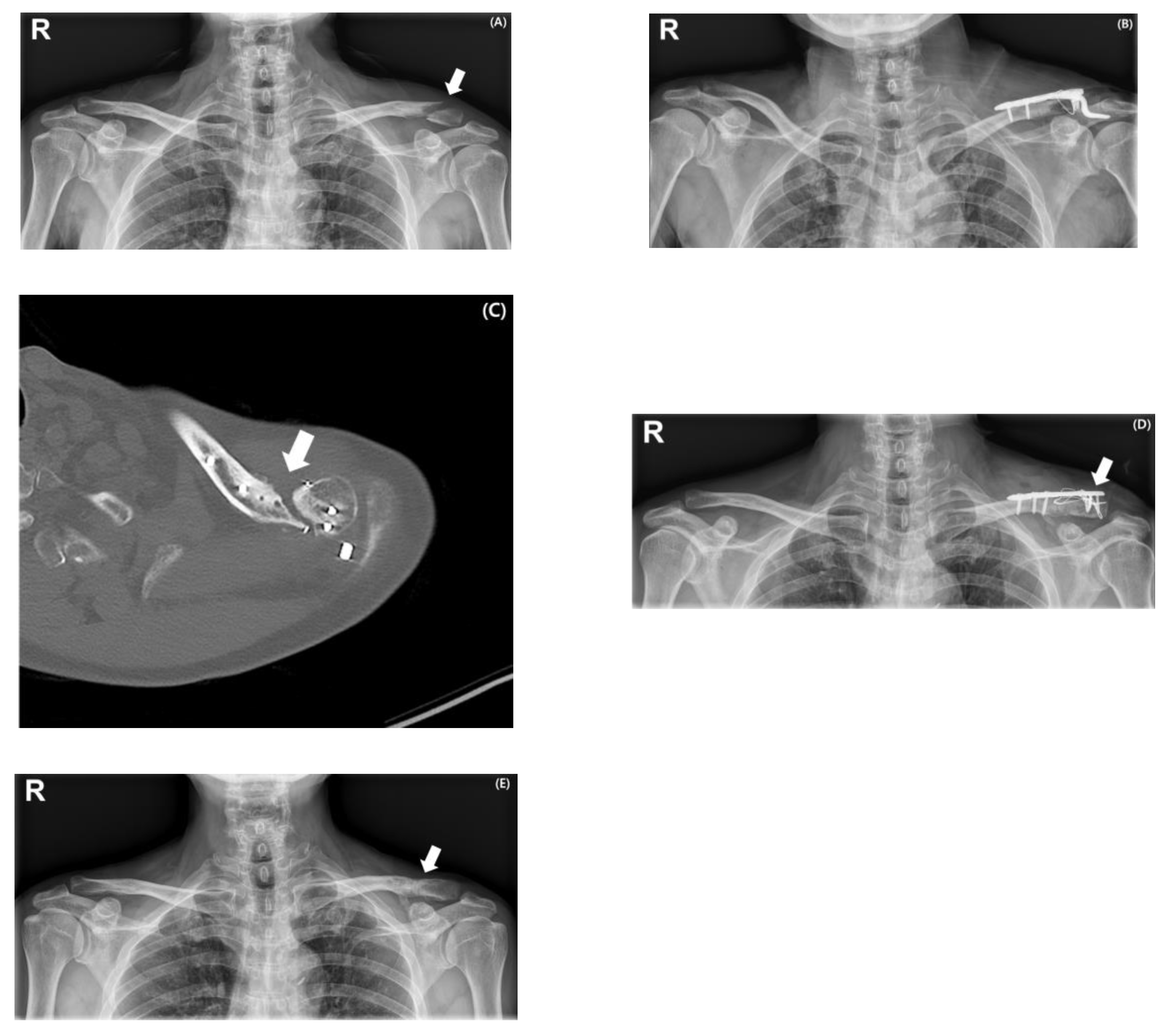
2.2. Surgical Procedures
2.3. Clinical and Radiologic Assessment
2.4. Statistical Analysis
3. Results
3.1. Patient Demographics
3.2. Clinical and Radiologic Outcomes
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Kim, J.U.; Yoon, J.Y.; Park, H.J.; Park, J.H. Surgical treatment options of displaced midshaft fractures of the clavicle in young adults: Plate fixation versus intramedullary nailing. Clin. Shoulder Elb. 2024, 27, 447–453. [Google Scholar] [CrossRef]
- Kim, H.; Jung, Y.; Song, H.S. Plate prebending using a three-dimensional–printed model affords effective anatomical reduction in clavicular shaft fractures. Clin. Shoulder Elb. 2023, 26, 397–405. [Google Scholar] [CrossRef]
- Song, H.S.; Kim, H. Current concepts in the treatment of midshaft clavicle fractures in adults. Clin. Shoulder Elb. 2021, 24, 189–198. [Google Scholar] [CrossRef] [PubMed]
- Kim, D.-W.; Kim, D.-H.; Kim, B.-S.; Cho, C.-H. Current Concepts for Classification and Treatment of Distal Clavicle Fractures. Clin. Orthop. Surg. 2020, 12, 135–144. [Google Scholar] [CrossRef] [PubMed]
- Chen, P.-H.; Chen, C.-Y.; Lin, K.-C.; Tarng, Y.-W. Fixing Cho Type IIC Distal Clavicle Fractures with Hook Plates Leads to a High Incidence of Subacromial Osteolysis: A Retrospective Study and Literature Review. Clin. Orthop. Surg. 2024, 16, 694–701. [Google Scholar] [CrossRef]
- Hall, J.A.; Schemitsch, C.E.; Vicente, M.R.; Dehghan, N.; Nauth, A.; Nowak, L.L.; Schemitsch, E.H.; McKee, M.D. Operative Versus Nonoperative Treatment of Acute Displaced Distal Clavicle Fractures: A Multicenter Randomized Controlled Trial. J. Orthop. Trauma 2021, 35, 660–666. [Google Scholar] [CrossRef]
- Lee, J.-W.; Song, M.-J.; Lee, S.-J.; Song, H.S.; Jung, Y.-S.; Kim, H. Biomechanical comparison between low profile 2.7 mm distal locking hook plate and 3.5 mm distal locking hook plate for acromioclavicular joint injury: A finite element analysis. Injury 2024, 55, 111657. [Google Scholar] [CrossRef]
- Asadollahi, S.; Bucknill, A. Hook Plate Fixation for Acute Unstable Distal Clavicle Fracture: A Systematic Review and Meta-analysis. J. Orthop. Trauma 2019, 33, 417–422. [Google Scholar] [CrossRef]
- Lee, S.-J.; Eom, T.-W.; Hyun, Y.-S. Complications and Frequency of Surgical Treatment with AO-Type Hook Plate in Shoulder Trauma: A Retrospective Study. J. Clin. Med. 2022, 11, 1026. [Google Scholar] [CrossRef]
- Lopiz, Y.; Checa, P.; García-Fernández, C.; Valle, J.; Vega, M.L.; Marco, F. Complications with the clavicle hook plate after fixation of Neer type II clavicle fractures. Int. Orthop. 2019, 43, 1701–1708. [Google Scholar] [CrossRef] [PubMed]
- Choi, J.-H.; Chun, Y.-M.; Yoon, T.-H. Effect of cigarette smoking on the maintenance of reduction after treatment of acute acromioclavicular joint dislocation with hook plate fixation. Clin. Shoulder Elb. 2023, 26, 373–379. [Google Scholar] [CrossRef] [PubMed]
- Bhatia, D.; Page, R. Surgical treatment of lateral clavicle fractures associated with complete coracoclavicular ligament disruption: Clinico-radiological outcomes of acromioclavicular joint sparing and spanning implants. Int. J. Shoulder Surg. 2012, 6, 116–120. [Google Scholar] [CrossRef]
- Sharma, V.; Modi, A.; Armstrong, A.; Pandey, R.; Sharma, D.; Singh, H. The Management of Distal Clavicle Fractures—A Survey of UK Shoulder and Elbow Surgeons. Cureus 2021, 13, e17305. [Google Scholar] [CrossRef] [PubMed]
- Uittenbogaard, S.J.; van Es, L.J.M.; den Haan, C.; van Deurzen, D.F.P.; van den Bekerom, M.P.J. Outcomes, Union Rate, and Complications After Operative and Nonoperative Treatments of Neer Type II Distal Clavicle Fractures: A Systematic Review and Meta-analysis of 2284 Patients. Am. J. Sports Med. 2023, 51, 534–544. [Google Scholar] [CrossRef] [PubMed]
- Jo, Y.-H.; Lee, B.G. Clavicle midshaft fractures should not be considered an easy surgery: Reduction and prebending. Clin. Shoulder Elb. 2023, 26, 341–342. [Google Scholar] [CrossRef]
- Constant, C.R.M.; Murley, A.G.M. A clinical method of functional assessment of the shoulder. Clin. Orthop. Relat. Res. 1987, 214, 160–164. [Google Scholar] [CrossRef]
- Rajani, A.M.; Shah, U.A.; Mittal, A.R.; Gupta, S.; Garg, R.; Rajani, A.A.; Shetty, G.; Punamiya, M.; Singhal, R. Effects of glenohumeral corticosteroid injection on stiffness following arthroscopic rotator cuff repair: A prospective, multicentric, case-control study with 18-month follow-up. Clin. Shoulder Elb. 2023, 26, 64–70. [Google Scholar] [CrossRef]
- Hong, S.-Y.; Lee, S.-J.; Hahm, H.-B.; Chang, J.-W.; Hyun, Y.-S. Onlay patch augmentation in rotator cuff repair for moderate to large tears in elderly patients: Clinical and radiologic outcomes. Clin. Shoulder Elb. 2023, 26, 71–81. [Google Scholar] [CrossRef]
- Kim, Y.-S.; Lee, H.-J.; Jin, H.-K.; Kim, S.-E.; Lee, J.-W. Conventional En Masse Repair Versus Separate Double-Layer Double-Row Repair for the Treatment of Delaminated Rotator Cuff Tears. Am. J. Sports Med. 2016, 44, 1146–1152. [Google Scholar] [CrossRef]
- Kim, Y.-K.; Jung, K.-H.; Kwon, H.-M. Comparison of Structural Integrity and Functional Outcome Between Delaminated and Nondelaminated Rotator Cuff Tears After En Masse Arthroscopic Repair: A Retrospective Cohort Study with Propensity Score Matching. Am. J. Sports Med. 2019, 47, 1411–1419. [Google Scholar] [CrossRef]
- Kim, S.C.; Yoo, S.J.; Jo, J.H.; Lee, J.H.; Baek, E.; Lee, S.M.; Yoo, J.C. The impact of supraspinatus tear on subscapularis muscle atrophy and fatty infiltration. Clin. Shoulder Elb. 2024, 27, 437–446. [Google Scholar] [CrossRef]
- Panagopoulos, A.; Solou, K.; Tatani, I.; Triantafyllopoulos, I.K.; Lakoumentas, J.; Kouzelis, A.; Athanasiou, V.; Kokkalis, Z.T. What is the optimal surgical treatment for Neer type IIB (IIC) distal clavicle fractures? A systematic review and meta-analysis. J. Orthop. Surg. Res. 2022, 17, 215. [Google Scholar] [CrossRef]
- Teimouri, M.; Ravanbod, H.; Farrokhzad, A.; Sabaghi, J.; Mirghaderi, S.P. Comparison of hook plate versus T-plate in the treatment of Neer type II distal clavicle fractures: A prospective matched comparative cohort study. J. Orthop. Surg. Res. 2022, 17, 369. [Google Scholar] [CrossRef] [PubMed]
- Orlandi, T.-V.; Rogers, N.S.; Burger, M.C.; King, P.R.; Lamberts, R.P. A prospective randomized controlled trial comparing plating augmented with coracoclavicular fixation and hook plate fixation of displaced distal-third clavicle fractures. J. Shoulder Elb. Surg. 2022, 31, 906–913. [Google Scholar] [CrossRef]
- Li, L.; Li, T.-Y.; Jiang, P.; Lin, G.; Wu, H.; Han, X.; Yu, X. Clavicle hook plate versus distal clavicle locking plate for Neer type II distal clavicle fractures. J. Orthop. Surg. Res. 2019, 14, 472. [Google Scholar] [CrossRef]
- Verstift, D.E.; Heisen, J.; Somford, M.P.; van den Bekerom, M.P.J. Eponymous terms in acromioclavicular joint surgery. Clin. Shoulder Elb. 2024, 27, 229–236. [Google Scholar] [CrossRef]
- Beisemann, N.; Spiller, Y.M.; Schnetzke, M.; Grützner, P.A.; Nolte, P.-C. Hook plate fixation of Neer type II distal clavicle fractures results in satisfactory patient-reported outcomes but complications and revisions are high. BMC Musculoskelet. Disord. 2023, 24, 850. [Google Scholar] [CrossRef] [PubMed]
- Singh, A.; Schultzel, M.; Fleming, J.F.; Navarro, R.A. Complications after surgical treatment of distal clavicle fractures. Orthop. Traumatol. Surg. Res. 2019, 105, 853–859. [Google Scholar] [CrossRef]
- Moldovan, F. Anterior Radial Head Dislocation Associated with a Bifocal Fracture of the Ulna: A Bado Type ID Monteggia Fracture–Dislocation? Life 2025, 15, 637. [Google Scholar] [CrossRef] [PubMed]

| Variable | Group 1 (n = 27) | Group 2 (n = 25) | p-Value |
|---|---|---|---|
| Mean age (years) | 50.96 ± 15.69 (range: 28–76) | 49.56 ± 17.25 (range: 20–69) | 0.760 |
| Follow-up duration (months) | 14.41 ± 5.63 (range: 12–36) | 11.84 ± 10.82 (range: 12–42) | 0.283 |
| Sex | 0.427 | ||
| Male | 21 (77.8%) | 17 (68%) | |
| Female | 6 (22.2%) | 8 (32%) | |
| Affected side | 0.376 | ||
| Right | 13 (48.1%) | 9 (36%) | |
| Left | 14 (51.9%) | 16 (64%) | |
| Smoking status | 7 (25.9%) | 8 (32%) | 0.629 |
| Mechanism of injury | 0.609 | ||
| Low energy | 10 (37%) | 11 (44%) | |
| High energy | 17 (63%) | 14 (56%) | |
| Cho’s classification | 0.694 | ||
| IIA | 8 (29.6%) | 3 | |
| IIB | 5 (18.5%) | 9 | |
| IIC | 1 (3.8%) | 2 | |
| IID | 13 (48.1%) | 11 |
| Variable | Group 1 (n = 27) | Group 2 (n = 25) | p-Value |
|---|---|---|---|
| Complication | 1 (3.7%) | 10 (40%) | 0.002 |
| Non-union | 0 (0%) | 2 (20%) | |
| Postoperative stiffness | 0 (0%) | 7 (70%) | |
| Peri-implant fracture | 1 (100%) | 1 (10%) | |
| Time to union (months) | 3.65 ± 1.20 | 4.06 ± 1.89 | 0.256 |
| Range of motion at final follow-up | |||
| Forward flexion | 169.62 ± 2.42 | 169.20 ± 1.87 | 0.497 |
| Internal rotation at back | 4.04 ± 0.45 | 4.64 ± 0.35 | 0.570 |
| Side external rotation | 76.92 ± 7.49 | 72.80 ± 8.79 | 0.077 |
| Abduction | 94.04 ± 2.46 | 92.20 ± 4.81 | 0.096 |
| Abduction external rotation | 81.73 ± 8.36 | 77.20 ± 9.90 | 0.083 |
| Abduction internal rotation | 70.38 ± 3.72 | 70.80 ± 5.72 | 0.759 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Published by MDPI on behalf of the Lithuanian University of Health Sciences. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Song, H.S.; Kim, H. Locking Plate with Cerclage Wiring Versus Hook Plate Fixation for Unstable Distal Clavicle Fractures: Is There Still a Role for Hook Plates? Medicina 2025, 61, 1882. https://doi.org/10.3390/medicina61101882
Song HS, Kim H. Locking Plate with Cerclage Wiring Versus Hook Plate Fixation for Unstable Distal Clavicle Fractures: Is There Still a Role for Hook Plates? Medicina. 2025; 61(10):1882. https://doi.org/10.3390/medicina61101882
Chicago/Turabian StyleSong, Hyun Seok, and Hyungsuk Kim. 2025. "Locking Plate with Cerclage Wiring Versus Hook Plate Fixation for Unstable Distal Clavicle Fractures: Is There Still a Role for Hook Plates?" Medicina 61, no. 10: 1882. https://doi.org/10.3390/medicina61101882
APA StyleSong, H. S., & Kim, H. (2025). Locking Plate with Cerclage Wiring Versus Hook Plate Fixation for Unstable Distal Clavicle Fractures: Is There Still a Role for Hook Plates? Medicina, 61(10), 1882. https://doi.org/10.3390/medicina61101882






