Clinical Outcomes of Transdiscal Screws for Thoracolumbar Spinal Fractures with Marked Anterior Distraction Gap Accompanied by Diffuse Idiopathic Skeletal Hyperostosis
Abstract
1. Introduction
2. Materials and Methods
2.1. Operation Procedure
2.2. Statistical Analysis
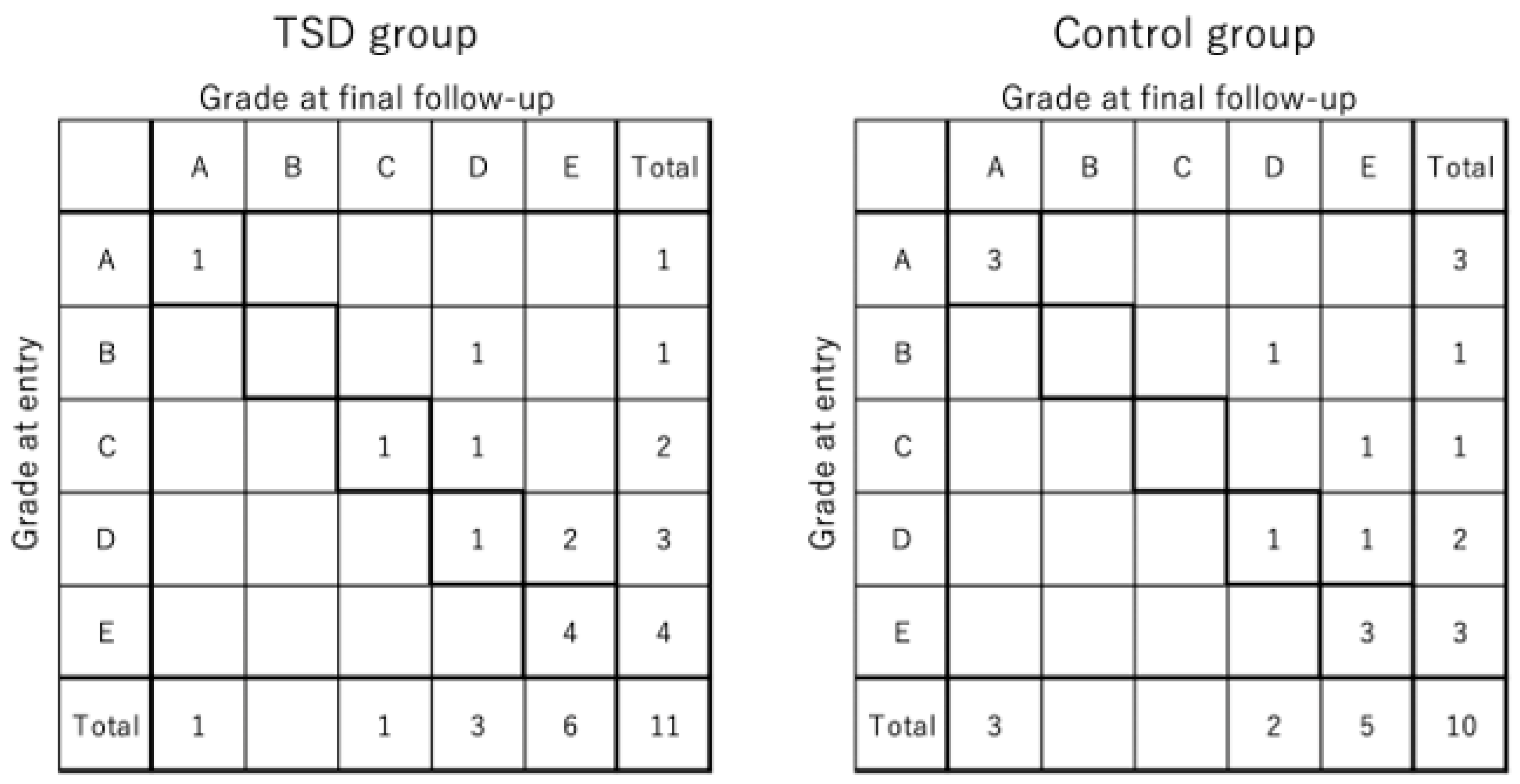
3. Results
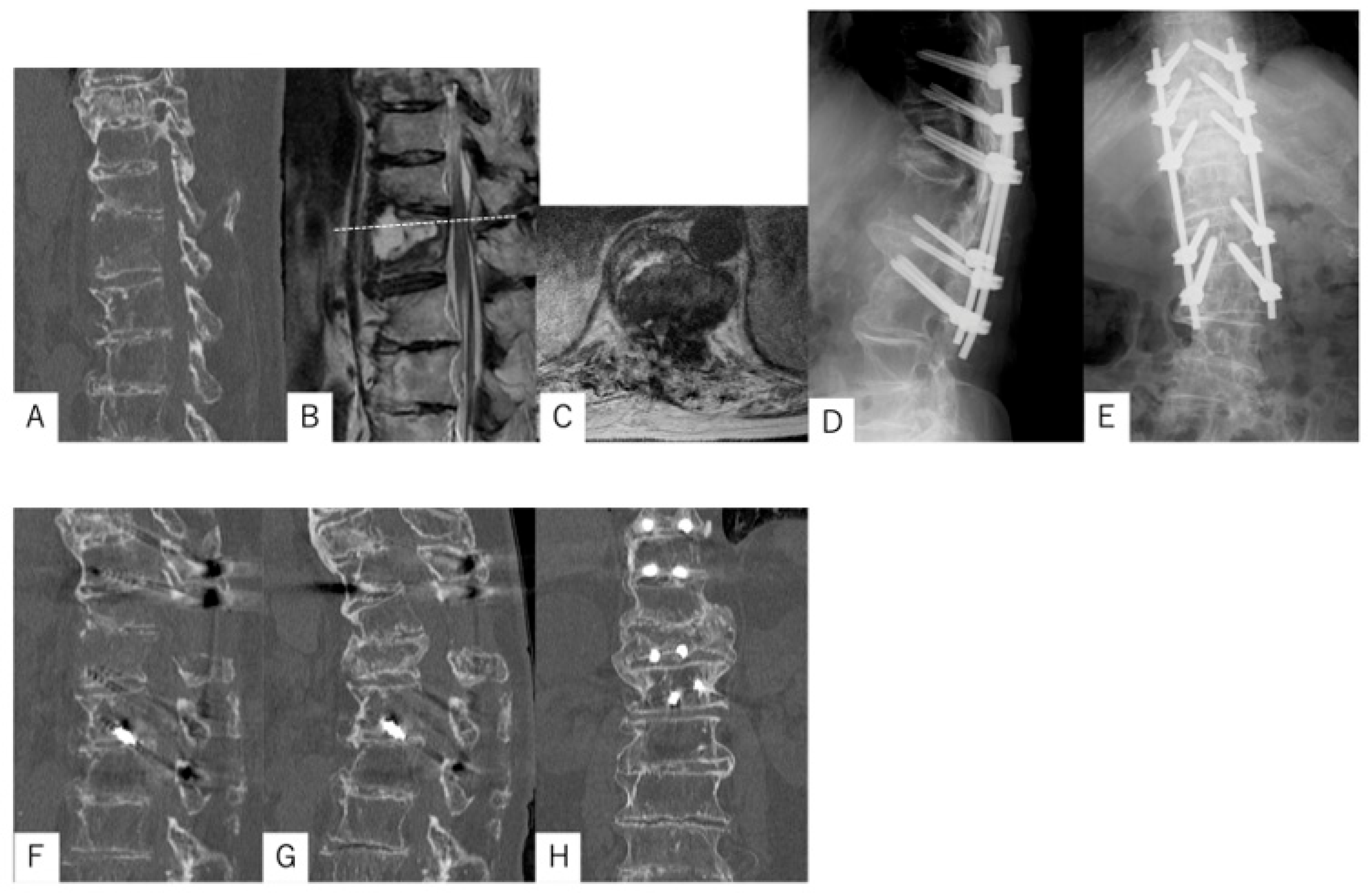
3.1. Case Presentation 1
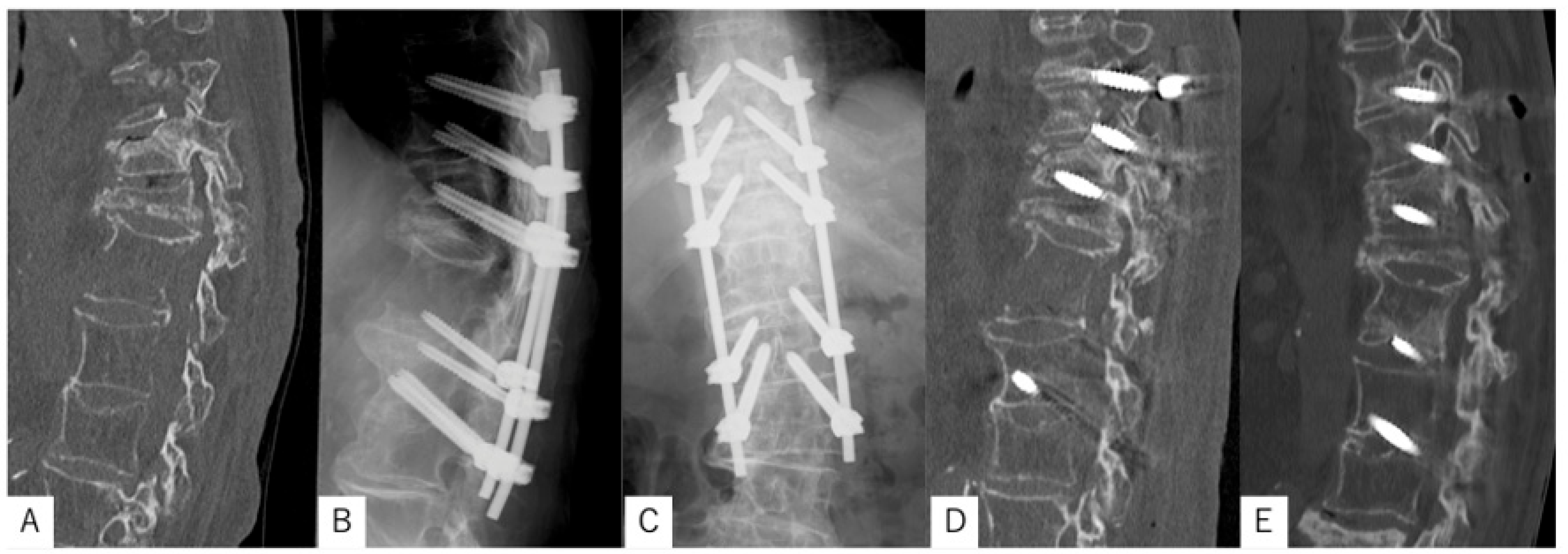
3.2. Case Presentation 2
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Okada, E.; Tsuji, T.; Shimizu, K.; Kato, M.; Fukuda, K.; Kaneko, S.; Ogawa, J.; Watanabe, K.; Ishii, K.; Nakamura, M.; et al. CT-based morphological analysis of spinal fractures in patients with diffuse idiopathic skeletal hyperostosis. J. Orthop. Sci. 2017, 22, 3–9. [Google Scholar] [CrossRef] [PubMed]
- Rustagi, T.; Drazin, D.; Oner, C.; York, J.; Schroeder, G.D.; Vaccaro, A.R.; Oskouian, R.J.; Chapman, J.R. Fractures in spinal ankylosing disorders: A narrative review of disease and injury types, treatment techniques, and outcomes. J. Orthop. Trauma. 2017, 31 (Suppl 4), S57–S74. [Google Scholar] [CrossRef] [PubMed]
- Ikuma, H.; Takao, S.; Inoue, Y.; Hirose, T.; Matsukawa, K.; Kawasaki, K. Treatment of thoracolumbar spinal fracture accompanied by diffuse idiopathic skeletal hyperostosis using transdiscal screws for diffuse idiopathic skeletal hyperostosis: Preliminary results. Asian Spine J. 2021, 15, 340–348. [Google Scholar] [CrossRef] [PubMed]
- Westerveld, L.A.; van Bemmel, J.C.; Dhert, W.J.; Oner, F.C.; Verlaan, J.J. Clinical outcome after traumatic spinal fractures in patients with ankylosing spinal disorders compared with control patients. Spine J. 2014, 14, 729–740. [Google Scholar] [CrossRef] [PubMed]
- Westerveld, L.A.; Verlaan, J.J.; Oner, F.C. Spinal fractures in patients with ankylosing spinal disorders: A systematic review of the literature on treatment, neurological status and complications. Eur. Spine J. 2009, 18, 145–156. [Google Scholar] [CrossRef] [PubMed]
- Okada, E.; Shimizu, K.; Kato, M.; Fukuda, K.; Kaneko, S.; Ogawa, J.; Yagi, M.; Fujita, N.; Tsuji, O.; Suzuki, S.; et al. Spinal fractures in patients with diffuse idiopathic skeletal hyperostosis: Clinical characteristics by fracture level. J. Orthop. Sci. 2019, 24, 393–399. [Google Scholar] [CrossRef] [PubMed]
- Caron, T.; Bransford, R.; Nguyen, Q.; Agel, J.; Chapman, J.; Bellabarba, C. Spine fractures in patients with ankylosing spinal disorders. Spine 2010, 35, E458–E464. [Google Scholar] [CrossRef] [PubMed]
- Buxbaum, R.E.; Shani, A.; Mulla, H.; Rod, A.; Rahamimov, N. Percutaneous, PMMA-augmented, pedicle screw instrumentation of thoracolumbar ankylotic spine fractures. J. Orthop. Surg. Res. 2021, 16, 317. [Google Scholar] [CrossRef] [PubMed]
- Yagi, M.; Ogiri, M.; Holy, C.E.; Bourcet, A. Comparison of clinical effectiveness of fenestrated and conventional pedicle screws in patients undergoing spinal surgery: A systematic review and meta-analysis. Expert. Rev. Med. Devices 2021, 18, 995–1022. [Google Scholar] [CrossRef] [PubMed]
- Reinhold, M.; Knop, C.; Kneitz, C.; Disch, A. Spine fractures in ankylosing diseases: Recommendations of the spine section of the German society for orthopaedics and trauma (DGOU). Glob. Spine J. 2018, 8 (Suppl. S2), 56S–68S. [Google Scholar] [CrossRef] [PubMed]
- Kai, K.; Ikuta, K.; Masuda, K.; Kitamura, T.; Senba, H.; Shidahara, S. Surgical outcomes of minimally invasive stabilization for spinal fractures in patients with ankylosing spinal disorders. Asian Spine J. 2018, 12, 434–441. [Google Scholar] [CrossRef] [PubMed]
- Moussallem, C.D.; McCutcheon, B.A.; Clarke, M.J.; Cui, Q.; Currier, B.L.; Yaszemski, M.J.; Huddleston, P.M.; Rose, P.S.; Freedman, B.; Dekutoski, M.B.; et al. Perioperative complications in open versus percutaneous treatment of spinal fractures in patients with an ankylosed spine. J. Clin. Neurosci. 2016, 30, 88–92. [Google Scholar] [CrossRef] [PubMed]
- Takeuchi, T.; Takamizawa, Y.; Konishi, K.; Sano, H.; Takahashi, M.; Kouno, H.; Hosogane, N. Comparison of the fixation strengths of screws between the traditional trajectory and the single and double endplate penetrating screw trajectories using osteoporotic vertebral body models based on the finite element method. Asian Spine J. 2024, 18, 12–20. [Google Scholar] [CrossRef] [PubMed]
- Xavier, F.; Jauregui, J.J.; Cornish, N.; Jason-Rousseau, R.; Chatterjee, D.; Feuer, G.; Hayes, W.; Kapadia, B.H.; Carter, J.N.; Yoshihara, H.; et al. Regional variations in shear strength and density of the human thoracic vertebral endplate and trabecular bone. Int. J. Spine Surg. 2017, 11, 7. [Google Scholar] [CrossRef] [PubMed]
- Hou, Y.; Yuan, W. Influences of disc degeneration and bone mineral density on the structural properties of lumbar end plates. Spine J. 2012, 12, 249–256. [Google Scholar] [CrossRef] [PubMed]
- Matsukawa, K.; Yato, Y.; Imabayashi, H. Impact of screw diameter and length on pedicle screw fixation strength in osteoporotic vertebrae: A finite element analysis. Asian Spine J. 2021, 15, 566–574. [Google Scholar] [CrossRef] [PubMed]
- Xu, L.; Qian, Z.; Wang, S.; Wang, R.; Pu, X.; Yang, B.; Zhou, Q.; Du, C.; Chen, Q.; Feng, Z.; et al. Galectin-3 enhances osteogenic differentiation of precursor cells from patients with diffuse idiopathic skeletal hyperostosis via Wnt/β-catenin signaling. J. Bone Miner. Res. 2022, 37, 724–739. [Google Scholar] [CrossRef] [PubMed]
- Sethi, A.; Ruby, J.G.; Veras, M.A.; Telis, N.; Melamud, E. Genetics implicates overactive osteogenesis in the development of diffuse idiopathic skeletal hyperostosis. Nat. Commun. 2023, 14, 2644. [Google Scholar] [CrossRef] [PubMed]
- Licini, C.; Farinelli, L.; Cerqueni, G.; Hosein, A.; Marchi, S.; Gigante, A.; Mattioli-Belmonte, M. Heterotopic ossification in a patient with diffuse idiopathic skeletal hyperostosis: Input from histological findings. Eur. J. Histochem. 2020, 64, 3176. [Google Scholar] [CrossRef] [PubMed]


| TSD Group (N = 11) | Control Group (N = 10) | p Value | |
|---|---|---|---|
| Sex | Male 2, Female 9 | Male 2, Female 8 | 0.916 |
| Age (year) | 81.8 ± 7.1 | 81.9 ± 8.6 | 0.981 |
| Follow-up time (month) | 15.4 ± 6.6 | 19.4 ± 8.4 | 0.236 |
| Fracture region | Th11: 2, Th12: 1, L1: 6, L2: 1, L3: 1 | Th10: 1, Th11: 1, Th12: 4, L1: 1, L2: 1, L4: 2 |
| TSD Group (n = 11) | Control Group (n = 10) | p Value | |
|---|---|---|---|
| Number of fused segments | 5 ± 1 | 5 ± 1 | 0.433 |
| Operative time (min) | 164 ± 57 | 168 ± 60 | 0.900 |
| Blood loss (mL) | 306 ± 334 | 528 ± 659 | 0.334 |
| Screw loosening (n) | 3 (27%) | 6 (60%) | 0.198 |
| Bone union at final follow-up (n) | 11 (100%) | 8 (80%) | 0.214 |
| Implant back-out (n) | 0 (0%) | 4 (40%) | 0.035 * |
| Reoperation (n) | 0 (0%) | 3 (30%) | 0.090 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Published by MDPI on behalf of the Lithuanian University of Health Sciences. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ugawa, R.; Fujiwara, Y.; Matsumoto, T. Clinical Outcomes of Transdiscal Screws for Thoracolumbar Spinal Fractures with Marked Anterior Distraction Gap Accompanied by Diffuse Idiopathic Skeletal Hyperostosis. Medicina 2025, 61, 1874. https://doi.org/10.3390/medicina61101874
Ugawa R, Fujiwara Y, Matsumoto T. Clinical Outcomes of Transdiscal Screws for Thoracolumbar Spinal Fractures with Marked Anterior Distraction Gap Accompanied by Diffuse Idiopathic Skeletal Hyperostosis. Medicina. 2025; 61(10):1874. https://doi.org/10.3390/medicina61101874
Chicago/Turabian StyleUgawa, Ryo, Yoshihiro Fujiwara, and Toshiyuki Matsumoto. 2025. "Clinical Outcomes of Transdiscal Screws for Thoracolumbar Spinal Fractures with Marked Anterior Distraction Gap Accompanied by Diffuse Idiopathic Skeletal Hyperostosis" Medicina 61, no. 10: 1874. https://doi.org/10.3390/medicina61101874
APA StyleUgawa, R., Fujiwara, Y., & Matsumoto, T. (2025). Clinical Outcomes of Transdiscal Screws for Thoracolumbar Spinal Fractures with Marked Anterior Distraction Gap Accompanied by Diffuse Idiopathic Skeletal Hyperostosis. Medicina, 61(10), 1874. https://doi.org/10.3390/medicina61101874






