A Minimally Invasive Fixation Versus Double Plating of Associated Posterior Malleolus and Fibula Fractures—A Comparative Human Cadaveric Biomechanical Study
Abstract
1. Introduction
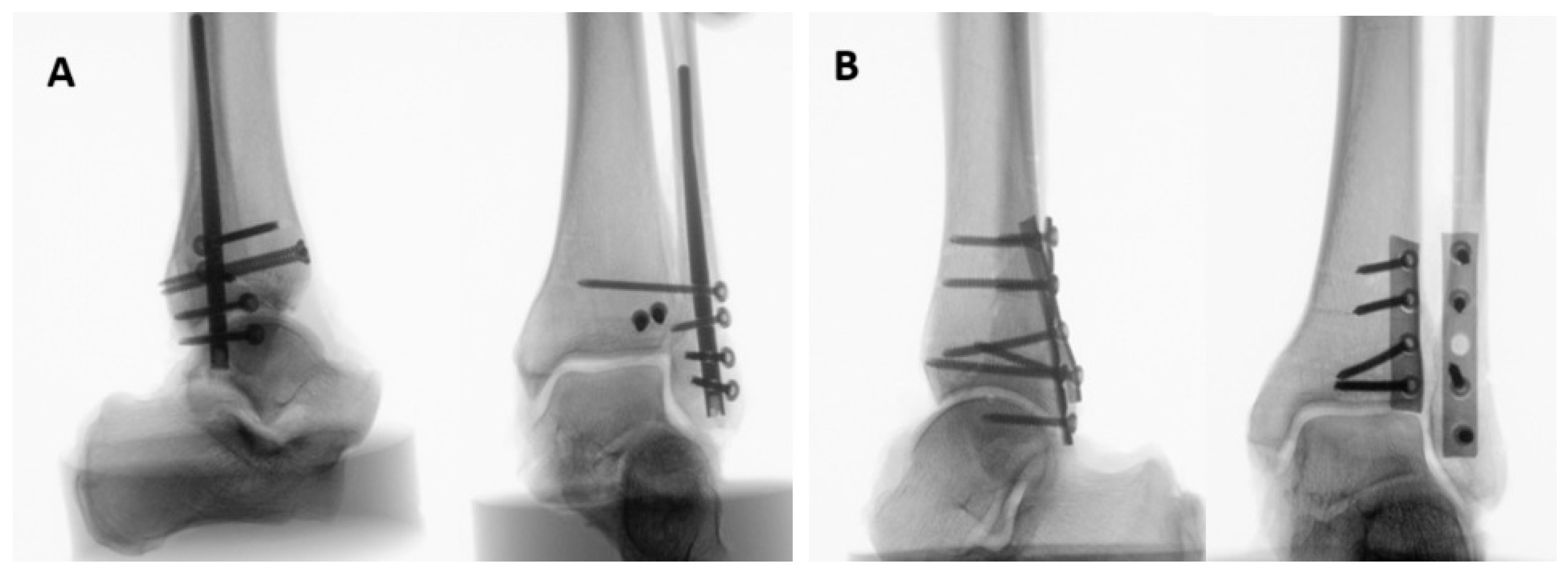
2. Materials and Methods
2.1. Specimens and Preparation
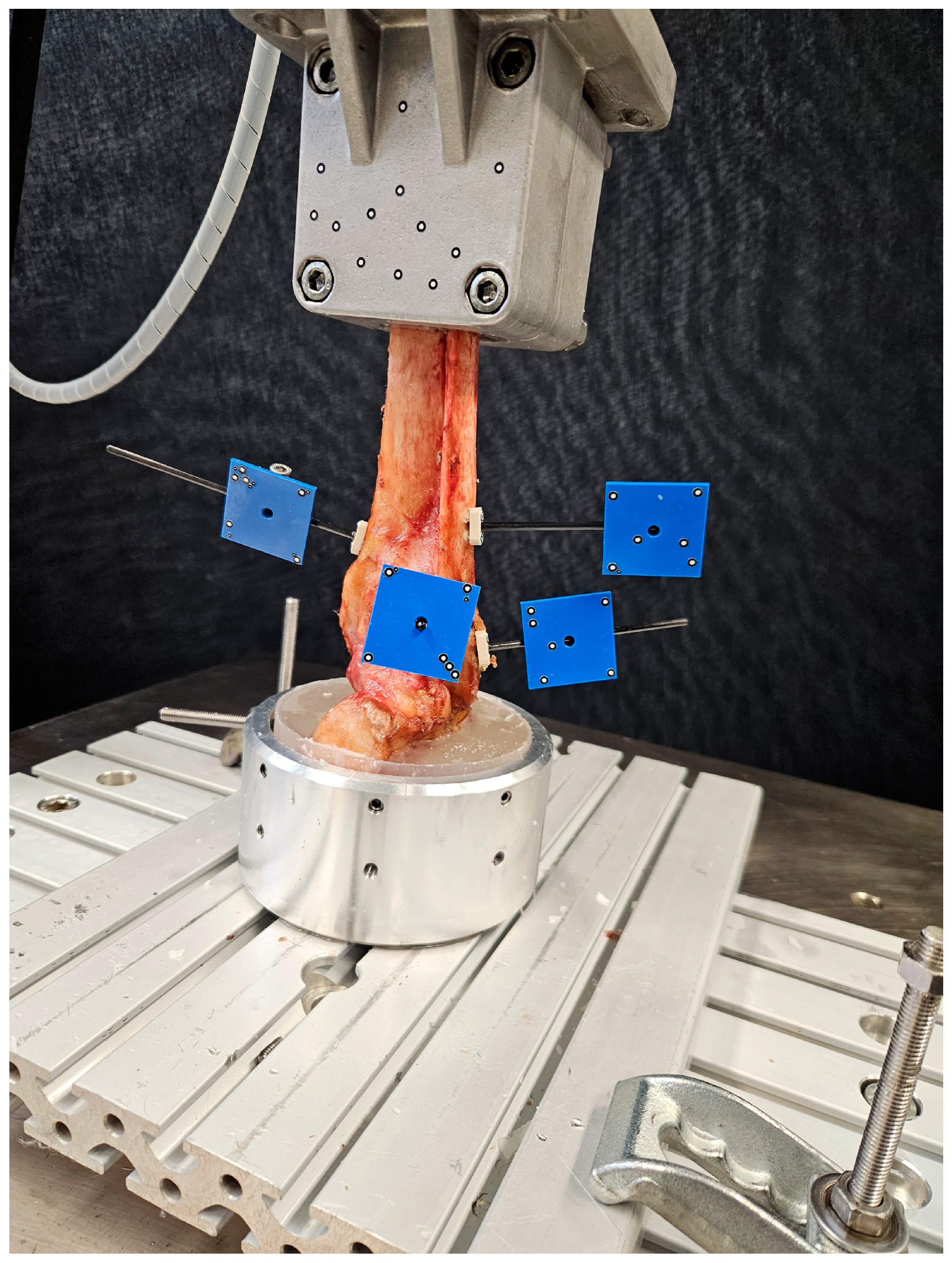
2.2. Biomechanical Testing
2.3. Data Acquisition and Evaluation
2.4. Statistical Analysis
3. Results
3.1. Initial Axial Stiffness
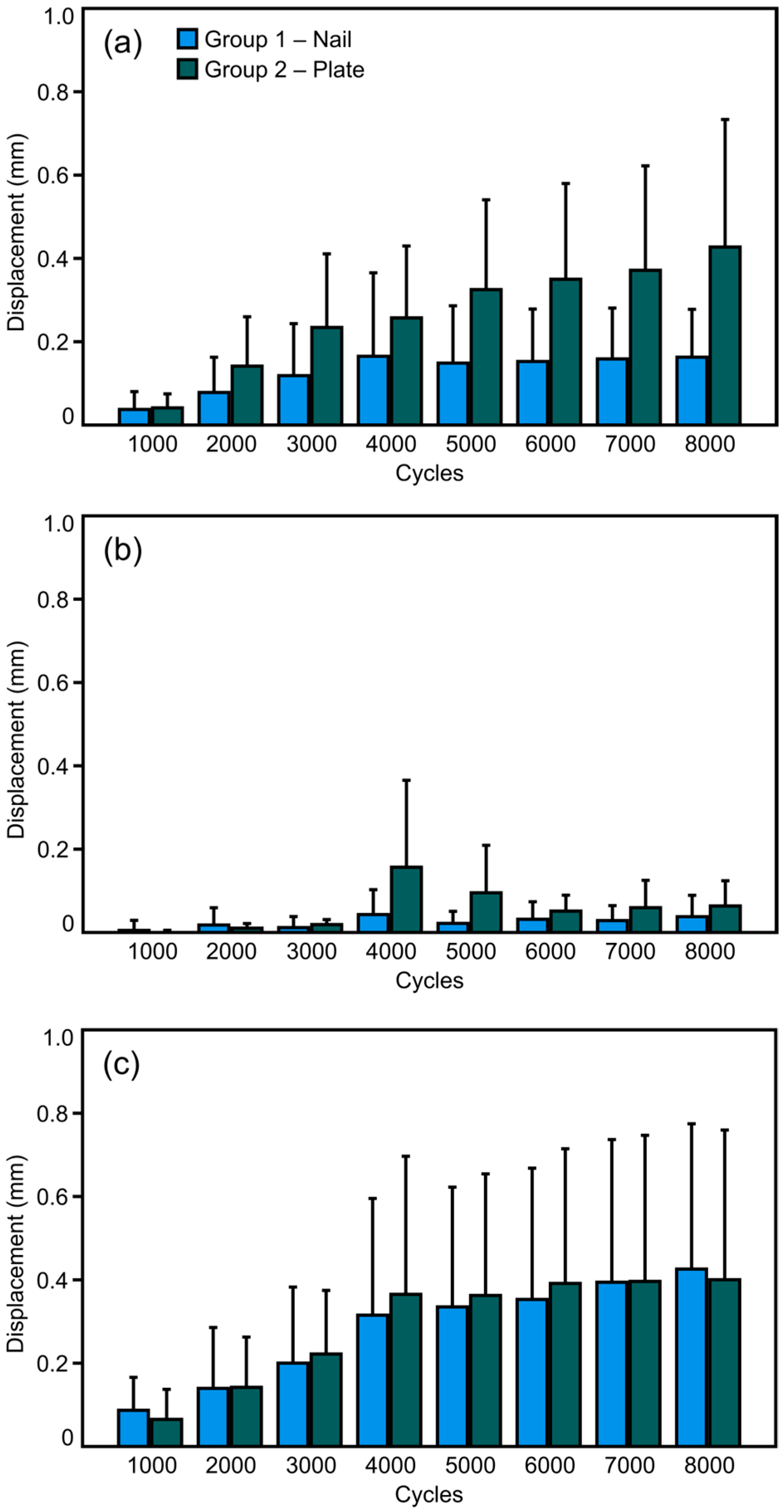
3.2. Fracture Displacement
3.3. Cycles to Failure
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Rydberg, E.M.; Wennergren, D.; Stigevall, C.; Ekelund, J.; Möller, M. Epidemiology of more than 50,000 ankle fractures in the Swedish Fracture Register during a period of 10 years. J. Orthop. Surg. Res. 2023, 18, 79. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Koval, K.J.; Lurie, J.; Zhou, W.; Sparks, M.B.; Cantu, R.V.; Sporer, S.M.; Weinstein, J.D. Ankle fractures in the elderly: What you get depends on where you live and who you see. J. Orthop. Trauma 2005, 19, 635–639. [Google Scholar] [CrossRef] [PubMed]
- Li, Y.; Luo, R.; Li, B.; Xia, J.; Zhou, H.; Huang, H.; Yang, Y. Analysis of the epidemiological characteristics of posterior malleolus fracture in adults. J. Orthop. Surg. Res. 2023, 18, 507. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Miller, A.G.; Margules, A.; Raikin, S.M. Risk factors for wound complications after ankle fracture surgery. J. Bone Jt. Surg. Am. 2012, 94, 2047–2052. [Google Scholar] [CrossRef] [PubMed]
- Lopez-Capdevila, L.; Rios-Ruh, J.M.; Fortuño, J.; Costa, A.E.; Santamaria-Fumas, A.; Dominguez-Sevilla, A.; Sales-Perez, M. Diabetic ankle fracture complications: A meta-analysis. Foot Ankle Surg. 2021, 27, 832–837. [Google Scholar] [CrossRef] [PubMed]
- SooHoo, N.F.; Krenek, L.; Eagan, M.J.; Gurbani, B.; Ko, C.Y.; Zingmond, D.S. Complication rates following open reduction and internal fixation of ankle fractures. J. Bone Jt. Surg. Am. 2009, 91, 1042–1049. [Google Scholar] [CrossRef] [PubMed]
- de Pinho Tavares, C.M.; Castilho, R.S.; Lopes, F.A.S.; Baumfeld, D.S.; Silva, T.A.A.; de Almeida Pinto, R.Z. Incidence of early complications in the posterolateral approach to posterior malleolus fractures. J. Foot Ankle 2020, 14, 178–182. [Google Scholar] [CrossRef]
- Bua, N.; Jeyaseelan, L.A.; Parker, L.; Trockels, A.; Sohrabi, C.; Vris, A.; Heidari, N.; Romans, F.M. Outcomes of Posterior Malleolar Fixation in Ankle Fractures in A Major Trauma Centre. Foot Ankle Orthop. 2022, 7, 2473011421S00121. [Google Scholar] [CrossRef] [PubMed Central]
- Neumann, A.P.; Kroker, L.; Beyer, F.; Rammelt, S. Complications following surgical treatment of posterior malleolar fractures: An analysis of 300 cases. Arch. Orthop. Trauma Surg. 2023, 143, 3129–3136. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Abdelgaid, S.M.; Moursy, A.F.; Elgebaly, E.A.A.; Aboelenien, A.M. Minimally Invasive Treatment of Ankle Fractures in Patients at High Risk of Soft Tissue Wound Healing Complications. J. Foot Ankle Surg. 2018, 57, 557–571. [Google Scholar] [CrossRef] [PubMed]
- Wordie, S.J.; Carter, T.H.; MacDonald, D.; Duckworth, A.D.; White, T.O. Percutaneous Fixation of Posterior Malleolar Fractures in Patients with Unstable Ankle Fractures Treated with a Fibular Intramedullary Nail: A Description of a Technique and Review of Outcomes. J. Orthop. Trauma 2022, 36, 195–200. [Google Scholar] [CrossRef] [PubMed]
- Kohler, F.C.; Schenk, P.; Nies, T.; Hallbauer, J.; Hofmann, G.O.; Biedermann, U.; Kielstein, H.; Wildemann, B.; Ramm, R.; Ullrich, B.W. Fibula Nail versus Locking Plate Fixation-A Biomechanical Study. J. Clin. Med. 2023, 12, 698. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Carter, T.H.; Wallace, R.; Mackenzie, S.A.; Oliver, W.M.; Duckworth, A.D.; White, T.O. The Fibular Intramedullary Nail Versus Locking Plate and Lag Screw Fixation in the Management of Unstable Elderly Ankle Fractures: A Cadaveric Biomechanical Comparison. J. Orthop. Trauma 2020, 34, e401–e406. [Google Scholar] [CrossRef] [PubMed]
- Smith, G.; Mackenzie, S.P.; Wallace, R.J.; Carter, T.; White, T.O. Biomechanical Comparison of Intramedullary Fibular Nail Versus Plate and Screw Fixation. Foot Ankle Int. 2017, 38, 1394–1399. [Google Scholar] [CrossRef] [PubMed]
- Switaj, P.J.; Fuchs, D.; Alshouli, M.; Patwardhan, A.G.; Voronov, L.I.; Muriuki, M.; Havey, R.M.; Kadakia, A.R. A biomechanical comparison study of a modern fibular nail and distal fibular locking plate in AO/OTA 44C2 ankle fractures. J. Orthop. Surg. Res. 2016, 11, 100. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Attia, A.K.; Fayed, A.; Mahmoud, K.; Labib, S.A.; Aydogan, U.; Juliano, P. Locked intramedullary nailing provides superior functional outcomes and lower complication rates than plate fixation of distal fibula fractures. A systematic review and meta-analysis of comparative studies. Foot Ankle Surg. 2022, 28, 986–994. [Google Scholar] [CrossRef] [PubMed]
- Brown, O.L.; Dirschl, D.R.; Obremskey, W.T. Incidence of hardware-related pain and its effect on functional outcomes after open reduction and internal fixation of ankle fractures. J. Orthop. Trauma 2001, 15, 271–274. [Google Scholar] [CrossRef] [PubMed]
- Schumann, J.; Burgess, B.; Ryan, D.; Garras, D. A Retrospective Analysis of Distal Fibula Fractures Treated with Intramedullary Fibular Nail Fixation. J. Foot Ankle Surg. 2023, 62, 737–741. [Google Scholar] [CrossRef] [PubMed]
- Vidović, D.; Elabjer, E.; Muškardin, I.; Milosevic, M.; Bekic, M.; Bakota, B. Posterior fragment in ankle fractures: Anteroposterior vs posteroanterior fixation. Injury 2017, 48 (Suppl. S5), S65–S69. [Google Scholar] [CrossRef] [PubMed]
- Saltzman, C.L.; Anderson, R.B.; Coughlin, M.J. Mann’s Surgery of the Foot and Ankle, 9th ed.; Saunders/Elsevier: Philadelphia, PA, USA, 2014. [Google Scholar]
- Rodriguez-Materon, S.; Trynz, S.; Fanfan, D.; Fleites, J.; Gil, J.; Hodgkins, C. Use of Fibula Nails with Proximal and Distal Fixation. Foot Ankle Orthop. 2024, 9, 24730114241230563. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Langenhuijsen, J.F.; Heetveld, M.J.; Ultee, J.M.; Steller, E.P.; Butzelaar, R.M.J.M. Results of ankle fractures with involvement of the posterior tibial margin. J. Trauma 2002, 53, 55–60. [Google Scholar] [CrossRef]
- Anwar, A.; Zhang, Z.; Lv, D.; Lv, G.; Zhao, Z.; Wang, Y.; Cai, Y.; Qasim, W.; Nazir, M.U.; Lu, M. Biomechanical efficacy of AP, PA lag screws and posterior plating for fixation of posterior malleolar fractures: A three dimensional finite element study. BMC Musculoskelet. Disord. 2018, 19, 73. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- O’COnnor, T.J.; Mueller, B.; Ly, T.V.; Jacobson, A.R.; Nelson, E.R.; Cole, P.A. “A to p” screw versus posterolateral plate for posterior malleolus fixation in trimalleolar ankle fractures. J. Orthop. Trauma 2015, 29, e151–e156. [Google Scholar] [CrossRef] [PubMed]
- Gao, Y.; Liu, Y.; Zhao, Y.; Shan, L.; Wang, H.; Xu, X.; Zhao, B.; Zhou, J. Comparison between anterior-to-posterior screw fixation versus posterolateral approach plate fixation for posterior malleous fracture: A systematic review and meta-analysis. Foot Ankle Surg. 2024, 30, 594–602. [Google Scholar] [CrossRef] [PubMed]
- Baecker, H.C.; Vosseller, J.T. Fibula Fracture: Plate versus Nail Fixation. Clin. Orthop. Surg. 2020, 12, 529–534. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Miller, A.N.; Carroll, E.A.; Parker, R.J.; Helfet, D.L.; Lorich, D.G. Posterior malleolar stabilization of syndesmotic injuries is equivalent to screw fixation. Clin. Orthop. Relat. Res. 2010, 468, 1129–1135. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Bugler, K.E.; Watson, C.D.; Hardie, A.R.; Appleton, P.; McQueen, M.M.; Court-Brown, C.M.; White, T.O. The treatment of unstable fractures of the ankle using the Acumed fibular nail: Development of a technique. J. Bone Jt. Surg. Br. 2012, 94, 1107–1112. [Google Scholar] [CrossRef] [PubMed]


Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Published by MDPI on behalf of the Lithuanian University of Health Sciences. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ganchev, K.; Penev, P.; Zderic, I.; Klos, K.; Richards, R.G.; Raykov, D.; Gueorguiev, B.; Llano, L.; Stoffel, K. A Minimally Invasive Fixation Versus Double Plating of Associated Posterior Malleolus and Fibula Fractures—A Comparative Human Cadaveric Biomechanical Study. Medicina 2025, 61, 1847. https://doi.org/10.3390/medicina61101847
Ganchev K, Penev P, Zderic I, Klos K, Richards RG, Raykov D, Gueorguiev B, Llano L, Stoffel K. A Minimally Invasive Fixation Versus Double Plating of Associated Posterior Malleolus and Fibula Fractures—A Comparative Human Cadaveric Biomechanical Study. Medicina. 2025; 61(10):1847. https://doi.org/10.3390/medicina61101847
Chicago/Turabian StyleGanchev, Konstantin, Preslav Penev, Ivan Zderic, Kajetan Klos, R. Geoff Richards, Dimitar Raykov, Boyko Gueorguiev, Lionel Llano, and Karl Stoffel. 2025. "A Minimally Invasive Fixation Versus Double Plating of Associated Posterior Malleolus and Fibula Fractures—A Comparative Human Cadaveric Biomechanical Study" Medicina 61, no. 10: 1847. https://doi.org/10.3390/medicina61101847
APA StyleGanchev, K., Penev, P., Zderic, I., Klos, K., Richards, R. G., Raykov, D., Gueorguiev, B., Llano, L., & Stoffel, K. (2025). A Minimally Invasive Fixation Versus Double Plating of Associated Posterior Malleolus and Fibula Fractures—A Comparative Human Cadaveric Biomechanical Study. Medicina, 61(10), 1847. https://doi.org/10.3390/medicina61101847






