Comparison of Ultrasound-Guided Quadratus Lumborum Plane Block and External Oblique Intercostal Plane Block for Postoperative Analgesia After Laparoscopic Cholecystectomy: A Two-Center Randomized Controlled Trial
Abstract
1. Introduction
2. Materials and Methods
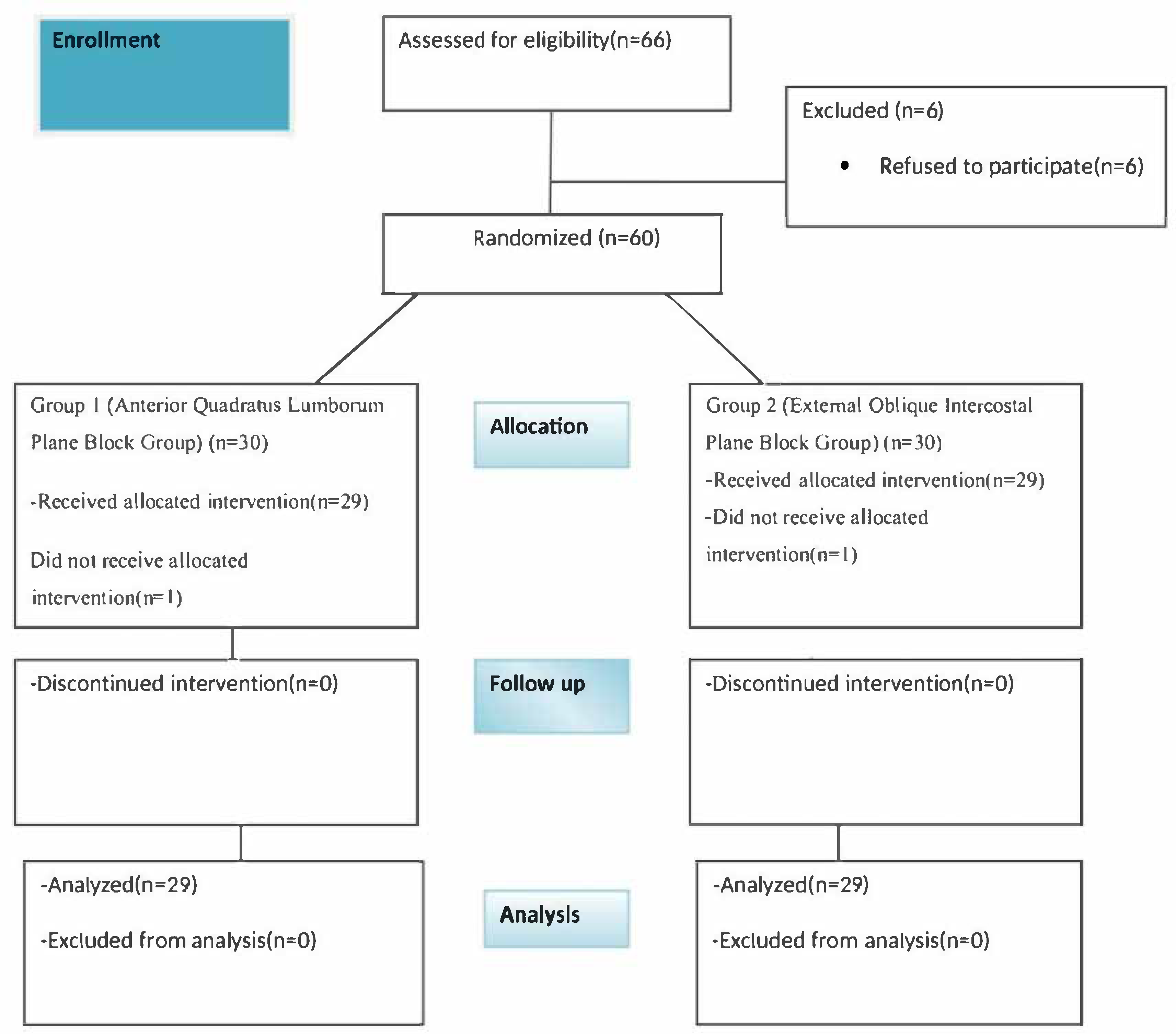
2.1. Study Design, Population, and Data
2.2. Procedure
2.2.1. Preoperative Period
2.2.2. Anesthesia Induction and Maintenance
2.2.3. Block Procedure
Group 1 (QLB)
Grup 2 (EOIPB)
2.2.4. Final Stage of the Operation
2.2.5. Postoperative Period
2.3. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Aygun, H.; Kavrut Ozturk, N.; Pamukcu, A.S.; Inal, A.; Kiziloglu, I.; Thomas, D.T.; Tulgar, S.; Nart, A. Comparison of ultrasound guided Erector Spinae Plane Block and quadratus lumborum block for postoperative analgesia in laparoscopic cholecystectomy patients; a prospective randomized study. J. Clin. Anesth. 2020, 62, 109696. [Google Scholar] [CrossRef] [PubMed]
- Ökmen, K.; Metin Ökmen, B.; Topal, S. Ultrasound-guided posterior quadratus lumborum block for postoperative pain after laparoscopic cholecystectomy: A randomized controlled double blind study. J. Clin. Anesth. 2018, 49, 112–117. [Google Scholar] [CrossRef] [PubMed]
- Vamnes, J.S.; Sørenstua, M.; Solbakk, K.I.; Sterud, B.; Leonardsen, A.C. Anterior quadratus lumborum block for ambulatory laparoscopic cholecystectomy: A randomized controlled trial. Croat. Med. J. 2021, 62, 137–145. [Google Scholar] [CrossRef] [PubMed]
- Baytar, Ç.; Yılmaz, C.; Karasu, D.; Topal, S. Comparison of Ultrasound-Guided Subcostal Transversus Abdominis Plane Block and Quadratus Lumborum Block in Laparoscopic Cholecystectomy: A Prospective, Randomized, Controlled Clinical Study. Pain Res. Manag. 2019, 2019, 2815301. [Google Scholar] [CrossRef]
- Alsharari, A.F.; Abuadas, F.H.; Alnassrallah, Y.S.; Salihu, D. Transversus Abdominis Plane Block as a Strategy for Effective Pain Management in Patients with Pain during Laparoscopic Cholecystectomy: A Systematic Review. J. Clin. Med. 2022, 11, 6896. [Google Scholar] [CrossRef]
- Ibrahim, M. Erector Spinae Plane Block in Laparoscopic Cholecystectomy, Is There a Difference? A Randomized Controlled Trial. Anesth. Essays Res. 2020, 14, 119–126. [Google Scholar] [CrossRef]
- Mehmet Selim, Ç.; Halide, S.; Erkan Cem, Ç.; Onur, K.; Sedat, H.; Senem, U. Efficacy of Unilateral External Oblique Intercostal Fascial Plane Block Versus Subcostal TAP Block in Laparoscopic Cholecystectomy: Randomized, Prospective Study. Surg. Innov. 2024, 31, 381–388. [Google Scholar] [CrossRef]
- He, W.Q.; Li, Y.J.; Li, Y.S.; Zhang, X.-H.; Cao, J.; Lu, K.-Z.; Cheung, C.W.; Gu, J.-T.; Xia, Z.-Y.; Yi, B. Advantages of Transmuscular Quadratus Lumborum Block via Subfascial Approach Versus Extrafascial Approach for Postoperative Analgesia After Laparoscopic Cholecystectomy: A Randomized Controlled Study. Clin. J. Pain 2022, 38, 730–738. [Google Scholar] [CrossRef]
- Hamilton, D.L.; Manickam, B.P.; Wilson, M.A.J.; Abdel Meguid, E. External oblique fascial plane block. Reg. Anesth. Pain Med. 2019, 44, 528–529. [Google Scholar] [CrossRef]
- Elsharkawy, H.; Kolli, S.; Soliman, L.M.; Seif, J.; Drake, R.L.; Mariano, E.R.; El-Boghdadly, K. The External Oblique Intercostal Block: Anatomic Evaluation and Case Series. Pain Med. 2021, 22, 2436–2442. [Google Scholar] [CrossRef]
- Salmonsen, C.B.; Lange, K.H.W.; Rothe, C.; Kleif, J.; Bertelsen, C.A. Cutaneous sensory block area of the ultrasound-guided subcostal transversus abdominis plane block: An observational study. Reg. Anesth. Pain Med. 2024, 49, 289–292. [Google Scholar] [CrossRef]
- Fernández Martín, M.T.; López Álvarez, S.; Pérez Herrero, M.A. Serratus-intercostal interfascial block as an opioid-saving strategy in supra-umbilical open surgery. Bloqueo interfascial serrato-intercostal como estrategia ahorradora de opioides en cirugía supraumbilical abierta. Rev. Esp. Anestesiol. Reanim. 2018, 65, 456–460. [Google Scholar] [CrossRef]
- Cesana, B.M.; Cavaliere, F. Could the use of a table make power analysis description more reader-friendly? Minerva Anestesiol. 2020, 86, 1003–1005. [Google Scholar] [CrossRef] [PubMed]
- Ozdemir, H.; Araz, C.; Karaca, O.; Turk, E. Comparison of Ultrasound-Guided Erector Spinae Plane Block and Subcostal Transversus Abdominis Plane Block for Postoperative Analgesia after Laparoscopic Cholecystectomy: A Randomized, Controlled Trial. J. Invest. Surg. 2022, 35, 870–877. [Google Scholar] [CrossRef] [PubMed]
- Lee, D.K. Alternatives to P value: Confidence interval and effect size. Korean J. Anesthesiol. 2016, 69, 555–562. [Google Scholar] [CrossRef]
- Mitra, S.; Khandelwal, P.; Roberts, K.; Kumar, S.; Vadivelu, N. Pain relief in laparoscopic cholecystectomy—A review of the current options. Pain. Pract. 2012, 12, 485–496. [Google Scholar] [CrossRef]
- Li, T.T.; Chang, Q.Y.; Xiong, L.L.; Chen, Y.-J.; Li, Q.-J.; Liu, F.; Wang, T.-H. Patients with gastroenteric tumor after upper abdominal surgery were more likely to require rescue analgesia than lower abdominal surgery. BMC Anesthesiol. 2022, 22, 156. [Google Scholar] [CrossRef]
- Ragupathy, R.; Prabhu, S.C.G.; Thiyagarajan, D.; Anto, V. Opioid-free anaesthesia for laparoscopic surgeries—A prospective non-randomised study in a tertiary care hospital. Indian J. Anaesth. 2022, 66, 207–212. [Google Scholar] [CrossRef]
- Vrsajkov, V.; Ilić, N.; Uvelin, A.; Ilić, R.; Lukić-Šarkanović, M.; Plećaš-Đurić, A. Erector spinae plane block reduces pain after laparoscopic cholecystectomy. Blockierung der Erector-spinae-Ebene reduziert Schmerzen nach laparoskopischer Cholezystektomie. Anaesthesist 2021, 70 (Suppl. 1), 48–52. [Google Scholar] [CrossRef]
- Elsharkawy, H.; Maniker, R.; Bolash, R.; Kalasbail, P.; Drake, R.L.; Elkassabany, N. Rhomboid Intercostal and Subserratus Plane Block: A Cadaveric and Clinical Evaluation. Reg. Anesth. Pain Med. 2018, 43, 745–751. [Google Scholar] [CrossRef]
- De Cassai, A.; Sella, N.; Geraldini, F.; Tulgar, S.; Ahiskalioglu, A.; Dost, B.; Manfrin, S.; Karapinar, Y.E.; Paganini, G.; Beldagli, M.; et al. Single-shot regional anesthesia for laparoscopic cholecystectomies: A systematic review and network meta-analysis. Korean J. Anesthesiol. 2023, 76, 34–46. [Google Scholar] [CrossRef] [PubMed]
- Korgvee, A.; Junttila, E.; Koskinen, H.; Huhtala, H.; Kalliomaki, M.L. Ultrasound-guided quadratus lumborum block for postoperative analgesia: A systematic review and meta-analysis. Eur. J. Anaesthesiol. 2021, 38, 115–129. [Google Scholar] [CrossRef] [PubMed]
- Evans, B.G.A.; Ihnat, J.M.H.; Zhao, K.L.; Kim, L.; Pierson, D.; Yu, C.T.; Lin, H.-M.; Li, J.; Golshan, M.; Ayyala, H.S. Meta-analysis: The utility of the anterior quadratus lumborum block in abdominal surgery. Am. J. Surg. 2025, 239, 116014. [Google Scholar] [CrossRef] [PubMed]
- Hamilton, D.L.; Manickam, B.P. Is a Thoracic Fascial Plane Block the Answer to Upper Abdominal Wall Analgesia? Reg. Anesth. Pain Med. 2018, 43, 891–892. [Google Scholar] [CrossRef]
- Kavakli, A.S.; Sahin, T.; Koc, U.; Karaveli, A. Ultrasound-Guided External Oblique Intercostal Plane Block for Postoperative Analgesia in Laparoscopic Sleeve Gastrectomy: A Prospective, Randomized, Controlled, Patient and Observer-Blinded Study. Obes. Surg. 2024, 34, 1505–1512. [Google Scholar] [CrossRef]
- Doymus, O.; Ahiskalioglu, A.; Kaciroglu, A.; Bedir, Z.; Tayar, S.; Yeni, M.; Karadeniz, E. External Oblique Intercostal Plane Block Versus Port-Site Infiltration for Laparoscopic Sleeve Gastrectomy: A Randomized Controlled Study. Obes. Surg. 2024, 34, 1826–1833. [Google Scholar] [CrossRef]
- Petiz, C.; Barbosa, R.; Ribeiro Boneco, T.; Pacheco, J.; Resende, A. External Oblique Intercostal Block for Living Kidney Donor Open Nephrectomy: A Case Series. Cureus 2023, 15, e39139. [Google Scholar] [CrossRef]
- Liotiri, D.; Diamantis, A.; Papapetrou, E.; Grapsidi, V.; Sioka, E.; Stamatiou, G.; Zacharoulis, D. External oblique intercostal (EOI) block for enhanced recovery after liver surgery: A case series. Anaesth. Rep. 2023, 11, e12225. [Google Scholar] [CrossRef]
- Coşarcan, S.K.; Erçelen, Ö. The analgesic contribution of external oblique intercostal block: Case reports of 3 different surgeries and 3 spectacular effects. Medicine 2022, 101, e30435. [Google Scholar] [CrossRef]
- Lee, S.H.; Sohn, J.T. Mechanisms underlying lipid emulsion resuscitation for drug toxicity: A narrative review. Korean J. Anesthesiol. 2023, 76, 171–182. [Google Scholar] [CrossRef]
- Uppal, V.; Retter, S.; Kehoe, E.; McKeen, D.M. Quadratus lumborum block for postoperative analgesia: A systematic review and meta-analysis. Bloc du muscle du carré des lombes (quadratus lomburum) pour l’analgésie postopératoire: Revue systématique et méta-analyse. Can. J. Anaesth. 2020, 67, 1557–1575. [Google Scholar] [CrossRef]
- Liu, X.; Song, T.; Chen, X.; Zhang, J.; Shan, C.; Chang, L.; Xu, H. Quadratus lumborum block versus transversus abdominis plane block for postoperative analgesia in patients undergoing abdominal surgeries: A systematic review and meta-analysis of randomized controlled trials. BMC Anesthesiol. 2020, 20, 53. [Google Scholar] [CrossRef] [PubMed]
- Akerman, M.; Pejčić, N.; Veličković, I. A Review of the Quadratus Lumborum Block and ERAS. Front. Med. 2018, 5, 44. [Google Scholar] [CrossRef] [PubMed]
- Tanggaard, K.; Gronlund, C.; Nielsen, M.V.; la Cour, K.; Tvarnø, C.D.; Børglum, J.; Maagaard, M.; Mathiesen, O. Anterior quadratus lumborum blocks for postoperative pain treatment following intra-abdominal surgery: A systematic review with meta-analyses and trial sequential analyses. Acta Anaesthesiol. Scand. 2025, 69, e14526. [Google Scholar] [CrossRef] [PubMed]
- Hassanein, A.; Abdel-Haleem, M.; Mohamed, S.R. Regional Analgesia for Laparoscopic Cholecystectomy Using Ultrasound-guided Quadratus Lumborum Block or Erector Spinae Block: A Randomized Controlled Trial. Pain Physician 2023, 26, E133–E141. [Google Scholar] [CrossRef]
| We performed the POWER analysis | Before starting |
| On the primary outcome | NRS |
| Based on the two-tailed statistical test: | Two-tailed |
| And accepting the cutoff for significance (α) | 0.05 |
| And a power (1 − β) of | 0.90 |
| The variability of the primary outcome was | In the study by Özdemir et al., 2 h NRS scores were taken into account (mean + SD for group 1 = 1.4 ± 0.9 and for group 2 = 2.4 ± 1.1) [14] |
| Consequently, the effect size was | 0.99 |
| The total sample size needed was | 48 |
| Characteristic | All Patients (N= 58) | Group 1 (n = 29) | Group 2 (n = 29) | p-Value |
|---|---|---|---|---|
| Mean ± SD | Mean ± SD | Mean ± SD | ||
| Age (years) | 43.50 ± 9.80 | 42.83 ± 8.12 | 44.17 ± 11.33 | 0.60 |
| BMI (kg/m2) | 28.02 ± 3.63 | 27.68 ± 3.35 | 28.36 ± 3.92 | 0.47 |
| Median (IQR) | Median (IQR) | Median (IQR) | ||
| Surgery duration (min) | 59 (52–60.25) | 60 (55–60) | 56 (51–62) | 0.53 |
| Anesthesia duration (min) | 70 (68–80) | 70 (70–80) | 70 (64–79) | 0.13 |
| n (%) | n (%) | n (%) | ||
| Gender | 0.26 | |||
| Male | 20 (%) | 12 (%41) | 8 (%27) | |
| Female | 38 (%) | 17 (%59) | 21 (%73) | |
| Comorbidity | 1 | |||
| Yes | 12 (%21) | 6 (%21) | 6 (%21) | |
| No | 46 (%79) | 23 (%79) | 23 (%79) | |
| ASA | 0.59 | |||
| I | 28 (%48) | 15 (%52) | 13 (%45) | |
| II | 30 (%52) | 14 (%48) | 16 (%55) |
| Group 1 (n = 29) | Group 2 (n = 29) | Effect Size (r) | p-Value | Bonferroni α = 0.01 | |
|---|---|---|---|---|---|
| Median (IQR) | Median (IQR) | ||||
| NRS1 | 2 (1–2) | 3 (2–4) | 0.37 (medium) | 0.005 | Significant |
| NRS2 | 2 (2–2.5) | 2 (2–3.5) | 0.23 (small) | 0.074 | NS |
| NRS3 | 2 (1–2) | 2 (1–3.5) | 0.29 (small-medium) | 0.028 | NS |
| NRS4 | 1 (1–2) | 3 (2–5) | 0.61 (large) | <0.000 | Significant |
| NRS5 | 1 (1–1) | 2 (1.5–3) | 0.52 (large) | <0.000 | Significant |
| Group 1 (n = 29) | Group 2 (n = 29) | p-Value | |
|---|---|---|---|
| n (%) | n (%) | ||
| RSAS Score | 0.005 | ||
| 1 Unarousable | 0 (%) | 0 (%0) | |
| 2 Very sedated | 4 (%) | 0 (%) | |
| 3 Sedated | 12 (%) | 8 (%) | |
| 4 Calm and cooperative | 9 (%) | 9 (%) | |
| 5 Agitated | 4 (%) | 10 (%) | |
| 6 Very agitated | 0 (%) | 2 (%) | |
| 7 Dangerously agitated | 0 (%0) | 0 (%0) |
| Group 1 (n = 29) | Group 2 (n = 29) | Effect Size (r) | p-Value | |
|---|---|---|---|---|
| Median (IQR) | Median (IQR) | |||
| Amount of Tramadol Used (mg) | 0 (0–0) | 0 (0–100) | 0.46 (small-medium) | <0.000 |
| Group 1 (n = 29) | Group 2 (n = 29) | p-Value | |
|---|---|---|---|
| n (%) | n (%) | ||
| Patient Satisfaction Score | <0.000 | ||
| Very dissatisfied | 0 (%) | 0 (%) | |
| Somewhat dissatisfied | 0 (%) | 7 (%) | |
| Neutral | 2 (%) | 9 (%) | |
| Quite satisfied | 13 (%) | 10 (%) | |
| Very satisfied | 14 (%) | 3 (%) | |
| Side Effects (Nausea–Vomiting) | 0.68 | ||
| Yes | 3 (%) | 4 (%) | |
| No | 26 (%) | 25 (%) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Published by MDPI on behalf of the Lithuanian University of Health Sciences. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kaçar, C.K.; Dedeoğlu, A.; Tosun Söner, H.; Çelik, E.; Andıç, O.; Acil, F.; Akelma, H.; Uzundere, O.; Gökçek, E. Comparison of Ultrasound-Guided Quadratus Lumborum Plane Block and External Oblique Intercostal Plane Block for Postoperative Analgesia After Laparoscopic Cholecystectomy: A Two-Center Randomized Controlled Trial. Medicina 2025, 61, 1838. https://doi.org/10.3390/medicina61101838
Kaçar CK, Dedeoğlu A, Tosun Söner H, Çelik E, Andıç O, Acil F, Akelma H, Uzundere O, Gökçek E. Comparison of Ultrasound-Guided Quadratus Lumborum Plane Block and External Oblique Intercostal Plane Block for Postoperative Analgesia After Laparoscopic Cholecystectomy: A Two-Center Randomized Controlled Trial. Medicina. 2025; 61(10):1838. https://doi.org/10.3390/medicina61101838
Chicago/Turabian StyleKaçar, Cem Kıvılcım, Andaç Dedeoğlu, Hülya Tosun Söner, Enes Çelik, Okan Andıç, Fatma Acil, Hakan Akelma, Osman Uzundere, and Erhan Gökçek. 2025. "Comparison of Ultrasound-Guided Quadratus Lumborum Plane Block and External Oblique Intercostal Plane Block for Postoperative Analgesia After Laparoscopic Cholecystectomy: A Two-Center Randomized Controlled Trial" Medicina 61, no. 10: 1838. https://doi.org/10.3390/medicina61101838
APA StyleKaçar, C. K., Dedeoğlu, A., Tosun Söner, H., Çelik, E., Andıç, O., Acil, F., Akelma, H., Uzundere, O., & Gökçek, E. (2025). Comparison of Ultrasound-Guided Quadratus Lumborum Plane Block and External Oblique Intercostal Plane Block for Postoperative Analgesia After Laparoscopic Cholecystectomy: A Two-Center Randomized Controlled Trial. Medicina, 61(10), 1838. https://doi.org/10.3390/medicina61101838






