Low-Dose Subarachnoid Anesthesia Combined with PENG and FLCN Blocks Reduces Hypotensive Episodes Without Compromising Anesthetic Depth and Duration in Hip Fracture Surgery: A Retrospective Observational Study
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design and Ethics
2.2. Group Characteristics and Data Collection
2.3. Study Objectives
2.4. Variables, Data Handling, and Statistical Analysis
3. Results
4. Discussion
Study Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Sessler, D.I.; Bloomstone, J.A.; Aronson, S.; Berry, C.; Gan, T.J.; Kellum, J.A.; Plumb, J.; Mythen, M.G.; Grocott, M.P.; Edwards, M.R.; et al. Perioperative Quality Initiative consensus statement on intraoperative blood pressure, risk and outcomes for elective surgery. Br. J. Anaesth. 2019, 122, 563–574. [Google Scholar] [CrossRef] [PubMed]
- White, S.M.; Moppett, I.K.; Griffiths, R.; Johansen, A.; Wakeman, R.; Boulton, C.; Plant, F.; Williams, A.; Pappenheim, K.; Majeed, A.; et al. Secondary analysis of outcomes after 11,085 hip fracture operations from the prospective UK Anaesthesia Sprint Audit of Practice (ASAP-2). Anaesthesia 2016, 71, 506–514. [Google Scholar] [CrossRef]
- Wesselink, E.; Kappen, T.; Torn, H.; Slooter, A.; van Klei, W. Intraoperative hypotension and the risk of postoperative adverse outcomes: A systematic review. Br. J. Anaesth. 2018, 121, 706–721. [Google Scholar] [CrossRef]
- Gregory, A.; Stapelfeldt, W.H.; Khanna, A.K.; Smischney, N.J.; Boero, I.J.; Chen, Q.; Stevens, M.; Shaw, A.D. Intraoperative Hypotension Is Associated with Adverse Clinical Outcomes After Noncardiac Surgery. Anesth. Analg. 2021, 132, 1654–1665. [Google Scholar] [CrossRef]
- Sessler, D.I.; Sigl, J.C.; Kelley, S.D.; Chamoun, N.G.; Manberg, P.J.; Saager, L.; Kurz, A.; Greenwald, S. Hospital Stay and Mortality Are Increased in Patients Having a “Triple Low” of Low Blood Pressure, Low Bispectral Index, and Low Minimum Alveolar Concentration of Volatile Anesthesia. Anesthesiology 2012, 116, 1195–1203. [Google Scholar] [CrossRef]
- Wood, R.J.; White, S.M. Anaesthesia for 1131 patients undergoing proximal femoral fracture repair: A retrospective, observational study of effects on blood pressure, fluid administration and perioperative anaemia. Anaesthesia 2011, 66, 1017–1022. [Google Scholar] [CrossRef]
- Griffiths, R.; Babu, S.; Dixon, P.; Freeman, N.; Hurford, D.; Kelleher, E.; Moppett, I.; Ray, D.; Sahota, O.; Shields, M.; et al. Guideline for the management of hip fractures 2020. Anaesthesia 2021, 76, 225–237. [Google Scholar] [CrossRef]
- Azagra, R.; López-Expósito, F.; Martin-Sánchez, J.C.; Aguyé, A.; Moreno, N.; Cooper, C.; Díez-Pérez, A.; Dennison, E.M. Changing trends in the epidemiology of hip fracture in Spain. Osteoporos. Int. 2014, 25, 1267–1274. [Google Scholar] [CrossRef]
- The IOFCSA Working Group on Fracture, Epidemiology; Cooper, C.; Cole, Z.A.; Holroyd, C.R.; Earl, S.C.; Harvey, N.C.; Dennison, E.M.; Melton, L.J.; Cummings, S.R.; Kanis, J.A. Secular trends in the incidence of hip and other osteoporotic fractures. Osteoporos. Int. 2011, 22, 1277–1288. [Google Scholar] [CrossRef] [PubMed]
- Hoogendijk, E.O.; Afilalo, J.; Ensrud, K.E.; Kowal, P.; Onder, G.; Fried, L.P. Frailty: Implications for clinical practice and public health. Lancet 2019, 394, 1365–1375. [Google Scholar] [CrossRef] [PubMed]
- Huang, A.R.; Mallet, L.; Rochefort, C.M.; Eguale, T.; Buckeridge, D.L.; Tamblyn, R. Medication-related falls in the elderly: Causative factors and preventive strategies. Drugs Aging 2012, 29, 359–376. [Google Scholar] [CrossRef] [PubMed]
- Khalili, H.; Huang, E.S.; Jacobson, B.C.; Camargo, C.A.; Feskanich, D.; Chan, A.T. Use of proton pump inhibitors and risk of hip fracture in relation to dietary and lifestyle factors: A prospective cohort study. BMJ 2012, 344, e372. [Google Scholar] [CrossRef]
- Turner, M.R.; Camacho, X.; Fischer, H.D.; Austin, P.C.; Anderson, G.M.; Rochon, P.A.; Lipscombe, L.L. Levothyroxine dose and risk of fractures in older adults: Nested case-control study. BMJ 2011, 342, d2238. [Google Scholar] [CrossRef]
- Salgado-García, D.; Díaz-Álvarez, A.; González-Rodríguez, J.L.; López-Iglesias, M.R.; Sánchez-López, E.; Sánchez-Ledesma, M.J.; Martínez-Trufero, M.I. Comparison of the Analgesic Efficacy between Levobupivacaine 0.25% and Ropivacaine 0.375% for PENG (Pericapsular Nerve Group) Block in the Context of Hip Fracture Surgery of Elderly Patients: A Single-Center, Randomized, and Controlled Clinical Trial. J. Clin. Med. 2024, 13, 770. [Google Scholar] [CrossRef]
- Ojeda-Thies, C.; Sáez-López, P.; Currie, C.; Tarazona-Santalbina, F.; Alarcón, T.; Muñoz-Pascual, A.; Pareja, T.; Gómez-Campelo, P.; Montero-Fernández, N. Spanish National Hip Fracture Registry (RNFC): Analysis of its first annual report and international comparison with other established registries. Osteoporos. Int. 2019, 30, 1243–1254. [Google Scholar] [CrossRef]
- Azagra, R.; López-Expósito, F.; Martin-Sánchez, J.C.; Aguyé-Batista, A.; Gabriel-Escoda, P.; Zwart, M.; Diaz-Herrera, M.G.; Pujol-Salud, J.; Iglesias-Martinez, M.; Puchol-Ruiz, N. Incidencia de la fractura de fémur en España (1997–2010). Med. Clín. 2015, 145, 465–470. [Google Scholar] [CrossRef]
- Kanis, J.A.; Odén, A.; McCloskey, E.V.; Johansson, H.; Wahl, D.A.; Cooper, C.; on behalf of the IOF Working Group on Epidemiology and Quality of Life. A systematic review of hip fracture incidence and probability of fracture worldwide. Osteoporos. Int. 2012, 23, 2239–2256. [Google Scholar] [CrossRef]
- Cunha, A.I.L.; Veronese, N.; Borges, S.d.M.; Ricci, N.A. Frailty as a predictor of adverse outcomes in hospitalized older adults: A systematic review and meta-analysis. Ageing Res. Rev. 2019, 56, 100960. [Google Scholar] [CrossRef] [PubMed]
- Pilotto, A.; Custodero, C.; Maggi, S.; Polidori, M.C.; Veronese, N.; Ferrucci, L. A multidimensional approach to frailty in older people. Ageing Res. Rev. 2020, 60, 101047. [Google Scholar] [CrossRef] [PubMed]
- Rooke, G. Cardiovascular aging and anesthetic implications. J. Cardiothorac. Vasc. Anesth. 2003, 17, 512–523. [Google Scholar] [CrossRef]
- Groban, L. Diastolic dysfunction in the older heart. J. Cardiothorac. Vasc. Anesth. 2005, 19, 228–236. [Google Scholar] [CrossRef]
- White, S.M. A retrospective, observational, single-centre, cohort database analysis of the haemodynamic effects of low-dose spinal anaesthesia for hip fracture surgery. BJA Open 2024, 9, 100261. [Google Scholar] [CrossRef] [PubMed]
- Mounet, B.; Choquet, O.; Swisser, F.; Biboulet, P.; Bernard, N.; Bringuier, S.; Capdevila, X. Impact of multiple nerves blocks anaesthesia on intraoperative hypotension and mortality in hip fracture surgery intermediate-risk elderly patients: A propensity score-matched comparison with spinal and general anaesthesia. Anaesth. Crit. Care Pain Med. 2021, 40, 100924. [Google Scholar] [CrossRef]
- Gropper, M.A.; Eriksson, L.I.; Fleisher, L.A.; Wiener-Kronish, J.P.; Cohen, N.H.; Leslie, K. Miller’s Anesthesia, 9th ed.; Elsevier: Amsterdam, The Netherlands, 2019. [Google Scholar]
- White, S. Duration of low-dose subarachnoid anaesthesia for hip fracture surgery. Anaesthesia 2017, 72, 127–128. [Google Scholar] [CrossRef] [PubMed]
- Lemoine, A.; Mazoit, J.X.; Bonnet, F. Modelling of the optimal bupivacaine dose for spinal anaesthesia in ambulatory surgery based on data from systematic review. Eur. J. Anaesthesiol. 2016, 33, 846–852. [Google Scholar] [CrossRef] [PubMed]
- Valanne, J.V.; Korhonen, A.-M.; Jokela, R.M.; Ravaska, P.; Korttila, K.K. Selective Spinal Anesthesia: A Comparison of Hyperbaric Bupivacaine 4 mg Versus 6 mg for Outpatient Knee Arthroscopy. Anesth. Analg. 2001, 93, 1377–1379. [Google Scholar] [CrossRef]
- Jankowski, C.J.; Hebl, J.R.; Stuart, M.J.; Rock, M.G.; Pagnano, M.W.; Beighley, C.M.; Schroeder, D.R.; Horlocker, T.T. A Comparison of Psoas Compartment Block and Subarachnoid and General Anesthesia for Outpatient Knee Arthroscopy. Anesth. Analg. 2003, 97, 1003. [Google Scholar] [CrossRef]
- Minville, V.; Fourcade, O.; Grousset, D.; Chassery, C.; Nguyen, L.; Asehnoune, K.; Colombani, A.; Goulmamine, L.; Samii, K. Spinal Anesthesia Using Single Injection Small-Dose Bupivacaine Versus Continuous Catheter Injection Techniques for Surgical Repair of Hip Fracture in Elderly Patients. Anesth. Analg. 2006, 102, 1559–1563. [Google Scholar] [CrossRef]
- Olofsson, C.; Nygårds, E.; Bjersten, A.; Hessling, A. Low-dose bupivacaine with sufentanil prevents hypotension after spinal anesthesia for hip repair in elderly patients. Acta Anaesthesiol. Scand. 2004, 48, 1240–1244. [Google Scholar] [CrossRef]
- Martyr, J.W.; Stannard, K.J.D.; Gillespie, G. Subarachnoid-induced Hypotension in Elderly Patients with Hip Fracture. A Com-parison of Glucose-free Bupivacaine with Glucose-free Bupivacaine and Fentanyl. Anaesth. Intensive Care 2005, 33, 64–68. [Google Scholar] [CrossRef] [PubMed]
- Errando, C.; Soriano-Bru, J.; Peiró, C.; Úbeda, J. Single shot spinal anaesthesia with hypobaric bupivacaine for hip fracture repair surgery in the elderly. Randomized, double blinded comparison of 3.75mg vs. 7.5mg. Rev. Espanola Anestesiol. Reanim. 2014, 61, 541–548. [Google Scholar] [CrossRef]
- Ben-David, B.; Frankel, R.; Arzumonov, T.; Marchevsky, Y.; Volpin, G. Minidose Bupivacaine–Fentanyl Subarachnoid Anesthesia for Surgical Repair of Hip Fracture in the Aged. Anesthesiology 2000, 92, 6. [Google Scholar] [CrossRef]
- Kahloul, M.; Nakhli, M.S.; Chouchene, A.; Chebbi, N.; Mhamdi, S.; Naija, W. Comparison of two doses of hypobaric bupivacaine in unilateral spinal anesthesia for hip fracture surgery: 5 mg versus 7.5 mg. Pan Afr. Med. J. 2017, 28, 108. [Google Scholar] [CrossRef]
- Messina, A.; La Via, L.; Milani, A.; Savi, M.; Calabrò, L.; Sanfilippo, F.; Negri, K.; Castellani, G.; Cammarota, G.; Robba, C.; et al. Spinal anesthesia and hypotensive events in hip fracture surgical repair in elderly patients: A meta-analysis. J. Anesth. Analg. Crit. Care 2022, 2, 19. [Google Scholar] [CrossRef]
- Jeevendiran, A.; Suganya, S.; Sujatha, C.; Rajaraman, J.; Surya, R.S.; Asokan, A.; Radhakrishnan, A. Comparative Evaluation of Analgesic Efficacy of Ultrasound-Guided Pericapsular Nerve Group Block and Femoral Nerve Block During Positioning of Patients with Hip Fractures for Spinal Anesthesia: A Prospective, Double-Blind, Randomized Controlled Study. Cureus 2024, 16, e56270. [Google Scholar] [CrossRef]
- Erten, E.; Kara, U.; Şimşek, F.; Eşkin, M.B.; Bilekli, A.B.; Öcal, N.; Şenkal, S.; Ozdemirkan, I. Comparison of pericapsular nerve group block and femoral nerve block in spinal anesthesia position analgesia for proximal femoral fractures in geriatric patients: A randomized clinical trial. Turk. J. Trauma Emerg. Surg. 2023, 29, 1368–1375. [Google Scholar] [CrossRef] [PubMed]
- Aygun, H.; Tulgar, S.; Yigit, Y.; Tasdemir, A.; Kurt, C.; Genc, C.; Bilgin, S.; Senoğlu, N.; Koksal, E. Effect of ultrasound-guided pericapsular nerve group (PENG) block on pain during patient positioning for central nervous blockade in hip surgery: A randomized controlled trial. BMC Anesthesiol. 2023, 23, 316. [Google Scholar] [CrossRef] [PubMed]
- Sahnoun, N.; Keskes, M.; Mtibaa, M.A.; Abid, A.; Ketata, S.; Derbel, R.; Zouche, I.; Cheikhrouhou, H. Pericapsular nerve group block versus fascia iliaca block for perioperative analgesia in hip fracture surgery: A prospective randomized trial. Pan Afr. Med. J. 2023, 46, 93. [Google Scholar] [CrossRef] [PubMed]
- Chaudhary, K.; Bose, N.; Tanna, D.; Chandnani, A. Ultrasound-guided pericapsular nerve group (PENG) block versus femoral nerve block for positioning during spinal anaesthesia in proximal femur fractures: A randomised comparative study. Indian J. Anaesth. 2023, 67, 913–919. [Google Scholar] [CrossRef]
- Brady, K.; Hogue, C.W. Intraoperative Hypotension and Patient Outcome. Anesthesiology 2013, 119, 495–497. [Google Scholar] [CrossRef]
- Ke, J.; George, R.; Beattie, W. Making sense of the impact of intraoperative hypotension: From populations to the individual patient. Br. J. Anaesth. 2018, 121, 689–691. [Google Scholar] [CrossRef] [PubMed]
- White, S.M.; Griffiths, R. Problems defining ‘hypotension’ in hip fracture anaesthesia. Br. J. Anaesth. 2019, 123, e528–e529. [Google Scholar] [CrossRef] [PubMed]
- Grüne, F.; Klimek, M. Cerebral blood flow and its autoregulation—When will there be some light in the black box? Br. J. Anaesth. 2017, 119, 1077–1079. [Google Scholar] [CrossRef] [PubMed]
| Group B (n = 108) | Group S (n = 76) | p | |
|---|---|---|---|
| Age, years (median (IQR)) | 86.5 (16.0) | 90.0 (6) | p = 0.853 |
| Gender, n (%) | p = 0.401 | ||
| Male | 24 (22.22) | 21 (27.63) | |
| Female | 84 (77.78) | 55 (72.37) | |
| Duration of surgery, min (mean (SD)) | 52.63 (18.40) | 73.24 (26.12) | p = 0.000 |
| Type of fracture, n (%) | |||
| Subcapital | 38 (35.19) | 24 (31.58) | |
| Pertrochanteric | 67 (62.04) | 47 (61.84) | |
| Subpertrochanteric | 1 (0.95) | 4 (5.26) | |
| Others | 2 (1.85) | 2 (2.63) | |
| Type of surgery, n (%) | p = 0.919 | ||
| Partial Hip Arthroplasty | 38 (35.19) | 28 (36.84) | |
| Endomedullary Nailing | 69 (63.89) | 46 (60.53) | |
| Others | 1 (0.93) | 1 (1.32) |
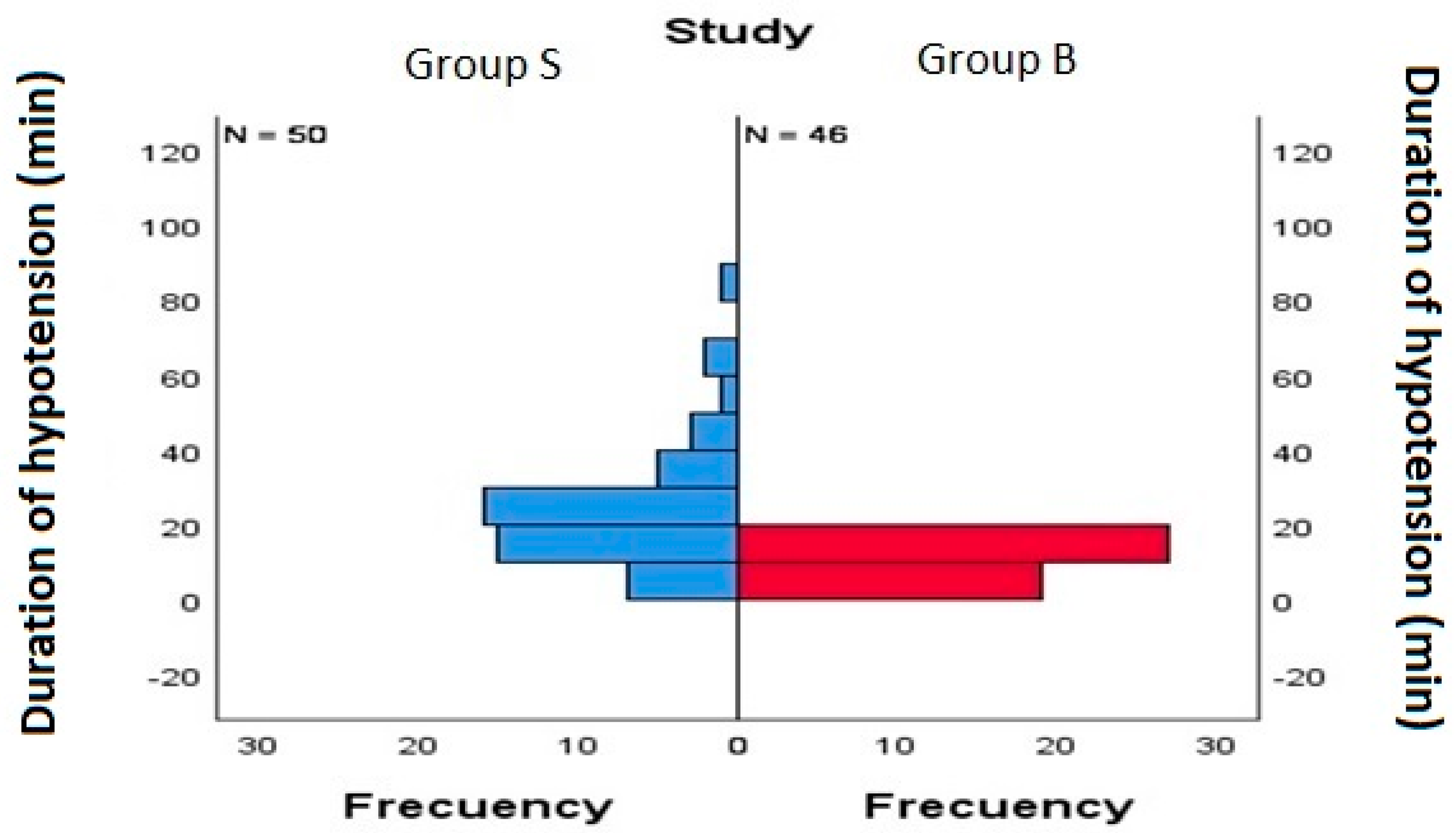
| Study Group | Median (IQR) | p | |
|---|---|---|---|
| Time of hypotension (min) | Group S | 20 (16) | 0.000 |
| Group B | 10 (5) | ||
| Episodes of hypotension (n) | Group S | 2 (1) | 0.000 |
| Group B | 4 (3.25) |
| Vasoconstrictor | Study Group | Median (IQR) | p |
|---|---|---|---|
| Efedrine (mg) | Group S | 12 (18) | 0.463 |
| Group B | 9 (5) | ||
| Fenilefrine (mg) | Group S | 0.25 (0.20) | 0.056 |
| Group B | 0.20 (0.23) |
| Study | Type of Study | Bupivacaine Dose Used | Need for Supplementary Analgesia |
|---|---|---|---|
| White | Retrospective | 6.5–7.5 mg 0.5%, hiper/isobaric | |
| Wood | Retrospective | 4–5 mg 0.5%, hiperbaric | Not stated |
| Minville | Prospective | 7.5 mg 0.5%, isobaric | |
| Olofson | Prospective | 7.5 mg 0.5%, isobaric | |
| Martyr | Prospective | 9 mg 0.5%, isobaric | |
| Errando | Prospective | 3.75 mg 0.25%, hypobaric | Ketamine and fentanyl, PO + IO |
| Ben-David | Prospective | 4 mg 0.5%, isobaric | Fentanyl, PO + IO |
| Kahloul | Prospective | 5 mg 0.5% hypobaric + IFB | 2 cases of insufficient SA |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Published by MDPI on behalf of the Lithuanian University of Health Sciences. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Salgado-García, D.; Díaz-Álvarez, A.; González-Rodríguez, J.L.; López-Iglesias, M.R.; Sánchez-López, E.; Sánchez-Ledesma, M.J.; Martínez-Trufero, M.I. Low-Dose Subarachnoid Anesthesia Combined with PENG and FLCN Blocks Reduces Hypotensive Episodes Without Compromising Anesthetic Depth and Duration in Hip Fracture Surgery: A Retrospective Observational Study. Medicina 2025, 61, 1808. https://doi.org/10.3390/medicina61101808
Salgado-García D, Díaz-Álvarez A, González-Rodríguez JL, López-Iglesias MR, Sánchez-López E, Sánchez-Ledesma MJ, Martínez-Trufero MI. Low-Dose Subarachnoid Anesthesia Combined with PENG and FLCN Blocks Reduces Hypotensive Episodes Without Compromising Anesthetic Depth and Duration in Hip Fracture Surgery: A Retrospective Observational Study. Medicina. 2025; 61(10):1808. https://doi.org/10.3390/medicina61101808
Chicago/Turabian StyleSalgado-García, Daniel, Agustín Díaz-Álvarez, José L. González-Rodríguez, María R. López-Iglesias, Eduardo Sánchez-López, Manuel J. Sánchez-Ledesma, and María I. Martínez-Trufero. 2025. "Low-Dose Subarachnoid Anesthesia Combined with PENG and FLCN Blocks Reduces Hypotensive Episodes Without Compromising Anesthetic Depth and Duration in Hip Fracture Surgery: A Retrospective Observational Study" Medicina 61, no. 10: 1808. https://doi.org/10.3390/medicina61101808
APA StyleSalgado-García, D., Díaz-Álvarez, A., González-Rodríguez, J. L., López-Iglesias, M. R., Sánchez-López, E., Sánchez-Ledesma, M. J., & Martínez-Trufero, M. I. (2025). Low-Dose Subarachnoid Anesthesia Combined with PENG and FLCN Blocks Reduces Hypotensive Episodes Without Compromising Anesthetic Depth and Duration in Hip Fracture Surgery: A Retrospective Observational Study. Medicina, 61(10), 1808. https://doi.org/10.3390/medicina61101808






