Tracheostomy Practice in the Italian Intensive Care Units: A Point-Prevalence Survey
Abstract
1. Introduction
2. Methods
2.1. Study Design
2.2. Participants
2.3. Data Collection
2.4. Definitions
2.5. Statistical Analysis
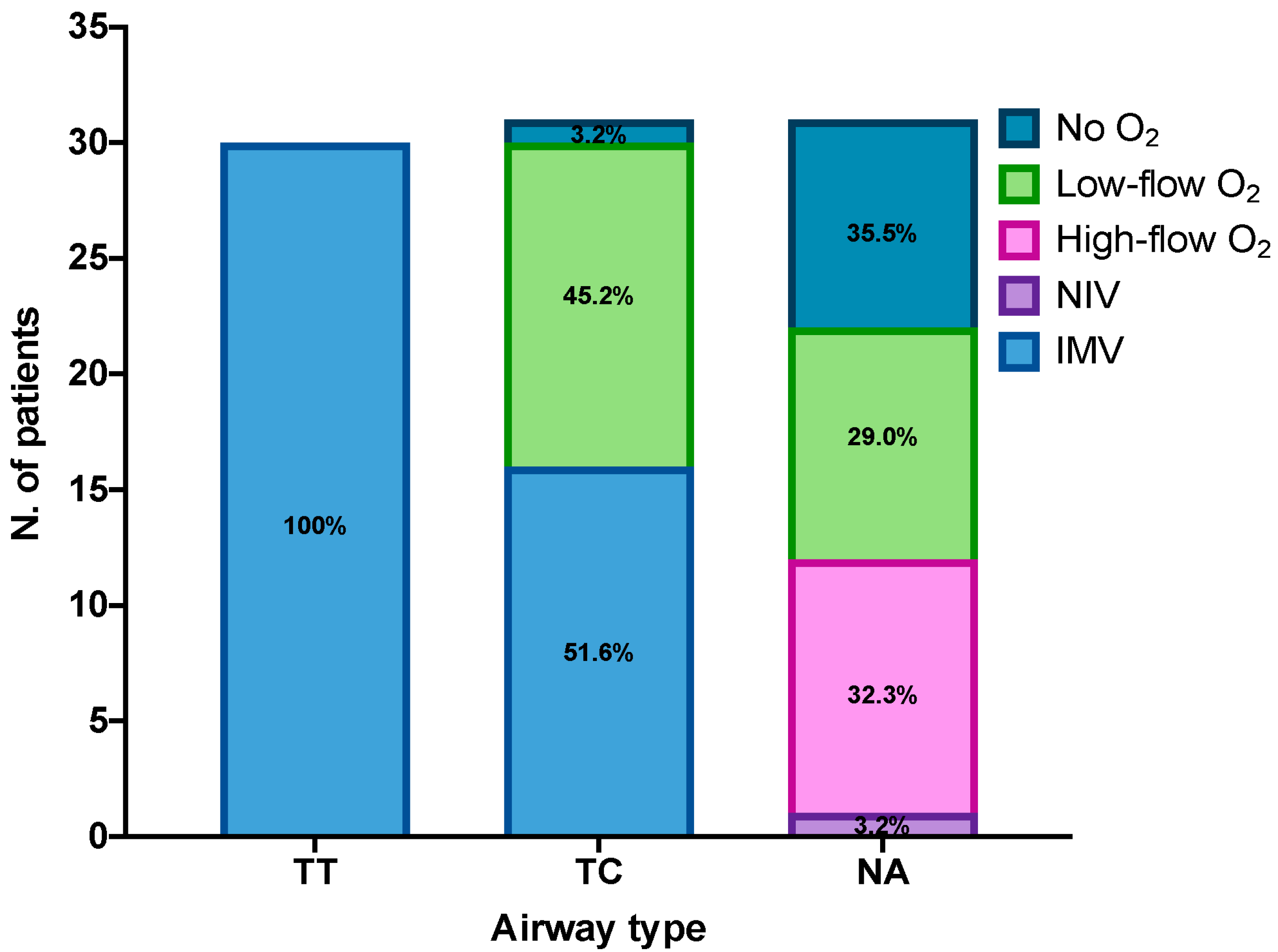
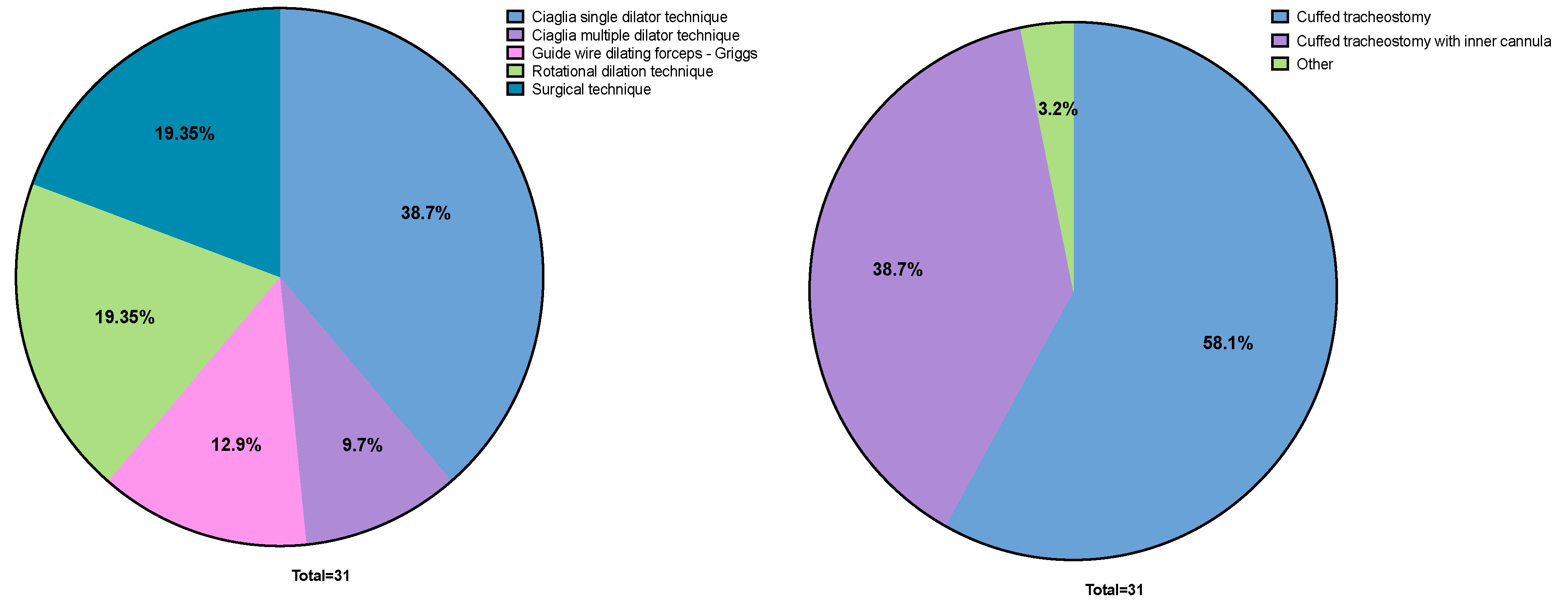
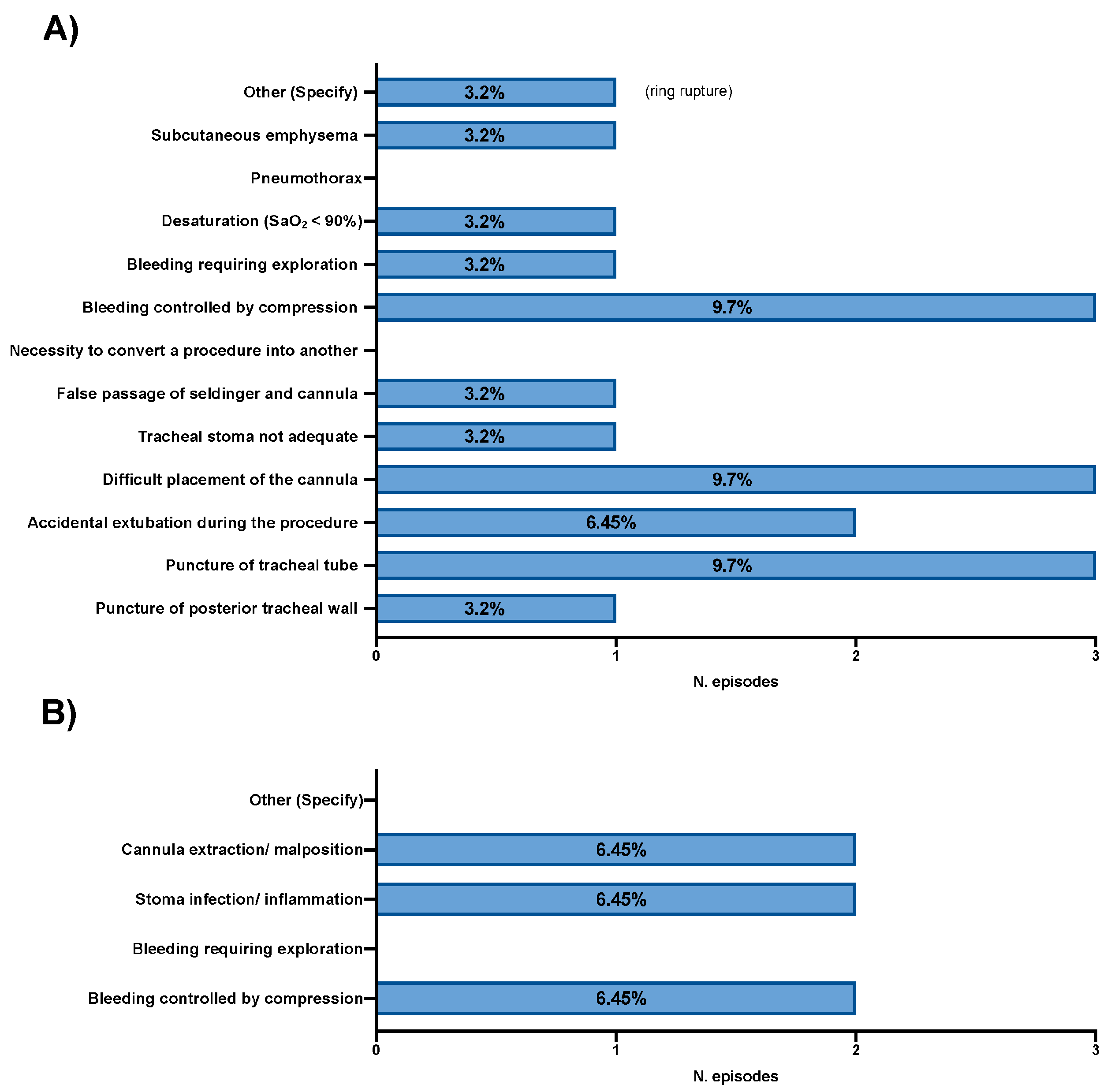
3. Results
3.1. Characteristics of Participating ICUs
3.2. Characteristics of Tracheostomized Patients
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Vargas, M.; Sutherasan, Y.; Antonelli, M.; Brunetti, I.; Corcione, A.; Laffey, J.G.; Putensen, C.; Servillo, G.; Pelosi, P. Tracheostomy procedures in the intensive care unit: An international survey. Crit. Care 2015, 19, 291. [Google Scholar] [CrossRef] [PubMed]
- Battaglini, D.; Premraj, L.; White, N.; Sutt, A.L.; Robba, C.; Cho, S.M.; Di Giacinto, I.; Bressan, F.; Sorbello, M.; Cuthbertson, B.H.; et al. Tracheostomy outcomes in critically ill patients with COVID-19: A systematic review, meta-analysis, and meta-regression. Br. J. Anaesth. 2022, 129, 679–692. [Google Scholar] [CrossRef] [PubMed]
- Piombino, P.; Troise, S.; Vargas, M.; Marra, A.; Buonanno, P.; Fusetti, S.; Apolloni, F.; Crimi, S.; Bianchi, A.; Mariniello, D.; et al. A systematic review of the literature on the role of tracheostomy in COVID-19 patients. Eur. Rev. Med. Pharmacol. Sci. 2020, 24, 12558–12574. [Google Scholar] [PubMed]
- Merola, R.; Iacovazzo, C.; Troise, S.; Marra, A.; Formichella, A.; Servillo, G.; Vargas, M. Timing of Tracheostomy in ICU Patients: A Systematic Review and Meta-Analysis of Randomized Controlled Trials. Life 2024, 14, 1165. [Google Scholar] [CrossRef]
- Battaglini, D.; Missale, F.; Schiavetti, I.; Filauro, M.; Iannuzzi, F.; Ascoli, A.; Bertazzoli, A.; Pascucci, F.; Grasso, S.; Murgolo, F.; et al. Tracheostomy Timing and Outcome in Severe COVID-19: The WeanTrach Multicenter Study. J. Clin. Med. 2021, 10, 2651. [Google Scholar] [CrossRef]
- Vargas, M.; Chiumello, D.; Sutherasan, Y.; Ball, L.; Esquinas, A.M.; Pelosi, P.; Servillo, G. Heat and moisture exchangers (HMEs) and heated humidifiers (HHs) in adult critically ill patients: A systematic review, meta-analysis and meta-regression of randomized controlled trials. Crit. Care 2017, 21, 123. [Google Scholar] [CrossRef]
- Nieszkowska, A.; Combes, A.; Luyt, C.E.; Ksibi, H.; Trouillet, J.L.; Gibert, C.; Chastre, J. Impact of tracheotomy on sedative administration, sedation level, and comfort of mechanically ventilated intensive care unit patients. Crit. Care Med. 2005, 33, 2527–2533. [Google Scholar] [CrossRef]
- Merola, R.; Troise, S.; Palumbo, D.; D’Auria, D.; Dell’Aversana Orabona, G.; Vargas, M. Airway management in patients undergoing maxillofacial surgery: State of art review. J. Stomatol. Oral Maxillofac. Surg. 2024, 126, 102044. [Google Scholar] [CrossRef]
- Abbate, V.; Committeri, U.; Troise, S.; Bonavolontà, P.; Vaira, L.A.; Gabriele, G.; Biglioli, F.; Tarabbia, F.; Califano, L.; Dell’Aversana Orabona, G. Virtual Surgical Reduction in Atrophic Edentulous Mandible Fractures: A Novel Approach Based on “in House” Digital Work-Flow. Appl. Sci. 2023, 13, 1474. [Google Scholar] [CrossRef]
- Merola, R.; Vargas, M.; Marra, A.; Buonanno, P.; Coviello, A.; Servillo, G.; Iacovazzo, C. Videolaryngoscopy versus Fiberoptic Bronchoscopy for Awake Tracheal Intubation: A Systematic Review and Meta-Analysis of Randomized Controlled Trials. J. Clin. Med. 2024, 13, 3186. [Google Scholar] [CrossRef]
- Merola, R.; Mancino, D.; Vargas, M. Videolaryngoscopy versus direct laryngoscopy: A bibliometric analysis. Br. J. Anaesth. 2024, 132, 166–168. [Google Scholar] [CrossRef] [PubMed]
- Diehl, J.L.; El Atrous, S.; Touchard, D.; Lemaire, F.; Brochard, L. Changes in the work of breathing induced by tracheotomy in ventilator-dependent patients. Am. J. Respir. Crit. Care Med. 1999, 159, 383–388. [Google Scholar] [CrossRef] [PubMed]
- Vargas, M.; Battaglini, D.; Antonelli, M.; Corso, R.; Frova, G.; Merli, G.; Petrini, F.; Ranieri, M.V.; Sorbello, M.; Di Giacinto, I.; et al. Follow-up short and long-term mortalities of tracheostomized critically ill patients in an Italian multi-center observational study. Sci. Rep. 2024, 14, 2319. [Google Scholar] [CrossRef] [PubMed]
- Epstein, S.K. Late complications of tracheostomy. Respir. Care 2005, 50, 542–549. [Google Scholar]
- Wang, F.; Wu, Y.; Bo, L.; Lou, J.; Zhu, J.; Chen, F.; Li, J.; Deng, X. The timing of tracheotomy in critically ill patients undergoing mechanical ventilation: A systematic review and meta-analysis of randomized controlled trials. Chest 2011, 140, 1456–1465. [Google Scholar] [CrossRef]
- Vargas, M.; Pelosi, P.; Servillo, G. Percutaneous tracheostomy: It’s time for a shared approach! Crit. Care 2014, 18, 448. [Google Scholar] [CrossRef]
- Miles, B.A.; Schiff, B.; Ganly, I.; Ow, T.; Cohen, E.; Genden, E.; Culliney, B.; Mehrotra, B.; Savona, S.; Wong, R.J.; et al. Tracheostomy during SARS-CoV-2 pandemic: Recommendations from the New York Head and Neck Society. Head Neck 2020, 42, 1282–1290. [Google Scholar] [CrossRef]
- Zimmerman, F.S.; Shaul, C.; Helviz, Y.; Levin, P.D. The Effect of Delay Following the Clinical Decision to Perform Tracheostomy in the Critical Care Setting. Respir. Care 2024, 69, 463–469. [Google Scholar] [CrossRef]
- Esteban, A.; Anzueto, A.; Alía, I.; Gordo, F.; Apezteguía, C.; Pálizas, F.; Cide, D.; Goldwaser, R.; Soto, L.; Bugedo, G.; et al. How is mechanical ventilation employed in the intensive care unit? An international utilization review. Am. J. Respir. Crit. Care Med. 2000, 161, 1450–1458. [Google Scholar] [CrossRef]
- Mehta, A.B.; Syeda, S.N.; Bajpayee, L.; Cooke, C.R.; Walkey, A.J.; Wiener, R.S. Trends in Tracheostomy for Mechanically Ventilated Patients in the United States, 1993–2012. Am. J. Respir. Crit. Care Med. 2015, 192, 446–454. [Google Scholar] [CrossRef]
- Abe, T.; Madotto, F.; Pham, T.; Nagata, I.; Uchida, M.; Tamiya, N.; Kurahashi, K.; Bellani, G.; Laffey, J.G.; LUNG-SAFE Investigators and the ESICM Trials Group. Epidemiology and patterns of tracheostomy practice in patients with acute respiratory distress syndrome in ICUs across 50 countries. Crit. Care 2018, 22, 195. [Google Scholar] [CrossRef] [PubMed]
- Bösel, J.; Niesen, W.D.; Salih, F.; Morris, N.A.; Ragland, J.T.; Gough, B.; Schneider, H.; Neumann, J.O.; Hwang, D.Y.; Kantamneni, P.; et al. Effect of Early vs Standard Approach to Tracheostomy on Functional Outcome at 6 Months Among Patients With Severe Stroke Receiving Mechanical Ventilation: The SETPOINT2 Randomized Clinical Trial. JAMA 2022, 327, 1899–1909. [Google Scholar] [CrossRef] [PubMed]
- Robba, C.; Galimberti, S.; Graziano, F.; Wiegers, E.J.A.; Lingsma, H.F.; Iaquaniello, C.; Stocchetti, N.; Menon, D.; Citerio, G.; CENTER-TBI ICU Participants and Investigators. Tracheostomy practice and timing in traumatic brain-injured patients: A CENTER-TBI study. Intensive Care Med. 2020, 46, 983–994. [Google Scholar] [CrossRef] [PubMed]
- Premraj, L.; Camarda, C.; White, N.; Godoy, D.A.; Cuthbertson, B.H.; Rocco, P.R.M.; Pelosi, P.; Robba, C.; Suarez, J.I.; Cho, S.M.; et al. Tracheostomy timing and outcome in critically ill patients with stroke: A meta-analysis and meta-regression. Crit. Care 2023, 27, 132. [Google Scholar] [CrossRef]
- Camarda, C.; Premraj, L.; Pelosi, P.; Cho, S.M.; Battaglini, D. The stroke care puzzle: Does tracheostomy timing fit? Crit. Care 2023, 27, 216. [Google Scholar] [CrossRef]
- Terragni, P.P.; Antonelli, M.; Fumagalli, R.; Faggiano, C.; Berardino, M.; Pallavicini, F.B.; Miletto, A.; Mangione, S.; Sinardi, A.U.; Pastorelli, M.; et al. Early vs. late tracheotomy for prevention of pneumonia in mechanically ventilated adult ICU patients: A randomized controlled trial. JAMA 2010, 303, 1483–1489. [Google Scholar] [CrossRef]
- Szakmany, T.; Russell, P.; Wilkes, A.R.; Hall, J.E. Effect of early tracheostomy on resource utilization and clinical outcomes in critically ill patients: Meta-analysis of randomized controlled trials. Br. J. Anaesth. 2015, 114, 396–405. [Google Scholar] [CrossRef]
- Chorath, K.; Hoang, A.; Rajasekaran, K.; Moreira, A. Association of Early vs Late Tracheostomy Placement with Pneumonia and Ventilator Days in Critically Ill Patients: A Meta-analysis. JAMA Otolaryngol. Head Neck Surg. 2021, 147, 450–459. [Google Scholar] [CrossRef]
- Kost, K.M. Percutaneous tracheostomy: Comparison of Ciaglia and Griggs techniques. Crit. Care 2000, 4, 143–146. [Google Scholar] [CrossRef][Green Version]
- Byhahn, C.; Westphal, K.; Meininger, D.; Gürke, B.; Kessler, P.; Lischke, V. Single-dilator percutaneous tracheostomy: A comparison of PercuTwist and Ciaglia Blue Rhino techniques. Intensive Care Med. 2002, 28, 1262–1266. [Google Scholar] [CrossRef]
- Lee, S.A.; Kim, J.S.; Ji, M.; Kim, D.K.; Moon, H.J.; Lee, W.S. Optimal methodology for percutaneous dilatational tracheostomy: A comparative analysis between conventional and multidisciplinary approaches utilizing ultrasound, flexible bronchoscopy, and microcatheter puncture in critically ill individuals of diminutive stature-a longitudinal single-institutional experience and retrospective analysis. J. Thorac. Dis. 2024, 16, 3668–3684. [Google Scholar] [PubMed]
- Schneider, H.; Meis, J.; Klose, C.; Ratzka, P.; Niesen, W.D.; Seder, D.B.; Bösel, J.; SETPOINT2 and IGNITE study groups. Surgical Versus Dilational Tracheostomy in Patients with Severe Stroke: A SETPOINT2 Post hoc Analysis. Neurocrit. Care 2024, 41, 146–155. [Google Scholar] [CrossRef] [PubMed]
- Merola, R.; Vargas, M. Economic Indicators, Quantity and Quality of Health Care Resources Affecting Post-surgical Mortality. J. Epidemiol. Glob. Health 2024, 14, 613–620. [Google Scholar] [CrossRef] [PubMed]
- Murray, M.; Shen, C.; Massey, B.; Stadler, M.; Zenga, J. Retrospective analysis of post-tracheostomy complications. Am. J. Otolaryngol. 2022, 43, 103350. [Google Scholar] [CrossRef]
- Noy, R.; Shkedy, Y.; Simchon, O.; Gvozdev, N.; Roimi, M.; Miller, A.; Epstein, D. Impact of radiological surveillance for major blood vessels on complications of percutaneous dilatational tracheostomy: A retrospective cohort study. Am. J. Otolaryngol. 2024, 45, 104146. [Google Scholar] [CrossRef]
- Roy, C.F.; Silver, J.A.; Turkdogan, S.; Siafa, L.; Correa, J.A.; Kost, K. Complication Rate of Percutaneous Dilatational Tracheostomy in Critically Ill Adults with Obesity: A Systematic Review and Meta-analysis. JAMA Otolaryngol. Head Neck Surg. 2023, 149, 334–343. [Google Scholar] [CrossRef]
| ICU ID | Country | Type of Hospital | ICU Type | Maximum Number of ICU Beds | Approximate Number of Admitted Patients/Year | Number of Tracheostomies Performed in 2022 |
|---|---|---|---|---|---|---|
| 1 | Italy | Academic | Mixed | 20 | 301–600 | 42 |
| 2 | Italy | Academic | Mixed | 14 | 301–600 | 58 |
| 3 | Italy | Academic | Surgical | 8 | 301–600 | 22 |
| 4 | Italy | Academic | Mixed | 8 | 301–600 | 18 |
| 5 | Italy | Tertiary | Surgical, Medical | 13 | 601–999 | 68 |
| 6 | Italy | Academic | Mixed, Surgical, Medical, Neurological | 28 | 601–999 | 75 |
| 7 | Italy | Academic | Medical | 16 | 601–999 | 120 |
| 8 | Italy | Academic | Surgical, Medical | 16 | ≥1000 | 72 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Published by MDPI on behalf of the Lithuanian University of Health Sciences. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Merola, R.; Vargas, M.; Sanfilippo, F.; Vergano, M.; Mistraletti, G.; Vetrugno, L.; De Pascale, G.; Bignami, E.G.; Servillo, G.; Battaglini, D. Tracheostomy Practice in the Italian Intensive Care Units: A Point-Prevalence Survey. Medicina 2025, 61, 87. https://doi.org/10.3390/medicina61010087
Merola R, Vargas M, Sanfilippo F, Vergano M, Mistraletti G, Vetrugno L, De Pascale G, Bignami EG, Servillo G, Battaglini D. Tracheostomy Practice in the Italian Intensive Care Units: A Point-Prevalence Survey. Medicina. 2025; 61(1):87. https://doi.org/10.3390/medicina61010087
Chicago/Turabian StyleMerola, Raffaele, Maria Vargas, Filippo Sanfilippo, Marco Vergano, Giovanni Mistraletti, Luigi Vetrugno, Gennaro De Pascale, Elena Giovanna Bignami, Giuseppe Servillo, and Denise Battaglini. 2025. "Tracheostomy Practice in the Italian Intensive Care Units: A Point-Prevalence Survey" Medicina 61, no. 1: 87. https://doi.org/10.3390/medicina61010087
APA StyleMerola, R., Vargas, M., Sanfilippo, F., Vergano, M., Mistraletti, G., Vetrugno, L., De Pascale, G., Bignami, E. G., Servillo, G., & Battaglini, D. (2025). Tracheostomy Practice in the Italian Intensive Care Units: A Point-Prevalence Survey. Medicina, 61(1), 87. https://doi.org/10.3390/medicina61010087











