A 10-Year Risk Assessment and Primary Prevention Study of Atherosclerotic Cardiovascular Disease Among Adult Patients in Saudi Arabia: A Cross-Sectional Study
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design and Population
2.2. Ethical Considerations
2.3. Statistical Analysis
3. Results
3.1. Participant Characteristics
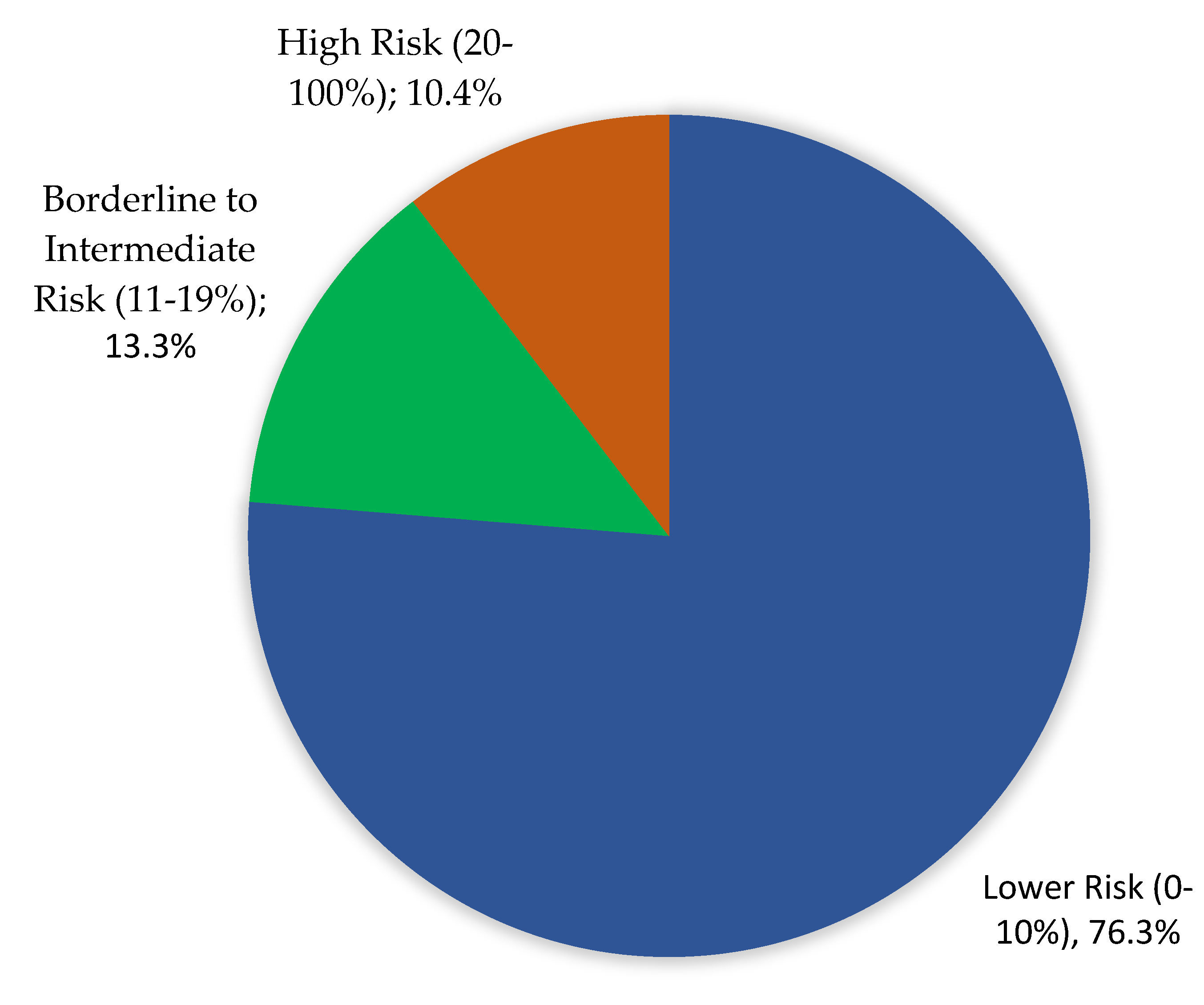
3.2. ASCVD Risk Distribution
3.3. Predictors of High ASCVD Risk
3.4. Aspirin and Statin Use
4. Discussion
4.1. Clinical Implications
4.2. Study Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- World Health Organization. News-Room, Fact Sheet, Cardiovascular-Diseases-(Cvds). June 2021. Available online: https://www.who.int/news-room/fact-sheets/detail/cardiovascular-diseases-(cvds) (accessed on 11 June 2021).
- Manla, Y.; Almahmeed, W. The Pandemic of Coronary Heart Disease in the Middle East and North Africa: What Clinicians Need to Know. Curr. Atheroscler. Rep. 2023, 25, 543–557. [Google Scholar] [CrossRef] [PubMed]
- Public Health Authority. The Burden of Disease in Saudi Arabia 2022. Available online: https://www.pha.gov.sa/ar-sa/OpenData/Pages/default.aspx (accessed on 11 August 2024).
- Khambhati, J.; Allard-Ratick, M.; Dhindsa, D.; Lee, S.; Chen, J.; Sandesara, P.B.; O’Neal, W.; Quyyumi, A.A.; Wong, N.D.; Blumenthal, R.S.; et al. The art of cardiovascular risk assessment. Clin. Cardiol. 2018, 41, 677–684, Erratum in Clin. Cardiol. 2018, 41, 1111. [Google Scholar] [CrossRef] [PubMed]
- Agarwala, A.; Liu, J.; Ballantyne, C.M.; Virani, S.S. The Use of Risk Enhancing Factors to Personalize ASCVD Risk Assessment: Evidence and Recommendations from the 2018 AHA/ACC Multi-society Cholesterol Guidelines. Curr. Cardiovasc. Risk Rep. 2019, 13, 18. [Google Scholar] [CrossRef] [PubMed]
- Grundy, S.M.; Stone, N.J.; Bailey, A.L.; Beam, C.; Birtcher, K.K.; Blumenthal, R.S. 2018 AHA/ACC/AACVPR/AAPA/ABC/ACPM/ADA/AGS/APhA/ASPC/NLA/PCNA Guideline on the Management of Blood Cholesterol: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. Circulation 2019, 139, e1082–e1143. Available online: https://www.ahajournals.org/doi/10.1161/CIR.0000000000000625 (accessed on 2 November 2024). [PubMed]
- Kannan, R.; Kiran, P.R.; Gnanaselvam, N.A.; Mathew, K.G.; Johnson, J.C. “Healthy Heart, Healthy You”: Ten-Year Cardiovascular Disease (CVD) Risk among Adults in Anekal Taluk Hospital, Bangalore Urban District, Karnataka. Indian J. Community Med. 2022, 47, 429–432. [Google Scholar] [CrossRef]
- Hassan, K.; Mohydin, B.; Fawwad, A.; Waris, N.; Iqbal, S.; Jawaid, M. Predicting the risk of atherosclerotic cardiovascular disease (ASCVD) in Pakistani population. Clin. Epidemiol. Glob. Health 2019, 7, 184–187. [Google Scholar] [CrossRef]
- Zibaeenejad, F.; Mohammadi, S.S.; Sayadi, M.; Safari, F.; Zibaeenezhad, M.J. Ten-year atherosclerosis cardiovascular disease (ASCVD) risk score and its components among an Iranian population: A cohort-based cross-sectional study. BMC Cardiovasc. Disord. 2022, 22, 162. [Google Scholar] [CrossRef]
- Hazazi, A.; Wilson, A. Noncommunicable diseases and health system responses in Saudi Arabia: Focus on policies and strategies. A qualitative study. Health Res. Policy Sys. 2022, 20, 63. [Google Scholar] [CrossRef]
- AlQuaiz, A.M.; Kazi, A.; Alodhayani, A.A.; Almeneessier, A.; AlHabeeb, K.M.; Siddiqui, A.R. Age and gender differences in the prevalence of chronic diseases and atherosclerotic cardiovascular disease risk scores in adults in Riyadh city, Saudi Arabia. Saudi Med. J. 2021, 42, 526–536. [Google Scholar] [CrossRef]
- Saeed, A.B.; Abaalkhail, B.A.; Ismail, I.; Saeed, A.; Al-Khammash, S. Estimate a patient’s 10 years cardiovascular risk using the Arteriosclerotic cardiovascular disease tool in a cross-sectional study in Al-Harja, Asser, Saudi Arabia, 2021. J. Fam. Med. Prim. Care. 2023, 12, 1106–1112. [Google Scholar] [CrossRef]
- Almulhim, M.; Alqattan, J.; Almajed, A.; Alkhars, M.A.; Alhafith, A.A.; Alajmi, M.S.; Alhussain, R.; Ali, S.; Elsheikh, E.; Al Sahlawi, M. Prediction of the 10-Year Risk of Cardiovascular Diseases Among Patients in Primary Health Care Centers in Eastern Province, Saudi Arabia. Cureus 2023, 15, e47551. [Google Scholar] [CrossRef] [PubMed]
- Qasem Surrati, A.M.; Mohammedsaeed, W.; Shikieri, A.B.E. Cardiovascular Risk Awareness and Calculated 10-Year Risk Among Female Employees at Taibah University 2019. Front. Public Health 2021, 9, 658243. [Google Scholar] [CrossRef] [PubMed]
- Tutor, A.W.; Lavie, C.J.; Kachur, S.; Milani, R.V.; Ventura, H.O. Updates on obesity and the obesity paradox in cardiovascular diseases. Prog. Cardiovasc. Dis. 2023, 78, 2–10. [Google Scholar] [CrossRef] [PubMed]
- Nakhaie, M.R.; Koor, B.E.; Salehi, S.O.; Karimpour, F. Prediction of cardiovascular disease risk using framingham risk score among office workers, Iran, 2017. Saudi J. Kidney Dis. Transpl. 2018, 29, 608–614. [Google Scholar] [CrossRef]
- Alhabib, K.F.; Batais, M.A.; Almigbal, T.H.; Alshamiri, M.Q.; Altaradi, H.; Rangarajan, S.; Yusuf, S. Demographic, behavioral, and cardiovascular disease risk factors in the Saudi population: Results from the Prospective Urban Rural Epidemiology study (PURE-Saudi). BMC Public Health 2020, 20, 1213. [Google Scholar] [CrossRef]
- Fahs, I.; Khalife, Z.; Malaeb, D.; Iskandarani, M.; Salameh, P. The Prevalence and Awareness of Cardiovascular Diseases Risk Factors among the Lebanese Population: A Prospective Study Comparing Urban to Rural Populations. Cardiol. Res. Pract. 2017, 2017, 3530902. [Google Scholar] [CrossRef]
- Al-Nooh, A.A.; Abdulabbas Abdulla Alajmi, A.; Wood, D. The Prevalence of Cardiovascular Disease Risk Factors among Employees in the Kingdom of Bahrain between October 2010 and March 2011: A Cross-Sectional Study from a Workplace Health Campaign. Cardiol. Res. Pract. 2014, 2014, 832421. [Google Scholar] [CrossRef][Green Version]
- Visseren, F.L.; Mach, F.; Smulders, Y.M.; Carballo, D.; Koskinas, K.C.; Bäck, M.; Benetos, A.; Biffi, A.; Boavida, J.M.; Capodanno, D.; et al. 2021 ESC Guidelines on cardiovascular disease prevention in clinical practice. Eur. Heart J. 2021, 42, 3227–3337. [Google Scholar] [CrossRef]
- Khan, S.U.; Lone, A.N.; Kleiman, N.S.; Arshad, A.; Jain, V.; Al Rifai, M.; Arshad, H.B.; Dani, S.S.; Khera, A.; Morris, P.B.; et al. Aspirin with or without Statin in Individuals Without Atherosclerotic Cardiovascular Disease Across Risk Categories. JACC Adv. 2023, 2, 100197. [Google Scholar] [CrossRef]
- Taylor, F.; Ward, K.; Moore, T.H.; Burke, M.; Davey Smith, G.; Casas, J.P.; Ebrahim, S. Statins for the primary prevention of cardiovascular disease. Cochrane Database Syst. Rev. 2011, 1, CD004816, Erratum in Cochrane Database Syst. Rev. 2013, 1, CD004816. [Google Scholar] [CrossRef]
- McNeil, J.J.; Woods, R.L.; Nelson, M.R.; Reid, C.M.; Kirpach, B.; Wolfe, R.; Storey, E.; Shah, R.C.; Lockery, J.E.; Tonkin, A.M.; et al. Effect of Aspirin on Disability-free Survival in the Healthy Elderly. N. Engl. J. Med. 2018, 379, 1499–1508. [Google Scholar] [CrossRef] [PubMed]
- McNeil, J.J.; Wolfe, R.; Woods, R.L.; Tonkin, A.M.; Donnan, G.A.; Nelson, M.R.; Reid, C.M.; Lockery, J.E.; Kirpach, B.; Storey, E. Effect of Aspirin on Cardiovascular Events and Bleeding in the Healthy Elderly. N. Engl. J. Med. 2018, 379, 1509–1518. [Google Scholar] [CrossRef] [PubMed]
- McNeil, J.J.; Nelson, M.R.; Woods, R.L.; Lockery, J.E.; Wolfe, R.; Reid, C.M.; Kirpach, B.; Shah, R.C.; Ives, D.G.; Storey, E.; et al. Effect of Aspirin on All-Cause Mortality in the Healthy Elderly. N. Engl. J. Med. 2018, 379, 1519–1528. [Google Scholar] [CrossRef] [PubMed]
- Gaziano, J.M.; Brotons, C.; Coppolecchia, R.; Cricelli, C.; Darius, H.; Gorelick, P.B.; Howard, G.; Pearson, T.A.; Rothwell, P.M.; Ruilope, L.M.; et al. Use of aspirin to reduce risk of initial vascular events in patients at moderate risk of cardiovascular disease (ARRIVE): A randomised, double-blind, placebo-controlled trial. Lancet 2018, 392, 1036–1046. [Google Scholar] [CrossRef]
- Bowman, L.; Mafham, M.; Wallendszus, K.; Stevens, W.; Buck, G.; Barton, J. Effects of Aspirin for Primary Prevention in Persons with Diabetes Mellitus. N. Engl. J. Med. 2018, 379, 1529–1539. [Google Scholar] [CrossRef]
- Shah, R.; Khan, B.; Latham, S.B.; Khan, S.A.; Rao, S.V. A Meta-Analysis of Aspirin for the Primary Prevention of Cardiovascular Diseases in the Context of Contemporary Preventive Strategies. Am J. Med. 2019, 132, 1295–1304.e3. [Google Scholar] [CrossRef]

| Variables (Mean ± SD *) | Categories | Frequency | Percentage |
|---|---|---|---|
| Zone | Middle | 16,545 | 28.2 |
| Northern | 15,179 | 25.8 | |
| Eastern | 16,982 | 28.9 | |
| Southern | 8711 | 14.8 | |
| NA | 1326 | 2.3 | |
| Age (50.98 ± 10.034) | 35–39 Years | 7971 | 13.6 |
| 40–45 Years | 12,781 | 21.8 | |
| 46–50 Years | 9765 | 16.6 | |
| 51–55 Years | 8703 | 14.8 | |
| 56–60 Years | 7592 | 12.9 | |
| 61–65 Years | 6585 | 11.2 | |
| 66–70 Years | 3464 | 5.9 | |
| 71–75 Years | 1883 | 3.2 | |
| Sex | Male | 22,428 | 38.2 |
| Female | 36,315 | 61.8 | |
| Smoking | Yes | 7138 | 12.1 |
| No | 51,624 | 87.9 | |
| Diabetic | Yes | 23,282 | 39.6 |
| No | 35,480 | 60.4 | |
| Hypertensive | Yes | 23,962 | 40.8 |
| No | 34,800 | 59.2 | |
| Using Aspirin | Yes | 4822 | 8.2 |
| No | 53,940 | 91.8 | |
| Taking Statin | Yes | 14,455 | 24.6 |
| No | 44,307 | 75.4 |
| Factors | ASCVD—Risk in Percentage | p-Value | |||||
|---|---|---|---|---|---|---|---|
| Low-Risk | Borderline-to-Intermediate Risk | High Risk | |||||
| No | % | No | % | No | % | ||
| Age in Years | 0.001 * | ||||||
| 35–39 | 7914 | 99.3% | 46 | 0.6% | 11 | 0.1% | |
| 40–45 | 12,469 | 97.6% | 261 | 2.0% | 50 | 0.4% | |
| 46–50 | 9169 | 93.9% | 487 | 5.0% | 109 | 1.1% | |
| 51–55 | 7444 | 85.5% | 994 | 11.4% | 265 | 3.0% | |
| 56–60 | 5054 | 66.6% | 1839 | 24.2% | 699 | 9.2% | |
| 61–65 | 2414 | 36.7% | 2640 | 40.1% | 1531 | 23.2% | |
| 66–70 | 334 | 9.6% | 1319 | 38.1% | 1811 | 52.3% | |
| 71–75 | 31 | 1.6% | 233 | 12.4% | 1619 | 86.0% | |
| Sex | 0.001 * | ||||||
| Male | 13,687 | 61.0% | 4483 | 20.0% | 4258 | 19.0% | |
| Female | 31,142 | 85.8% | 3336 | 9.2% | 1837 | 5.1% | |
| Smoking | 0.001 * | ||||||
| Yes | 3518 | 49.3% | 1808 | 25.3% | 1811 | 25.4% | |
| No | 41,311 | 80.1% | 6011 | 11.6% | 4284 | 8.3% | |
| Diabetes mellitus | 0.001 * | ||||||
| Yes | 11,926 | 51.2% | 5774 | 24.8% | 5574 | 23.9% | |
| No | 32,903 | 92.8% | 2045 | 5.8% | 521 | 1.5% | |
| Cholesterol Level | 0.043 * | ||||||
| 0.00–200.00—Desirable | 29,374 | 75.8% | 5138 | 13.3% | 4223 | 10.9% | |
| 200.01–239.00 Borderline | 11,629 | 79.1% | 1835 | 12.5% | 1235 | 8.4% | |
| 239.01–500—High | 3826 | 72.1% | 846 | 15.9% | 637 | 12.0% | |
| HDL Level | 0.001 * | ||||||
| ≤40—Low | 7853 | 62.5% | 2417 | 19.2% | 2287 | 18.2% | |
| 41–59 Average | 25,097 | 77.3% | 4283 | 13.2% | 3098 | 9.5% | |
| ≥60 High | 11,879 | 86.7% | 1119 | 8.2% | 710 | 5.2% | |
| Blood Pressure | 0.001 * | ||||||
| Normal Blood Pressure (≤120) | 21,102 | 89.9% | 1645 | 7.0% | 727 | 3.1% | |
| Elevated (121–129) | 8800 | 81.0% | 1294 | 11.9% | 776 | 7.1% | |
| Hypertension Stage 1 (130–139) | 7798 | 71.0% | 1911 | 17.4% | 1272 | 11.6% | |
| Hypertension Stage 2 (≥140) | 7129 | 53.1% | 2969 | 22.1% | 3320 | 24.7% | |
| Zone | 0.047 * | ||||||
| Middle | 12,302 | 74.4% | 2370 | 14.3% | 1873 | 11.3% | |
| Northern | 11,994 | 79.0% | 1796 | 11.8% | 1389 | 9.2% | |
| Eastern | 12,871 | 75.8% | 2310 | 13.6% | 1801 | 10.6% | |
| Southern | 6559 | 75.3% | 1218 | 14.0% | 934 | 10.7% | |
| Risk Factors | B | S.E. | p-Value | ORA | 95% CI | |
|---|---|---|---|---|---|---|
| LL | UL | |||||
| HDL (high level) | −0.045 | 0.044 | 0.005 * | 0.97 | 0.85 | 0.99 |
| Smoking | 3.559 | 0.068 | 0.001 * | 35.1 | 33.2 | 39.4 |
| Hypertension | 1.514 | 0.046 | 0.001 * | 4.54 | 3.7 | 5.1 |
| Diabetes Mellitus | 2.927 | 0.053 | 0.001 * | 18.7 | 16.8 | 20.4 |
| Age in years | 0.26 | 0.002 | 0.001 * | 1.29 | 1.28 | 1.31 |
| Male gender | 3.478 | 0.057 | 0.006 * | 3.58 | 2.7 | 5.9 |
| Medications | ASCVD 10-Year Risk | Total | p Value | |||
|---|---|---|---|---|---|---|
| Lower Risk | Borderline-to-Intermediate Risk | High Risk | ||||
| ASA | 0.001 * | |||||
| Yes | No | 1516 | 1496 | 1809 | 4821 | |
| % within ASCVD—Risk | 3.4% | 19.1% | 29.7% | 8.2% | ||
| No | No | 43,313 | 6323 | 4286 | 53,922 | |
| % within ASCVD—Risk | 96.6% | 80.9% | 70.3% | 91.8% | ||
| Statin | 0.001 * | |||||
| Yes | No | 7045 | 3850 | 3555 | 14,450 | |
| % within ASCVD—Risk | 15.7% | 49.2% | 58.3% | 24.6% | ||
| No | No | 37,784 | 3969 | 2540 | 44,293 | |
| % within ASCVD—Risk | 84.3% | 50.8% | 41.7% | 75.4% | ||
| Zone | Statin | Total | ASCVD—Risk in Percentage | p-Value | |||||
|---|---|---|---|---|---|---|---|---|---|
| Lower Risk | Borderline-to-Intermediate Risk | High Risk | |||||||
| No | % | No | % | No | % | ||||
| Middle | Yes | 4347 (26.3%) | 2000 | 16.3% | 1229 | 51.9% | 1118 | 59.7% | 0.001 * |
| No | 12,198 (73.7%) | 10,302 | 83.7% | 1141 | 48.1% | 755 | 40.3% | ||
| Northern | Yes | 3369 (22.2%) | 1762 | 14.7% | 840 | 46.8% | 767 | 55.2% | 0.001 * |
| No | 11,810 (77.8%) | 10,232 | 85.3% | 956 | 53.2% | 622 | 44.8% | ||
| Eastern | Yes | 4542 (26.7%) | 2211 | 17.2% | 1182 | 51.2% | 1149 | 63.8% | 0.001 * |
| No | 12,440 (73.3%) | 10,660 | 82.8% | 1128 | 48.8% | 652 | 36.2% | ||
| Southern | Yes | 1944 (22.3%) | 935 | 14.3% | 538 | 44.2% | 471 | 50.4% | 0.001 * |
| No | 6767 (77.7%) | 5624 | 85.7% | 680 | 55.8% | 463 | 49.6% | ||
| NA | Yes | 248 (18.7%) | 137 | 12.4% | 61 | 48.8% | 50 | 51.0% | 0.001 * |
| No | 1087 (81.3%) | 966 | 87.6% | 64 | 51.2% | 48 | 49.0% | ||
| Zone | ASA | Total | ASCVD—Risk in Percentage | p-Value | ||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Lower Risk | Borderline-to-Intermediate Risk | High Risk | ||||||||
| No | % | No | % | No | % | No | % | |||
| Middle | Yes | 1508 | 9.1% | 471 | 3.8% | 479 | 20.2% | 558 | 29.8% | 0.001 * |
| No | 15,037 | 90.9% | 11,831 | 96.2% | 1891 | 79.8% | 1315 | 70.2% | ||
| Northern | Yes | 1032 | 6.8% | 336 | 2.8% | 321 | 17.9% | 375 | 27.0% | 0.001 * |
| No | 14,147 | 93.2% | 11,658 | 97.2% | 1475 | 82.1% | 1014 | 73.0% | ||
| Eastern | Yes | 1653 | 9.7% | 499 | 3.9% | 515 | 22.3% | 639 | 35.5% | 0.001 * |
| No | 15,329 | 90.3% | 12,372 | 96.1% | 1795 | 77.7% | 1162 | 64.5% | ||
| Southern | Yes | 561 | 6.4% | 181 | 2.8% | 163 | 13.4% | 217 | 23.2% | 0.001 * |
| No | 8150 | 93.6% | 6378 | 97.2% | 1055 | 86.6% | 717 | 76.8% | ||
| NA | Yes | 67 | 5.1% | 29 | 2.6% | 18 | 14.4% | 20 | 20.4% | 0.001 * |
| No | 1259 | 94.9% | 1074 | 97.4% | 107 | 85.6% | 78 | 79.6% | ||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Published by MDPI on behalf of the Lithuanian University of Health Sciences. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Alkhalaf, A.; Aljabr, Q.; Al Mulla, K.; Almubarak, D.; Khan, A.S.; Al Jaziri, Z.Y.; Albahrani, I. A 10-Year Risk Assessment and Primary Prevention Study of Atherosclerotic Cardiovascular Disease Among Adult Patients in Saudi Arabia: A Cross-Sectional Study. Medicina 2025, 61, 132. https://doi.org/10.3390/medicina61010132
Alkhalaf A, Aljabr Q, Al Mulla K, Almubarak D, Khan AS, Al Jaziri ZY, Albahrani I. A 10-Year Risk Assessment and Primary Prevention Study of Atherosclerotic Cardiovascular Disease Among Adult Patients in Saudi Arabia: A Cross-Sectional Study. Medicina. 2025; 61(1):132. https://doi.org/10.3390/medicina61010132
Chicago/Turabian StyleAlkhalaf, Abdulhameed, Qasem Aljabr, Khalid Al Mulla, Duaa Almubarak, Abdul Sattar Khan, Zainab Y. Al Jaziri, and Ibrahim Albahrani. 2025. "A 10-Year Risk Assessment and Primary Prevention Study of Atherosclerotic Cardiovascular Disease Among Adult Patients in Saudi Arabia: A Cross-Sectional Study" Medicina 61, no. 1: 132. https://doi.org/10.3390/medicina61010132
APA StyleAlkhalaf, A., Aljabr, Q., Al Mulla, K., Almubarak, D., Khan, A. S., Al Jaziri, Z. Y., & Albahrani, I. (2025). A 10-Year Risk Assessment and Primary Prevention Study of Atherosclerotic Cardiovascular Disease Among Adult Patients in Saudi Arabia: A Cross-Sectional Study. Medicina, 61(1), 132. https://doi.org/10.3390/medicina61010132






