Preoperative Factors on Loss of Range of Motion after Posterior Cervical Foraminotomy
Abstract
1. Introduction
2. Materials and Methods
2.1. Patients
2.2. Surgical Procedures
2.3. Clinical Measures
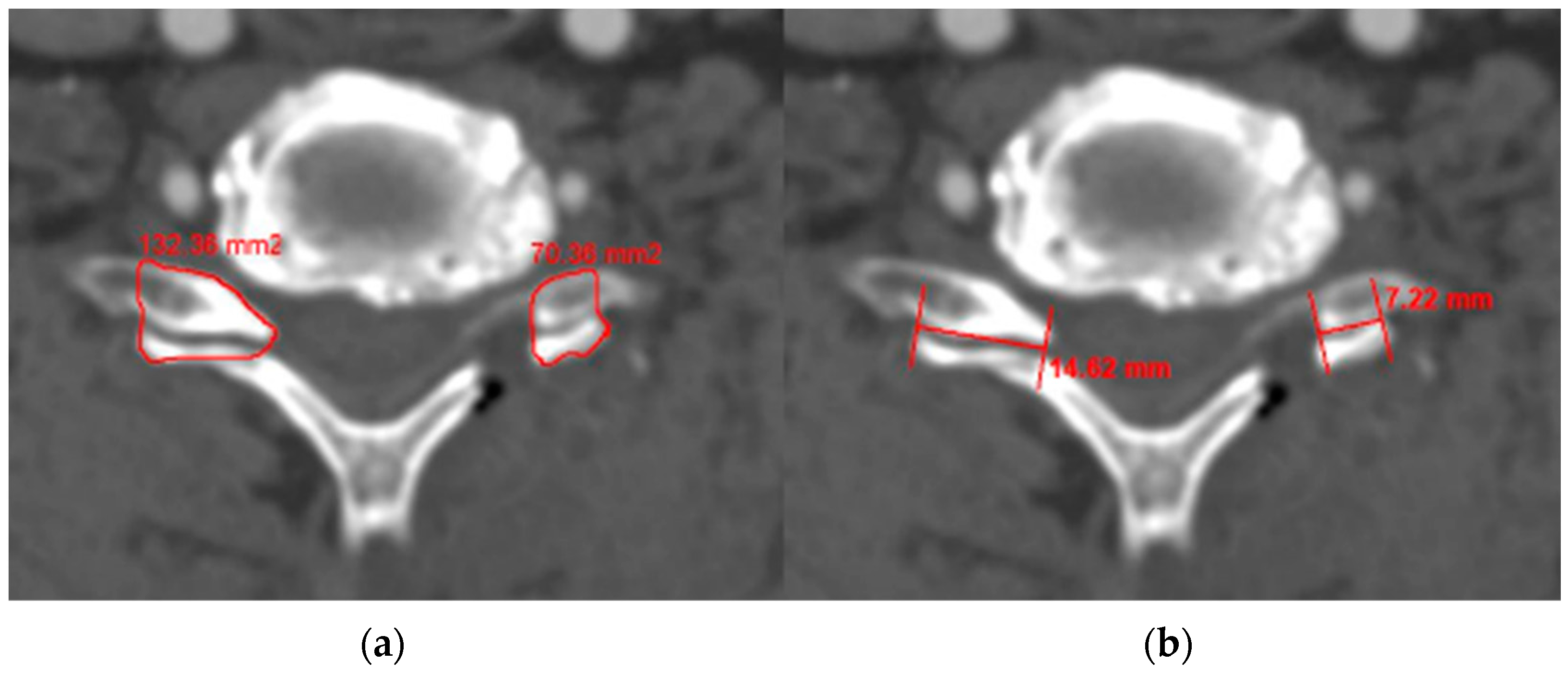
2.4. Radiological Measures
2.5. Statistical Analysis
3. Results
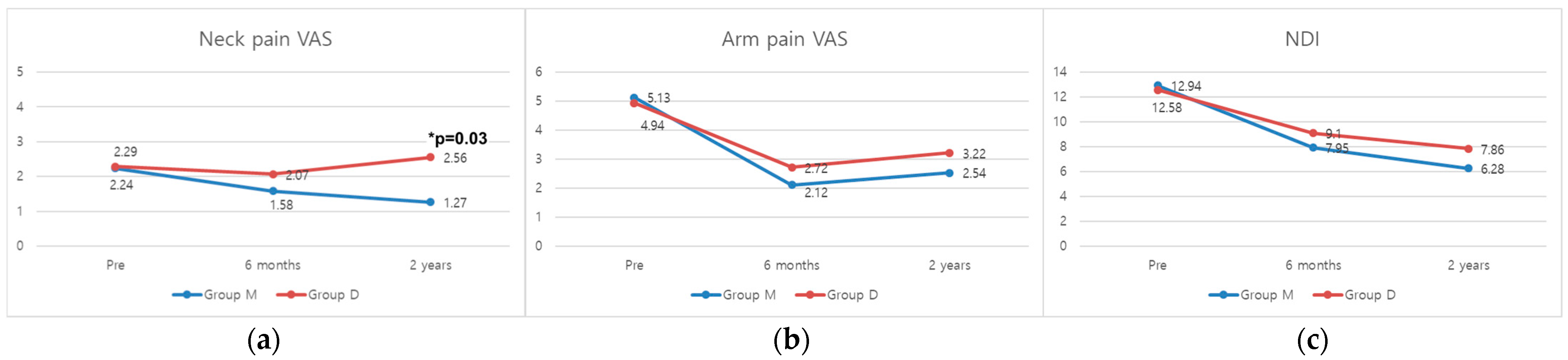
3.1. Clinical Outcomes
3.2. Radiological Assessment
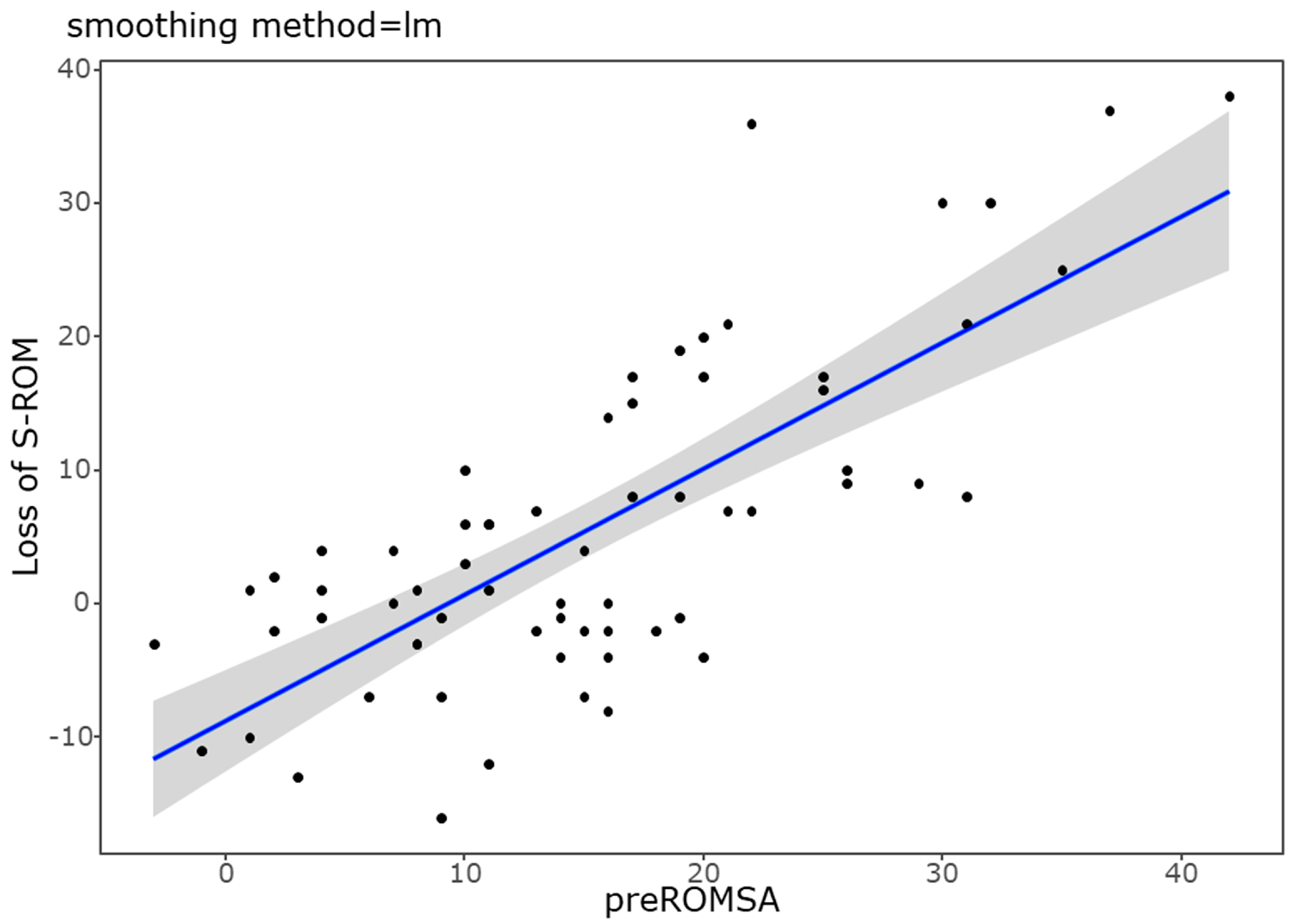
3.3. Factors Related to the ROM Loss after PCF
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Yoo, H.J.; Park, J.H.; Seong, H.Y.; Roh, S.W. Comparison of Surgical Results between Soft Ruptured Disc and Foraminal Stenosis Patients in Posterior Cervical Laminoforaminotomy. Korean J. Neurotrauma 2017, 13, 124–129. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Liu, W.J.; Hu, L.; Chou, P.H.; Wang, J.W.; Kan, W.S. Comparison of Anterior Cervical Discectomy and Fusion versus Posterior Cervical Foraminotomy in the Treatment of Cervical Radiculopathy: A Systematic Review. Orthop. Surg. 2016, 8, 425–431. [Google Scholar] [CrossRef] [PubMed]
- Dodwad, S.J.; Dodwad, S.N.; Prasarn, M.L.; Savage, J.W.; Patel, A.A.; Hsu, W.K. Posterior Cervical Foraminotomy: Indications, Technique, and Outcomes. Clin. Spine Surg. 2016, 29, 177–185. [Google Scholar] [CrossRef]
- Fehlings, M.G.; Gray, R.J. Posterior cervical foraminotomy for the treatment of cervical radiculopathy. J. Neurosurg. Spine 2009, 10, 343–344. [Google Scholar] [CrossRef] [PubMed]
- Zdeblick, T.A.; Zou, D.; Warden, K.E.; McCabe, R.; Kunz, D.; Vanderby, R. Cervical stability after foraminotomy. A biomechanical in vitro analysis. J. Bone Jt. Surg. Am. Vol. 1992, 74, 22–27. [Google Scholar] [CrossRef]
- Won, S.; Kim, C.H.; Chung, C.K.; Choi, Y.; Park, S.B.; Moon, J.H.; Heo, W.; Kim, S.M. Comparison of Cervical Sagittal Alignment and Kinematics after Posterior Full-endoscopic Cervical Foraminotomy and Discectomy According to Preoperative Cervical Alignment. Pain Physician 2017, 20, 77–87. [Google Scholar]
- Grieve, J.P.; Kitchen, N.D.; Moore, A.J.; Marsh, H.T. Results of posterior cervical foraminotomy for treatment of cervical spondylitic radiculopathy. Br. J. Neurosurg. 2000, 14, 40–43. [Google Scholar] [CrossRef]
- Totera, J.I.C.; Vargas, G.H.; Martini, I.F.; Romero, M.G.; Bacciarini, A.U.; Plaza, J.V.B. Unilateral Cervical Facet Fractures: Relevance of Acute Disc Injury in Conservative Treatment Failure. Asian Spine J. 2023, 17, 30–36. [Google Scholar] [CrossRef]
- Wang, S.J.; Jiang, S.D.; Jiang, L.S.; Dai, L.Y. Axial pain after posterior cervical spine surgery: A systematic review. Eur. Spine J. 2011, 20, 185–194. [Google Scholar] [CrossRef]
- Kim, M.W.; Kang, C.N.; Choi, S.H. Update of the Natural History, Pathophysiology, and Treatment Strategies of Degenerative Cervical Myelopathy: A Narrative Review. Asian Spine J. 2023, 17, 213–221. [Google Scholar] [CrossRef]
- Hyun, S.J.; Riew, K.D.; Rhim, S.C. Range of motion loss after cervical laminoplasty: A prospective study with minimum 5-year follow-up data. Spine J. 2013, 13, 384–390. [Google Scholar] [CrossRef] [PubMed]
- Raynor, R.B.; Pugh, J.; Shapiro, I. Cervical facetectomy and its effect on spine strength. J. Neurosurg. 1985, 63, 278–282. [Google Scholar] [CrossRef] [PubMed]
- Platt, A.; Gerard, C.S.; O’Toole, J.E. Comparison of outcomes following minimally invasive and open posterior cervical foraminotomy: Description of minimally invasive technique and review of literature. J. Spine Surg. 2020, 6, 243–251. [Google Scholar] [CrossRef] [PubMed]
- Lee, S.H.; Hyun, S.J.; Jain, A. Cervical Sagittal Alignment: Literature Review and Future Directions. Neurospine 2020, 17, 478–496. [Google Scholar] [CrossRef] [PubMed]
- Park, M.; Kelly, M.; Lee, D. Sagittal alignment as a predictor of clinical adjacent segment pathology requiring surgery after anterior cervical arthrodesis. Spine J. 2014, 14, 1228–1234. [Google Scholar] [CrossRef]
- Griffith, J.F.; Wang, Y.X.; Antonio, G.E.; Choi, K.C.; Yu, A.; Ahuja, A.T.; Leung, P.C. Modified Pfirrmann grading system for lumbar intervertebral disc degeneration. Spine 2007, 32, E708–E712. [Google Scholar] [CrossRef]
- Lee, T.H.; Kim, S.J.; Lim, S.M. Prevalence of disc degeneration in asymptomatic korean subjects. Part 2: Cervical spine. J. Korean Neurosurg. Soc. 2013, 53, 89–95. [Google Scholar] [CrossRef]
- Park, H.J.; Kim, S.S.; Lee, S.Y.; Park, N.H.; Chung, E.C.; Rho, M.H.; Kwon, H.J.; Kook, S.H. A practical MRI grading system for cervical foraminal stenosis based on oblique sagittal images. Br. J. Radiol. 2013, 86, 20120515. [Google Scholar] [CrossRef]
- Lee, D.H.; Lee, H.J.; Cho, J.H.; Hwang, C.J.; Yang, J.J.; Lee, C.S.; Park, S. Foraminal Restenosis after Posterior Cervical Foraminotomy for the Treatment of Cervical Radiculopathy. Global Spine J. 2023, 13, 2357–2366. [Google Scholar] [CrossRef]
- Lee, H.J.; Jeon, D.G.; Park, J.H. Correlation between kinematic sagittal parameters of the cervical lordosis or head posture and disc degeneration in patients with posterior neck pain. Open Med. 2021, 16, 161–168. [Google Scholar] [CrossRef]
- Lee, J.S.; Son, D.W.; Lee, S.H.; Kim, D.H.; Lee, S.W.; Song, G.S. The Predictable Factors of the Postoperative Kyphotic Change of Sagittal Alignment of the Cervical Spine after the Laminoplasty. J. Korean Neurosurg. Soc. 2017, 60, 577–583. [Google Scholar] [CrossRef] [PubMed]
- Lee, H.R.; Lee, D.H.; Seok, S.Y.; Lee, W.S.; Kim, M.; Cho, J.H.; Hwang, C.J.; Lee, C.S. Predictable factors for aggravation of cervical alignment after posterior cervical foraminotomy. J. Neurosurg. Spine 2023, 38, 174–181. [Google Scholar] [CrossRef] [PubMed]
- Jagannathan, J.; Sherman, J.H.; Szabo, T.; Shaffrey, C.I.; Jane, J.A. The posterior cervical foraminotomy in the treatment of cervical disc/osteophyte disease: A single-surgeon experience with a minimum of 5 years’ clinical and radiographic follow-up. J. Neurosurg. Spine 2009, 10, 347–356. [Google Scholar] [CrossRef] [PubMed]
- Schmieder, K.; Kettner, A.; Brenke, C.; Harders, A.; Pechlivanis, I.; Wilke, H.J. In vitro flexibility of the cervical spine after ventral uncoforaminotomy. Laboratory investigation. J. Neurosurg. Spine 2007, 7, 537–541. [Google Scholar] [CrossRef]
- Liu, B.; Wu, B.; Van Hoof, T.; Okito, J.P.; Liu, Z.; Zeng, Z. Are the standard parameters of cervical spine alignment and range of motion related to age, sex, and cervical disc degeneration? J. Neurosurg. Spine 2015, 23, 274–279. [Google Scholar] [CrossRef]
- Grob, D.; Frauenfelder, H.; Mannion, A.F. The association between cervical spine curvature and neck pain. Eur. Spine J. 2007, 16, 669–678. [Google Scholar] [CrossRef]
- Iizuka, H.; Iizuka, Y.; Nakagawa, Y.; Nakajima, T.; Toda, N.; Shimegi, A.; Tsutsumi, S.; Takagishi, K. Interlaminar bony fusion after cervical laminoplasty: Its characteristics and relationship with clinical results. Spine 2006, 31, 644–647. [Google Scholar] [CrossRef]
- Chen, Q.; Baba, H.; Kamitani, K.; Furusawa, N.; Imura, S. Postoperative bone re-growth in lumbar spinal stenosis. A multivariate analysis of 48 patients. Spine 1994, 19, 2144–2149. [Google Scholar] [CrossRef]
- Sawa, A.G.U.; de Andrada Pereira, B.; Rodriguez-Martinez, N.G.; Reyes, P.M.; Kelly, B.P.; Crawford, N.R. In Vitro Biomechanics of Human Cadaveric Cervical Spines with Mature Fusion. Int. J. Spine Surg. 2021, 15, 890–898. [Google Scholar] [CrossRef]
- Bono, C.M.; Khandha, A.; Vadapalli, S.; Holekamp, S.; Goel, V.K.; Garfin, S.R. Residual sagittal motion after lumbar fusion: A finite element analysis with implications on radiographic flexion-extension criteria. Spine 2007, 32, 417–422. [Google Scholar] [CrossRef]
- Lee, D.H.; Cho, J.H.; Hwang, C.J.; Lee, C.S.; Cho, S.K.; Ha, J.K. Can C3 Laminectomy Reduce Interlaminar Bony Fusion and Preserve the Range of Motion After Cervical Laminoplasty? Spine 2016, 41, 1884–1890. [Google Scholar] [CrossRef] [PubMed]
- Meisingset, I.; Woodhouse, A.; Stensdotter, A.K.; Stavdahl, Ø.; Lorås, H.; Gismervik, S.; Andresen, H.; Austreim, K.; Vasseljen, O. Evidence for a general stiffening motor control pattern in neck pain: A cross sectional study. BMC Musculoskelet Disord. 2015, 16, 56. [Google Scholar] [CrossRef] [PubMed]
- Mantel, N.; Haenszel, W. Statistical aspects of the analysis of data from retrospective studies of disease. J. Natl. Cancer Inst. 1959, 22, 719–748. [Google Scholar] [PubMed]
- Cho, T.G.; Kim, Y.B.; Park, S.W. Long term effect on adjacent segment motion after posterior cervical foraminotomy. Korean J. Spine 2014, 11, 1–6. [Google Scholar] [CrossRef][Green Version]
- Kwon, Y.J. Long-term clinical and radiologic outcomes of minimally invasive posterior cervical foraminotomy. J. Korean Neurosurg. Soc. 2014, 56, 224–229. [Google Scholar] [CrossRef]

| Group D (n = 34) | Group M (n = 42) | p | |
|---|---|---|---|
| Age (years) | 63.00 ± 9.50 | 64.29 ± 10.67 | 0.710 |
| Sex (M:F) | 24:10 | 32:10 | 0.485 |
| Level (1:2:3:4) | 0:16:16:2 | 4:20:16:2 | 0.362 |
| BMD | −0.86 ± 1.11 | −0.82 ± 1.52 | 0.954 |
| DM | 0.78 ± 0.39 | 0.38 ± 0.50 | 0.176 |
| Smoking | 0.18 ± 0.39 | 0.14 ± 0.36 | 0.785 |
| CAD | 0.06 ± 0.24 | 0.14 ± 0.36 | 0.415 |
| Hospital stay (days) | 6.30 ± 2.80 | 5.80 ± 2.00 | 0.368 |
| Operation time (min) | 102.4 ± 34.10 | 95.90 ± 29.2 | 0.436 |
| Group D (n = 34) | Group M (n = 42) | p | |
|---|---|---|---|
| Segmental Angle (°) | |||
| Preoperative | −0.3 ± 6.0 | −2.8 ± 5.4 | 0.089 |
| Postoperative 6 M | −0.5 ± 5.6 | −4.1 ± 6.5 | 0.021 * |
| Postoperative 2 Y | −0.1 ± 4.6 | −3.8 ± 6.1 | 0.012 * |
| Cervical Angle (°) | |||
| Preoperative | −5.0 ± 9.0 | −9.0 ± 10.1 | 0.098 |
| Postoperative 6 M | −4.6 ± 8.0 | −11.8 ± 11.5 | 0.006 * |
| Postoperative 2 Y | −4.7 ± 8.8 | −13.0 ± 12.3 | 0.005 * |
| C2–C7 SVA (mm) | |||
| Preoperative | 21.0 ± 10.4 | 21.6 ± 12.5 | 0.816 |
| Postoperative 6 M | 21.2 ± 9.5 | 17.9 ± 11.7 | 0.211 |
| Postoperative 2 Y | 19.8 ± 11.8 | 19.1 ± 10.6 | 0.822 |
| Flexion Segmental Angle (°) | |||
| Preoperative | 12.6 ± 6.9 | 3.9 ± 7.5 | <0.001 * |
| Postoperative 6 M | 9.2 ± 6.3 | 5.2 ± 5.5 | 0.010 * |
| Postoperative 2 Y | 7.0 ± 7.5 | 6.2 ± 5.6 | 0.641 |
| Extension Segmental Angle (°) | |||
| Preoperative | −7.8 ± 7.5 | −5.9 ± 6.8 | 0.287 |
| Postoperative 6 M | −3.7 ± 6.4 | −8.0 ± 5.7 | 0.007 * |
| Postoperative 2 Y | −0.8 ± 6.0 | −8.5 ± 6.7 | <0.001 * |
| Flexion Cervical Angle (°) | |||
| Preoperative | 23.6 ± 10.0 | 11.4 ± 16.0 | 0.001 * |
| Postoperative 6 M | 17.2 ± 10.4 | 13.6 ± 12.8 | 0.216 |
| Postoperative 2 Y | 16.2 ± 12.5 | 14.3 ± 10.6 | 0.548 |
| Extension Cervical Angle (°) | |||
| Preoperative | −15.2 ± 13.2 | −18.8 ± 14.2 | 0.293 |
| Postoperative 6 M | −11.9 ± 10.6 | −20.8 ± 11.0 | 0.002 * |
| Postoperative 2 Y | −10.2 ± 10.1 | −22.8 ± 12.3 | <0.001 * |
| Group D (n = 34) | Group M (n = 42) | p | |
|---|---|---|---|
| Pre-segmental ROM | 20.4 ± 9.6 | 9.8 ± 6.3 | <0.001 * |
| 6 M segmental ROM | 12.2 ± 6.6 | 12.8 ± 7.2 | 0.714 |
| ROM change (pre-6 M) | −8.2 ± 8.6 | 3.0 ± 6.9 | <0.001 * |
| 2 Y segmental ROM | 6.1 ± 7.3 | 13.7 ± 7.1 | <0.001 * |
| ROM change (6 M-2 Y) | −6.2 ± 7.9 | 0.9 ± 6.3 | <0.001 * |
| Pre-cervical ROM | 38.7 ± 15.5 | 30.2 ± 18.9 | 0.049 * |
| 6 M cervical ROM | 20.8 ± 15.7 | 34.7 ± 17.0 | 0.001 * |
| ROM change (pre-6 M) | −18.3 ± 18.7 | 3.1 ± 17.8 | 0.002 * |
| 2 Y cervical ROM | 27.4 ± 13.9 | 33.2 ± 15.4 | 0.114 |
| ROM change (6 M-2 Y) | 7.2 ± 17.7 | −1.5 ± 13.5 | 0.030 * |
| Group D (n = 34) | Group M (n = 42) | p | |
|---|---|---|---|
| Disc height (mm) | 3.6 ± 0.9 | 3.9 ± 0.8 | 0.161 |
| Gliding distance (mm) | 1.9 ± 3.3 | 1.4 ± 0.8 | 0.452 |
| Pre-foraminal dimension (mm2) | 31.5 ± 7.8 | 34.3 ± 8.5 | 0.164 |
| Post-foraminal dimension (mm2) | 53.3 ± 7.4 | 54.5 ± 8.2 | 0.517 |
| Foraminal enlargement (%) | 75.5 ± 34.6 | 63.8 ± 26.1 | 0.132 |
| Foraminal stenosis grade | 3.7 ± 0.4 | 3.6 ± 0.5 | 0.103 |
| Pfirrmann grade | 4.0 ± 0.5 | 3.6 ± 0.5 | 0.014 * |
| Facetectomy, area (%) | 52.9 ± 12.9 | 46.9 ± 15.9 | 0.101 |
| Facetectomy, width (%) | 49.5 ± 10.3 | 46.1 ± 11.7 | 0.451 |
| Bone bridge (n, %) | 21 (61.8%) | 11 (26.2%) | 0.004 * |
| Variable | Univariate | Multivariate | |||
|---|---|---|---|---|---|
| B (SE) | p | B (SE) | 95% CI | p | |
| (R2 = 0.5755, p < 0.001) | |||||
| Bone bridge | 5.33 (2.71) | 0.046 * | 1.53 (2.06) | −0.15–0.32 | 0.118 |
| Facetectomy (%) | 0.01 (0.11) | 0.903 | |||
| Preop SA | −0.04 (0.3) | 0.881 | |||
| Preop CA | 0.25 (0.18) | 0.184 | |||
| C2–C7 SVA | −0.24 (0.15) | 0.117 | |||
| Pre-segmental ROM | 0.82 (0.12) | <0.001 * | 0.80 (0.12) | 0.51–0.94 | <0.001 * |
| Disc height | −0.81 (1.91) | 0.675 | |||
| Gliding distance | 0.22 (0.54) | 0.683 | |||
| Pfirmann grade | 4.38 (2.94) | 0.145 | |||
| Foraminal stenosis grade | 5.53 (4.03) | 0.178 | |||
| Preop foraminal area | −0.31 (0.21) | 0.142 | |||
| Foraminal enlargement (%) | 0.02 (0.05) | 0.724 | |||
| Number of levels | 1.76 (2.62) | 0.506 | |||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Published by MDPI on behalf of the Lithuanian University of Health Sciences. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lee, D.-H.; Lee, H.R.; Seok, S.Y.; Choi, J.U.; Park, J.M.; Yang, J.-H. Preoperative Factors on Loss of Range of Motion after Posterior Cervical Foraminotomy. Medicina 2024, 60, 1496. https://doi.org/10.3390/medicina60091496
Lee D-H, Lee HR, Seok SY, Choi JU, Park JM, Yang J-H. Preoperative Factors on Loss of Range of Motion after Posterior Cervical Foraminotomy. Medicina. 2024; 60(9):1496. https://doi.org/10.3390/medicina60091496
Chicago/Turabian StyleLee, Dong-Ho, Hyung Rae Lee, Sang Yun Seok, Ji Uk Choi, Jae Min Park, and Jae-Hyuk Yang. 2024. "Preoperative Factors on Loss of Range of Motion after Posterior Cervical Foraminotomy" Medicina 60, no. 9: 1496. https://doi.org/10.3390/medicina60091496
APA StyleLee, D.-H., Lee, H. R., Seok, S. Y., Choi, J. U., Park, J. M., & Yang, J.-H. (2024). Preoperative Factors on Loss of Range of Motion after Posterior Cervical Foraminotomy. Medicina, 60(9), 1496. https://doi.org/10.3390/medicina60091496






