Perspectives in Using Multiple Flaps Reconstructions for Advanced Head and Neck Tumors (Scoping Review)
Abstract
1. Introduction
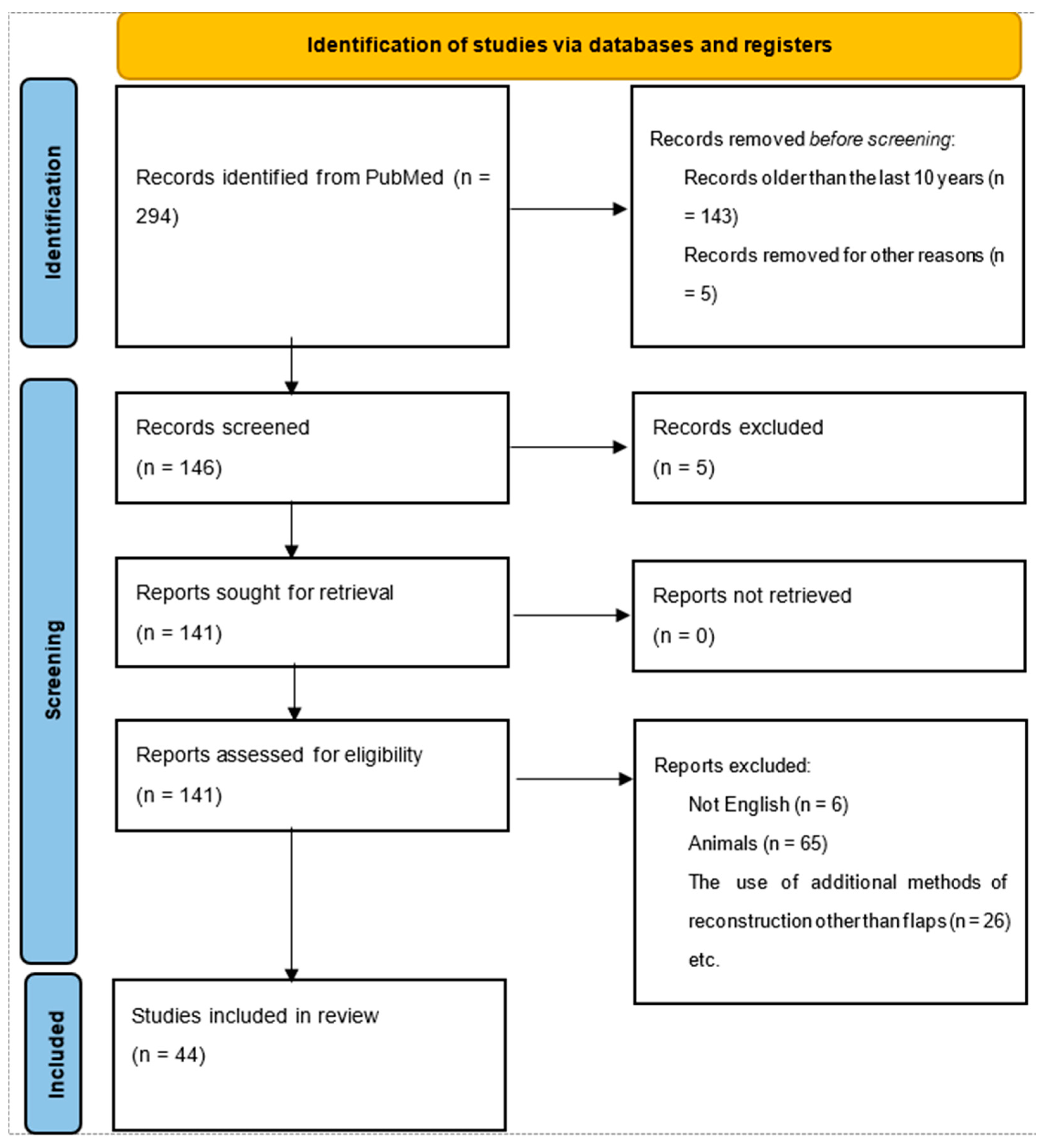
2. Methods
2.1. Data Collection Process
2.2. Literature Sources
3. Results
3.1. Success Rate
3.2. Factors Influencing Outcome
3.3. Flaps Used in Salvage Surgery
3.4. Other Factors
4. Discussions
4.1. Exploration of New Reconstruction Techniques
4.2. The Future of Head and Neck Reconstruction
4.3. Limitations and Future Directions
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| DFF | Double free flap |
| PMMC | Pectoralis major myocutaneous flap |
| LMIC | Low–middle income countries |
| SFF | Single free flap |
| TUG | Transverse upper gracilis flap |
| RAFF | Radial artery free flap |
| ALT | Anterolateral thigh flap |
| MSAP | Medial sural artery perforator |
| HPV | Human papilomavirus |
| RFFF | Radial forearm free flap |
| HNC | Head and neck carcinoma |
| MDT | Multidisciplinary team |
| GSV | Greater saphenous vein |
| STFF | Scapular tip free flap |
| 3D | Three dimensional |
References
- Barsouk, A.; Aluru, J.S.; Rawla, P.; Saginala, K.; Barsouk, A. Epidemiology, Risk Factors, and Prevention of Head and Neck Squamous Cell Carcinoma. Med. Sci. 2023, 11, 42. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Ferlay, J.; Colombet, M.; Soerjomataram, I.; Parkin, D.M.; Piñeros, M.; Znaor, A.; Bray, F. Cancer statistics for the year 2020: An overview. Int. J. Cancer 2021, 149, 778–789. [Google Scholar] [CrossRef] [PubMed]
- Wei, F.C.; Mardini, S. Flaps and Reconstructive Surgery. In Cummings Otolaryngology–Head and Neck Surgery, 7th ed.; Flint, P.W., Haughey, B.H., Lund, V.J., Robbins, T.K., Thomas, J.R., Lesperance, M.M., Francis, H.W., Eds.; Elsevier: Philadelphia, PA, USA, 2021; pp. 361–377. [Google Scholar]
- Khouri, R.K.; Cooley, B.C.; Kunselman, A.R.; Landis, J.R.; Yeramian, P.; Ingram, D.; Natarajan, N.; Benes, C.O.; Wallemark, C. A prospective study of microvascular free-flap surgery and outcome. Plast. Reconstr. Surg. 1998, 102, 711–721. [Google Scholar] [CrossRef] [PubMed]
- Tharakan, T.; Marfowaa, G.; Akakpo, K.; Jackson, R.; Zenga, J.; Puram, S.V.; Pipkorn, P. Multiple simultaneous free flaps for head and neck reconstruction: A multi-institutional cohort. Oral Oncol. 2023, 136, 106269. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Silva, A.; Caixeirinho, P.; Vilares, M.; Semedo, C.; Martins, M.; Zagalo, C.; Casal, D. Retrospective Study of 114 Free Flaps for Head and Neck Oncological Reconstruction in a Portuguese Tertiary Cancer Center. Acta Medica Port. 2022, 35, 192–200. [Google Scholar] [CrossRef] [PubMed]
- Fermi, M.; Bassano, E.; Molinari, G.; Alicandri-Ciufelli, M.; Scarpa, A.; Presutti, L.; De Santis, G.; Mattioli, F. Prelaminated flaps in head and neck cancer reconstructive surgery: A systematic review. Microsurgery 2021, 41, 584–593. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Okoturo, E. Regional Myocutaneous Flaps for Head and Neck Reconstruction: Experience of a Head and Neck Cancer Unit. Niger. J. Surg. 2015, 21, 85–90. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Gan, W.; Xiang, Y.; Lv, D.; Liu, J.; Wang, H.; Deng, D.; Wang, J.; Li, L.; Ma, T.; Liu, S.; et al. Complex reconstruction technique applied in advanced head and neck cancer. Medicine 2020, 99, e18810. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Deganello, A.; Rampinelli, V.; Gualtieri, T.; Piazza, C. Versatility of the subscapular system of flaps in head and neck oncologic reconstruction. Curr. Opin. Otolaryngol. Head Neck Surg. 2022, 30, 161–167. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Choi, N.; Cho, J.-K.; Jang, J.Y.; Cho, J.K.; Cho, Y.S.; Baek, C.-H. Scapular Tip Free Flap for Head and Neck Reconstruction. Clin. Exp. Otorhinolaryngol. 2015, 8, 422–429. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Mo, K.W.; Vlantis, A.; Wong, E.W.; Chiu, T. Double free flaps for reconstruction of complex/composite defects in head and neck surgery. Hong Kong Med. J. 2014, 20, 279–284. [Google Scholar] [CrossRef] [PubMed]
- Kaul, P.; Poonia, D.R.; Seenivasagam, R.K.; Maharaj, D.D.; Jat, B.R.; Garg, P.K.; Agarwal, S.P. Technical Considerations and Outcome Analysis of Using Extended Bipaddle Pectoralis Major Myocutaneous Flaps for Reconstructions of Large and Complex Oral Cavity Defects: Expanding the Horizons. Indian J. Surg. Oncol. 2021, 12, 484–490. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Pastars, K.; Zarins, J.; Tars, J.; Ivanova, A.; Skagers, A. Microsurgical reconstruction of oral defects with free flaps for patients with oral cancer: An 8 year experience with 153 consecutive cases. Stomatologija 2018, 20, 39–42. [Google Scholar] [PubMed]
- Chien, S.-H.; Hsu, H.M.; Huang, C.-C.; Lee, C.-Y.; Chiu, C.-H.M.; Lin, C.-M. Reconstruction of advance head and neck cancer patients after tumor ablation with simultaneous multiple free flaps: Indications and prognosis. Ann. Plast. Surg. 2012, 69, 611–615. [Google Scholar] [CrossRef] [PubMed]
- Jiang, C.; Guo, F.; Li, N.; Liu, W.; Su, T.; Chen, X.; Zheng, L.; Jian, X. Multipaddled anterolateral thigh chimeric flap for reconstruction of complex defects in head and neck. PLoS ONE 2014, 9, e106326. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Huang, T.C.; Ciudad, P.; Manrique, O.J.; Agko, M.; Chen, S.-H.; Tang, P.Y.-B.; Sabbagh, M.D.; Chen, H.-C. Staged inset of free flaps for complex microsurgical head and neck reconstruction to ensure total flap survival. Microsurgery 2018, 38, 844–851. [Google Scholar] [CrossRef] [PubMed]
- Smith, J.; Black, N.; Vallejo-Torres, L.; Morris, S.; Knight, J.C. Costs and Outcomes of Microsurgical Reconstruction after Head and Neck Cancer: A Systematic Review. Plast. Reconstr. Surg. 2023, 151, 89–99. [Google Scholar] [CrossRef] [PubMed]
- Gugliotta, Y.; Rubattino, S.; Fasolis, M.; Ramieri, G.; Copelli, C. Postoperative infections associated with microvascular free flaps in head and neck reconstruction: Analysis of risk factors and results with a standardized prophylaxis protocol. J. Plast. Reconstr. Aesthetic Surg. 2023, 87, 61–68. [Google Scholar] [CrossRef] [PubMed]
- Scaglioni, M.F.; Kuo, Y.-R.; Yang, J.C.-S.; Chen, Y.-C. The Posteromedial Thigh Flap for Head and Neck Reconstruction: Anatomical Basis, Surgical Technique, and Clinical Applications. Plast. Reconstr. Surg. 2015, 136, 363–375. [Google Scholar] [CrossRef] [PubMed]
- Patel, U.A.; Moore, B.A.; Wax, M.K.; Rosenthal, E.L. Composite resection and free flap reconstruction: Outcomes and evolution. Laryngoscope 2019, 129, 1877–1883. [Google Scholar] [CrossRef] [PubMed]
- Wang, Y.; Zhang, L.; Zhang, H.; Wang, H.; Yang, J.; Hu, Q. Outcomes of scalp reconstruction using the latissimus dorsi myocutaneous flap after oncological resection: A retrospective case series. Plast. Reconstr. Surg. 2019, 143, 1294–1302. [Google Scholar] [CrossRef]
- Agrawal, G.; Gupta, A.; Chaudhary, V.; Qureshi, F.; Choraria, A.; Dubey, H. Medial Sural Artery Perforator Flap for Head and Neck Reconstruction. Ann. Maxillofac. Surg. 2018, 8, 61–65. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Ki, S.H.; Ma, S.H.; Sim, S.H.; Choi, M.S.S. Unplanned change from double free flap to a chimeric anterolateral thigh flap in recurrent laryngeal cancer. Arch. Craniofacial Surg. 2019, 20, 416–420. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Chung, J.-H.; Kim, K.-J.; Jung, K.-Y.; Baek, S.-K.; Park, S.-H.; Yoon, E.-S. Recipient vessel selection for head and neck reconstruction: A 30-year experience in a single institution. Arch. Craniofacial Surg. 2020, 21, 269–275. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Kota, S.; Khan, N.S.; Bollig, K.; Bridgeman, M.; Bollig, C.A. Outcomes of Head and Neck Free Tissue Transfer Requiring Vein Grafting: Systematic Review and Meta-analysis. Otolaryngol. Neck Surg. 2024, 170, 1280–1288. [Google Scholar] [CrossRef] [PubMed]
- Momeni, A.; Jacobson, J.Y.; Lee, G.K. Systematic Reviews Addressing Microsurgical Head and Neck Reconstruction. J. Craniofacial Surg. 2015, 26, 210–213. [Google Scholar] [CrossRef]
- Johnson, A.B.; Smith, C.D.; Jones, E.F. Intraoperative monitoring techniques for assessing flap perfusion in reconstructive surgery. Plast. Reconstr. Surg. 2018, 141, 382e–394e. [Google Scholar]
- Khoong, Y.M.; Huang, X.; Gu, S.; Zan, T. Imaging for thinned perforator flap harvest: Current status and future perspectives. Burns Trauma 2021, 9, tkab042. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Chae, M.P.; Hunter-Smith, D.J.; Chung, R.D.; Smith, J.A.; Rozen, W.M. 3D-printed, patient-specific DIEP flap templates for preoperative planning in breast reconstruction: A prospective case series. Gland. Surg. 2021, 10, 2192–2199. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Dhondge, R.; Hussain, M.; Singh, A.; Nagarkar, R. Lingual Artery as the Recipient Vessel of Choice in Patients Requiring a Second or Third Free Flap in Recurrent Oral Cancers and Vessel-Depleted Neck: A 5-Year Experience in a Single Institute. Indian J. Plast. Surg. 2023, 56, 494–498. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Chang, B.A.; Asarkar, A.A.; Horwich, P.M.; Nathan, C.A.O.; Hayden, R.E. Regional pedicled flap salvage options for large head and neck defects: The old, the new, and the forgotten. Laryngoscope Investig. Otolaryngol. 2022, 8, 63–75. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Weert, S.; Leemans, C.R. Salvage surgery in head and neck cancer. Oral Dis. 2021, 27, 117–124. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Deng, D.; Liu, J.; Chen, F.; Lv, D.; Gan, W.; Li, L.; Wang, J. Double-island anterolateral thigh free flap used in reconstruction for salvage surgery for locally recurrent head and neck carcinoma. Medicine 2018, 97, e12839. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Choi, B.H.; Park, S.O.; Ahn, H.C. Reconstructive methods to resolve intractable fistulas that develop after radiation therapy in patients with head and neck cancer. Arch. Craniofacial Surg. 2021, 22, 247–253. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Alotaibi, A.S.; Mardan, Q.N.S.; Almarghoub, M.A.; Mahabbat, N.A.; Almarshad, F.A.; Hashem, F.K. The pedicled lateral forehead flap in reconstructing oral floor defect—The last resort; case report. Int. J. Surg. Case Rep. 2021, 89, 106521. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Wang, L.; Zhang, H.; Liu, Y.; Wu, H. Impact of neoadjuvant therapy on outcomes following head and neck reconstruction: A meta-analysis. J. Surg. Oncol. 2022, 125, 859–867. [Google Scholar] [CrossRef]
- Jones, A.B.; Smith, C.D.; Brown, K.L. Innovations in head and neck oncology: A systematic review of 3D printing and virtual surgical planning. Otolaryngol.–Head Neck Surg. 2023, 169, 515–523. [Google Scholar]
- Gao, L.L.; Basta, M.; Kanchwala, S.K.; Serletti, J.M.; Low, D.W.; Wu, L.C. Cost-effectiveness of microsurgical reconstruction for head and neck defects after oncologic resection. Head Neck 2017, 39, 541–547. [Google Scholar] [CrossRef] [PubMed]
- Dort, J.C.; Sauro, K.M.; Chandarana, S.; Schrag, C.; Matthews, J.; Nakoneshny, S.; Manoloto, V.; Miller, T.; McKenzie, C.D.; Hart, R.D.; et al. The impact of a quality management program for patients undergoing head and neck resection with free-flap reconstruction: Longitudinal study examining sustainability. J. Otolaryngol.—Head Neck Surg. 2020, 49, 42. [Google Scholar] [CrossRef] [PubMed]
- Johnson, A.B.; Smith, C.D.; Martinez, E.F. Intraoperative flap monitoring techniques in head and neck reconstruction: A scoping review. J. Reconstr. Microsurg. 2018, 34, 347–355. [Google Scholar]
- Meyer-Szary, J.; Luis, M.S.; Mikulski, S.; Patel, A.; Schulz, F.; Tretiakow, D.; Fercho, J.; Jaguszewska, K.; Frankiewicz, M.; Pawłowska, E.; et al. The Role of 3D Printing in Planning Complex Medical Procedures and Training of Medical Professionals—Cross-Sectional Multispecialty Review. Int. J. Environ. Res. Public Health 2022, 19, 3331. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Gorphe, P.; Temam, S.; Moya-Plana, A.; Leymarie, N.; Kolb, F.; Bout-Roumazeilles, A.; Qassemyar, Q.; Benmoussa, N.; Honart, J.-F. Indications and Clinical Outcomes of Transoral Robotic Surgery and Free Flap Reconstruction. Cancers 2021, 13, 2831. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Virós, P.D.; Viña, S.C.; Vila, P.J.; Palau, V.M.; Malagon, L.P.; Gonzàlez, L.C.; Higueras, S.C.; Pollán, G.C.M.; Carrasco, L.C. Oropharyngeal free flap reconstruction: Transoral robotic surgery versus open approach. Laryngoscope Investig. Otolaryngol. 2023, 8, 1564–1570. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Chen, X.; Wang, T.; Wang, Y.; Zhou, X.; Zhang, J. Application of computer-aided design and computer-aided manufacturing for complex head and neck reconstruction. J. Oral Maxillofac. Surg. 2020, 78, 89–96. [Google Scholar] [CrossRef] [PubMed]
- Lee, J.; Hwang, J.H.; Roh, J.L.; Choi, S.H.; Nam, S.Y.; Kim, S.Y. Clinical feasibility of three-dimensional virtual surgical simulation in head and neck reconstruction using a two-dimensional to three-dimensional fusion concept: A pilot study. J. Oral Maxillofac. Surg. 2022, 80, 612.e1–612.e14. [Google Scholar] [CrossRef] [PubMed]
- Li, J.J.; Kaplan, D.L.; Zreiqat, H. Scaffold-based regeneration of skeletal tissues to meet clinical challenges. J. Mater. Chem. B 2014, 2, 7272–7306. [Google Scholar] [CrossRef] [PubMed]
- McInnes, A.D.; Moser, M.A.J.; Chen, X. Preparation and Use of Decellularized Extracellular Matrix for Tissue Engineering. J. Funct. Biomater. 2022, 13, 240. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Park, J.H.; Lee, H.J.; Kim, Y.W.; Yang, C.E.; Park, Y.J. Efficacy and safety of adipose-derived stem cells for improving skin flap survival in ischemic wounds. Plast. Reconstr. Surg. 2018, 141, 382e–394e. [Google Scholar] [CrossRef] [PubMed]
- Wang, X.; Zhong, Y.; Zhu, Y.; Zhu, R.; Wang, X.; Mao, C. The role of stem cells in the accelerated blood flow in the arteriovenous loop flap. Biomaterials 2020, 262, 120359. [Google Scholar] [PubMed]
- Wei, F.-C.; Yazar, S.; Lin, C.-H.; Cheng, M.-H.; Tsao, C.-K.; Chiang, Y.-C. Double free flaps in head and neck reconstruction. Clin. Plast. Surg. 2005, 32, 303–308. [Google Scholar] [CrossRef] [PubMed]
- Ibrahim, A.; Javed, M.U.; Harbison, J.; Roy, J.M.; Caplash, Y. Double free flaps for head and neck reconstruction: A single centre experience. J. Plast. Reconstr. Aesthetic Surg. 2023, 86, 17–18. [Google Scholar] [CrossRef] [PubMed]
- Brinkman, J.N.; Kambiz, S.; de Jong, T.; Mureau, M.A.M. Long-Term Outcomes after Double Free Flap Reconstruction for Locally Advanced Head and Neck Cancer. J. Reconstr. Microsurg. 2019, 35, 66–73. [Google Scholar] [CrossRef] [PubMed]
- Wallace, C.G.; Tsao, C.-K.; Wei, F.-C. Role of multiple free flaps in head and neck reconstruction. Curr. Opin. Otolaryngol. Head Neck Surg. 2014, 22, 140–146. [Google Scholar] [CrossRef] [PubMed]
- Stalder, M.W.; Mundinger, G.S.; Bartow, M.; Pharo, A.; Patterson, C.; Sharma, S.; Aslam, R.; Hilaire, H.S. Single Versus Simultaneous Double Free Flaps for Head and Neck Reconstruction: Comparison of Flap Outcomes and Donor-Site Morbidity. Ann. Plast. Surg. 2019, 82, 184–189. [Google Scholar] [CrossRef]
- Cîrstea, A.-I.; Berteșteanu, V.G.; Scăunașu, R.-V.; Popescu, B.; Bejenaru, P.L.; Simion-Antonie, C.B.; Berteșteanu, G.S.; Diaconu, T.E.; Taher, P.B.; Rujan, S.-A.; et al. Management of Locally Advanced Laryngeal Cancer—From Risk Factors to Treatment, the Experience of a Tertiary Hospital from Eastern Europe. Int. J. Environ. Res. Public Health 2023, 20, 4737. [Google Scholar] [CrossRef] [PubMed]
- Taciuc, I.-A.; Dumitru, M.; Vrinceanu, D.; Gherghe, M.; Manole, F.; Marinescu, A.; Serboiu, C.; Neagos, A.; Costache, A. Applications and challenges of neural networks in otolaryngology (Review). Biomed. Rep. 2024, 20, 92. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Alfouzan, A.F. Review of surgical resection and reconstruction in head and neck cancer. Traditional versus current concepts. Saudi. Med. J. 2018, 39, 971–980. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Won, J.; Hong, J.W.; Kim, M.J.; Yun, I.-S.; Baek, W.Y.; Lee, W.J.; Lew, D.H.; Koh, Y.W.; Kim, S.-H. Methodology in Conventional Head and Neck Reconstruction Following Robotic Cancer Surgery: A Bridgehead Robotic Head and Neck Reconstruction. Yonsei Med. J. 2022, 63, 759–766. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Arora, R.; Verma, V.K.; Mishra, K.S.; Bhoye, H.; Kapoor, R. Reconstruction with free flaps in robotic head-and-neck onco-surgeries. Indian J. Plast. Surg. 2018, 51, 283–289. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Niu, Q.; Yang, Y.; Li, D.; Guo, W.; Wang, C.; Xu, H.; Feng, Z.; Han, Z. Exosomes Derived from Bone Marrow Mesenchymal Stem Cells Alleviate Ischemia-Reperfusion Injury and Promote Survival of Skin Flaps in Rats. Life 2022, 12, 1567. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Stern-Straeter, J.; Riedel, F.; Bran, G.; Hörmann, K.; Goessler, U.R. Advances in skeletal muscle tissue engineering. In Vivo 2007, 21, 435–444. [Google Scholar] [PubMed]
- Burnham, A.J.; Wicks, J.; Baugnon, K.L.; El-Deiry, M.W.; Schmitt, N.C. Free Flap Fat Volume is Not Associated With Recurrence or Wound Complications in Oral Cancer. OTO Open 2023, 7, e46. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Grošelj, A.; Tancer, I.; Jerman, A.; Paučič, J.; Pušnik, L. Pharyngeal reconstruction after total laryngectomy with sliding epiglottis: Technical aspects with retrospective review. Front. Oncol. 2024, 13, 1284266. [Google Scholar] [CrossRef] [PubMed]
- Gupta, A.; Baliarsing, A.S.; Thorat, T.S.; Bhat, U.; Garg, S.; Bhattacharyya, D. Flap Selection in Head and Neck Cancer Reconstruction. Int. J. Otorhinolaryngol. Clin. 2013, 5, 63–76. [Google Scholar] [CrossRef]
- D’Andréa, G.; Scheller, B.; Gal, J.; Chamorey, E.; Château, Y.; Dassonville, O.; Poissonnet, G.; Culié, D.; Koulmann, P.-H.; Hechema, R.; et al. How to select candidates for microvascular head and neck reconstruction in the elderly? Predictive factors of postoperative outcomes. Surg. Oncol. 2020, 34, 168–173. [Google Scholar] [CrossRef] [PubMed]
- Ota, Y.; Moore, A.; Spector, M.; Casper, K.; Stucken, C.; Malloy, K.; Lobo, R.; Baba, A.; Srinivasan, A. Prediction of Wound Failure in Patients with Head and Neck Cancer Treated with Free Flap Reconstruction: Utility of CT Perfusion and MR Perfusion in the Early Postoperative Period. Am. J. Neuroradiol. 2022, 43, 585–591, Erratum in AJNR Am. J. Neuroradiol. 2022, 43, E14. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Dekerle, L.; Cortese, S.; Salleron, J.; Rauch, P.; Mastronicola, R.; Beulque, E.; Chatard, M.; Hamitouche, S.; Alao, O.; Dolivet, G. Long-term survival after head and neck cancer surgery with immediate free flap reconstruction. Ann. Chir. Plast. Esthet. 2021, 66, 357–363. [Google Scholar] [CrossRef] [PubMed]
- Mazzola, F.; Smithers, F.; Cheng, K.; Mukherjee, P.; Low, T.-H.; Ch’ng, S.; Palme, C.E.; Clark, J.R. Time and cost-analysis of virtual surgical planning for head and neck reconstruction: A matched pair analysis. Oral Oncol. 2020, 100, 104491. [Google Scholar] [CrossRef] [PubMed]
- Lin, Z.; Lei, C.; Yang, L. Modern Image-Guided Surgery: A Narrative Review of Medical Image Processing and Visualization. Sensors 2023, 23, 9872. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Prasad, K.; Miller, A.; Sharif, K.; Colazo, J.M.; Ye, W.; Necker, F.; Baik, F.; Lewis, J.S.; Rosenthal, E.; Wu, J.Y.; et al. Augmented-Reality Surgery to Guide Head and Neck Cancer Re-resection: A Feasibility and Accuracy Study. Ann. Surg. Oncol. 2023, 30, 4994–5000. [Google Scholar] [CrossRef] [PubMed]
- Tricco, A.C.; Lillie, E.; Zarin, W.; O’Brien, K.K.; Colquhoun, H.; Levac, D.; Moher, D.; Peters, M.D.; Horsley, T.; Weeks, L.; et al. PRISMA Extension for Scoping Reviews (PRISMAScR): Checklist and Explanation. Ann. Intern. Med. 2018, 169, 467–473. [Google Scholar] [CrossRef]
| Source | Subjects | Region | Flap Used | Complications | Results/Conclusions |
|---|---|---|---|---|---|
| Silva A. et al. [6] | 114 microvascular free flap procedures | Oral | Radial forearm and fibular free flap | 6.1% partial necrosis 3.5% total necrosis | Microvascular reconstruction is a reliable treatment in head and neck reconstructive surgery |
| Matteo Fermi et al. [7] | 102 prelaminated flaps | Oral facial skin oropharynx laryngotracheal region | 92 free 10 pedicled | 0% total necrosis 17.6% partial flap loss | Low donor-site morbidity More studies would be needed for oncologic outcome |
| Okutoro E. et al. [8] | 17 regional myocutaneous pedicle flaps | Head and neck defects | 10 pectoralis major 7 others (platysma, trapezius, deltopectoral, forehead) | 0% total necrosis 17.6% partial flap loss 11.8% flap skin dehiscence 11.8% donor site infection | Useful in salvage surgery after free flap failure |
| Tharakan T. et al. [5] | 71 patients with multiple simultaneous free tissue transfer | Oral Maxillary sinus Pharynx Skull base Parotid | ALT Fibula RFFF Scapula Latissimus dorsi Parascapular Gracilis Femoral condyle Solear perforator MSAP | 26.8% major complications:
| |
| Gan W. et al. [9] | 7 patients with advanced HNC recurrence after MDT therapy | Head and neck defects (greater then 20 × 10 cm) Skull base | ALT Fascia lata flap Greater saphenous vein graft | 0% total necrosis 1 oral flap edge infections and necrosis | Composited reconstruction with ALT/fascia lata flap and GSV graft could repair large defects and inadequate vessels after advanced HNC tumor resection |
| Choi N. et al. [11] | 17 patients | Maxillary and mandibular defects | Angular branch-based scapular tip free flap | 5.9% flap failure 25% orbital revision for diplopia 12.5% oroantral fistula | The STFF offers a favorable toolbox of chimeric options for a vast variety of head and neck oncological defects |
| Mo KW et al. [12] | 12 patients | 0% total flap loss 2 (24%) reexploration of the flap 1 (12%) venous congestion of the fibula skin flap—reconstruction with pedicled pectoralis major flap (wound dehiscence after that) | Advantages: long pedicle, low flap failure, 3D nature of bone and soft tissue, small rate of donor site morbidity | ||
| Kaul P. et al. [13] | 72 oral cancer patients | Buccoalveolar defects | Extended bipaddle PMMC | 1 total flap loss 13.8% partial flap loss 25.1% major complications | |
| Pasters K. et al. [14] | 153 patients | Oral | Free flaps | 3.2% vascular thrombosis of the flap 4 total flap floss | Can be safely used for oral defects ≥ 10 cm in resource-limited LMIC countries |
| Chien S. et al. [15] | 58 patients (37 single free flap + 21 double free flap) | ALT Ulnar forearm Fibula TUG | 8.1% total flap loss SFF 4.8% total flap loss DFF 0% partial flap loss SFF 9.5% partial flap loss DFF | Simultaneous double-flap reconstructions of head and neck defects can be performed with a complication profile equivalent to single-flap reconstructions | |
| Jiang C. et al. [16] | 12 patients | Complex 3D defects: Oral Pharyngoesophagus Anterior neck skin | Multipaddled ALT chimeric flaps | 0% flap loss 0% problems with the donor or recipient sites | Multipaddled ALT chimeric flap provides several independent skin paddles for multiple separate defects simultaneously with minimal donor site morbidity. |
| Source (Main Author) | Study Design | Subjects | Region Reconstructed | Flap Used | Flap Success Rate (%) | Complications | Recipient Vessel |
|---|---|---|---|---|---|---|---|
| Tharakan et al. (2023) [5] | Prospective observational study | 30 | Oropharynx | ALT | 95 | Infection (8%) | Facial artery |
| Silva et al. (2022) [6] | Retrospective cohort study | 50 | Oral cavity | Radial forearm flap | 92 | Flap necrosis (12%) | External carotid artery |
| Gan et al. (2020) [9] | Case series | 15 | Hypopharynx | Scapular tip flap | 85 | Hematoma (5%) | Superior thyroid artery |
| Mo et al. (2014) [12] | Prospective observational study | 25 | Scalp | Supraclavicular artery island flap | 87 | Fistula (12%) | Superficial temporal artery |
| Huang et al. (2018) [17] | Retrospective case–control study | 25 | Larynx | Myocutaneous flap | 88 | Donor site morbidity (10%) | Internal jugular vein |
| Smith et al. (2021) [18] | Retrospective cohort study | 40 | Tongue | Fibula osteocutaneous flap | 94 | Hematoma (6%) | Inferior alveolar artery |
| Gugliotta et al. (2023) [19] | Prospective cohort study | 40 | Mandible | Fibula osteocutaneous flap | 98 | Wound dehiscence (7%) | Inferior alveolar artery |
| Scaglioni et al. (2015) [20] | Case–control study | 18 | Cheek | Posteromedial thigh flap | 96 | Hematoma (4%) | Facial artery |
| Patel et al. (2020) [21] | Prospective cohort study | 25 | Hypopharynx | Jejunal free flap | 91 | Anastomotic leak (10%) | Superior thyroid artery |
| Source (Main Author) | Study Design | Subjects (Number) | Region Reconstructed | Flap Used | Flap Success Rate (%) | Complications | Recipient Vessel |
|---|---|---|---|---|---|---|---|
| Okoturo (2015) [8] | Retrospective case series | 20 | Maxilla | Pectoralis major myocutaneous flap | 90 | Flap failure (5%) | Facial artery |
| Kaul et al. (2021) [13] | Retrospective cohort study | 35 | Parotid gland | Temporoparietal fascial flap | 93 | Seroma (8%) | External carotid artery |
| Wang et al. (2019) [22] | Retrospective case series | 30 | Scalp | Latissimus dorsi myocutaneous flap | 92 | Flap necrosis (8%) | Superficial temporal artery |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Cîrstea, A.-I.; Berteșteanu, Ș.V.G.; Vrînceanu, D.; Dumitru, M.; Bejenaru, P.L.; Simion-Antonie, C.B.; Schipor-Diaconu, T.E.; Taher, P.B.; Rujan, S.-A.; Grigore, R. Perspectives in Using Multiple Flaps Reconstructions for Advanced Head and Neck Tumors (Scoping Review). Medicina 2024, 60, 1340. https://doi.org/10.3390/medicina60081340
Cîrstea A-I, Berteșteanu ȘVG, Vrînceanu D, Dumitru M, Bejenaru PL, Simion-Antonie CB, Schipor-Diaconu TE, Taher PB, Rujan S-A, Grigore R. Perspectives in Using Multiple Flaps Reconstructions for Advanced Head and Neck Tumors (Scoping Review). Medicina. 2024; 60(8):1340. https://doi.org/10.3390/medicina60081340
Chicago/Turabian StyleCîrstea, Anca-Ionela, Șerban Vifor Gabriel Berteșteanu, Daniela Vrînceanu, Mihai Dumitru, Paula Luiza Bejenaru, Catrinel Beatrice Simion-Antonie, Teodora Elena Schipor-Diaconu, Petra Bianca Taher, Simona-Andreea Rujan, and Raluca Grigore. 2024. "Perspectives in Using Multiple Flaps Reconstructions for Advanced Head and Neck Tumors (Scoping Review)" Medicina 60, no. 8: 1340. https://doi.org/10.3390/medicina60081340
APA StyleCîrstea, A.-I., Berteșteanu, Ș. V. G., Vrînceanu, D., Dumitru, M., Bejenaru, P. L., Simion-Antonie, C. B., Schipor-Diaconu, T. E., Taher, P. B., Rujan, S.-A., & Grigore, R. (2024). Perspectives in Using Multiple Flaps Reconstructions for Advanced Head and Neck Tumors (Scoping Review). Medicina, 60(8), 1340. https://doi.org/10.3390/medicina60081340








