Vascular Port Complication Leading to Surgery of Pulmonary Artery Branch—A Case Report
Abstract
1. Introduction
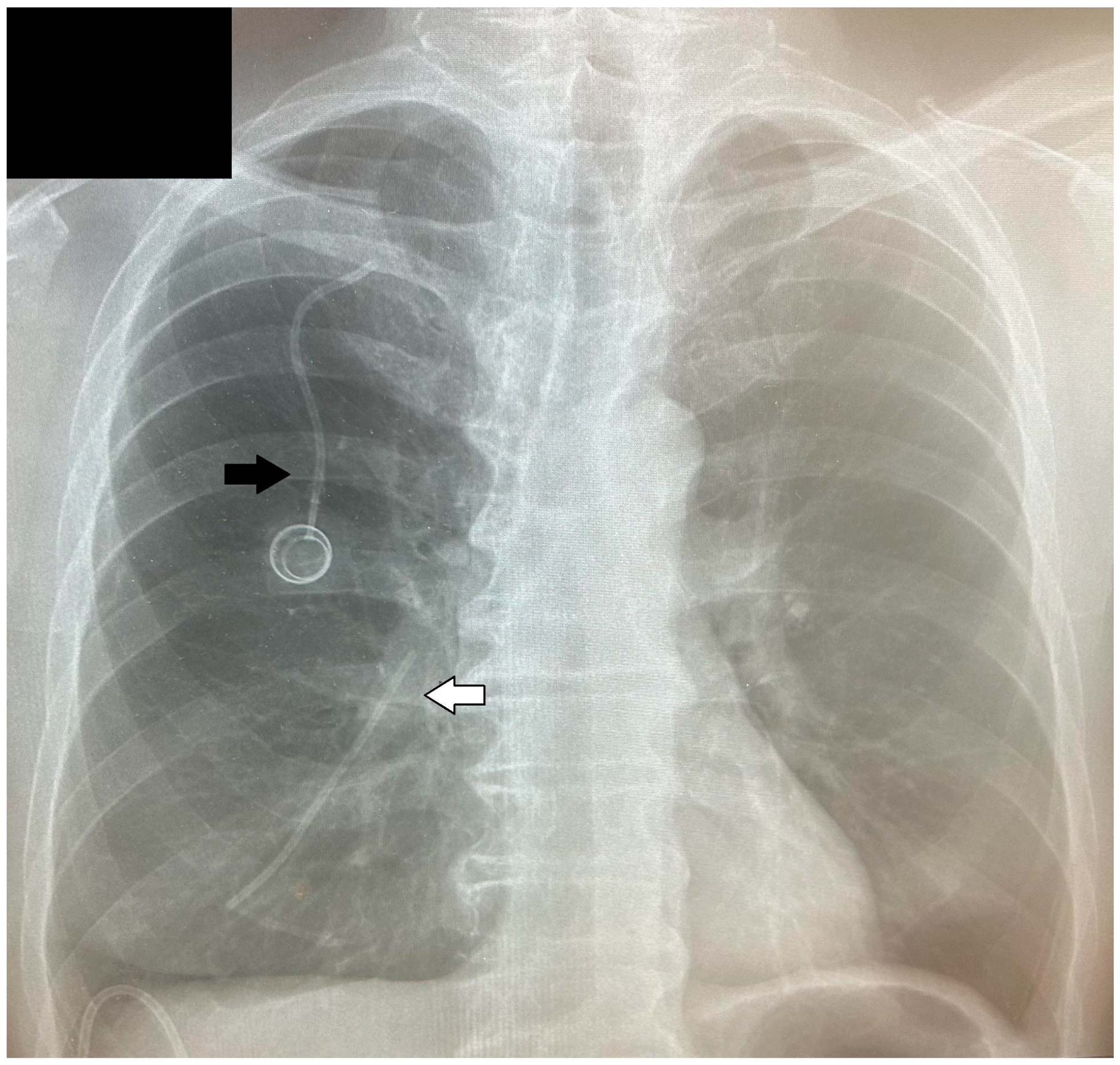
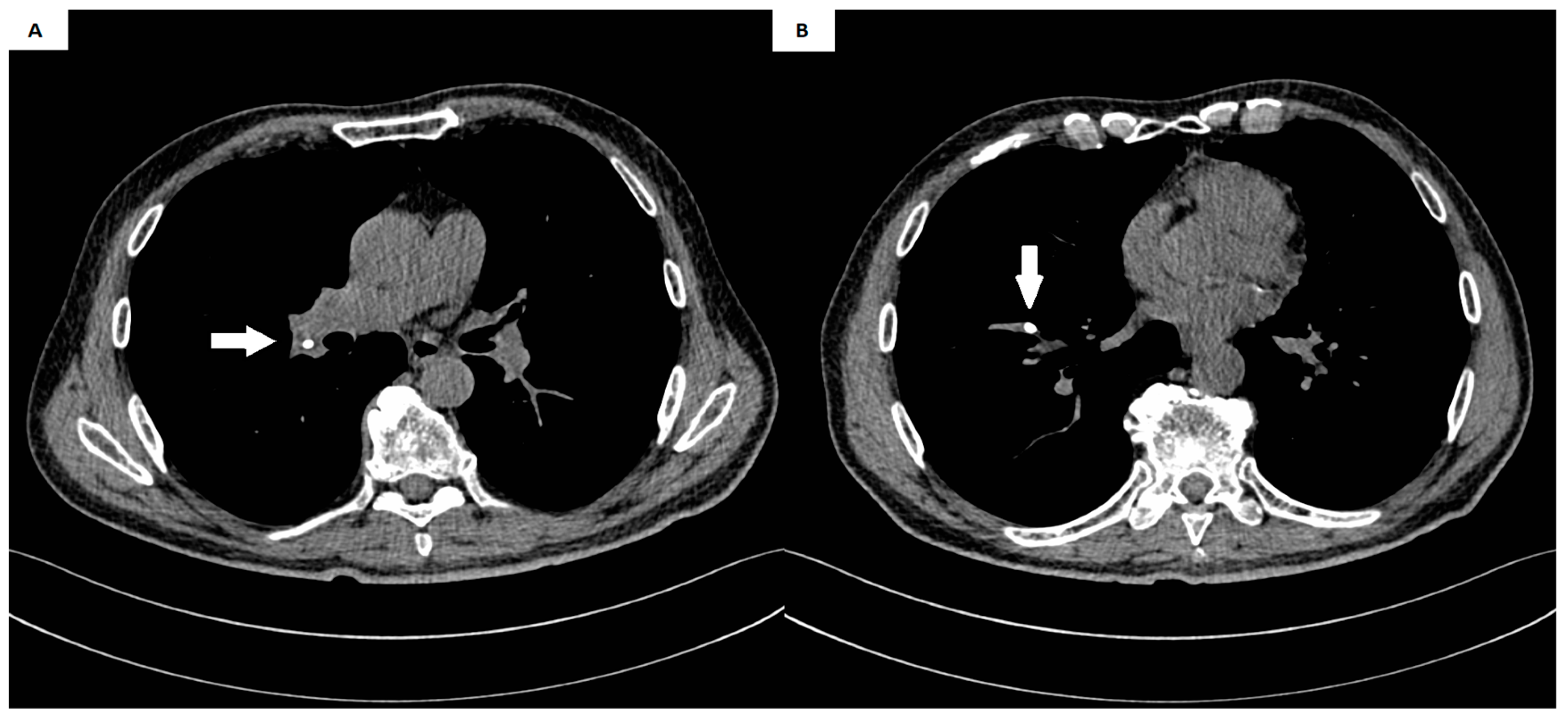
2. Case Presentation
3. Discussion
4. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Machat, S.; Eisenhuber, E.; Pfarl, G.; Stübler, J.; Koelblinger, C.; Zacherl, J.; Schima, W. Complications of central venous port systems: A pictorial review. Insights Imaging 2019, 10, 86. [Google Scholar] [CrossRef] [PubMed]
- Rydell, H.; Huge, Y.; Eriksson, V.; Johansson, M.; Alamdari, F.; Svensson, J.; Aljabery, F.; Sherif, A. Central Venous Access and the Risk for Thromboembolic Events in Patients Undergoing Neoadjuvant Chemotherapy and Radical Cystectomy for Muscle-Invasive Bladder Cancer. Life 2022, 12, 1198. [Google Scholar] [CrossRef] [PubMed]
- Akhtar, N.; Lee, L. Utilization and Complications of Central Venous Access Devices in Oncology Patients. Curr. Oncol. 2021, 28, 367–377. [Google Scholar] [CrossRef] [PubMed]
- Hoppe, A.; Rupa-Matysek, J.; Małecki, B.; Dytfeld, D.; Hoppe, K.; Gil, L. Risk Factors for Catheter-Related Thrombosis in Multiple Myeloma Patients Undergoing Autologous Stem Cell Transplantation. Medicina 2021, 57, 1020. [Google Scholar] [CrossRef] [PubMed]
- Ballarini, C.; Intra, M.; Ceretti, A.P.; Cordovana, A.; Pagani, M.; Farina, G.; Perrone, S.; Tomirotti, M.; Scanni, A.; Spina, G. Complications of subcutaneous infusion port in the general oncology population. Oncology 1999, 56, 97–102. [Google Scholar] [CrossRef] [PubMed]
- Kock, H.; Pietsch, M.; Krause, U.; Wilke, H.; Eigler, F. Implantable vascular access systems: Experience in 1500 patients with totally implanted central venous port systems. World J. Surg. 1998, 22, 12–16. [Google Scholar] [CrossRef] [PubMed]
- Kakkos, A.; Bresson, L.; Hudry, D.; Cousin, S.; Lervat, C.; Bogart, E.; Meurant, J.; El Bedoui, S.; Decanter, G.; Hannebicque, K.; et al. Complication-related removal of totally implantable venous access port systems: Does the interval between placement and first use and the neutropenia-inducing potential of chemotherapy regimens influence their incidence? A four-year prospective study of 4045 patients. Eur. J. Surg. Oncol. 2017, 43, 689–695. [Google Scholar] [CrossRef] [PubMed]
- Surov, A.; Jordan, K.; Buerke, M.; Persing, M.; Wollschlaeger, B.; Behrmann, C. Atypical pulmonary embolism of port catheter fragments in oncology patients. Support Care Cancer 2006, 14, 479–483. [Google Scholar] [CrossRef] [PubMed]
- Koller, M.; Papa, M.Z.; Zweig, A.; Ben-Ari, G. Spontaneous leak and transection of permanent subclavian catheters. J. Surg. Oncol. 1998, 68, 166–168. [Google Scholar] [CrossRef]
- Doering, R.B.; Stemmer, E.A.; Connolly, J.E.; Marx, G.F. Complications of indwelling venous catheters: With particular reference to catheter embolus. Am. J. Surg. 1967, 114, 259–266. [Google Scholar] [CrossRef]
- Sofue, K.; Arai, Y.; Takeuchi, Y.; Sugimura, K. Flow confirmation study for central venous port in oncologic outpatient undergoing chemotherapy: Evaluation of suspected system-related mechanical complications. Eur. J. Radiol. 2013, 82, e691–e696. [Google Scholar] [CrossRef] [PubMed]
- Surov, A.; Wienke, A.; Carter, J.M.; Stoevesandt, D.; Behrmann, C.; Spielmann, R.P.; Werdan, K.; Buerke, M. Intravascular Embolization of Venous Catheter—Causes, Clinical Signs, and Management: A Systematic Review. J. Parenter. Enter. Nutr. 2009, 33, 677–685. [Google Scholar] [CrossRef] [PubMed]
- Kaptein, F.; Kroft, L.; Hammerschlag, G.; Ninaber, M.; Bauer, M.; Huisman, M.; Klok, F. Pulmonary infarction in acute pulmonary embolism. Thromb. Res. 2021, 202, 162–169. [Google Scholar] [CrossRef] [PubMed]
- Mauri, D.; Zafeiri, G.; Tsali, L.; Chalkidou, A.; Zarkavelis, G.; Papadaki, A.; Filis, P.; Pentheroudakis, G. Identification of catheter misplacement in early port CVC dysfunction. Contemp. Oncol. 2018, 22, 129–134. [Google Scholar] [CrossRef] [PubMed]
- Dato, G.M.A.; Arslanian, A.; Di Marzio, P.; Filosso, P.L.; Ruffini, E. Posttraumatic and iatrogenic foreign bodies in the heart: Report of fourteen cases and review of the literature. J. Thorac. Cardiovasc. Surg. 2003, 126, 408–414. [Google Scholar] [CrossRef]
- Chandrashekhara, S.; Kumar, N. Inadvertently migrated fractured chemo port in pulmonary artery: A rare complication. Indian J. Med. Res. 2023, 157, 484–485. [Google Scholar] [CrossRef] [PubMed]
- Francisco, A.R.G.; Duarte, J.; de Oliveira, E.I. Port-A-Cath Catheter Embolization to Distal Pulmonary Artery Branches: Two Tailored Percutaneous Retrieval Approaches. Vasc. Endovasc. Surg. 2018, 52, 361–366. [Google Scholar] [CrossRef] [PubMed]
- Wu, K.; Lai, H.; Liu, Y.; Zhang, B. Percutaneous transvenous retrieval of fractured catheter in cancer patients receiving chemotherapy. J. X-ray Sci. Technol. 2018, 26, 1029–1037. [Google Scholar] [CrossRef] [PubMed]
- Cheng, C.-C.; Tsai, T.-N.; Yang, C.-C.; Han, C.-L. Percutaneous retrieval of dislodged totally implantable central venous access system in 92 cases: Experience in a single hospital. Eur. J. Radiol. 2009, 69, 346–350. [Google Scholar] [CrossRef]
- Dondelinger, R.; Lepoutre, B.; Kurdziel, J. Percutaneous vascular foreign body retrieval: Experience of an 11-year period. Eur. J. Radiol. 1991, 12, 4–10. [Google Scholar] [CrossRef]
- Abad, C.; Reina, V.-C.; Rodriguez-Suarez, P.-M. Surgical versus Percutaneous Removal of a Port-A-Catheter Tip Embolized in the Peripheral Pulmonary Artery. J. Vasc. Access. 2010, 11, 73. [Google Scholar] [CrossRef] [PubMed]
- Oz, K.; Demirhan, R.; Onan, B.; Sancakli, I. Pulmonary Artery Pseudoaneurysm after a Vascular Access Port Catheter Implantation. Ann. Thorac. Surg. 2009, 87, 295–297. [Google Scholar] [CrossRef] [PubMed]
- Fisher, R.G.; Ferreyro, R. Evaluation of current techniques for nonsurgical removal of intravascular foreign bodies. Am. J. Roentgenol. 1978, 130, 541–548. [Google Scholar] [CrossRef] [PubMed]
- Balbi, M.; Bertero, G.; Bellotti, S.; Rolandelli, M.-L.; Caponnetto, S. Right-sided valvular endocarditis supported by an unexpected intracardiac foreign body. Chest 1990, 97, 1486–1488. [Google Scholar] [CrossRef] [PubMed]
- Suarez-Penaranda, J.M.; Guitian-Barreiro; Concheiro-Carro, L. Longstanding intracardiac catheter embolism: An unusual autopsy finding. Am. J. Forensic. Med. Pathol. 1995, 16, 124–126. [Google Scholar] [CrossRef] [PubMed]
- Roye, G.D.; Breazeale, E.E.; Byrnes, J.P.M.; Rue, L.W. Management of catheter emboli. South. Med. J. 1996, 89, 714–717. [Google Scholar] [CrossRef] [PubMed]
- Tazzioli, G.; Gargaglia, E.; Vecchioni, I.; Papi, S.; Di Blasio, P.; Rossi, R. Retained embolized fragment of totally implantable central venous catheter in right ventricle: It is really necessary to remove? J. Vasc. Access. 2015, 16, 431–433. [Google Scholar] [CrossRef]
- Kara, H.; Arikan, A.E.; Dulgeroglu, O.; Uras, C.; Icten, G.E.; Tutar, B.; Parlakkilic, U.T.; Sonmez, O. Detachment and embolization of totally implantable central venous access devices: Diagnosis and management. Acta Chir. Belg. 2022, 122, 240–247. [Google Scholar] [CrossRef]


| First Author | Sex | Age | Primary Diagnosis | Symptoms | Localization | Length of Catheter Fragment [cm] | Method |
|---|---|---|---|---|---|---|---|
| Dato [15] | M | 22 | NR | Anxiety | Right pulmonary artery | 4 | Thoracotomy |
| Abad [21] | M | 48 | Colorectal carcinoma | Asymptomatic | Right pulmonary artery | 5.5 | Thoracotomy |
| Oz [22] | M | 57 | Gastric malignancy | Dyspnea, chest pain, fever | Left pulmonary artery | NR | Thoracotomy |
| Presented case | M | 67 | Gastric cancer | Cough, weakness, nausea, and heartburn | Right pulmonary artery | 8 | Thoracotomy |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kordykiewicz, D.; Skórka, P.; Morozik, M.; Wójcik, J.; Wojtyś, M.E. Vascular Port Complication Leading to Surgery of Pulmonary Artery Branch—A Case Report. Medicina 2024, 60, 1093. https://doi.org/10.3390/medicina60071093
Kordykiewicz D, Skórka P, Morozik M, Wójcik J, Wojtyś ME. Vascular Port Complication Leading to Surgery of Pulmonary Artery Branch—A Case Report. Medicina. 2024; 60(7):1093. https://doi.org/10.3390/medicina60071093
Chicago/Turabian StyleKordykiewicz, Dawid, Patryk Skórka, Maja Morozik, Janusz Wójcik, and Małgorzata Edyta Wojtyś. 2024. "Vascular Port Complication Leading to Surgery of Pulmonary Artery Branch—A Case Report" Medicina 60, no. 7: 1093. https://doi.org/10.3390/medicina60071093
APA StyleKordykiewicz, D., Skórka, P., Morozik, M., Wójcik, J., & Wojtyś, M. E. (2024). Vascular Port Complication Leading to Surgery of Pulmonary Artery Branch—A Case Report. Medicina, 60(7), 1093. https://doi.org/10.3390/medicina60071093






