Use of CPAP Ventilation in Non-ICU Wards May Influence Outcomes in Patients with Severe Respiratory COVID-19
Abstract
1. Introduction
2. Materials and Methods
- A group of 153 (one hundred and fifty-three) COVID-positive patients in the 2nd and 3rd pandemic waves, from 1 September 2020 to 4 January 2021, treated in a specially formed Intensive Care Unit—CRC at the University Hospital Rijeka with invasive mechanical ventilation (IMV) and NIV application. The aforementioned group will be labelled “CRC (2nd and 3rd Wave)”. The inclusive criteria were CRC admission due to worsening of the COVID-19 clinical presentation in units where oxygen was supplied via mask with a maximal flow of 10 L/min and the above-mentioned clinical status.
- A group of 102 (one hundred and two) COVID-positive 4th wave patients, from 1 October 2021 to 1 January 2022, initially treated in COVID 6 Non-ICU (Infectiology/Internal Isolation Unit/Ward). Respiratory failure was treated with oxygen supplementation with up to 10 L/min flow and, with the advent of the 4th wave, CPAP non-invasive ventilation, either helmet CPAP or full-face Venturi masks (Qmed twin-dual oxygen flowmeter, Italy). The inclusive criteria were a documented application of CPAP. A portion of patients required a transfer to the CRC, with advanced ventilation therapy, either IMV or NIV, due to their worsening clinical status. The aforementioned group will be labelled as “COVID 6/CRC (4th wave)”.
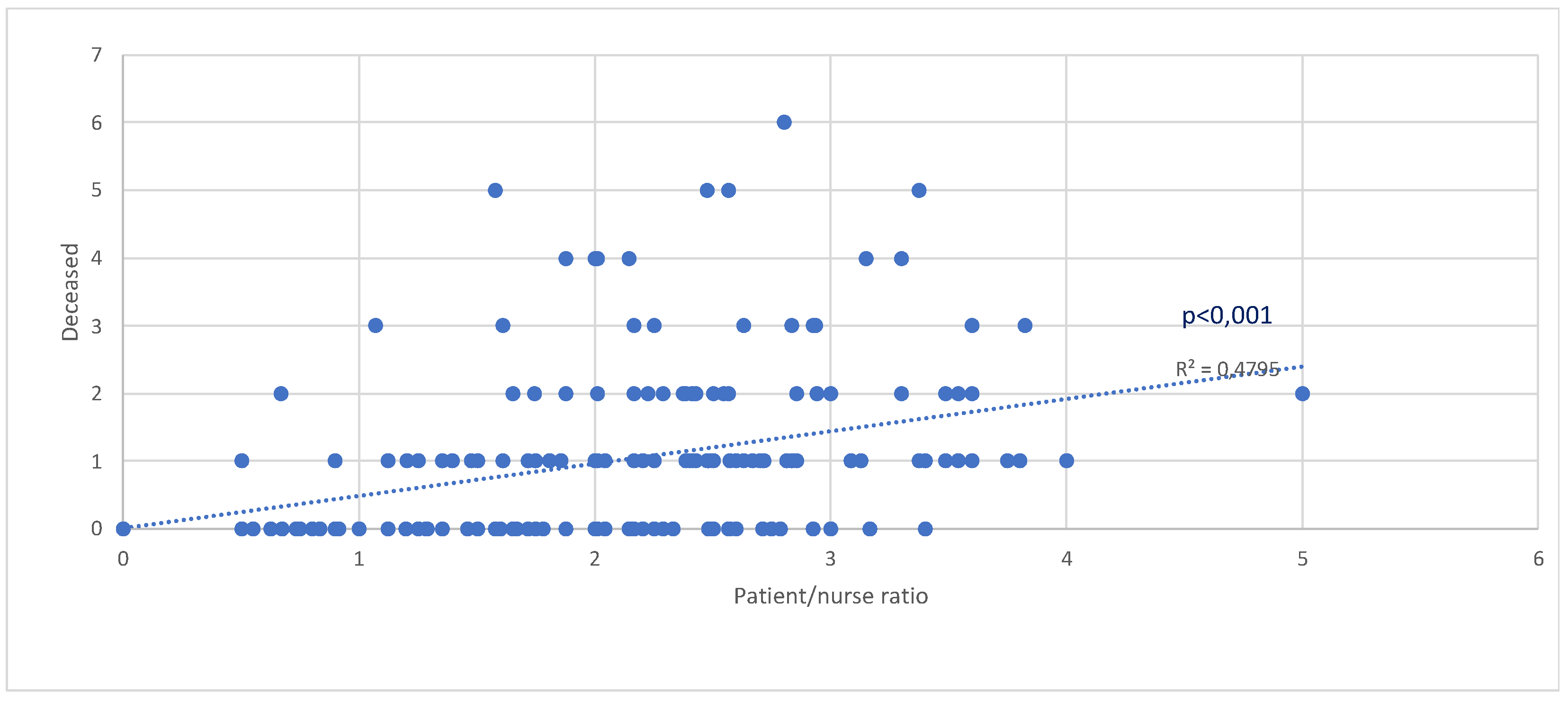
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Croatian Institute of Public Health. Available online: https://www.hzjz.hr/priopcenja-mediji/covid-19-priopcenje-prvog-slucaja/ (accessed on 19 September 2023).
- Global Change Data Lab. Available online: https://ourworldindata.org/explorers/coronavirus-data-explorer (accessed on 19 September 2023).
- Dimnjaković, J.; Capak, K.; Pavić, I.; Ivanko, P.; Pristaš, I.; Poljičanin, T. Peak Health Care Burden During the First Three COVID-19 Waves in the Republic of Croatia. Infektološki Glas. 2022, 41, 110–114. [Google Scholar] [CrossRef]
- Primmaz, S.; Le Terrier, C.; Suh, N.; Ventura, F.; Boroli, F.; Bendjelid, K.; Cereghetti, S.; Giraud, R.; Heidegger, C.; Pugin, D.; et al. Preparedness and Reorganization of Care for Coronavirus Disease 2019 Patients in a Swiss ICU: Characteristics and Outcomes of 129 Patients. Crit Care Explor. 2020, 2, e0173. [Google Scholar] [CrossRef] [PubMed]
- Džupová, O.; Moravec, M.; Bartoš, H.; Brestovanský, P.; Tencer, T.; Hyánek, T.; Beroušek, J.; Krupková, Z.; Mošna, F.; Vymazal, T.; et al. COVID-19 severe pneumonia: Prospective multicentre study on demands on intensive care capacities. Cent. Eur. J. Public Health 2021, 29, 3–8. [Google Scholar] [CrossRef] [PubMed]
- Jovandaric, M.Z.; Dokic, M.; Babovic, I.R.; Milicevic, S.; Dotlic, J.; Milosevic, B.; Culjic, M.; Andric, L.; Dimic, N.; Mitrovic, O.; et al. The Significance of COVID-19 Diseases in Lipid Metabolism Pregnancy Women and Newborns. Int. J. Mol. Sci. 2022, 23, 15098. [Google Scholar] [CrossRef] [PubMed]
- Kohler, M.; Stoewhas, A.-C.; Ayers, L.; Senn, O.; Bloch, K.E.; Russi, E.W.; Stradling, J.R. Effects of Continuous Positive Airway Pressure Therapy Withdrawal in Patients with Obstructive Sleep Apnea. Am. J. Respir. Crit. Care Med. 2011, 184, 1192–1199. [Google Scholar] [CrossRef] [PubMed]
- Demirovic, S.; Kalcina, L.L.; Dodig, I.P.; Pecotic, R.; Valic, M.; Ivkovic, N.; Dogas, Z. The COVID-19 Lockdown and CPAP Adherence: The More Vulnerable Ones Less Likely to Improve Adherence? Nat. Sci. Sleep 2021, 13, 1097–1108. [Google Scholar] [CrossRef] [PubMed]
- Grieco, D.L.; Maggiore, S.M.; Roca, O.; Spinelli, E.; Patel, B.K.; Thille, A.W.; Barbas, C.S.V.; de Acilu, M.G.; Cutuli, S.L.; Bongiovanni, F.; et al. Non-invasive ventilatory support and high-flow nasal oxygen as first-line treatment of acute hypoxemic respiratory failure and ARDS. Intensiv. Care Med. 2021, 47, 851–866. [Google Scholar] [CrossRef] [PubMed]
- Menzella, F.; Barbieri, C.; Fontana, M.; Scelfo, C.; Castagnetti, C.; Ghidoni, G.; Ruggiero, P.; Livrieri, F.; Piro, R.; Ghidorsi, L.; et al. Effectiveness of noninvasive ventilation in COVID-19 related-acute respiratory distress syndrome. Clin. Respir. J. 2021, 15, 779–787. [Google Scholar] [CrossRef] [PubMed]
- Pagano, A.; Porta, G.; Bosso, G.; Allegorico, E.; Serra, C.; Dello Vicario, F.; Minerva, V.; Russo, T.; Altruda, C.; Arbo, P.; et al. Non-invasive CPAP in mild and moderate ARDS secondary to SARS-CoV-2. Respir. Physiol. Neurobiol. 2020, 280, 103489. [Google Scholar] [CrossRef] [PubMed]
- Ferreyro, B.L.; Angriman, F.; Munshi, L.; Del Sorbo, L.; Ferguson, N.D.; Rochwerg, B.; Ryu, M.J.; Saskin, R.; Wunsch, H.; da Costa, B.R.; et al. Association of Noninvasive Oxygenation Strategies with All-Cause Mortality in Adults with Acute Hypoxemic Respiratory Failure: A Systematic Review and Meta-analysis. JAMA 2020, 324, 57–67. [Google Scholar] [CrossRef] [PubMed]
- Sullivan, Z.P.; Zazzeron, L.; Berra, L.; Hess, D.R.; Bittner, E.A.; Chang, M.G. Noninvasive respiratory support for COVID-19 patients: When, for whom, and how? J. Intensiv. Care 2022, 10, 3. [Google Scholar] [CrossRef] [PubMed]
- Perkins, G.D.; Ji, C.; Connolly, B.A.; Couper, K.; Lall, R.; Baillie, J.K.; Bradley, J.M.; Dark, P.; Dave, C.; De Soyza, A.; et al. Effect of Noninvasive Respiratory Strategies on Intubation or Mortality Among Patients with Acute Hypoxemic Respiratory Failure and COVID-19: The RECOVERY-RS Randomized Clinical Trial. JAMA 2022, 327, 546–558. [Google Scholar] [CrossRef] [PubMed]
- Cammarota, G.; Esposito, T.; Azzolina, D.; Cosentini, R.; Menzella, F.; Aliberti, S.; Coppadoro, A.; Bellani, G.; Foti, G.; Grasselli, G.; et al. Noninvasive respiratory support outside the intensive care unit for acute respiratory failure related to coronavirus-19 disease: A systematic review and meta-analysis. Crit. Care 2021, 25, 268. [Google Scholar] [CrossRef]
- Duca, A.; Memaj, I.; Zanardi, F.; Preti, C.; Alesi, A.; Della Bella, L.; Ghezzi, E.; Di Marco, F.; Lorini, F.L.; Venturelli, S.; et al. Severity of respiratory failure and outcome of patients needing a ventilatory support in the Emergency Department during Italian novel coronavirus SARS-CoV2 outbreak: Preliminary data on the role of Helmet CPAP and Non-Invasive Positive Pressure Ventilation. EClinicalMedicine 2020, 24, 100419. [Google Scholar] [CrossRef]
- Bignami, E.; Bellini, V.; Maspero, G.; Pifferi, B.; Fortunati Rossi, L.; Ticinesi, A.; Craca, M.; Meschi, T.; Baciarello, M. COVID-19 respiratory support outside the ICU’s doors. An observational study for a new operative strategy. Acta Biomed. 2021, 92, e2021365. [Google Scholar] [CrossRef]
- Boscolo, A.; Pasin, L.; Sella, N.; Pretto, C.; Tocco, M.; Tamburini, E.; Rosi, P.; Polati, E.; Donadello, K.; Gottin, L.; et al. Outcomes of COVID-19 patients intubated after failure of non-invasive ventilation: A multicenter observational study. Sci. Rep. 2021, 11, 17730. [Google Scholar] [CrossRef] [PubMed]
- Benes, J.; Jankowski, M.; Szułdrzynski, K.; Zahorec, R.; Lainscak, M.; Ruszkai, Z.; Podbregar, M.; Zatloukal, J.; Kletecka, J.; Kusza, K.; et al. SepsEast Registry indicates high mortality associated with COVID-19 caused acute respiratory failure in Central-Eastern European intensive care units. Sci. Rep. 2022, 12, 14906. [Google Scholar] [CrossRef] [PubMed]

| Group | Deceased % (N) | p |
|---|---|---|
| COVID 6/CRC (4th wave) (N = 102) | 29 (30) | <0.001 |
| CRC (2nd and 3rd wave) (N = 153) | 58 (89) |
| Group | Age Mean | Standard Deviation | p | Age Mean Deceased | Standard Deviation Deceased | p |
|---|---|---|---|---|---|---|
| COVID 6/CRC (4th wave) (N = 102) | 66.7 | 13.65 | 0.776 | 75.7 | 9.95 | 0.067 |
| CRC (2nd and 3rd wave) (N = 153) | 67.2 | 13.42 | 71.4 | 11.19 |
| Group | Female % (N) | Male % (N) | p | Female Deceased % (N) | Male Deceased % (N) | p |
|---|---|---|---|---|---|---|
| COVID 6/CRC (4th wave) (N = 102) | 40 (41) | 60 (61) | 0.099 | 50 (15) | 50 (15) | 0.036 |
| CRC (2nd and 3rd wave) (N = 153) | 29 (45) | 71 (108) | 27 (24) | 73 (65) |
| Group | Diabetes Mellitus Deceased % (N) | p | Arterial Hypertension Deceased % (N) | p | Heart Disease Deceased % (N) | p |
|---|---|---|---|---|---|---|
| COVID 6/CRC (4th wave) (N = 102) | 40 (15) | 0.772 | 60 (18) | 0.133 | 47 (14) | 0.127 |
| CRC (2nd and 3rd wave) (N = 153) | 35 (24) | 76 (68) | 29 (26) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Brusić, J.; Grubešić, A.; Jarić, F.; Vučković, T.; Lekić, A.; Šustić, A.; Protić, A. Use of CPAP Ventilation in Non-ICU Wards May Influence Outcomes in Patients with Severe Respiratory COVID-19. Medicina 2024, 60, 582. https://doi.org/10.3390/medicina60040582
Brusić J, Grubešić A, Jarić F, Vučković T, Lekić A, Šustić A, Protić A. Use of CPAP Ventilation in Non-ICU Wards May Influence Outcomes in Patients with Severe Respiratory COVID-19. Medicina. 2024; 60(4):582. https://doi.org/10.3390/medicina60040582
Chicago/Turabian StyleBrusić, Josip, Aron Grubešić, Filip Jarić, Tin Vučković, Andrica Lekić, Alan Šustić, and Alen Protić. 2024. "Use of CPAP Ventilation in Non-ICU Wards May Influence Outcomes in Patients with Severe Respiratory COVID-19" Medicina 60, no. 4: 582. https://doi.org/10.3390/medicina60040582
APA StyleBrusić, J., Grubešić, A., Jarić, F., Vučković, T., Lekić, A., Šustić, A., & Protić, A. (2024). Use of CPAP Ventilation in Non-ICU Wards May Influence Outcomes in Patients with Severe Respiratory COVID-19. Medicina, 60(4), 582. https://doi.org/10.3390/medicina60040582






