Arthroscopic Medialization Partial Repair with Biologic Interposition Tuberoplasty for Large to Massive Irreparable Rotator Cuff Tear
Abstract
1. Introduction
2. Patients and Methods
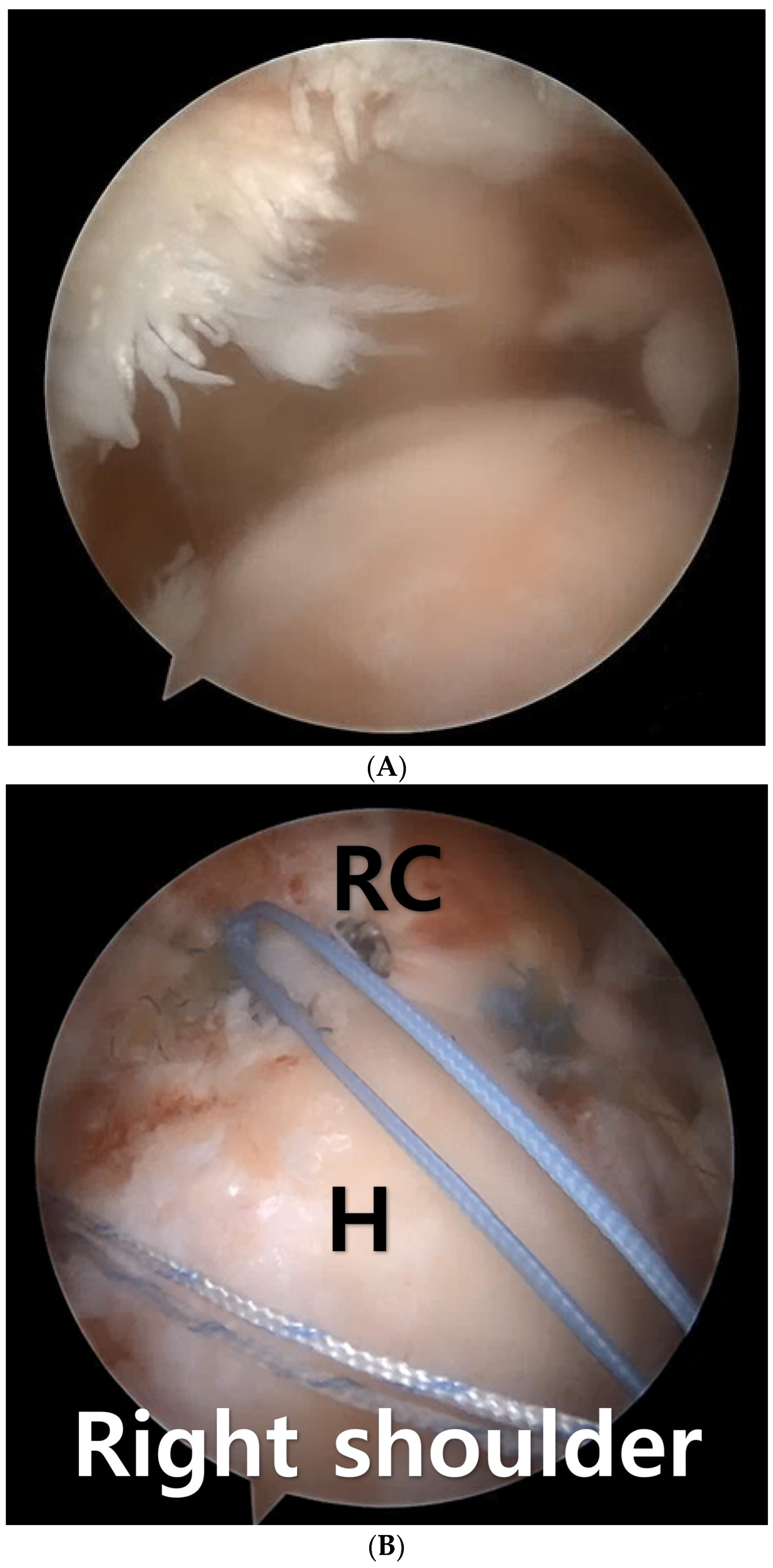
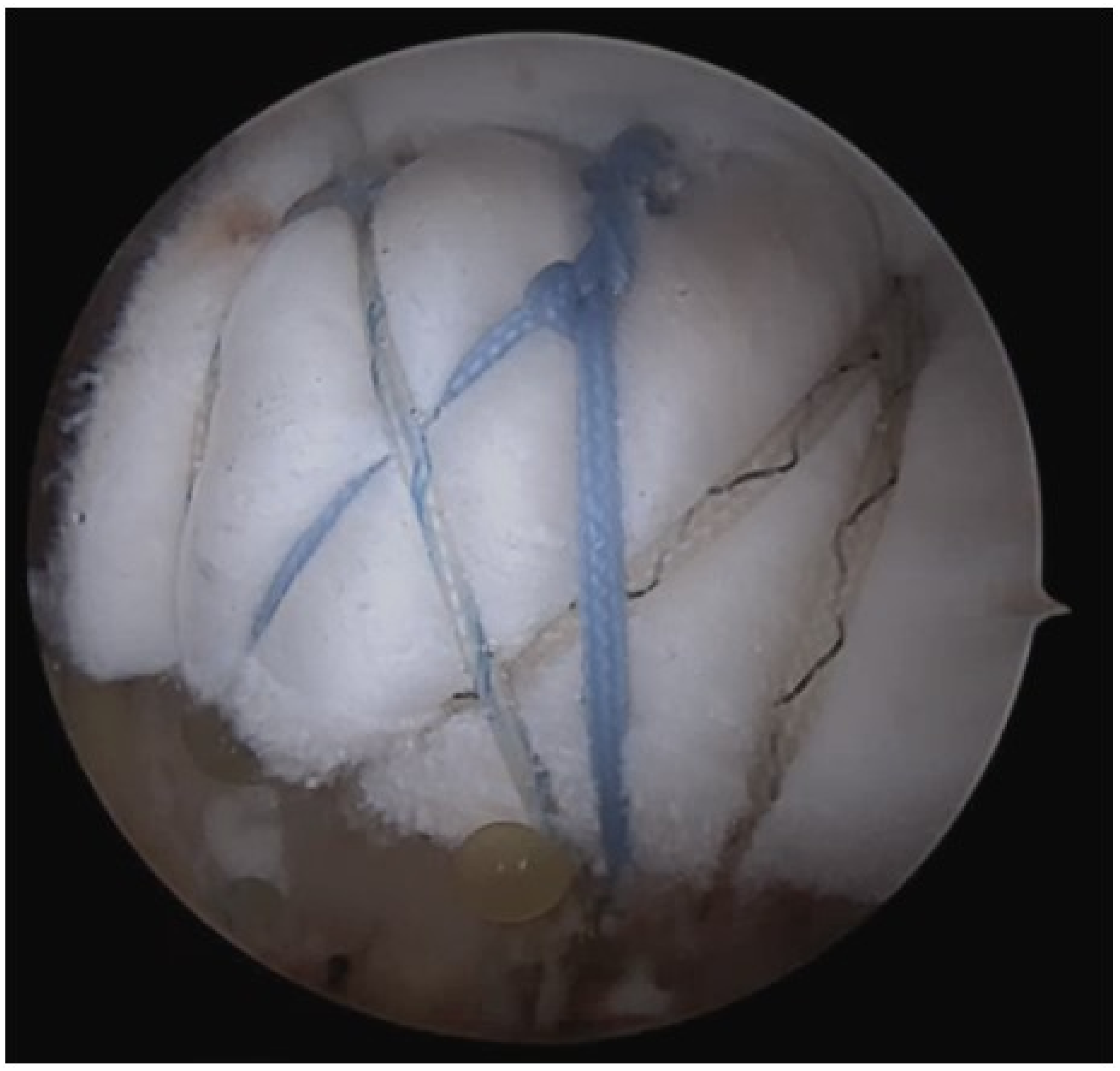
3. Surgical Technique
4. Postoperative Management
5. Result
Case
6. Discussion
7. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
References
- Tashjian, R.Z. Epidemiology, natural history, and indications for treatment of rotator cuff tears. Clin. Sports Med. 2012, 31, 589–604. [Google Scholar] [CrossRef]
- Mihata, T.; McGarry, M.H.; Pirolo, J.M.; Kinoshita, M.; Lee, T.Q. Superior capsule reconstruction to restore superior stability in irreparable rotator cuff tears: A biomechanical cadaveric study. Am. J. Sports Med. 2012, 40, 2248–2255. [Google Scholar] [CrossRef]
- Mirzayan, R.; Abboud, J.A.; Sethi, P.M.; Khan, A.Z.; Lohre, R.; Talamo, M.; Quintana, J.O.; Elhassan, B. Emerging Treatment Options for Massive Rotator Cuff Tears: Biologic Tuberoplasty, Balloon Arthroplasty, Anterior Cable Reconstruction, Lower Trapezius Transfer. Instr. Course Lect. 2023, 72, 223–238. [Google Scholar]
- Seo, J.B.; Kwak, K.Y.; Park, B.; Yoo, J.S. Anterior cable reconstruction using the proximal biceps tendon for reinforcement of arthroscopic rotator cuff repair prevent retear and increase acromiohumeral distance. J. Orthop. 2021, 23, 246–249. [Google Scholar] [CrossRef]
- Yoo, J.C.; Ahn, J.H.; Koh, K.H.; Lim, K.S. Rotator cuff integrity after arthroscopic repair for large tears with less-than-optimal footprint coverage. Arthroscopy 2009, 25, 1093–1100. [Google Scholar] [CrossRef] [PubMed]
- Burkhart, S.S.; Nottage, W.M.; Ogilvie-Harris, D.J.; Kohn, H.S.; Pachelli, A. Partial repair of irreparable rotator cuff tears. Arthroscopy 1994, 10, 363–370. [Google Scholar] [CrossRef] [PubMed]
- Kim, S.J.; Lee, I.S.; Kim, S.H.; Lee, W.Y.; Chun, Y.M. Arthroscopic partial repair of irreparable large to massive rotator cuff tears. Arthroscopy 2012, 28, 761–768. [Google Scholar] [CrossRef] [PubMed]
- Hyde, Z.B.; McMurtrie, J.T.; Lee, S.R.; Murali, S.; Hargreaves, M.D.; Ponce, B.A.; Brabston, E.W.; Momaya, A.M. Partial rotator cuff repair versus debridement for irreparable rotator cuff tears: A systematic review. J. Orthop. 2024, 49, 167–171. [Google Scholar] [CrossRef] [PubMed]
- Lee, K.W.; Lee, G.S.; Yang, D.S.; Park, S.H.; Chun, Y.S.; Choy, W.S. Clinical Outcome of Arthroscopic Partial Repair of Large to Massive Posterosuperior Rotator Cuff Tears: Medialization of the Attachment Site of the Rotator Cuff Tendon. Clin. Orthop. Surg. 2020, 12, 353–363. [Google Scholar] [CrossRef] [PubMed]
- Jordan, R.W.; Sharma, N.; Daggett, M.; Saithna, A. The role of Superior Capsule Reconstruction in the irreparable rotator cuff tear—A systematic review. Orthop. Traumatol. Surg. Res. 2019, 105, 1535–1542. [Google Scholar] [CrossRef]
- Sommer, M.C.; Wagner, E.; Zhu, S.; McRae, S.; MacDonald, P.B.; Ogborn, D.; Woodmass, J.M. Complications of Superior Capsule Reconstruction for the Treatment of Functionally Irreparable Rotator Cuff Tears: A Systematic Review. Arthroscopy 2021, 37, 2960–2972. [Google Scholar] [CrossRef]
- Denard, P.J.; Brady, P.C.; Adams, C.R.; Tokish, J.M.; Burkhart, S.S. Preliminary Results of Arthroscopic Superior Capsule Reconstruction with Dermal Allograft. Arthroscopy 2018, 34, 93–99. [Google Scholar] [CrossRef]
- Shin, S.J.; Lee, S.; Hwang, J.Y.; Lee, W.; Koh, K.H. Superior Capsular Reconstruction Using Acellular Dermal Allograft Combined with Remaining Rotator Cuff Augmentation Improved Shoulder Pain and Function at 1 Year after the Surgery. Arthroscopy 2022, 38, 1089–1098. [Google Scholar] [CrossRef] [PubMed]
- Mirzayan, R.; Bouz, G. Biologic Tuberoplasty With an Acellular Dermal Allograft for Massive Rotator Cuff Tears. Arthrosc. Tech. 2021, 10, e1743–e1749. [Google Scholar] [CrossRef] [PubMed]
- Mirzayan, R.; Stone, M.A.; Batech, M.; Acevedo, D.C.; Singh, A. Failed Dermal Allograft Procedures for Irreparable Rotator Cuff Tears Can Still Improve Pain and Function: The “Biologic Tuberoplasty Effect”. Orthop. J. Sports Med. 2019, 7, 2325967119863432. [Google Scholar] [CrossRef] [PubMed]
- Brolin, T.J.; Updegrove, G.F.; Horneff, J.G. Classifications in Brief: Hamada Classification of Massive Rotator Cuff Tears. Clin. Orthop. Relat. Res. 2017, 475, 2819–2823. [Google Scholar] [CrossRef] [PubMed]
- Seo, J.B.; Jung, J.W.; Yoo, J.S. Combination of arthroscopic biologic tuberoplasty and bursal acromial reconstruction. J. Orthop. 2024, 51, 1–6. [Google Scholar] [CrossRef] [PubMed]
- Lafosse, L.; Jost, B.; Reiland, Y.; Audebert, S.; Toussaint, B.; Gobezie, R. Structural integrity and clinical outcomes after arthroscopic repair of isolated subscapularis tears. J. Bone Jt. Surg. Am. 2007, 89, 1184–1193. [Google Scholar] [CrossRef]
- Adams, C.R.; DeMartino, A.M.; Rego, G.; Denard, P.J.; Burkhart, S.S. The Rotator Cuff and the Superior Capsule: Why We Need Both. Arthroscopy 2016, 32, 2628–2637. [Google Scholar] [CrossRef]
- Lo, I.K.; Burkhart, S.S. Current concepts in arthroscopic rotator cuff repair. Am. J. Sports Med. 2003, 31, 308–324. [Google Scholar] [CrossRef]
- Burkhart, S.S.; Esch, J.C.; Jolson, R.S. The rotator crescent and rotator cable: An anatomic description of the shoulder’s “suspension bridge”. Arthroscopy 1993, 9, 611–616. [Google Scholar] [CrossRef]
- Kim, H.M.; Dahiya, N.; Teefey, S.A.; Keener, J.D.; Galatz, L.M.; Yamaguchi, K. Relationship of tear size and location to fatty degeneration of the rotator cuff. J. Bone Jt. Surg. Am. 2010, 92, 829–839. [Google Scholar] [CrossRef]
- Namdari, S.; Donegan, R.P.; Dahiya, N.; Galatz, L.M.; Yamaguchi, K.; Keener, J.D. Characteristics of small to medium-sized rotator cuff tears with and without disruption of the anterior supraspinatus tendon. J. Shoulder Elbow Surg. 2014, 23, 20–27. [Google Scholar] [CrossRef] [PubMed]
- Kim, J.H.; Lee, H.J.; Park, T.Y.; Lee, J.U.; Kim, Y.S. Preliminary Outcomes of Arthroscopic Biceps Rerouting for the Treatment of Large to Massive Rotator Cuff Tears. J. Shoulder Elbow Surg. 2020, 30, 1384–1392. [Google Scholar] [CrossRef]
- Park, S.R.; Sun, D.H.; Kim, J.; Lee, H.J.; Kim, J.B.; Kim, Y.S. Is augmentation with the long head of the biceps tendon helpful in arthroscopic treatment of irreparable rotator cuff tears? J. Shoulder Elbow Surg. 2018, 27, 1969–1977. [Google Scholar] [CrossRef] [PubMed]
- Elhassan, B.T.; Wagner, E.R.; Werthel, J.D. Outcome of lower trapezius transfer to reconstruct massive irreparable posterior-superior rotator cuff tear. J. Shoulder Elbow Surg. 2016, 25, 1346–1353. [Google Scholar] [CrossRef]
- Galatz, L.M.; Ball, C.M.; Teefey, S.A.; Middleton, W.D.; Yamaguchi, K. The outcome and repair integrity of completely arthroscopically repaired large and massive rotator cuff tears. J. Bone Jt. Surg. Am. 2004, 86, 219–224. [Google Scholar] [CrossRef] [PubMed]
- Davies, A.; Singh, P.; Reilly, P.; Sabharwal, S.; Malhas, A. Superior capsule reconstruction, partial cuff repair, graft interposition, arthroscopic debridement or balloon spacers for large and massive irreparable rotator cuff tears: A systematic review and meta-analysis. J. Orthop. Surg. Res. 2022, 17, 552. [Google Scholar] [CrossRef]
- Jeong, J.H.; Yoon, E.J.; Kim, B.S.; Ji, J.H. Biceps-incorporating rotator cuff repair with footprint medialization in large-to-massive rotator cuff tears. Knee Surg. Sports Traumatol. Arthrosc. 2022, 30, 2113–2122. [Google Scholar] [CrossRef]


| Medialization | SCR | BT | Medialization + BT | |
|---|---|---|---|---|
| Repair area | GT medial side | Glenoid~GT | GT | All |
| Exposure area | GT | None | GT medial side | None |
| Retear rate | High | Moderate | Low | Low |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Jung, J.-W.; Seo, J.-B.; Lee, J.-Y.; Yoo, J.-S. Arthroscopic Medialization Partial Repair with Biologic Interposition Tuberoplasty for Large to Massive Irreparable Rotator Cuff Tear. Medicina 2024, 60, 484. https://doi.org/10.3390/medicina60030484
Jung J-W, Seo J-B, Lee J-Y, Yoo J-S. Arthroscopic Medialization Partial Repair with Biologic Interposition Tuberoplasty for Large to Massive Irreparable Rotator Cuff Tear. Medicina. 2024; 60(3):484. https://doi.org/10.3390/medicina60030484
Chicago/Turabian StyleJung, Jae-Wook, Joong-Bae Seo, Jun-Yeul Lee, and Jae-Sung Yoo. 2024. "Arthroscopic Medialization Partial Repair with Biologic Interposition Tuberoplasty for Large to Massive Irreparable Rotator Cuff Tear" Medicina 60, no. 3: 484. https://doi.org/10.3390/medicina60030484
APA StyleJung, J.-W., Seo, J.-B., Lee, J.-Y., & Yoo, J.-S. (2024). Arthroscopic Medialization Partial Repair with Biologic Interposition Tuberoplasty for Large to Massive Irreparable Rotator Cuff Tear. Medicina, 60(3), 484. https://doi.org/10.3390/medicina60030484








