Short-Term Changes in Weather Conditions and the Risk of Acute Coronary Syndrome Hospitalization with and without ST-Segment Elevation: A Focus on Vulnerable Subgroups
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Population
2.2. Meteorological Data
2.3. Statistical Analysis
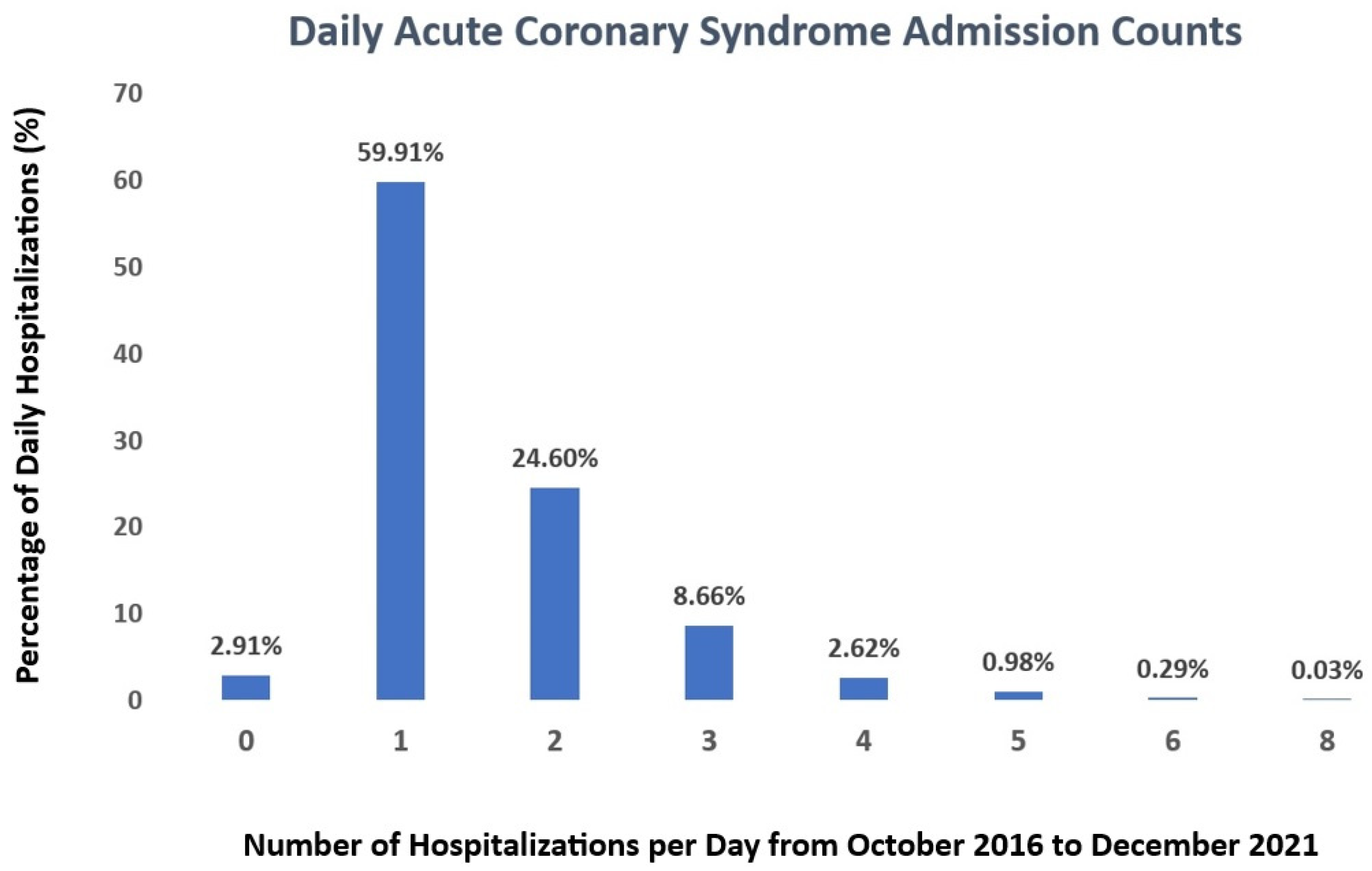
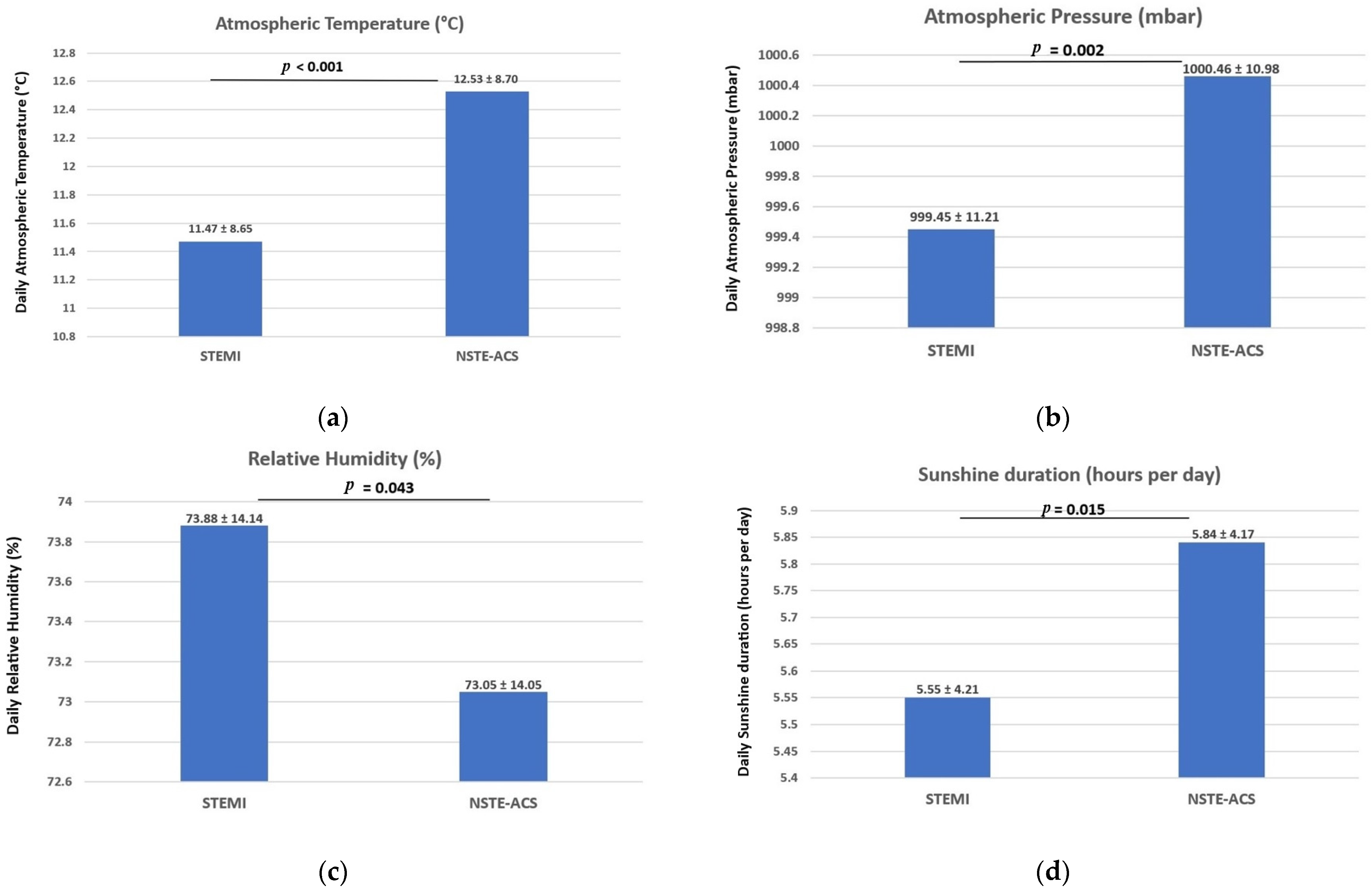
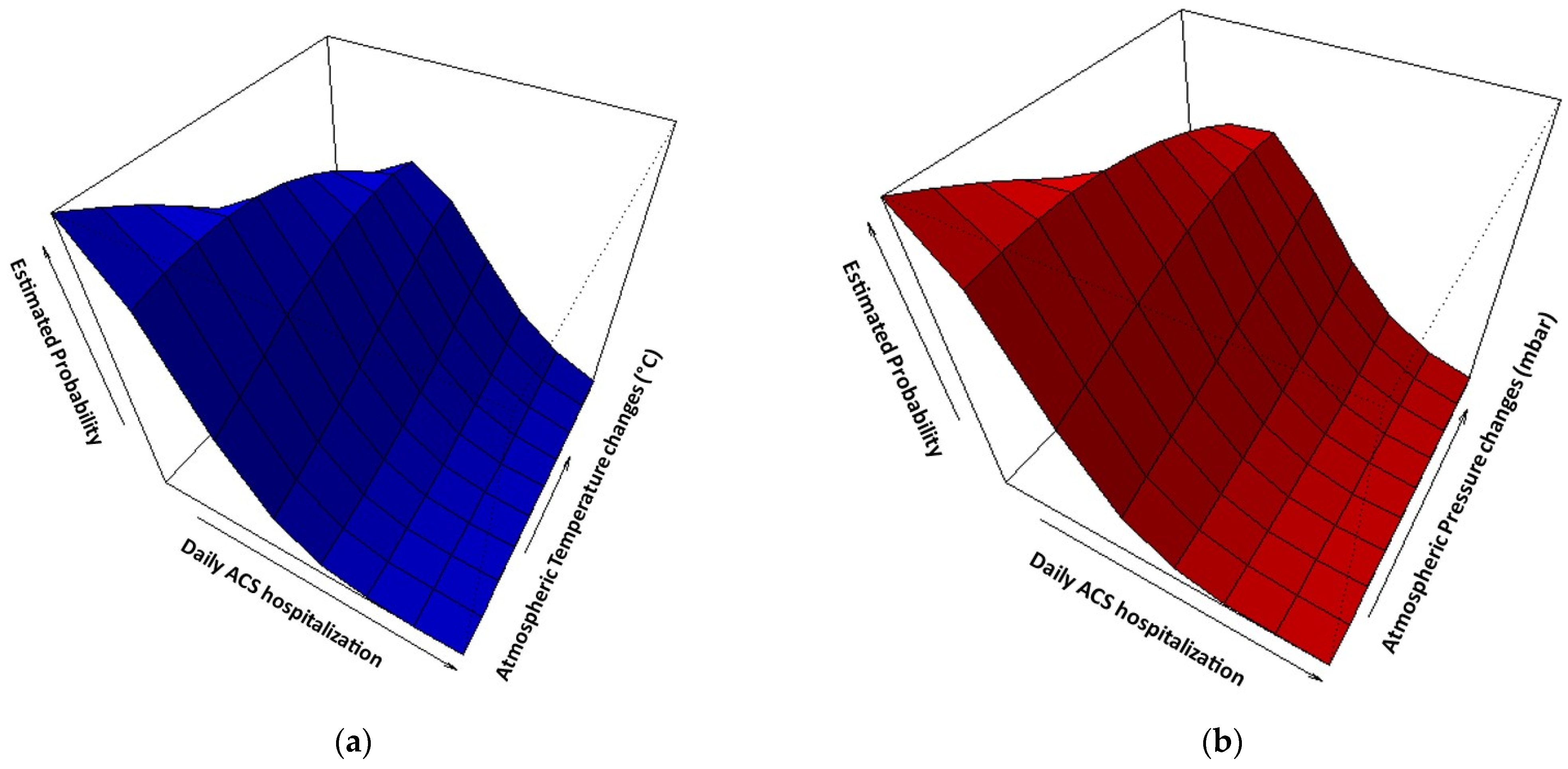
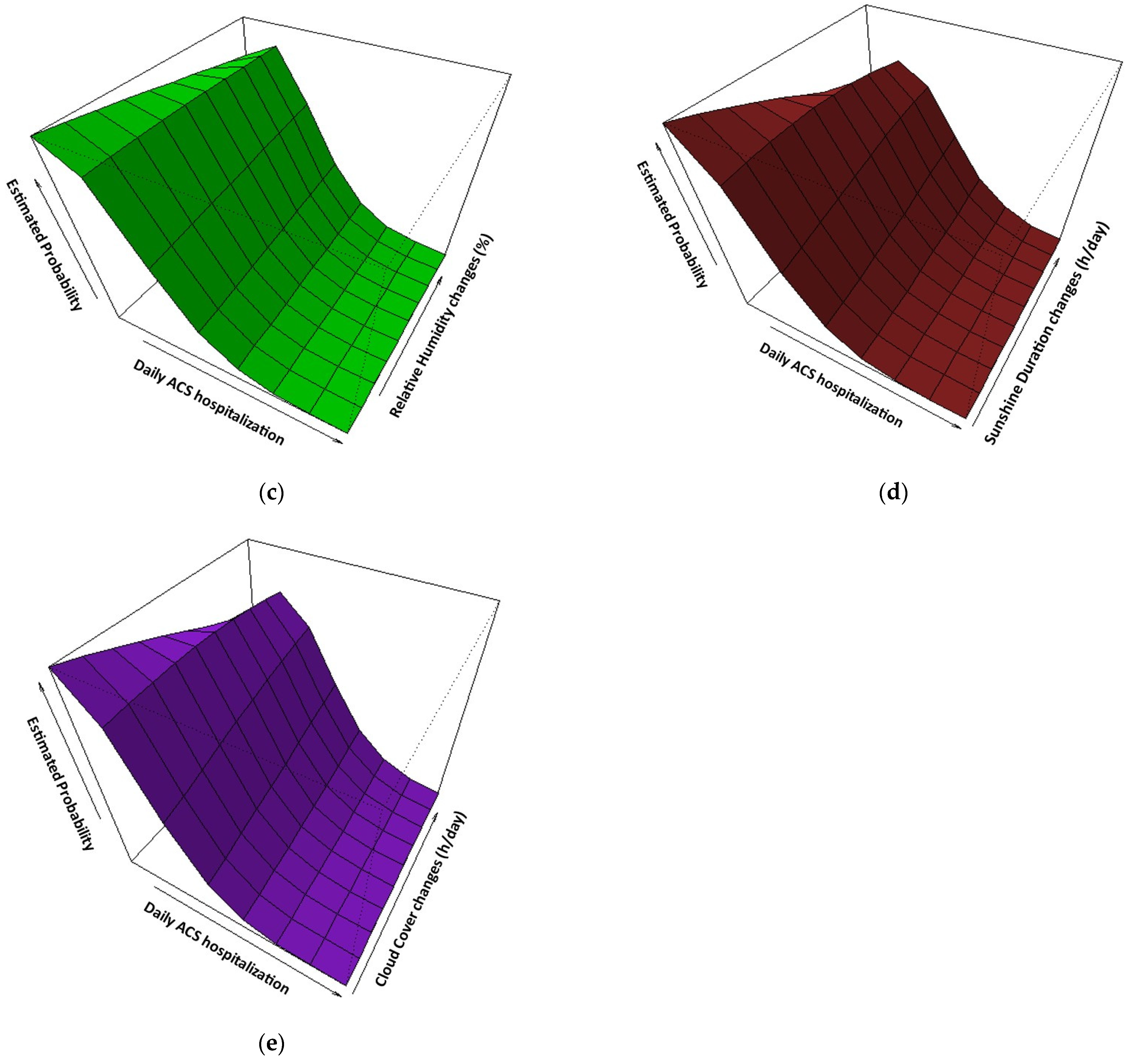
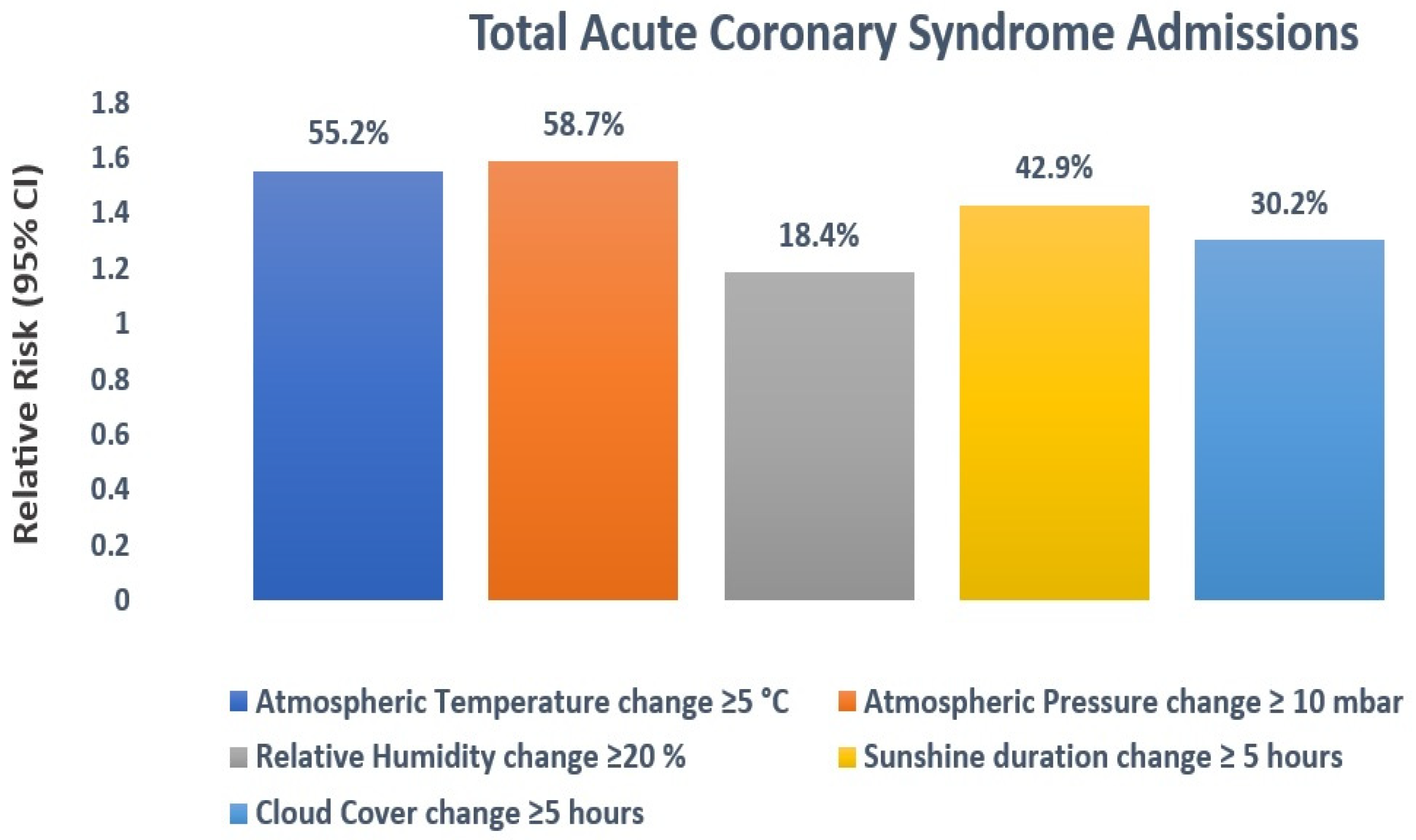
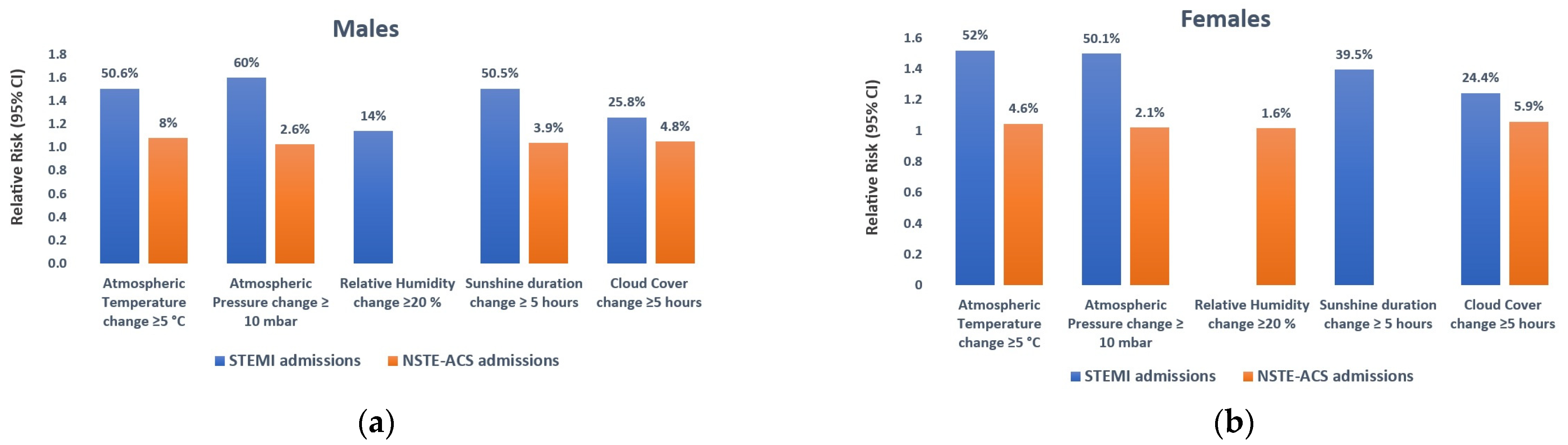
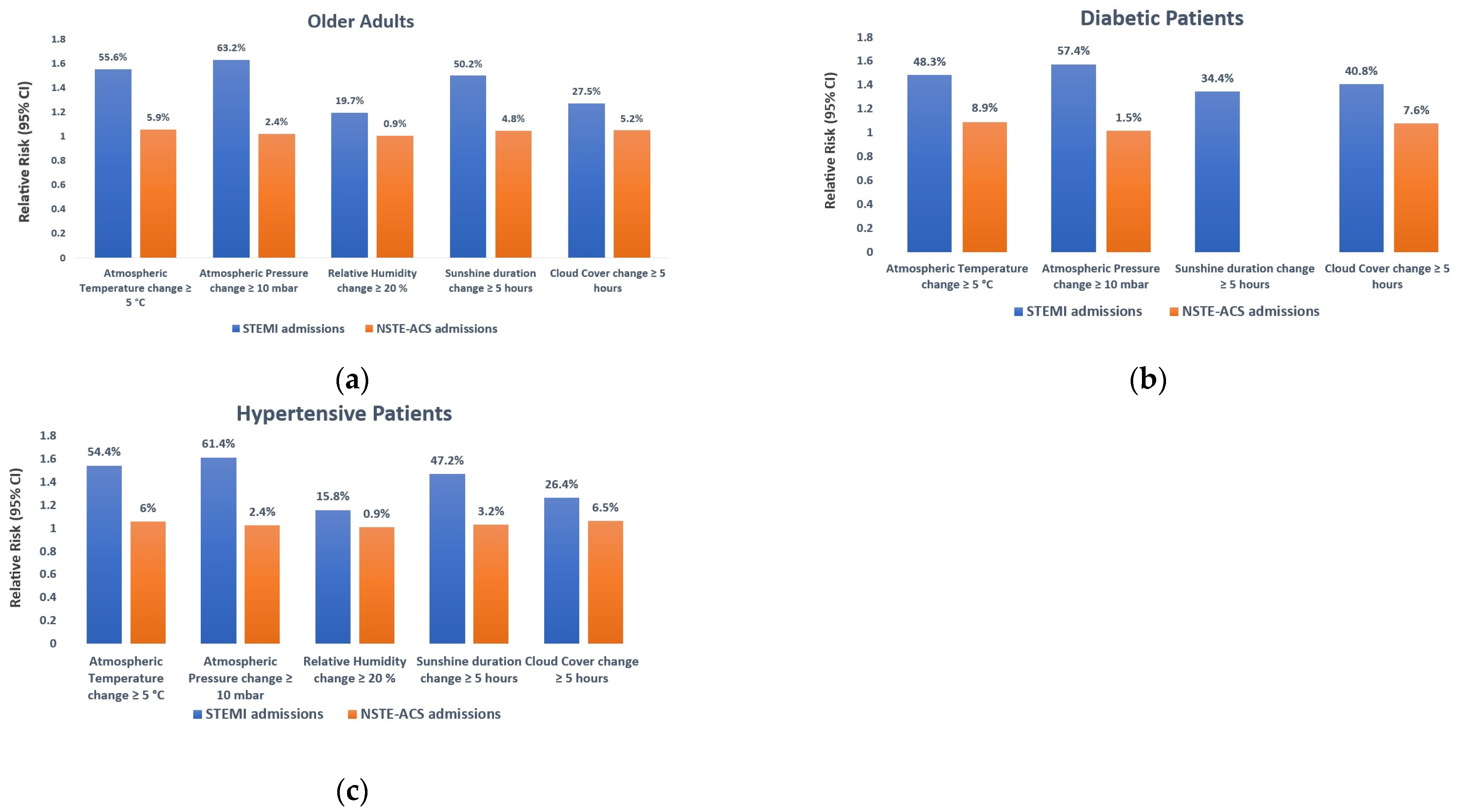
3. Results
4. Discussion
5. Conclusions
Study Limitations
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- World Health Organization. Global Status Report on Noncommunicable Diseases 2010. World Health Organization: Geneve, Switzerland. 2011. Available online: https://iris.who.int/bitstream/handle/10665/44579/9789240686458_eng.pdf (accessed on 29 October 2023).
- Bordejevic, D.A.; Caruntu, F.; Mornos, C.; Olariu, I.; Petrescu, L.; Tomescu, M.C.; Citu, I.; Mavrea, A.; Pescariu, S. Prognostic impact of blood pressure and heart rate at admission on in-hospital mortality after primary percutaneous intervention for acute myocardial infarction with ST-segment elevation in western Romania. Ther. Clin. Risk Manag. 2017, 13, 1061–1068. [Google Scholar] [CrossRef]
- Rosahn, P.D. Incidence of Coronary Thrombosis in Relation to Climate. J. Am. Med. Assoc. 1937, 109, 1294. [Google Scholar] [CrossRef]
- Bean, W.B.; Mills, C.A. Coronary occlusion, heart failure, and environmental temperatures. Am. Heart J. 1938, 16, 701–713. [Google Scholar] [CrossRef]
- Sharovsky, R.; César, L.A.M. Increase in mortality due to myocardial infarction in the Brazilian city of São Paulo during winter. Arq. Bras. Cardiol. 2002, 78, 106–109. [Google Scholar] [CrossRef] [PubMed]
- Arntz, H.-R.; Willich, S.; Schreiber, C.; Brüggemann, T.; Stern, R.; Schultheiß, H.-P. Diurnal, weekly and seasonal variation of sudden death. Population-based analysis of 24061 consecutive cases. Eur. Heart J. 2000, 21, 315–320. [Google Scholar] [CrossRef] [PubMed]
- Auliciems, A.; Skinner, J.L. Cardiovascular deaths and temperature in subtropical Brisbane. Int. J. Biometeorol. 1989, 33, 215–221. [Google Scholar] [CrossRef] [PubMed]
- Rumana, N.; Kita, Y.; Turin, T.C.; Murakami, Y.; Sugihara, H.; Morita, Y.; Tomioka, N.; Okayama, A.; Nakamura, Y.; Ueshima, H. Seasonal pattern of incidence and case fatality of acute myocardial infarction in a Japanese population (from the Takashima AMI Registry, 1988 to 2003). Am. J. Cardiol. 2008, 102, 1307–1311. [Google Scholar] [CrossRef] [PubMed]
- Vasconcelos, J.; Freire, E.; Almendra, R.; Silva, G.L.; Santana, P. The impact of winter cold weather on acute myocardial infarctions in Portugal. Environ. Pollut. 2013, 183, 14–18. [Google Scholar] [CrossRef] [PubMed]
- Danet, S.; Richard, F.; Montaye, M.; Beauchant, S.; Lemaire, B.; Graux, C.; Cottel, D.; Marécaux, N.; Amouyel, P. Unhealthy effects of atmospheric temperature and pressure on the occurrence of myocardial infarction and coronary deaths. A 10-year survey: The Lille-World Health Organization MONICA project (Monitoring trends and determinants in cardiovascular disease). Circ. 1999, 100, e1–e7. [Google Scholar] [CrossRef]
- Seretakis, D.; Lagiou, P.; Lipworth, L.; Signorello, L.B.; Rothman, K.J.; Trichopoulos, D. Changing seasonality of mortality from coronary heart disease. JAMA 1997, 278, 1012–1014. [Google Scholar] [CrossRef]
- Keatinge, W.R.; Coleshaw, S.R.; Cotter, F.; Mattock, M.; Murphy, M.; Chelliah, R. Increases in platelet and red cell counts, blood viscosity, and arterial pressure during mild surface cooling: Factors in mortality from coronary and cerebral thrombosis in winter. BMJ 1984, 289, 1405–1408. [Google Scholar] [CrossRef] [PubMed]
- Rus, A.-A.; Mornoş, C. The Impact of Meteorological Factors and Air Pollutants on Acute Coronary Syndrome. Curr. Cardiol. Rep. 2022, 24, 1337–1349. [Google Scholar] [CrossRef] [PubMed]
- Chen, K.; Breitner, S.; Wolf, K.; Hampel, R.; Meisinger, C.; Heier, M.; von Scheidt, W.; Kuch, B.; Peters, A.; Schneider, A.; et al. Temporal variations in the triggering of myocardial infarction by air temperature in Augsburg, Germany, 1987–2014. Eur. Heart J. 2019, 40, 1600–1608. [Google Scholar] [CrossRef]
- Akioka, H.; Yufu, K.; Teshima, Y.; Kawano, K.; Ishii, Y.; Abe, I.; Kondo, H.; Saito, S.; Fukui, A.; Okada, N.; et al. Seasonal variations of weather conditions on acute myocardial infarction onset: Oita AMI Registry. Heart Vessel. 2019, 34, 9–18. [Google Scholar] [CrossRef] [PubMed]
- Keatinge, W.R.; Coleshaw, S.R.; Easton, J.C.; Cotter, F.; Mattock, M.B.; Chelliah, R. Increased platelet and red cell counts, blood viscosity, and plasma cholesterol levels during heat stress, and mortality from coronary and cerebral thrombosis. Am. J. Med. 1986, 81, 795–800. [Google Scholar] [CrossRef]
- Dilaveris, P.; Synetos, A.; Giannopoulos, G.; Gialafos, E.; Pantazis, A.; Stefanadis, C. CLimate Impacts on Myocardial infarction deaths in the Athens TErritory: The CLIMATE study. Heart 2006, 92, 1747–1751. [Google Scholar] [CrossRef]
- Schwartz, J.; Samet, J.M.; Patz, J.A. Hospital admissions for heart disease: The effects of temperature and humidity. Epidemiology 2004, 15, 755–761. [Google Scholar] [CrossRef]
- Takagi, H.; Hari, Y.; Nakashima, K.; Kuno, T.; Ando, T.; for the ALICE (All-Literature Investigation of Cardiovascular Evidence). Group Wind and coronary artery disease. Eur. J. Prev. Cardiol. 2020, 27, 2259–2263. [Google Scholar] [CrossRef]
- Liang, W.-M.; Liu, W.-P.; Chou, S.-Y.; Kuo, H.-W. Ambient temperature and emergency room admissions for acute coronary syndrome in Taiwan. Int. J. Biometeorol. 2008, 52, 223–229. [Google Scholar] [CrossRef]
- National Meteorological Administration. Available online: https://www.meteoromania.ro/clima/clima-romaniei/ (accessed on 11 November 2023).
- National Institute of Statistics. Available online: https://insse.ro/cms/en/content/websites-regionalcounty-statistics-offices (accessed on 11 November 2023).
- Wang, H.; Matsumura, M.; Kakehashi, M.; Eboshida, A. Effects of atmospheric temperature and pressure on the occurrence of acute myocardial infarction in Hiroshima City, Japan. Hiroshima J. Med. Sci. 2006, 55, 45–51. [Google Scholar]
- Bhaskaran, K.; Hajat, S.; Haines, A.; Herrett, E.; Wilkinson, P.; Smeeth, L. Short term effects of temperature on risk of myocardial infarction in England and Wales: Time series regression analysis of the Myocardial Ischaemia National Audit Project (MINAP) registry. BMJ 2010, 341, c3823. [Google Scholar] [CrossRef] [PubMed]
- Didier, R.; Le Ven, F.; Ouchiha, M.; Nicol, P.P.; Auffret, V.; Oueslati, C.; Nasr, B.; Jobic, Y.; Noel, A.; Aidonidis, M.; et al. Analysis of weather exposure 7 days before occurrence of ST-segment elevation myocardial infarction. Arch. Cardiovasc. Dis. 2020, 113, 22–30. [Google Scholar] [CrossRef]
- Zhai, G.; Tian, Y.; Zhang, K.; Qi, J.; Chai, G. The effect of apparent temperature on hospital admissions for cardiovascular diseases in rural areas of Pingliang, China. J. Neurol. Sci. 2022, 29, 281–286. [Google Scholar] [CrossRef] [PubMed]
- Liu, X.; Kong, D.; Fu, J.; Zhang, Y.; Liu, Y.; Zhao, Y.; Lian, H.; Zhao, X.; Yang, J.; Fan, Z. Association between extreme temperature and acute myocardial infarction hospital admissions in Beijing, China: 2013–2016. PLoS ONE 2018, 13, e0204706. [Google Scholar] [CrossRef]
- Wang, B.; Chai, G.; Sha, Y.; Zha, Q.; Su, Y.; Gao, Y. Impact of ambient temperature on cardiovascular disease hospital admissions in farmers in China’s Western suburbs. Sci. Total. Environ. 2020, 761, 143254. [Google Scholar] [CrossRef]
- Chen, Y.; Chang, Z.; Zhao, Y.; Liu, Y.; Fu, J.; Liu, Y.; Liu, X.; Kong, D.; Han, Y.; Tang, S.; et al. Association of extreme precipitation with hospitalizations for acute myocardial infarction in Beijing, China: A time-series study. Front. Public Health 2022, 10, 1024816. [Google Scholar] [CrossRef]
- Ebi, K.L.; Exuzides, K.A.; Lau, E.; Kelsh, M.; Barnston, A. Weather changes associated with hospitalizations for cardiovascular diseases and stroke in California, 1983? Int. J. Biometeorol. 2004, 49, 48–58. [Google Scholar] [CrossRef]
- Boussoussou, N.; Boussoussou, M.; Merész, G.; Rakovics, M.; Entz, L.; Nemes, A. Complex effects of atmospheric parameters on acute cardiovascular diseases and major cardiovascular risk factors: Data from the CardiometeorologySM study. Sci. Rep. 2019, 9, 6358. [Google Scholar] [CrossRef]
- Mohammad, M.A.; Koul, S.; Rylance, R.; Fröbert, O.; Alfredsson, J.; Sahlén, A.; Witt, N.; Jernberg, T.; Muller, J.; Erlinge, D. Association of Weather With Day-to-Day Incidence of Myocardial Infarction. JAMA Cardiol. 2018, 3, 1081–1089. [Google Scholar] [CrossRef]
- Honda, T.; Fujimoto, K.; Miyao, Y. Influence of weather conditions on the frequent onset of acute myocardial infarction. J. Cardiol. 2016, 67, 42–50. [Google Scholar] [CrossRef] [PubMed]
- Li, N.; Ma, J.; Liu, F.; Zhang, Y.; Ma, P.; Jin, Y.; Zheng, Z.-J. Associations of apparent temperature with acute cardiac events and subtypes of acute coronary syndromes in Beijing, China. Sci. Rep. 2021, 11, 15229. [Google Scholar] [CrossRef] [PubMed]
- Versaci, F.; Biondi-Zoccai, G.; Giudici, A.D.; Mariano, E.; Trivisonno, A.; Sciarretta, S.; Valenti, V.; Peruzzi, M.; Cavarretta, E.; Frati, G.; et al. Climate changes and ST-elevation myocardial infarction treated with primary percutaneous coronary angioplasty. Int. J. Cardiol. 2019, 294, 1–5. [Google Scholar] [CrossRef] [PubMed]
- Goerre, S.; Egli, C.; Gerber, S.; Defila, C.; Minder, C.; Richner, H.; Meier, B. Impact of weather and climate on the incidence of acute coronary syndromes. Int. J. Cardiol. 2007, 118, 36–40. [Google Scholar] [CrossRef]
- Wijnbergen, I.; Veer, M.V.; Pijls, N.H.J.; Tijssen, J. Circadian and weekly variation and the influence of environmental variables in acute myocardial infarction. Neth. Heart J. 2012, 20, 354–359. [Google Scholar] [CrossRef]
- Abrignani, M.; Corrao, S.; Biondo, G.; Renda, N.; Braschi, A.; Novo, G.; Di Girolamo, A.; Braschi, G.; Novo, S. Influence of climatic variables on acute myocardial infarction hospital admissions. Int. J. Cardiol. 2009, 137, 123–129. [Google Scholar] [CrossRef]
- Guo, S.; Niu, Y.; Cheng, Y.; Chen, R.; Kan, J.; Kan, H.; Li, X.; Li, J.; Cao, J. Association between ambient temperature and daily emergency hospitalizations for acute coronary syndrome in Yancheng, China. Environ. Sci. Pollut. Res. 2020, 27, 3885–3891. [Google Scholar] [CrossRef] [PubMed]
- Panagiotakos, D.B.; Chrysohoou, C.; Pitsavos, C.; Nastos, P.; Anadiotis, A.; Tentolouris, C.; Stefanadis, C.; Toutouzas, P.; Paliatsos, A. Climatological variations in daily hospital admissions for acute coronary syndromes. Int. J. Cardiol. 2004, 94, 229–233. [Google Scholar] [CrossRef]
- Lee, J.H.; Chae, S.C.; Yang, D.H.; Park, H.S.; Cho, Y.; Jun, J.-E.; Park, W.-H.; Kam, S.; Lee, W.K.; Kim, Y.J.; et al. Influence of weather on daily hospital admissions for acute myocardial infarction (from the Korea Acute Myocardial Infarction Registry). Int. J. Cardiol. 2010, 144, 16–21. [Google Scholar] [CrossRef]
- Chang, C.L.; Shipley, M.; Marmot, M.; Poulter, N. Lower ambient temperature was associated with an increased risk of hospitalization for stroke and acute myocardial infarction in young women. J. Clin. Epidemiol. 2004, 57, 749–757. [Google Scholar] [CrossRef]
- Amiya, S.; Nuruki, N.; Tanaka, Y.; Tofuku, K.; Fukuoka, Y.; Sata, N.; Kashima, K.; Tsubouchi, H. Relationship between weather and onset of acute myocardial infarction: Can days of frequent onset be predicted? J. Cardiol. 2009, 54, 231–237. [Google Scholar] [CrossRef]
- Nia, H.S.; Chan, Y.H.; Froelicher, E.S.; Sharif, S.P.; Yaghoobzadeh, A.; Jafari, A.; Goudarzian, A.H.; Pourkia, R.; Haghdoost, A.A.; Arefinia, F.; et al. Weather fluctuations: Predictive factors in the prevalence of acute coronary syndrome. Health Promot. Perspect. 2019, 9, 123–130. [Google Scholar] [CrossRef]
- Radišauskas, R.; Bernotienė, G.; Bacevičienė, M.; Ustinavičienė, R.; Kirvaitienė, J.; Krančiukaitė-Butylkinienė, D. Trends of myocardial infarction morbidity and its associations with weather conditions. Medicina 2014, 50, 182–189. [Google Scholar] [CrossRef] [PubMed]
- Aylin, P.; Morris, S.; Wakefield, J.; Grossinho, A.; Jarup, L.; Elliott, P. Temperature, housing, deprivation and their relationship to excess winter mortality in Great Britain, 1986–1996. Leuk. Res. 2001, 30, 1100–1108. [Google Scholar] [CrossRef] [PubMed]
- Yamaji, K.; Kohsaka, S.; Morimoto, T.; Fujii, K.; Amano, T.; Uemura, S.; Akasaka, T.; Kadota, K.; Nakamura, M.; Kimura, T. Relation of ST-Segment Elevation Myocardial Infarction to Daily Ambient Temperature and Air Pollutant Levels in a Japanese Nationwide Percutaneous Coronary Intervention Registry. Am. J. Cardiol. 2017, 119, 872–880. [Google Scholar] [CrossRef]
| ACS (n = 5300) | |
|---|---|
| Age (years) | 62.1 ± 11.5 |
| Gender | |
| (male) | 3827 (72.2%) |
| (female) | 1473 (27.8%) |
| Body mass index (kg/m2) | 28.7 ± 5.1 |
| Cardiovascular risk factors | |
| Smoking | 2104 (39.7%) |
| Diabetes mellitus | 1427 (26.9%) |
| Arterial hypertension | 3826 (72.2%) |
| Hypercholesterolemia | 1978 (37.3%) |
| Family History | 188 (3.5%) |
| Clinical parameters at admission | |
| SBP (mmHg) | 138.4 ± 23.6 |
| DBP (mmHg) | 81.5 ± 14.1 |
| HR (bpm) | 77.4 ± 21.0 |
| Coronary angiography | |
| Single-vessel lesion | 2164 (40.8%) |
| Two-vessel lesion | 1702 (32.1%) |
| Three-vessel lesion | 1434 (27.1%) |
| LVEF (%) | 43.7 ± 7.9 |
| Type of treatment | |
| Conservative | 484 (9.1%) |
| Balloon angioplasty | 94 (1.8%) |
| Angioplasty and stent placement | 4537 (85.6%) |
| CABG | 185 (3.5%) |
| Total Days (n = 3475) | Mean ± SD | Minimum | Percentiles | Maximum | ||
|---|---|---|---|---|---|---|
| Variables | 25th | 50th | 75th | |||
| Atmospheric Temperature (°C) | 11.8 ± 8.7 | −15.4 | 4.9 | 11.2 | 19.1 | 31.5 |
| Atmospheric Pressure (mbar) | 999.8 ± 11.1 | 963.3 | 991.3 | 1001.0 | 1007.3 | 1033.9 |
| Relative Humidity (%) | 73.6 ± 14.1 | 32 | 63 | 74 | 85 | 100 |
| Wind Speed (m/s) | 1.9 ± 1.0 | 0.3 | 1.2 | 1.6 | 2.3 | 8.7 |
| Precipitation (mm/24 h) | 1.7 ± 4.4 | 0 | 0 | 0 | 0.9 | 61.2 |
| Sunshine duration (hours per day) | 5.7 ± 4.2 | 0 | 1.4 | 6.0 | 9.3 | 14.4 |
| Cloud Cover (hours per day) | 5.4 ± 3.3 | 0 | 2.5 | 5.5 | 8.5 | 10 |
| Variable | Relative Risk | 95% CI | p-Value |
|---|---|---|---|
| Atmospheric Temperature (°C) | 1.059 | 1.048–1.070 | <0.001 |
| Atmospheric Pressure (mbar) | 1.024 | 1.019–1.028 | <0.001 |
| Relative Humidity (%) | 1.005 | 1.001–1.008 | 0.012 |
| Wind Speed (m/s) | 1.014 | 0.983–1.045 | 0.394 |
| Precipitation (mm/24 h) | 1.004 | 0.999–1.008 | 0.112 |
| Sunshine Duration (hours per day) | 1.047 | 1.032–1.062 | <0.001 |
| Cloud Cover (hours per day) | 1.039 | 1.023–1.056 | <0.001 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Rus, A.-A.; Lazăr, M.-A.; Negrea, R.; Cozlac, A.-R.; Văcărescu, C.; Şoşdean, R.; Luca, S.-A.; Gaiţă, D.; Mornoş, C. Short-Term Changes in Weather Conditions and the Risk of Acute Coronary Syndrome Hospitalization with and without ST-Segment Elevation: A Focus on Vulnerable Subgroups. Medicina 2024, 60, 454. https://doi.org/10.3390/medicina60030454
Rus A-A, Lazăr M-A, Negrea R, Cozlac A-R, Văcărescu C, Şoşdean R, Luca S-A, Gaiţă D, Mornoş C. Short-Term Changes in Weather Conditions and the Risk of Acute Coronary Syndrome Hospitalization with and without ST-Segment Elevation: A Focus on Vulnerable Subgroups. Medicina. 2024; 60(3):454. https://doi.org/10.3390/medicina60030454
Chicago/Turabian StyleRus, Andreea-Alexandra, Mihai-Andrei Lazăr, Romeo Negrea, Alina-Ramona Cozlac, Cristina Văcărescu, Raluca Şoşdean, Silvia-Ana Luca, Dan Gaiţă, and Cristian Mornoş. 2024. "Short-Term Changes in Weather Conditions and the Risk of Acute Coronary Syndrome Hospitalization with and without ST-Segment Elevation: A Focus on Vulnerable Subgroups" Medicina 60, no. 3: 454. https://doi.org/10.3390/medicina60030454
APA StyleRus, A.-A., Lazăr, M.-A., Negrea, R., Cozlac, A.-R., Văcărescu, C., Şoşdean, R., Luca, S.-A., Gaiţă, D., & Mornoş, C. (2024). Short-Term Changes in Weather Conditions and the Risk of Acute Coronary Syndrome Hospitalization with and without ST-Segment Elevation: A Focus on Vulnerable Subgroups. Medicina, 60(3), 454. https://doi.org/10.3390/medicina60030454






