Comparative Analysis of COVID-19 Outcomes in Type 1 and Type 2 Diabetes: A Three-Year Retrospective Study
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design and Participants
2.2. Inclusion and Exclusion Criteria
2.3. Data Collection and Variables
2.4. Statistics
3. Results
Patients’ Background Analysis
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Kharroubi, A.T.; Darwish, H.M. Diabetes mellitus: The epidemic of the century. World J. Diabetes 2015, 6, 850–867. [Google Scholar] [CrossRef]
- Magliano, D.J.; Boyko, E.J. IDF Diabetes Atlas 10th Edition Scientific Committee. In IDF Diabetes Atlas [Internet], 10th ed.; International Diabetes Federation: Brussels, Belgium, 2021. Available online: https://www.ncbi.nlm.nih.gov/books/NBK581934/ (accessed on 25 October 2023).
- Allan, M.; Lièvre, M.; Laurenson-Schaefer, H.; de Barros, S.; Jinnai, Y.; Andrews, S.; Stricker, T.; Formigo, J.P.; Schultz, C.; Perrocheau, A.; et al. The World Health Organization COVID-19 surveillance database. Int. J. Equity Health 2023, 22 (Suppl. S3), 95, Erratum in Int. J. Equity Health 2023, 22, 95. [Google Scholar] [CrossRef]
- Nguyen, N.T.H.; Ou, T.-Y.; Huy, L.D.; Shih, C.-L.; Chang, Y.-M.; Phan, T.-P.; Huang, C.-C. A global analysis of COVID-19 infection fatality rate and its associated factors during the Delta and Omicron variant periods: An ecological study. Front. Public Health 2023, 11, 1145138. [Google Scholar] [CrossRef] [PubMed]
- Seiglie, J.; Platt, J.; Cromer, S.J.; Bunda, B.; Foulkes, A.S.; Bassett, I.V.; Hsu, J.; Meigs, J.B.; Leong, A.; Putman, M.S.; et al. Diabetes as a Risk Factor for Poor Early Outcomes in Patients Hospitalized With COVID-19. Diabetes Care 2020, 43, 2938–2944. [Google Scholar] [CrossRef] [PubMed]
- Pelle, M.C.; Zaffina, I.; Provenzano, M.; Moirano, G.; Arturi, F. COVID-19 and diabetes—Two giants colliding: From pathophysiology to management. Front. Endocrinol. 2022, 13, 974540. [Google Scholar] [CrossRef]
- Mantovani, A.; Byrne, C.D.; Zheng, M.-H.; Targher, G. Diabetes as a risk factor for greater COVID-19 severity and in-hospital death: A meta-analysis of observational studies. Nutr. Metab. Cardiovasc. Dis. 2020, 30, 1236–1248. [Google Scholar] [CrossRef]
- Khunti, K.; Valabhji, J.; Misra, S. Diabetes and the COVID-19 pandemic. Diabetologia 2023, 66, 255–266. [Google Scholar] [CrossRef]
- Zaccardi, F.; Webb, D.R.; Yates, T.; Davies, M.J. Pathophysiology of type 1 and type 2 diabetes mellitus: A 90-year perspective. Postgrad. Med. J. 2016, 92, 63–69. [Google Scholar] [CrossRef] [PubMed]
- Narasimhulu, C.A.; Singla, D.K. Mechanisms of COVID-19 pathogenesis in diabetes. Am. J. Physiol. Heart Circ. Physiol. 2022, 323, H403–H420. [Google Scholar] [CrossRef]
- Bedoya, J.P.P.; Muñoz, A.M.; Barengo, N.C.; Valencia, P.A.D. Type 1 and type 2 diabetes mellitus: Clinical outcomes due to COVID-19. Protocol of a systematic literature review. PLoS ONE 2022, 17, e0271851. [Google Scholar] [CrossRef]
- Simmons, K.M. Type 1 diabetes: A predictable disease. World J. Diabetes 2015, 6, 380–390. [Google Scholar] [CrossRef] [PubMed]
- Toren, E.; Burnette, K.S.; Banerjee, R.R.; Hunter, C.S.; Tse, H.M. Partners in Crime: Beta-Cells and Autoimmune Responses Complicit in Type 1 Diabetes Pathogenesis. Front. Immunol. 2021, 12, 756548. [Google Scholar] [CrossRef] [PubMed]
- Wondmkun, Y.T. Obesity, Insulin Resistance, and Type 2 Diabetes: Associations and Therapeutic Implications. Diabetes Metab. Syndr. Obes. 2020, 13, 3611–3616. [Google Scholar] [CrossRef] [PubMed]
- Olokoba, A.B.; Obateru, O.A.; Olokoba, L.B. Type 2 diabetes mellitus: A review of current trends. Oman Med. J. 2012, 27, 269–273. [Google Scholar] [CrossRef] [PubMed]
- Sutkowska, E.; Marciniak, D.M.; Sutkowska, K.; Biernat, K.; Mazurek, J.; Kuciel, N. The impact of lockdown caused by the COVID-19 pandemic on glycemic control in patients with diabetes. Endocrine 2022, 76, 273–281. [Google Scholar] [CrossRef] [PubMed]
- Khunti, K.; Aroda, V.R.; Aschner, P.; Chan, J.C.N.; Del Prato, S.; Hambling, C.E.; Harris, S.; Lamptey, R.; McKee, M.; Tandon, N.; et al. The impact of the COVID-19 pandemic on diabetes services: Planning for a global recovery. Lancet Diabetes Endocrinol. 2022, 10, 890–900. [Google Scholar] [CrossRef] [PubMed]
- Lim, S.; Bae, J.H.; Kwon, H.-S.; Nauck, M.A. COVID-19 and diabetes mellitus: From pathophysiology to clinical management. Nat. Rev. Endocrinol. 2021, 17, 11–30. [Google Scholar] [CrossRef]
- American Diabetes Association. Standards of Medical Care in Diabetes—2021 Abridged for Primary Care Providers. Clin. Diabetes 2021, 39, 14–43. [Google Scholar] [CrossRef]
- Cascella, M.; Rajnik, M.; Aleem, A.; Dulebohn, S.C.; Di Napoli, R. Features, Evaluation, and Treatment of Coronavirus (COVID-19) [Updated 2023 Aug 18]. In StatPearls [Internet]; StatPearls Publishing: Treasure Island, FL, USA, 2023. Available online: https://www.ncbi.nlm.nih.gov/books/NBK554776/ (accessed on 25 October 2023).
- Charlson, M.E.; Carrozzino, D.; Guidi, J.; Patierno, C. Charlson Comorbidity Index: A Critical Review of Clinimetric Properties. Psychother. Psychosom. 2022, 91, 8–35. [Google Scholar] [CrossRef]
- Zayed, N.E.; Abbas, A.; Lutfy, S.M. Criteria and potential predictors of severity in patients with COVID-19. Egypt. J. Bronchol. 2022, 16, 11. [Google Scholar] [CrossRef]
- Ssentongo, P.; Zhang, Y.; Witmer, L.; Chinchilli, V.M.; Ba, D.M. Association of COVID-19 with diabetes: A systematic review and meta-analysis. Sci. Rep. 2022, 12, 20191. [Google Scholar] [CrossRef] [PubMed]
- Tabrizi, F.M.; Rasmi, Y.; Hosseinzadeh, E.; Rezaei, S.; Balvardi, M.; Kouchari, M.R.; Ebrahimi, G. Diabetes is associated with increased mortality and disease severity in hospitalized patients with COVID-19. EXCLI J. 2021, 20, 444–453. [Google Scholar] [CrossRef]
- Barbosa, M.; Marques-Sá, J.; Carvalho, C.; Fernandes, V. Is elevated blood glucose at admission associated with poor outcomes in hospitalized COVID-19 patients? Arch. Endocrinol. Metab. 2023, 67, e000649. [Google Scholar] [CrossRef]
- Beshbishy, A.M.; Oti, V.B.; Hussein, D.E.; Rehan, I.F.; Adeyemi, O.S.; Rivero-Perez, N.; Zaragoza-Bastida, A.; Shah, M.A.; Abouelezz, K.; Hetta, H.F.; et al. Factors Behind the Higher COVID-19 Risk in Diabetes: A Critical Review. Front. Public Health 2021, 9, 591982. [Google Scholar] [CrossRef]
- Shafiee, A.; Athar, M.M.T.; Nassar, M.; Seighali, N.; Aminzade, D.; Fattahi, P.; Rahmannia, M.; Ahmadi, Z. Comparison of COVID-19 outcomes in patients with Type 1 and Type 2 diabetes: A systematic review and meta-analysis. Diabetes Metab. Syndr. Clin. Res. Rev. 2022, 16, 102512. [Google Scholar] [CrossRef] [PubMed]
- Edqvist, J.; Lundberg, C.; Andreasson, K.; Björck, L.; Dikaiou, P.; Ludvigsson, J.; Lind, M.; Adiels, M.; Rosengren, A. Severe COVID-19 Infection in Type 1 and Type 2 Diabetes During the First Three Waves in Sweden. Diabetes Care 2023, 46, 570–578. [Google Scholar] [CrossRef] [PubMed]
- Elith, J.; Leathwick, J.R.; Hastie, T. A working guide to boosted regression trees. J. Anim. Ecol. 2008, 77, 802–813. [Google Scholar] [CrossRef] [PubMed]
- Jennings, M.; Burova, M.; Hamilton, L.G.; Hunter, E.; Morden, C.; Pandya, D.; Beecham, R.; Moyses, H.; Saeed, K.; Afolabi, P.R.; et al. Body mass index and clinical outcome of severe COVID-19 patients with acute hypoxic respiratory failure: Unravelling the “obesity paradox” phenomenon. Clin. Nutr. ESPEN 2022, 51, 377–384. [Google Scholar] [CrossRef] [PubMed]
- Holman, N.; Knighton, P.; Kar, P.; O’Keefe, J.; Curley, M.; Weaver, A.; Barron, E.; Bakhai, C.; Khunti, K.; Wareham, N.J.; et al. Risk factors for COVID-19-related mortality in people with type 1 and type 2 diabetes in England: A population-based cohort study. Lancet Diabetes Endocrinol. 2020, 8, 823–833. [Google Scholar] [CrossRef] [PubMed]
- McGurnaghan, S.J.; Weir, A.; Bishop, J.; Kennedy, S.; Blackbourn, L.A.K.; McAllister, D.A.; Hutchinson, S.; Caparrotta, T.M.; Mellor, J.; Jeyam, A.; et al. Risks of and risk factors for COVID-19 disease in people with diabetes: A cohort study of the total population of Scotland. Lancet Diabetes Endocrinol. 2021, 9, 82–93. [Google Scholar] [CrossRef] [PubMed]
- Demeterco-Berggren, C.; Ebekozien, O.; Rompicherla, S.; Jacobsen, L.; Accacha, S.; Gallagher, M.P.; Alonso, G.T.; Seyoum, B.; Vendrame, F.; Haw, J.S.; et al. Age and Hospitalization Risk in People With Type 1 Diabetes and COVID-19: Data From the T1D Exchange Surveillance Study. J. Clin. Endocrinol. Metab. 2022, 107, 410–418. [Google Scholar] [CrossRef]
- Hamilton, K.; Stanton-Fay, S.H.; Chadwick, P.M.; Lorencatto, F.; de Zoysa, N.; Gianfrancesco, C.; Taylor, C.; Coates, E.; Breckenridge, J.P.; Cooke, D.; et al. Sustained type 1 diabetes self-management: Specifying the behaviours involved and their influences. Diabet. Med. 2021, 38, e14430. [Google Scholar] [CrossRef]
- Sen, S.; Chakraborty, R.; Kalita, P.; Pathak, M.P. Diabetes mellitus and COVID-19: Understanding the association in light of current evidence. World J. Clin. Cases 2021, 9, 8327–8339. [Google Scholar] [CrossRef] [PubMed]
- Patel, S.Y.; McCoy, R.G.; Barnett, M.L.; Shah, N.D.; Mehrotra, A. Diabetes Care and Glycemic Control During the COVID-19 Pandemic in the United States. JAMA Intern. Med. 2021, 181, 1412–1414. [Google Scholar] [CrossRef] [PubMed]
- Atwah, B.; Iqbal, M.S.; Kabrah, S.; Kabrah, A.; Alghamdi, S.; Tabassum, A.; Baghdadi, M.A.; Alzahrani, H. Susceptibility of Diabetic Patients to COVID-19 Infections: Clinico-Hematological and Complications Analysis. Vaccines 2023, 11, 561. [Google Scholar] [CrossRef] [PubMed]
| Variables | No Diabetes (n = 200) | T1D (n = 62) | T2D (n = 224) | p-Value | p-Value * |
|---|---|---|---|---|---|
| Age, years (mean ± SD) | 55.3 ± 12.5 | 53.6 ± 11.7 | 56.4 ± 13.1 | 0.281 | 0.129 |
| Gender, men | 118 (59.0%) | 35 (56.5%) | 121 (54.0%) | 0.586 | 0.733 |
| BMI (mean ± SD) | 25.8 ± 4.1 | 24.7 ± 5.0 | 26.0 ± 6.3 | 0.234 | 0.135 |
| Currently smoking | 58 (29.0%) | 20 (32.3%) | 68 (30.4%) | 0.878 | 0.774 |
| Alcohol use (frequent) | 19 (9.5%) | 4 (6.5%) | 12 (5.4%) | 0.249 | 0.739 |
| Place of origin (urban) | 126 (63.0%) | 40 (64.5%) | 144 (64.3%) | 0.955 | 0.973 |
| COVID-19 vaccinated | 52 (26.0%) | 20 (32.3%) | 68 (30.4%) | 0.498 | 0.774 |
| CCI > 2 | 46 (23.0%) | 17 (27.4%) | 56 (25.0%) | 0.756 | 0.698 |
| COVID-19 severity | <0.001 | 0.498 | |||
| Mild | 99 (49.5%) | 22 (35.5%) | 68 (30.4%) | ||
| Moderate | 71 (35.5%) | 24 (38.7%) | 81 (36.2%) | ||
| Severe | 30 (15.0%) | 16 (25.8%) | 75 (33.5%) | ||
| Duration of diabetes diagnosis, years (mean ± SD) | - | 10.9 ± 4.6 | 9.6 ± 5.1 | - | 0.071 |
| Diabetes-related complications | |||||
| Cardiovascular disease | - | 26 (41.9%) | 108 (48.2%) | - | 0.380 |
| Neuropathy | - | 19 (30.6%) | 81 (36.2%) | - | 0.420 |
| Kidney disease | - | 13 (21.0%) | 75 (33.5%) | - | 0.058 |
| Others | - | 9 (14.5%) | 36 (16.1%) | - | 0.766 |
| Hyperglycemia at admission | - | 20 (32.3%) | 116 (51.8%) | - | 0.006 |
| Insulin use | - | 62 (100%) | 38 (17.0%) | - | <0.001 |
| Dialysis users | - | 5 (8.1%) | 27 (12.1%) | - | 0.377 |
| ICU admissions | 34 (17.0%) | 14 (22.6%) | 71 (31.7%) | 0.002 | 0.164 |
| Mechanical ventilation | 36 (18.0%) | 18 (29.0%) | 79 (35.3%) | <0.001 | 0.358 |
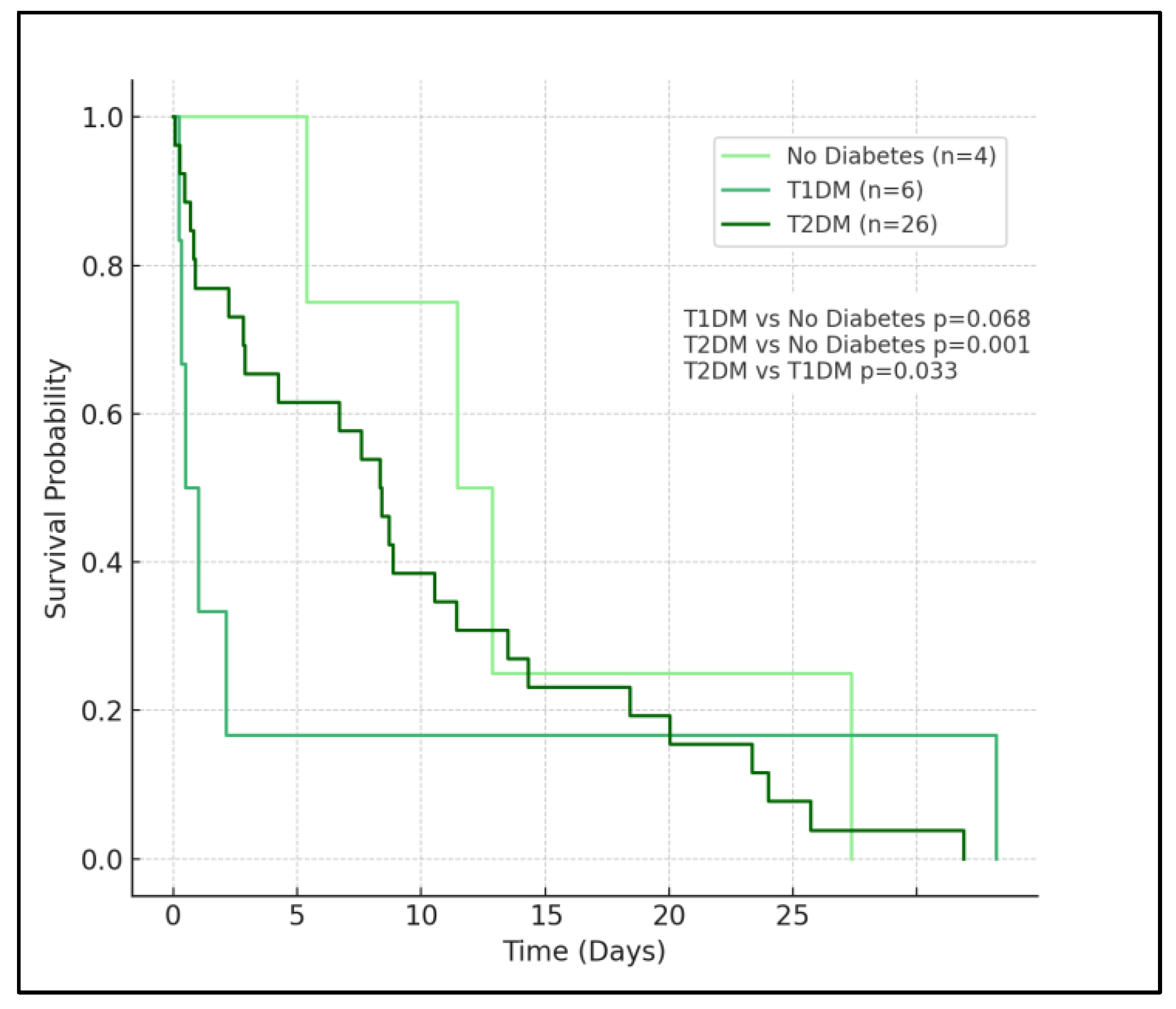
| Mortality | 7 (3.5%) | 5 (8.1%) | 26 (11.6%) | 0.008 | 0.427 |
| Variables | Normal Range | No Diabetes (n = 200) | T1D (n = 62) | T2D (n = 224) | p-Value | p-Value * |
|---|---|---|---|---|---|---|
| Blood Glucose (mg/dL) | 70–99 | 95.1 ± 15.2 | 164.8 ± 39.6 | 178.3 ± 34.7 | <0.001 | 0.009 |
| HbA1c (%) | 4.0–5.6 | 5.6 ± 0.5 | 7.7 ± 1.1 | 8.1 ± 1.4 | <0.001 | 0.038 |
| C-Reactive Protein (mg/L) | <5.0 | 15.2 ± 8.9 | 27.4 ± 13.8 | 38.2 ± 14.6 | <0.001 | <0.001 |
| D-Dimer (μg/mL) | <0.5 | 1.6 ± 1.2 | 2.8 ± 1.3 | 2.9 ± 2.0 | <0.001 | 0.798 |
| Oxygen Saturation (%) | 95–100 | 93.9 ± 10.8 | 91.7 ± 12.9 | 90.8 ± 13.7 | 0.037 | 0.643 |
| Creatinine (mg/dL) | 0.7–1.2 | 0.9 ± 0.4 | 1.2 ± 0.6 | 1.3 ± 0.9 | <0.001 | 0.410 |
| Lymphocyte Count (×109/L) | 1.0–3.0 | 3.4 ± 2.5 | 3.2 ± 2.6 | 3.1 ± 2.4 | 0.455 | 0.775 |
| WBC Count (×109/L) | 4.5–11.0 | 9.0 ± 6.6 | 10.5 ± 4.8 | 10.2 ± 5.0 | 0.052 | 0.673 |
| Variables | No Diabetes (n = 200) | T1D (n = 62) | T2D (n = 224) | p-Value | p-Value * |
|---|---|---|---|---|---|
| Length of hospital stay (days) | 7.2 ± 6.6 | 9.1 ± 5.8 | 11.6 ± 7.0 | <0.001 | 0.010 |
| Received antiviral treatment (%) | 156 (78.0%) | 51 (82.3%) | 192 (85.7%) | 0.117 | 0.501 |
| Received steroids (%) | 121 (60.5%) | 43 (69.4%) | 167 (74.6%) | 0.008 | 0.412 |
| Non-invasive ventilation (%) | 62 (31.0%) | 28 (45.2%) | 119 (53.1%) | <0.001 | 0.266 |
| Discharge status (recovered) (%) | 193 (96.5%) | 57 (91.9%) | 198 (88.4%) | 0.008 | 0.427 |
| Year | COVID-19 Severity | Length of Hospital Stay | ICU Admissions | Mortality | ||||
|---|---|---|---|---|---|---|---|---|
| T1D | T2D | T1D | T2D | T1D | T2D | T1D | T2D | |
| 2020 | Moderate: 30.6%, Severe: 14.5% | Moderate: 33.9%, Severe: 17.0% | 9.0 ± 5.8 * | 10.8 ± 6.1 * | 11.3% | 15.2% | 4.0% | 5.6% |
| 2021 | Moderate: 35.5%, Severe: 20.3% | Moderate: 40.2%, Severe: 25.0% | 9.9 ± 6.3 * | 12.4 ± 6.9 * | 19.4% | 26.3% | 7.7% | 11.2% |
| 2022 | Moderate: 32.3%, Severe: 16.1% | Moderate: 36.6%, Severe: 21.9% | 7.8 ± 4.9 * | 9.6 ± 5.6 * | 14.5% | 20.5% | 6.1% | 9.4% |
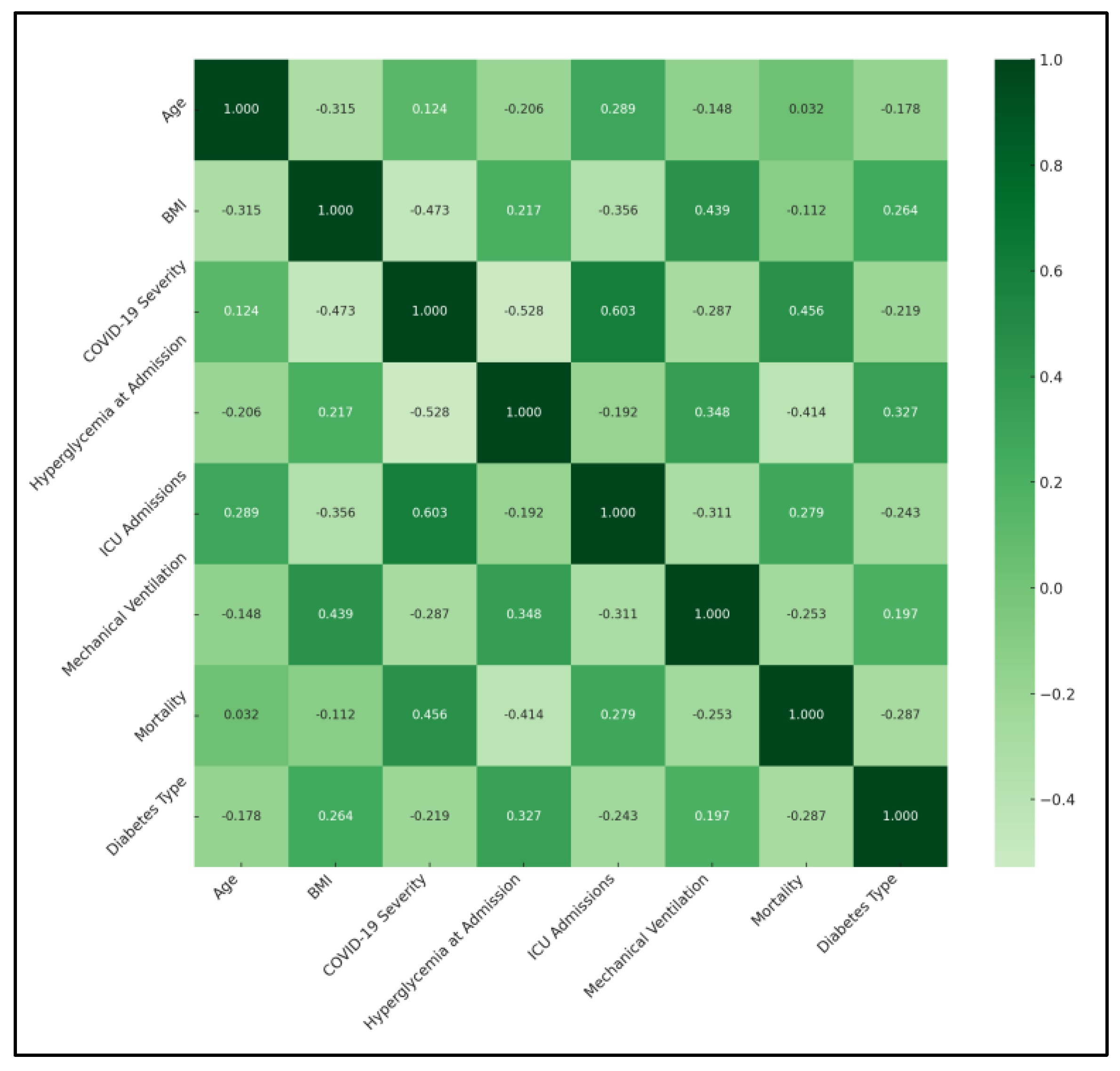
| Variables | Age | BMI | COVID-19 Severity | Hyperglycemia at Admission | ICU Admissions | Mechanical Ventilation | Mortality | Diabetes Type |
|---|---|---|---|---|---|---|---|---|
| Age | 1 | −0.315 | 0.124 | −0.206 | 0.289 * | −0.148 | 0.032 | −0.178 |
| BMI | −0.315 | 1 | −0.473 * | 0.217 | −0.356 | 0.439 * | −0.112 | 0.264 |
| COVID-19 Severity | 0.124 | −0.473 * | 1 | −0.528 * | 0.603 * | −0.287 | 0.456 * | −0.219 |
| Hyperglycemia at Admission | −0.206 | 0.217 | −0.528 * | 1 | −0.192 | 0.348 | −0.414 * | 0.327 |
| ICU Admissions | 0.289 * | −0.356 | 0.603 * | −0.192 | 1 | −0.311 | 0.279 | −0.243 |
| Mechanical Ventilation | −0.148 | 0.439 * | −0.287 | 0.348 | −0.311 | 1 | −0.253 | 0.197 |
| Mortality | 0.032 | −0.112 | 0.456 * | −0.414 * | 0.279 | −0.253 | 1 | −0.287 |
| Diabetes Type | −0.178 | 0.264 | −0.219 | 0.327 | −0.243 | 0.197 | −0.287 | 1 |
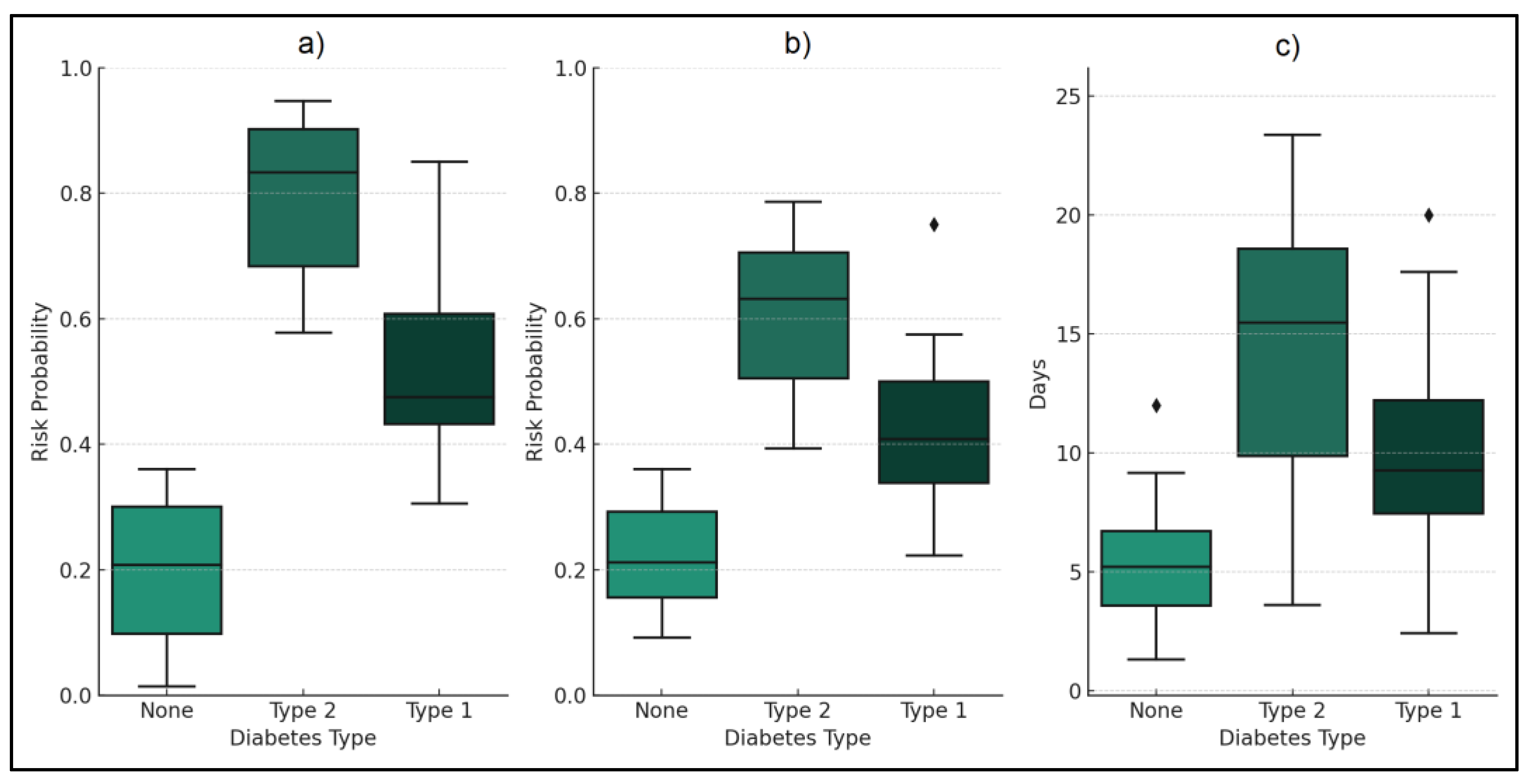
| Variables | No Diabetes (n = 200) | T1D (n = 62) | T2D (n = 224) | OR (T2D vs. None) (95% CI) | OR (T2D vs. T1D) (95% CI) |
|---|---|---|---|---|---|
| ICU admission risk | 17.00% | 22.60% | 31.70% | 2.24 (1.40–3.57) * | 1.59 (1.09–2.83) * |
| Mechanical Ventilation Risk | 18.00% | 29.00% | 35.30% | 2.46 (1.55–3.90) * | 1.37 (0.81–2.30) |
| Mortality | 3.50% | 8.10% | 11.60% | 3.60 (1.08–8.20) * | 1.48 (0.58–3.76) |
| Hospitalization Duration (Days) | 7.2 ± 6.6 | 9.1 ± 5.8 | 11.6 ± 7.0 | 1.61 (1.25–2.08) * | 1.28 (1.07–1.68) * |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Cioca, F.; Timar, R.; Ignuta, F.; Vlad, A.; Bratosin, F.; Rosca, O.; Jianu, A.M.; Rosca, D.; Septimiu-Radu, S.; Burtic, S.-R.; et al. Comparative Analysis of COVID-19 Outcomes in Type 1 and Type 2 Diabetes: A Three-Year Retrospective Study. Medicina 2024, 60, 210. https://doi.org/10.3390/medicina60020210
Cioca F, Timar R, Ignuta F, Vlad A, Bratosin F, Rosca O, Jianu AM, Rosca D, Septimiu-Radu S, Burtic S-R, et al. Comparative Analysis of COVID-19 Outcomes in Type 1 and Type 2 Diabetes: A Three-Year Retrospective Study. Medicina. 2024; 60(2):210. https://doi.org/10.3390/medicina60020210
Chicago/Turabian StyleCioca, Flavius, Romulus Timar, Flavia Ignuta, Adrian Vlad, Felix Bratosin, Ovidiu Rosca, Adelina Maria Jianu, Daniela Rosca, Susa Septimiu-Radu, Sonia-Roxana Burtic, and et al. 2024. "Comparative Analysis of COVID-19 Outcomes in Type 1 and Type 2 Diabetes: A Three-Year Retrospective Study" Medicina 60, no. 2: 210. https://doi.org/10.3390/medicina60020210
APA StyleCioca, F., Timar, R., Ignuta, F., Vlad, A., Bratosin, F., Rosca, O., Jianu, A. M., Rosca, D., Septimiu-Radu, S., Burtic, S.-R., Fildan, A. P., & Laitin, S. M. D. (2024). Comparative Analysis of COVID-19 Outcomes in Type 1 and Type 2 Diabetes: A Three-Year Retrospective Study. Medicina, 60(2), 210. https://doi.org/10.3390/medicina60020210







