Retrospective Study on Orthodontic Gingival Recession Correction Using Clear Aligners
Abstract
1. Introduction
- Recession type 1 (RT1) refers to gingival recession without interproximal attachment loss. The interproximal cementoenamel junction (CEJ) is not clinically detectable in the mesial and distal tooth parts. Complete coverage of the exposed tooth is possible.
- Recession type 2 (RT2) refers to the involvement of the interproximal attachment. The extent of interproximal attachment loss, measured by the distance from the interproximal CEJ to the interproximal depth, is typically less than or equal to the loss of vestibular attachment. This type of recession commonly occurs in malpositioned, rotated, or extruded vestibular teeth. While complete coverage of the exposed tooth may be achieved, the success rates are generally lower than RT1.
- Recession type 3 (RT3) is characterized by gingival recession with a loss of interproximal attachment, making the CEJ visible. The extent of interproximal attachment loss exceeds that of vestibular attachment loss. Achieving complete coverage of the roots is not feasible, but intervening to achieve a partial result is not contraindicated.
2. Materials and Methods
- Recession depth (RD) from the free gingival margin to the cementoenamel junction (CEJ);
- If present, loss of vestibular and interdental attachment or probing pocket depth (PPD), where gingival recession measurements were taken by two doctors, who then compared their results for validation, and if their measurements did not match, they repeated the process together.
3. Results
- -
- 9 in the upper central incisors;
- -
- 12 in the upper lateral incisors;
- -
- 29 in the lower central incisors;
- -
- 25 in the lower lateral incisors;
- -
- 12 in the upper canines;
- -
- 18 in the lower canines;
- -
- 22 in premolars;
- -
- 19 in molars.
4. Discussions
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Imber, J.C.; Kasaj, A. Treatment of Gingival Recession: When and How? Int. Dent. J. 2021, 71, 178–187. [Google Scholar] [CrossRef] [PubMed]
- Saab, F.J.; de Freitas, D.S.; Cotrin, P.; Oliveira, R.C.; Valarelli, F.P.; de Oliveira, R.C.G.; Salmeron, S.; Pinzan Vercelino, C.R.M.; Freitas, K.M.S. Comparison of Gingival Recession of Mandibular Incisors of Class III Patients Immediately after Compensatory or Surgical Orthodontic Treatment. Eur. J. Dent. 2023, 17, 1089–1096. [Google Scholar] [CrossRef] [PubMed]
- Górski, B.; Górska, R.; Wysokińska-Miszczuk, J.; Kaczyński, T. Tunnel technique with enamel matrix derivative in addition to subepithelial connective tissue graft compared with connective tissue graft alone for the treatment of multiple gingival recessions: A randomized clinical trial. Clin. Oral. Investig. 2020, 12, 4475–4486. [Google Scholar] [CrossRef] [PubMed]
- Penoni, D.C.; Gomes Miranda, M.E.D.S.N.; Sader, F.; Vettore, M.V.; Leão, A.T.T. Factors Associated with Noncarious Cervical Lesions in Different Age Ranges: A Cross-sectional Study. Eur. J. Dent. 2021, 15, 325–331. [Google Scholar] [CrossRef] [PubMed]
- Lee, J.B.; Baek, S.J.; Kim, M.; Pang, E.K. Correlation analysis of gingival recession after orthodontic treatment in the anterior region: An evaluation of soft and hard tissues. J. Periodontal Implant. Sci. 2020, 28, 146–158. [Google Scholar] [CrossRef]
- Meeran, N.A. Iatrogenic possibilities of orthodontic treatment and modalities of prevention. J. Orthod. Sci. 2013, 2, 73–86. [Google Scholar] [CrossRef]
- Wang, T.; Zhao, R.; Yang, R.; Li, Y.; Lien, H.L.; Mei, L.; Nogueira, G. Perceptions of NZ orthodontists and periodontists on the management of gingival recession in orthodontic patients. Aust. Dent. J. 2022, 67 (Suppl. 1), 41–49. [Google Scholar] [CrossRef]
- Feu, D. Orthodontic treatment of periodontal patients: Challenges and solutions, from planning to retention. Dent. Press J. Orthod. 2020, 25, 79–116. [Google Scholar] [CrossRef]
- Alasiri, M.M.; Almalki, A.; Alotaibi, S.; Alshehri, A.; Alkhuraiji, A.A.; Thomas, J.T. Association between Gingival Phenotype and Periodontal Disease Severity-A Comparative Longitudinal Study among Patients Undergoing Fixed Orthodontic Therapy and Invisalign Treatment. Healthcare 2024, 14, 656. [Google Scholar] [CrossRef]
- Ali, A.S.T.; Varghese, S.S.; Shenoy, R.P. Association Between Cervical Abrasion, Oral Hygiene Practices and Buccolingual Dimension of Tooth Surfaces: A Cross-Sectional Study. J. Pharm. Bioallied Sci. 2022, 14 (Suppl. 1), 403–409. [Google Scholar] [CrossRef]
- Ishak, H.; Field, J.; German, M. Baseline Specimens of Erosion and Abrasion Studies. Eur. J. Dent. 2021, 15, 369–378. [Google Scholar] [CrossRef] [PubMed]
- Kulkarni, V.; Duruel, O.; Ataman-Duruel, E.T.; Tözüm, M.D.; Nares, S.; Tözüm, T.F. In-depth morphological evaluation of tooth anatomic lengths with root canal configurations using cone beam computed tomography in North American population. J. Appl. Oral Sci. 2020, 28, e20190103. [Google Scholar] [CrossRef] [PubMed]
- Cepeda, M.S.; Weinstein, R.; Blacketer, C.; Lynch, M.C. Association of flossing/inter-dental cleaning and periodontitis in adults. J. Clin. Periodontol. 2017, 44, 866–871. [Google Scholar] [CrossRef]
- Mythri, S.; Arunkumar, S.M.; Hegde, S.; Rajesh, S.K.; Munaz, M.; Ashwin, D. Etiology and occurrence of gingival recession—An epidemiological study. J. Indian Soc. Periodontol. 2015, 19, 671–675. [Google Scholar] [CrossRef]
- Cairo, F.; Nieri, M.; Cincinelli, S.; Mervelt, J.; Pagliaro, U. The interproximal clinical attachment level to classify gingival recessions and predict root coverage outcomes: An explorative and reliability study. J. Clin. Periodontol. 2011, 38, 661–666. [Google Scholar] [CrossRef]
- Miller, P.D., Jr. A classification of marginal tissue recession. Int. J. Periodontics Restor. Dent. 1985, 5, 8–13. [Google Scholar] [PubMed]
- Pini-Prato, G. The Miller classification of gingival recession: Limits and drawbacks. J. Clin. Periodontol. 2011, 38, 243–245. [Google Scholar] [CrossRef] [PubMed]
- Fageeh, H.I.; Fageeh, H.N.; Bhati, A.K.; Thubab, A.Y.; Sharrahi, H.M.H.; Aljabri, Y.S.; Alotaibi, F.I. Assessing the Reliability of Miller’s Classification and Cairo’s Classification in Classifying Gingival Recession Defects: A Comparison Study. Medicina 2024, 25, 205. [Google Scholar] [CrossRef]
- Fernández-Jiménez, A.; García-De-La-Fuente, A.M.; Estefanía-Fresco, R.; Marichalar-Mendia, X.; Aguirre-Urizar, J.M.; Aguirre-Zorzano, L.A. Complete root coverage in the treatment of Miller class III or RT2 gingival recessions: A systematic review and meta-analysis. BMC Oral Health 2021, 22, 145. [Google Scholar] [CrossRef]
- Malhotra, S.; Tewari, S.; Sharma, R.; Sharma, R.K.; Tanwar, N.; Arora, R. Clinical evaluation of root coverage in Miller class III/RT2 labial gingival recession treated with interdisciplinary periodontal-orthodontic therapy: A randomized controlled clinical trial. J. Periodontal Implant. Sci. 2024, 54, 265–279. [Google Scholar] [CrossRef]
- Rotundo, R.; Genzano, L.; Nieri, M.; Covani, U.; Peñarrocha-Oltra, D.; Peñarrocha-Diago, M. Smile esthetic evaluation of mucogingival reconstructive surgery. Odontology 2021, 109, 295–302. [Google Scholar] [CrossRef] [PubMed]
- Pedowska, M.; Prokop, M.; Chałas, R.; Ptasiewicz, M. The Use of Collagen Matrix in the Treatment of Gingival Recession-A Pilot Study. J. Pers. Med. 2022, 12, 1902. [Google Scholar] [CrossRef] [PubMed]
- Jati, A.S.; Furquim, L.Z.; Consolaro, A. Gingival recession: Its causes and types, and the importance of orthodontic treatment. Dent. Press J. Orthod. 2016, 21, 18–29. [Google Scholar] [CrossRef]
- Goncharuk-Khomyn, M.; Krasnokutskyy, O.; Boichuk, M.; Rusyn, V.; Hliudzyk-Shemota, M. Spontaneous Recession Repair after Orthodontic Treatment: Case Report with the Use of Digital Approach for Quantification of Soft Tissue Changes. Case Rep. Dent. 2023, 24, 1831125. [Google Scholar] [CrossRef]
- Laursen, M.G.; Rylev, M.; Melsen, B. The role of orthodontics in the repair of gingival recessions. Am. J. Orthod. Dentofac. Orthop. 2020, 157, 29–34. [Google Scholar] [CrossRef] [PubMed]
- Schmidlin, P.R.; Sahrmann, P. Current management of dentin hypersensitivity. Clin. Oral Investig. 2013, 17, 55–59. [Google Scholar] [CrossRef]
- Kalina, E.; Grzebyta, A.; Zadurska, M. Bone Remodeling during Orthodontic Movement of Lower Incisors-Narrative Review. Int. J. Environ. Res. Public Health 2022, 19, 15002. [Google Scholar] [CrossRef]
- Kau, C.H.; Soh, J.; Christou, T.; Mangal, A. Orthodontic Aligners: Current Perspectives for the Modern Orthodontic Office. Medicina 2023, 59, 1773. [Google Scholar] [CrossRef]
- Tamer, İ.; Öztaş, E.; Marşan, G. Orthodontic Treatment with Clear Aligners and The Scientific Reality Behind Their Marketing: A Literature Review. Turk. J. Orthod. 2019, 32, 241–246. [Google Scholar] [CrossRef]
- Katib, H.S.; Hakami, A.M.; Albalawei, M.; Alhajri, S.A.; Alruwaily, M.S.; Almusallam, M.I.; Alqahtani, G.H. Stability and Success of Clear Aligners in Orthodontics: A Narrative Review. Cureus 2024, 16, 52038. [Google Scholar] [CrossRef]
- Mendes Ribeiro, S.M.; Aragón, M.L.S.C.; Espinosa, D.D.S.G.; Shibasaki, W.M.M.; Normando, D. Orthodontic aligners: Between passion and science. Dent. Press J. Orthod. 2024, 28, e23spe6. [Google Scholar] [CrossRef] [PubMed]
- Di Spirito, F.; D’Ambrosio, F.; Cannatà, D.; D’Antò, V.; Giordano, F.; Martina, S. Impact of Clear Aligners versus Fixed Appliances on Periodontal Status of Patients Undergoing Orthodontic Treatment: A Systematic Review of Systematic Reviews. Healthcare 2023, 11, 1340. [Google Scholar] [CrossRef] [PubMed]
- Figueiredo, M.A.; Romano, F.L.; Feres, M.F.N.; Stuani, M.B.S.; Nahás-Scocate, A.C.R.; Matsumoto, M.A.N. Effectiveness of Invisalign® aligners in the treatment of severe gingival recession: A case report. Korean J. Orthod. 2021, 51, 293–300. [Google Scholar] [CrossRef] [PubMed]
- AlMogbel, A. Clear Aligner Therapy: Up to date review article. J. Orthod. Sci. 2023, 12, 37. [Google Scholar] [CrossRef]
- Fitzgerald, B.P.; Hawley, C.E.; Harrold, C.Q.; Garrett, J.S.; Polson, A.M.; Rams, T.E. Reproducibility of Manual Periodontal Probing Following a Comprehensive Standardization and Calibration Training Program. J. Oral Biol. 2022, 8, 0063. [Google Scholar] [CrossRef]
- Pradeep, K.; Rajababu, P.; Satyanarayana, D.; Sagar, V. Gingival recession: Review and strategies in treatment of recession. Case Rep. Dent. 2012, 2012, 563421. [Google Scholar] [CrossRef]
- Crego-Ruiz, M.; Jorba-García, A. Assessment of the periodontal health status and gingival recession during orthodontic treatment with clear aligners and fixed appliances: A systematic review and meta-analysis. Med. Oral. Patol. Oral. Cir. Bucal. 2023, 28, 330–340. [Google Scholar] [CrossRef]
- Alsalhi, R.H.; Tabasum, S.T. Prevalence of gingival recession and its correlation with gingival phenotype in mandibular incisors region of orthodontically treated female patients: A cross-sectional study. J. Indian Soc. Periodontol. 2021, 25, 341–346. [Google Scholar] [CrossRef]
- Northway, W.M. Gingival recession--can orthodontics be a cure? Angle Orthod. 2013, 83, 1093–1101. [Google Scholar] [CrossRef]
- Romano, F.; Perotto, S.; Baima, G.; Macrì, G.; Picollo, F.; Romandini, M.; Mariani, G.M.; Aimetti, M. Estimates and multivariable risk assessment of mid-buccal gingival recessions in an Italian adult population according to the 2018 World Workshop Classification System. Clin. Oral Investig. 2022, 26, 4769–4780. [Google Scholar] [CrossRef]
- Romandini, M.; Soldini, M.C.; Montero, E.; Sanz, M. Epidemiology of mid-buccal gingival recessions in NHANES according to the 2018 World Workshop Classification System. J. Clin. Periodontol. 2020, 47, 1180–1190. [Google Scholar] [CrossRef] [PubMed]
- Ristoska, S.; Dzipunova, B.; Stefanovska, E.; Rendzova, V.; Radojkova-Nikolovska, V.; Evrosimovska, B. Orthodontic Treatment of a Periodontally—Affected Adult Patient (Case Report). Open Access Maced. J. Med. Sci. 2019, 14, 2343–2349. [Google Scholar] [CrossRef]
- Papageorgiou, S.N.; Antonoglou, G.N.; Eliades, T.; Martin, C.; Sanz, M. Orthodontic treatment of patients with severe (stage IV) periodontitis. Semin. Orthod. 2024, 30, 123–134. [Google Scholar] [CrossRef]
- Samulak, R.; Suwała, M.; Górski, B.; Machoy, M. Evaluating Clear Aligners Versus Fixed Appliances for Periodontal Patients: A Comprehensive Narrative Review of Current Evidence. Appl. Sci. 2024, 14, 9931. [Google Scholar] [CrossRef]
- Papageorgiou, S.N.; Koletsi, D.; Iliadi, A.; Peltomaki, T.; Eliades, T. Treatment outcome with orthodontic aligners and fixed appliances: A systematic review with meta-analyses. Eur. J. Orthod. 2020, 42, 331–343. [Google Scholar] [CrossRef] [PubMed]
- Nazir, M.A. Prevalence of periodontal disease, its association with systemic diseases and prevention. Int. J. Health Sci. 2017, 11, 72–80. [Google Scholar] [PubMed] [PubMed Central]
- Ustun, K.; Sari, Z.; Orucoglu, H.; Duran, I.; Hakki, S.S. Severe gingival recession caused by traumatic occlusion and mucogingival stress: A case report. Eur J Dent 2008, 2, 127–133. [Google Scholar] [CrossRef] [PubMed]
- Bucur, S.M.; Iantovics, L.B.; Bud, A.; Bud, E.S.; Cocoș, D.I.; Vlasa, A. Retrospective Study Regarding Orthodontic Retention Complications in Clinical Practice. Appl. Sci. 2022, 12, 273. [Google Scholar] [CrossRef]
- Bucur, S.M.; Chiarati, C.R.; Avino, P.; Migliorino, I.; Cocoș, D.I.; Bud, E.S.; Bud, A.; Vlasa, A. Retrospective Study Regarding the Status of the Superficial Marginal Periodontium in Adult Patients Wearing Orthodontic Retainers. Rom. J. Oral Rehabil. 2021, 13, 194–201. [Google Scholar]
- Moga, R.-A.; Olteanu, C.D.; Delean, A.G. Investigating the Ability of the Tooth and Surrounding Support Tissues to Absorb and Dissipate Orthodontic Loads during Periodontal Breakdown—Finite Elements Analysis. Appl. Sci. 2024, 14, 1041. [Google Scholar] [CrossRef]
- Moga, R.A.; Olteanu, C.D.; Buru, S.M.; Botez, M.D.; Delean, A.G. Finite Elements Analysis of Biomechanical Behavior of the Bracket in a Gradual Horizontal Periodontal Breakdown—A Comparative Analysis of Multiple Failure Criteria. Appl. Sci. 2023, 13, 9480. [Google Scholar] [CrossRef]
- Moga, R.A.; Delean, A.G.; Buru, S.M.; Botez, M.D.; Olteanu, C.D. Orthodontic Internal Resorption Assessment in Periodontal Breakdown-A Finite Elements Analysis (Part II). Healthcare 2023, 11, 2622. [Google Scholar] [CrossRef] [PubMed]


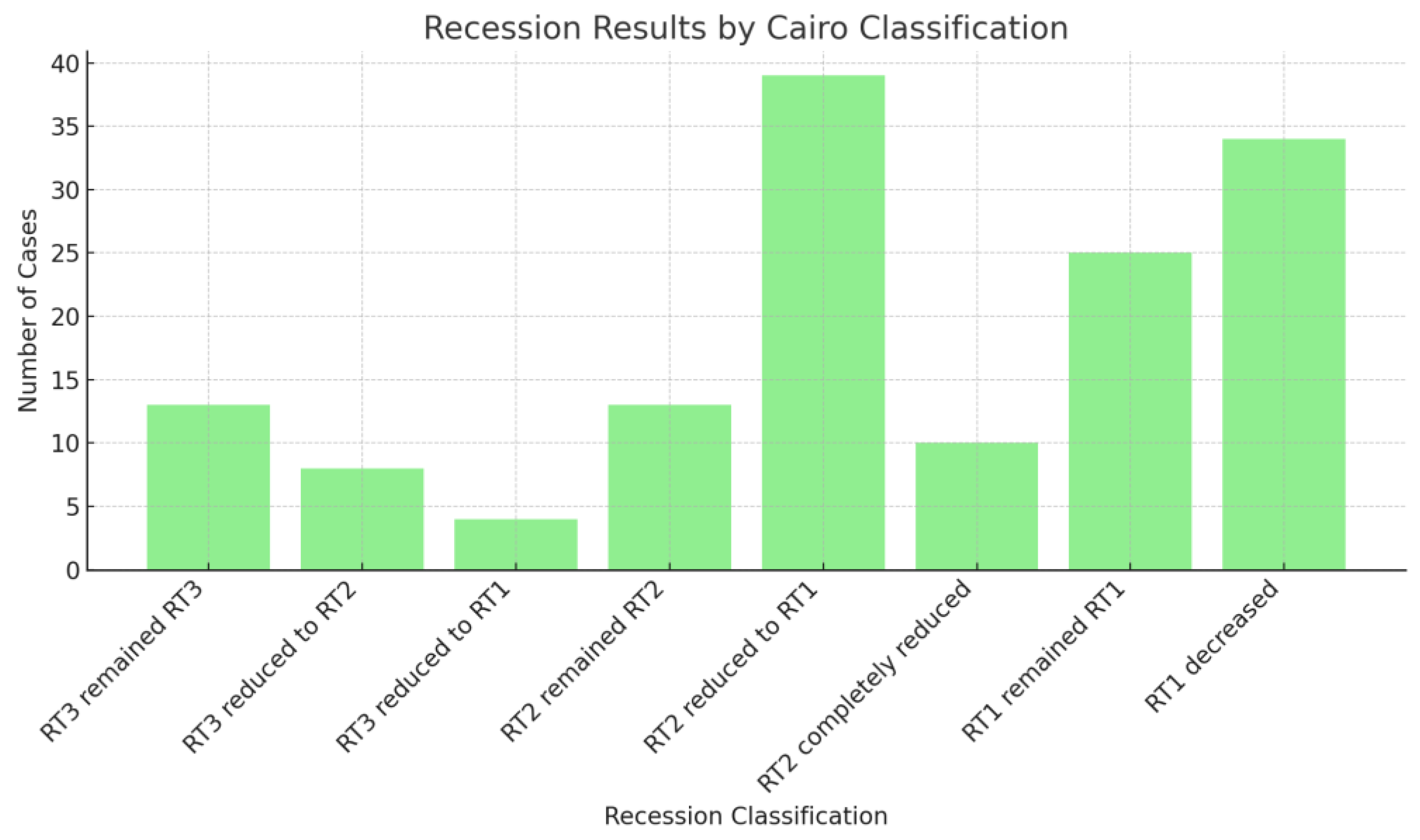




| Initial Classification | Stayed the Same | Improved One Level | Improved Two Levels | Completely Resolved | Further Decreased |
|---|---|---|---|---|---|
| RT3 (n = 25) | 52% (13) | 32% (8) | 16% (4) | N/A | N/A |
| RT2 (n = 62) | 21% (13) | 62.9% (39) | N/A | 16.1% (10) | N/A |
| RT1 (n = 59) | 42.4% (25) | N/A | N/A | N/A | 57.6% (34) |
| Category | Improved | Not Improved | Total |
|---|---|---|---|
| RT3 | 12 | 13 | 25 |
| RT2 | 49 | 13 | 62 |
| RT1 | 34 | 25 | 59 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Published by MDPI on behalf of the Lithuanian University of Health Sciences. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Bucur, S.M.; Bud, E.; Decusară, M.; Olteanu, C.-D. Retrospective Study on Orthodontic Gingival Recession Correction Using Clear Aligners. Medicina 2024, 60, 2024. https://doi.org/10.3390/medicina60122024
Bucur SM, Bud E, Decusară M, Olteanu C-D. Retrospective Study on Orthodontic Gingival Recession Correction Using Clear Aligners. Medicina. 2024; 60(12):2024. https://doi.org/10.3390/medicina60122024
Chicago/Turabian StyleBucur, Sorana Maria, Eugen Bud, Mioara Decusară, and Cristian-Doru Olteanu. 2024. "Retrospective Study on Orthodontic Gingival Recession Correction Using Clear Aligners" Medicina 60, no. 12: 2024. https://doi.org/10.3390/medicina60122024
APA StyleBucur, S. M., Bud, E., Decusară, M., & Olteanu, C.-D. (2024). Retrospective Study on Orthodontic Gingival Recession Correction Using Clear Aligners. Medicina, 60(12), 2024. https://doi.org/10.3390/medicina60122024






